Abstract
Background
Prior studies have suggested gender-based differences in the care of elderly patients with acute medical conditions such as myocardial infarction and stroke, but it is unknown whether these differences are seen in the care of abdominal pain.
Study Objectives
To examine differences in evaluation, management, and diagnoses between elderly men and women presenting to the emergency department with abdominal pain.
Methods
Observational cohort study; chart review of consecutive patients 70 years or age or older presenting with a chief complaint of abdominal pain. Primary outcomes were care processes (e.g. receipt of pain medications, imaging) and clinical outcomes (e.g. hospitalization, etiology of pain, and mortality).
Results
Of 131 patients evaluated, 60% were women. Groups were similar in age, ethnicity, insurance status, and predicted mortality. Men and women did not differ in the frequency of medical (56% vs. 57%), surgical (25% vs. 18%), or non-specific abdominal pain (19% vs. 25%, p=0.52) diagnoses. Similar proportions underwent abdominal imaging (62% vs. 68%, p=0.42), received antibiotics (29% vs. 30%, p=0.85), and opiates for pain (35% vs. 41%, p=0.50). Men had a higher rate of death within three months of the visit (19% vs. 1%, p<0.001).
Conclusion
Unlike prior research in younger patients with abdominal pain and among elders with other acute conditions, we noted no difference in management and diagnoses between older men and women with who presented with abdominal pain. Despite a similar predicted mortality and ED evaluation, men had a higher rate of death within three months.
Keywords: Abdominal pain, Gender, Emergency department, Geriatrics, Elderly
INTRODUCTION
7.6 million people a year visit emergency departments with abdominal pain, making it the most common reason for Emergency Department (ED) visits in the United States (1). Older patients with abdominal pain have a high likelihood of being admitted (2–4), often require surgical intervention (2, 5), and have a high mortality rate (3, 5). These associations may exist because elders manifest abdominal pathology atypically or because non-abdominal illnesses (e.g. myocardial infarction) may present as abdominal pain (2, 4, 6). As a result, guidelines caution against giving a diagnosis of nonspecific abdominal pain to older patients (7), and the evaluation of abdominal pain in elders is a time-consuming and expensive endeavor in the ED (8–10).
Although few studies have examined gender differences in the management and outcomes of elders with abdominal pain specifically, gender-based comparisons have been described in the care of elders with other acute medical conditions. Older men with chest pain or acute myocardial infarction may receive angiography and reperfusion more often than women (11–13), and men are more likely to get aspirin after acute coronary syndromes (13–15). Older women hospitalized for stroke are less likely to undergo brain imaging, doppler examination, echocardiogram, and angiography, as well as carotid surgery (16, 17). They are also less likely to receive aspirin, ticlopidine, angiotensin converting enzyme inhibitors, and statins after a cerebrovascular event (18, 19).
Despite the prevalence of the problem, there are few data to describe whether age and gender influence the management, workup, and eventual diagnosis in older patients presenting to the ED with abdominal pain. In particular, there are few data to describe whether gender influences the likelihood of an elder receiving pain medication, undergoing imaging, or leaving the ED with a diagnosis of non-specific abdominal pain. We undertook a retrospective analysis of emergency department visits to examine our hypothesis that gender would play an important role in abdominal pain evaluation and outcomes in elderly patients.
MATERIALS AND METHODS
Study Setting
The study site was the emergency department (ED) at the University of California, San Francisco (UCSF), an academic medical center providing quaternary care for a predominantly urban population. The UCSF ED has 40,000 patient visits per year.
At UCSF, adult patients with abdominal pain are initially evaluated by the ED service, composed of emergency medicine and internal medicine residents supervised by an attending physician board certified in emergency medicine. Further evaluation by surgical residents is at the discretion of the ED or the admitting services. There are no specific guidelines for managing abdominal pain and no systematic differences in how older patients receive care (i.e., no geriatrics unit, no standard criteria for surgical consultation) in the ED or hospital.
Our research was approved by the institutional review board of the University of California, San Francisco Medical Center.
Selection of Participants
Patients were included in the study if they had been seen in the UCSF ED between June 1, 2004 and August 31, 2004, were aged 70 or more, and had a chief complaint of abdominal pain. After reviewing every chart from the study period, we identified 131 consecutive subjects who reported abdominal pain as their chief complaint to either the triage nurse or the initial treating physician. This sample size was chosen in order to provide 80% power to detect a 25% absolute difference in discharge diagnosis frequency between men and women. While this might seem a large effect size, it is consistent with other studies of disparities(20–22). We chose 70 as our age cutoff to be consistent with other studies examining a geriatric population (23–26).
Data Collection
Data were abstracted from ED physician documentation, nursing notes, and medication records. If a patient was admitted, electronic and paper hospital records were reviewed to obtain information on further laboratory and radiographic studies, operative interventions, and final discharge diagnoses. Death dates for patients were obtained from the Social Security Death Index (27).
One reviewer (RG) abstracted charts and the electronic records using a data collection tool developed specifically for the study; the abstractor was not blinded to study objectives. Our chart abstraction process collected patient demographics, patient clinical characteristics (such as duration of abdominal pain, comorbidities, recent surgery), elements of the ED evaluation and management (such as use of imaging and pain medications), ED diagnosis, and hospital discharge diagnosis.
Discharge diagnoses were grouped a priori into three categories: medical causes of abdominal pain (e.g., urinary tract infection, myocardial infarction), surgical causes of abdominal pain (e.g., cholecystitis, small bowel obstruction), and nonspecific abdominal pain. The final discharge diagnosis was defined as the ED diagnosis if the patient was discharged home from the emergency department and was defined as the hospital discharge diagnosis if the patient was admitted to the hospital. For a nonspecific abdominal pain diagnosis, we included “nonspecific abdominal pain,” “undifferentiated abdominal pain,” “abdominal pain of unknown etiology,” or “abdominal pain not otherwise specified.” Two of the authors (RG and AA) independently determined the diagnosis category for each patient, and then resolved disagreements by consensus.
Statistical Analysis
A two-sided p-value of ≤ 0.05 was considered statistically significant. Chi-square tests and Wilcoxon rank sum tests were employed to test for differences in demographic characteristics, ED management, and hospital course and follow-up. We performed a sensitivity analysis excluding patients with a pain duration of more than seven days. A log rank test was used to compare survival curves. All analyses were performed using SAS statistical software (9th version; Cary, NC).
RESULTS
Baseline Characteristics (Table 1)
TABLE 1.
Baseline Characteristics of the Study Subjects*
| Characteristics | Men (n = 52) |
Women (n = 79) |
|---|---|---|
| Age, y | ||
| 70–79 | 24 (46%) | 38 (49%) |
| 80–89 | 22 (42%) | 31 (39%) |
| > or = 90 | 6 (12%) | 10 (12%) |
| Ethnicity | ||
| White | 25 (48%) | 29 (37%) |
| Black | 6 (12%) | 10 (13%) |
| Asian | 18 (35%) | 27 (34%) |
| Other | 3 (6%) | 13 (16%) |
| Primary language English | 31 (60%) | 45 (57%) |
| Medicare | 34 (81%) | 60 (88%) |
| Symptom duration, days | ||
| Median (range)† | 1 (1, 120) | 2 (1, 365) |
| Time of arrival in ED | ||
| Day (07:00 – 18:59) | 32 (62%) | 47 (59%) |
| Night (19:00 – 06:59) | 20 (38%) | 32 (41%) |
| Comorbidities | ||
| Asthma/COPD | 6 (12%) | 11 (14%) |
| Coronary artery disease | 16 (31%) | 26 (33%) |
| Cerebrovascular disease | 8 (15%) | 17 (22%) |
| Cancer – not metastatic | 9 (17%) | 13 (16%) |
| Cancer – metastatic | 2 (4%) | 1 (1%) |
| Past gastrointestinal bleeding | 6 (12%) | 4 (5%) |
| Chronic kidney disease | 6 (12%) | 6 (8%) |
| Charlson index(46) | ||
| Median (range)† | 1(0,10) | 1(0,6) |
ED = emergency department; COPD = chronic obstructive pulmonary disease.
P > 0.05 for all comparisons, by Chi-squared analysis except as noted.
P > 0.05 by Wilcoxon test of medians.
131 consecutive patients 70 years and older with abdominal pain were evaluated in the ED during the study period. Fifty-two (40%) were men and 79 (60%) were women; mean age was 81 years for men and 80 for women (p = 0.94). Other characteristics were similar in both groups, including ethnicity, primary language, insurance status, and baseline comorbidity.
ED Management (Table 2)
TABLE 2.
| Emergency Department Management* | ||
|---|---|---|
| Management | Men (n = 52) |
Women (n=79) |
| Time to evaluation, min | ||
| Median (range)† | 20 (0–125) | 24 (0–190) |
| Physical exam performed | ||
| Abdominal | 51 (98%) | 78 (99%) |
| Rectal | 27 (52%) | 41 (52%) |
| Pelvic or genital | 7 (13%) | 3 (4%) |
| Skin | 36 (69%) | 57 (72%) |
| Pulses | 17 (33%) | 40 (51%) |
| Palpation for aorta | 7 (13%) | 4 (5%) |
| Serial exams | 9 (17%) | 8 (10%) |
| Laboratory tests | ||
| Electrocardiogram | 35 (67%) | 62 (78%) |
| Urinalysis | 42 (81%) | 68 (86%) |
| Complete blood count | 46 (88%) | 74 (94%) |
| Basic metabolic panel | 46 (88%) | 74 (94%) |
| Liver function tests | 42 (81%) | 66 (84%) |
| Amylase or lipase | 37 (71%) | 62 (78%) |
| Oxygen saturation | 51 (98%) | 76 (96%) |
| Hemoccult | 27 (52%) | 41 (52%) |
| Rectal temperature | 3 (6%) | 5 (6%) |
| Troponin | 20 (38%) | 40 (51%) |
| Blood culture | 13 (25%) | 22 (28%) |
| Urine culture | 16 (31%) | 37 (47%) |
| Stool culture | 1 (2%) | 3 (4%) |
| Imaging | ||
| Chest x-ray | 31 (60%) | 56 (71%) |
| KUB | 14 (27%) | 21 (27%) |
| Abdominal ultrasound | 5 (10%) | 19 (24%) |
| Abdominal CT scan | 27 (52%) | 38 (48%) |
| Opioid analgesia | 18 (35%) | 32 (41%) |
| Antibiotics | 15 (29%) | 24 (30%) |
| Surgical consult | 13 (25%) | 17 (22%) |
| Admission | 31 (60%) | 55 (70%) |
| Time in ED (if discharged), min | ||
| Median (range)† | 280 (81,760) | 319 (65,1347) |
| Emergency Department Management* | |||
|---|---|---|---|
| Management | Men (n = 52) |
Women (n=79) |
Difference in percentages (95% CI) |
| Time to evaluation, min | |||
| Median (range)† | 20 (0−125) | 24 (0−190) | 4 (−8, 10) |
| Physical exam performed | |||
| Abdominal | 51 (98%) | 78 (99%) | 1 (−6, 10) |
| Rectal | 27 (52%) | 41 (52%) | 0 (−18, 18) |
| Pelvic or genital | 7 (13%) | 3 (4%) | 9 (−1, 23) |
| Skin | 36 (69%) | 57 (72%) | 3 (−13, 20) |
| Pulses | 17 (33%) | 40 (51%) | 18 (−5, 34) |
| Palpation for aorta | 7 (13%) | 4 (5%) | 8 (−3,22) |
| Serial exams | 9 (17%) | 8 (10%) | 7 (−6, 22) |
| Laboratory tests | |||
| Electrocardiogram | 35 (67%) | 62 (78%) | 11 (−5, 28) |
| Urinalysis | 42 (81%) | 68 (86%) | 5 (−8, 20) |
| Complete blood count | 46 (88%) | 74 (94%) | 6 (−6, 18) |
| Basic metabolic panel | 46 (88%) | 74 (94%) | 6 (−6, 18) |
| Liver function tests | 42 (81%) | 66 (84%) | 3 (−11, 18) |
| Amylase or lipase | 37 (71%) | 62 (78%) | 7 (−8, 24) |
| Oxygen saturation | 51 (98%) | 76 (96%) | 2 (−8, 10) |
| Hemoccult | 27 (52%) | 41 (52%) | 0 (18, 18) |
| Rectal temperature | 3 (6%) | 5 (6%) | 0 (−11, 10) |
| Troponin | 20 (38%) | 40 (51%) | 13 (−6, 29) |
| Blood culture | 13 (25%) | 22 (28%) | 3 (−14, 18) |
| Urine culture | 16 (31%) | 37 (47%) | 16 (−2, 32) |
| Stool culture | 1 (2%) | 3 (4%) | 2 (−8, 10) |
| Imaging | |||
| Chest x-ray | 31 (60%) | 56 (71%) | 11 (−6, 29) |
| KUB | 14 (27%) | 21 (27%) | 0 (−16, 17) |
| Abdominal ultrasound | 5 (10%) | 19 (24%) | 14 (0, 27) |
| Abdominal CT scan | 27 (52%) | 38 (48%) | 4 (−14, 22) |
| Opioid analgesia | 18 (35%) | 32 (41%) | 6 (−12, 23) |
| Antibiotics | 15 (29%) | 24 (30%) | 1 (−16, 18) |
| Surgical consult | 13 (25%) | 17 (22%) | 3 (−12, 20) |
| Admission | 31 (60%) | 55 (70%) | 10 (−7, 27) |
| Time in ED (if discharged), min | |||
| Median (range)† | 280 (81,760) | 319 (65,1347) | 39 (−101, 215) |
KUB = kidney, ureter, and bladder; CT = computed tomography; ED = emergency department.
P > 0.05 for all comparisons, by Chi-squared analysis except as noted.
P > 0.05 by Wilcoxon test of medians.
CI = confidence interval; KUB = kidney, ureter, and bladder; CT = computed tomography; ED = emergency department.
P > 0.05 for all comparisons, by Chi-squared analysis except as noted.
P > 0.05 by Wilcoxon test of medians.
Men and women were managed similarly in the ED. Both groups waited about 20 minutes to see a doctor, and those who were discharged home had a median ED length of stay of 280 minutes for men and 319 minutes for women (p = 0.47). Very few patients of either gender received a pelvic or genital examination: 13% of men and 4% of women. Diagnostic test ordering was similar in both groups, including electrocardiograms, laboratory tests, and imaging studies. About half of the patients, equally divided between men and women, had an abdominal CT scan. Rates of opioid analgesia, antibiotics, and surgical service consultation were also similar.
Hospital Course (Table 3)
TABLE 3.
| Hospital Course and Follow-Up* | ||
|---|---|---|
| Course | Men (n=31) |
Women (n=55) |
| Admitting service | ||
| Medicine | 23 (74%) | 33 (60%) |
| Surgery | 4 (13%) | 12 (22%) |
| Cardiology | 3 (10%) | 9 (16%) |
| Other | 1 (3%) | 1 (2%) |
| Surgical procedure | 5 (16%) | 11 (20%) |
| Endoscopy† | 2 (6%) | 7 (1%) |
| Length of stay, days | ||
| Median (range)‡ | 4 (1–20) | 4 (2–47) |
| ED diagnosis correlated with hospital discharge diagnosis | 16 (52%) | 38 (69%) |
| Return to ED within 7 days of visit§ | 3(6%) | 7(9%) |
| Death within 3 months of visit‖ | 10 (19%) | 1(1%) |
| Hospital Course and Follow-Up* | |||
|---|---|---|---|
| Course | Men (n=31) |
Women (n=55) |
Difference in percentages (95% CI) |
| Admitting service | |||
| Medicine | 23 (74%) | 33 (60%) | 14 (−9, 34) |
| Surgery | 4 (13%) | 12 (22%) | 9 (−11, 25) |
| Cardiology | 3 (10%) | 9 (16%) | 6 (−12, 21) |
| Other | 1 (3%) | 1 (2%) | 1 (−11, 14) |
| Surgical procedure | 5 (16%) | 11 (20%) | 4 (−17, 21) |
| Endoscopy† | 2 (6%) | 7 (1%) | 7 (−12, 20) |
| Length of stay, days | |||
| Median (range)‡ | 4 (1–20) | 4 (2–47) | 0 (−1, 3) |
| ED diagnosis correlated with hospital discharge diagnosis | 16 (52%) | 38 (69%) | 17 (−5, 39) |
| Return to ED within 7 days of visit§ | 3(6%) | 7(9%) | 3 (−9, 13) |
| Death within 3 months of visit‖ | 10 (19%) | 1(1%) | 18 (7, 32) |
P > 0.05 for all comparisons, by Chi-squared analysis except as noted.
Either esophagogastroduodenoscopy, colonoscopy, or endoscopic retrograde cholangiopancreatography. If a subject had more than one procedure, he or she was only counted once.
P > 0.05 by Wilcoxon test of medians.
Compares all of the subjects (52 men and 79 women), not just those hospitalized.
P < 0.0001 by Fisher’s exact test, compares all of the subjects (52 men and 79 women), not just those hospitalized.
CI = confidence interval.
P > 0.05 for all comparisons, by Chi-squared analysis except as noted.
Either esophagogastroduodenoscopy, colonoscopy, or endoscopic retrograde cholangiopancreatography. If a subject had more than one procedure, he or she was only counted once.
P > 0.05 by Wilcoxon test of medians.
Compares all of the subjects (52 men and 79 women), not just those hospitalized.
P < 0.0001 by Fisher’s exact test, compares all of the subjects (52 men and 79 women), not just those hospitalized.
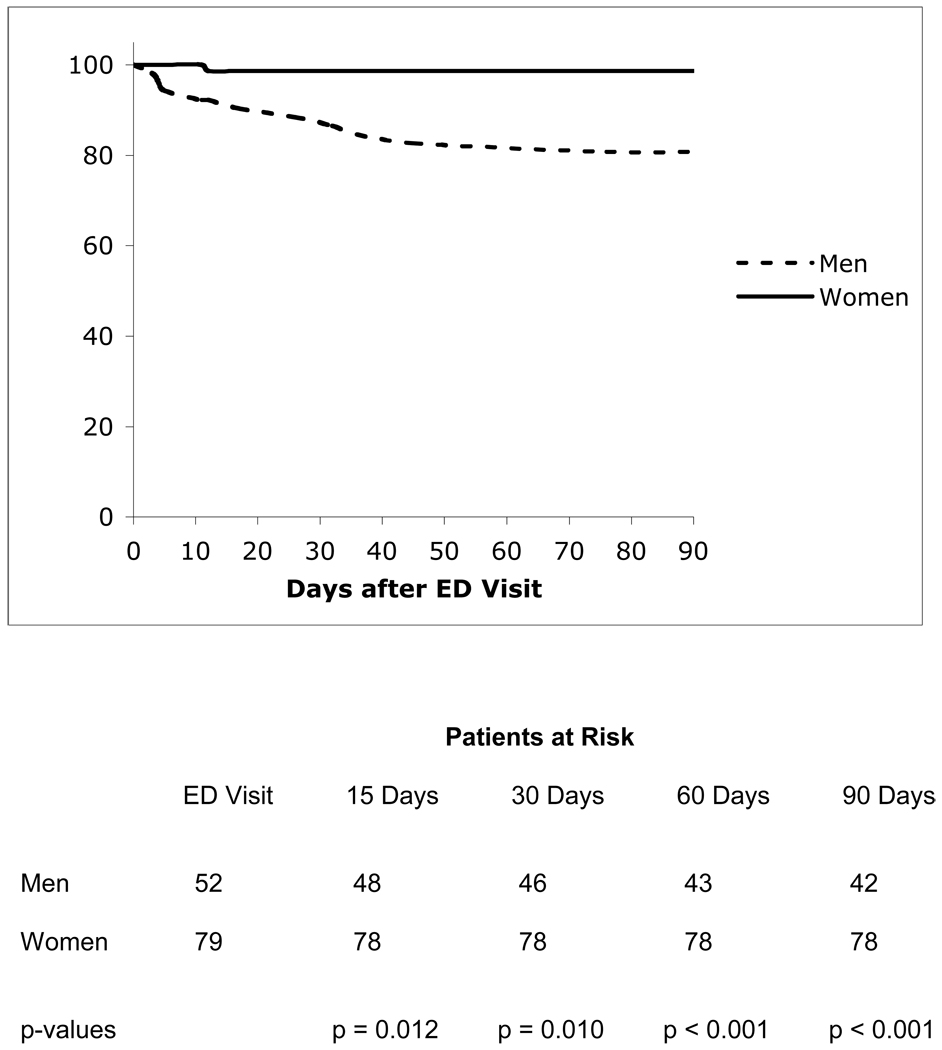
A majority of patients in both groups was admitted—60% of men and 70% of women (p = 0.20). Among the admitted patients, most were admitted to non-surgical services. Five (16%) of the men and 11 (20%) of the women required an operation during the hospitalization (p=0.46). Ten men (19%) died within three months of the ED visit; one woman died (p<0.001) (Figure).
FIGURE. Survival Curves to 90 Days of Follow-up.
Kaplan-Meier survival of patients, stratified by men (broken line) and women (solid line), seen in the Emergency Department (ED) with abdominal pain. The number of patients alive at the time of the ED visit, and at 15, 30, 60, and 90 days of follow-up, is displayed below the figure. P-values compare the survival curves of men and women at each time point, by the log-rank test.
Diagnoses
Among patients who were admitted, the ED diagnosis correlated with the hospital discharge diagnosis in 52% of the men and 69% of the women (p=0.11). There were no differences between elderly men and women in the frequency with which they were assigned a final diagnosis of medical, surgical, or nonspecific abdominal pain (p=0.52 for heterogeneity among the three groups) (Table 4). These results were not significantly changed when subjects with a pain duration of greater than seven days were excluded from the analysis (data not shown). The most common diagnoses for men included biliary disease, nonspecific abdominal pain, urinary retention, and constipation. For women, nonspecific abdominal pain, biliary disease, urinary tract infection, and small bowel obstruction were most commonly diagnosed.
TABLE 4.
| Abdominal Pain Diagnosis Category* | ||
|---|---|---|
| Diagnosis | Men (n=52) |
Women (n=79) |
| Medical | 29 (56%) | 45 (57%) |
| Surgical | 13 (25%) | 14 (18%) |
| NSAP | 10 (19%) | 20 (25%) |
| Abdominal Pain Diagnosis Category* | |||
|---|---|---|---|
| Diagnosis | Men (n=52) |
Women (n=79) |
Difference in percentages (95% CI) |
| Medical | 29 (56%) | 45 (57%) | 1 (−17, 19) |
| Surgical | 13 (25%) | 14 (18%) | 7 (−8, 23) |
| NSAP | 10 (19%) | 20 (25%) | 6 (−10, 21) |
NSAP = nonspecific abdominal pain.
P > 0.05 for all comparisons, by Chi-squared analysis.
CI = confidence interval; NSAP = nonspecific abdominal pain.
P > 0.05 for all comparisons, by Chi-squared analysis.
DISCUSSION
At our site, older men and women with acute abdominal pain were managed similarly in the ED and afterwards, suggesting that gender-based differences seen in the evaluation of other acute illnesses may not extend to abdominal pain. We also found that elderly men with abdominal pain appeared to have a substantially higher mortality in the 3 months after ED evaluation. However, whether this mortality difference represents differences in follow-up or hospital care or underlying comorbidity is unclear.
Several theories have been promulgated to explain why men and women are managed differently when presenting with similar conditions. For elective procedures, divergence in patients’ priorities and in their perceptions about their disease and the efficacy of intervention may drive differences in treatment rates (28, 29). For patients presenting with acute conditions, such as myocardial infarction or stroke, we would expect patient preferences to play less of a role. Anatomic or physiologic distinctions between men and women have been implicated (30, 31), as well as systemic differences in physician decision-making (13, 32). The role of physician bias has been contested, however, by those who have found little evidence for gender-based differences in management after multivariate adjustment (33–35).
While some studies have observed gender-based differences in care or outcomes among elders, others, like ours, have demonstrated comparable management of acute medical conditions. A study looking at the influence of gender on management and outcomes of mechanically ventilated patients in a medical intensive care unit found no difference in the evaluation, treatment, or mortality between men and women over 65 years old (36). Similarly, older men and women admitted to the hospital with bleeding peptic ulcers had had similar rates of surgery and hospital length of stay and no difference in mortality (34). In an older cohort of patients presenting to the ED with a chronic obstructive pulmonary disease exacerbation, men and women had similar ED care and hospital admission rates (37).
Among younger men and women, there are marked gender differences in the etiology and evaluation of abdominal pain. Gynecologic pathology accounts for a significant portion of abdominal pain in women in this age group (38, 39). About 25% of ED visits for abdominal pain result in a diagnosis of nonspecific abdominal pain (2, 39), and young women outnumber men three to one with this diagnosis (39–41), even after taking gynecologic diagnoses into account.
Because of the prevalence of gynecologic pathology in younger women, guidelines for the evaluation of abdominal pain recommend a pelvic exam in nearly all women who present to the ED with acute abdominal symptoms (7, 39, 41–43). In this study, however, only a small number of women received a pelvic examination. It is not clear why so few patients underwent the recommended evaluation, and this may represent a potential area for quality improvement. The ED and discharge diagnoses did not include any gynecological etiologies for the patients’ abdominal pain. Although it is possible that diagnoses designated as “nonspecific” really were gynecologic in origin, further studies are needed to determine if current guidelines could be revised to reflect the likely lower yield of this physical exam component in elderly female patients.
Guidelines for abdominal pain evaluation also often recommend digital rectal exams, while acknowledging that rectal exams may have limited diagnostic utility, particularly for appendicitis (44, 45). Despite the guidelines’ ambivalence about the value of the digital rectal exam, they do advocate testing stool for occult blood in all patients with abdominal pain (7, 39, 41). The rate of rectal exams and fecal occult blood testing in this study was about 50% in both men and women. It is not clear why this recommended evaluation was not performed in more patients, but the clinical practice may reflect the evidence showing low sensitivity and specificity for diagnosing acute abdominal pathology. Further research into the yield of fecal occult blood testing, in particular, in the emergency department evaluation of abdominal pain could help clarify the necessity of the rectal exam.
We are intrigued by our observation of higher mortality among men with abdominal pain. It remains possible that this finding is in part due to chance (and small death rates). It is also possible that we have been unable to adequately account for the influence of acute or chronic disease. Having said this, our mortality findings were present despite the fact that men and women in our cohort had similar predicted mortality according to their Charlson comorbidity scores, a valid measure of prognosis (46). If these findings are confirmed, guidelines for discharge instructions and follow-up care could be adjusted to reflect the greater risk for men presenting with abdominal pain.
This study had several limitations. We may have lacked the power to see small differences between elderly men and women in their evaluation, management, and diagnosis groupings. This seems less likely, however, given the similarity of the findings between men and women in chart-documented characteristics. Our study may have been subject to documentation biases, but it is unlikely that these biases would have disproportionately affected men or women. We did not blind the abstractor to the study hypotheses, nor did we check for interrater reliability. There may have been differences between the two genders in the frequency of particular diagnoses, such as urinary tract infections, but the study was designed to look at overall diagnosis groups and not individual diseases. We do not have information on whether patients were admitted to a different hospital after being discharged. Lastly, the study was conducted at an academic medical center, and the findings in this patient population may not be generalizable to other settings. However, the admission rates, prevalence of nonspecific abdominal pain, and the need for surgical intervention in this study were similar to other published reports and suggest this cohort may be a representative cross-section of elderly abdominal pain patients.
Unlike previous research in younger patients with abdominal pain and among elders with other acute conditions, we found no difference in diagnoses and management between older men and women who presented to the emergency department with abdominal pain. We did observe a higher mortality rate among men within 3 months of their ED visit. Our study requires confirmation in larger settings; future investigation should address the role of the pelvic and rectal exams in elderly patients and identify which factors increase mortality in elderly men.
ACKNOWLEDGMENTS
The authors wish to thank Dr. Otto Liebmann for his insightful review and comments on the manuscript.
Funding: Dr. Auerbach is supported by a K08 research and training grant (K08 HS11416-02) from the Agency for Healthcare Research and Quality, as well as an American Heart Association Grant-in-Aid (#0455008Y).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Rebekah L Gardner, Department of Medicine, University of California San Francisco, San Francisco, California.
Richard Almeida, Department of Emergency Medicine, Highland Hospital, Alameda County Medical Center, Oakland, California.
Judith H Maselli, Department of Medicine, University of California San Francisco, San Francisco, California.
Andrew Auerbach, Department of Medicine, University of California San Francisco, San Francisco, California.
REFERENCES
- 1.McCaig L, Burt C. In: National Hospital Ambulatory Medical Care Survey: 2003 emergency department summary. Hyattsville MD, editor. National Center for Health Statistics; 2005. Report No.: 358. [Google Scholar]
- 2.Bugliosi TF, Meloy TD, Vukov LF. Acute abdominal pain in the elderly. Ann Emerg Med. 1990;19:1383–1386. doi: 10.1016/s0196-0644(05)82602-2. [DOI] [PubMed] [Google Scholar]
- 3.Kizer KW, Vassar MJ. Emergency department diagnosis of abdominal disorders in the elderly. Am J Emerg Med. 1998;16:357–362. doi: 10.1016/s0735-6757(98)90127-9. [DOI] [PubMed] [Google Scholar]
- 4.Lewis LM, Banet GA, Blanda M, et al. Etiology and clinical course of abdominal pain in senior patients: a prospective, multicenter study. J Gerontol A Biol Sci Med Sci. 2005;60:1071–1076. doi: 10.1093/gerona/60.8.1071. [DOI] [PubMed] [Google Scholar]
- 5.van Geloven AA, Biesheuvel TH, Luitse JS, et al. Hospital admissions of patients aged over 80 with acute abdominal complaints. Eur J Surg. 2000;166:866–871. doi: 10.1080/110241500447254. [DOI] [PubMed] [Google Scholar]
- 6.de Dombal FT. Acute abdominal pain in the elderly. J Clin Gastroenterol. 1994;19:331–335. doi: 10.1097/00004836-199412000-00016. [DOI] [PubMed] [Google Scholar]
- 7.American College of Emergency Physicians. Clinical policy: critical issues for the initial evaluation and management of patients presenting with a chief complaint of nontraumatic acute abdominal pain. Ann Emerg Med. 2000;36:406–415. doi: 10.1067/mem.2000.109446. [DOI] [PubMed] [Google Scholar]
- 8.Baum SA, Rubenstein LZ. Old people in the emergency room: age-related differences in emergency department use and care. J Am Geriatr Soc. 1987;35:398–404. doi: 10.1111/j.1532-5415.1987.tb04660.x. [DOI] [PubMed] [Google Scholar]
- 9.Singal BM, Hedges JR, Rousseau EW, et al. Geriatric patient emergency visits. Part I: Comparison of visits by geriatric and younger patients. Ann Emerg Med. 1992;21:802–807. doi: 10.1016/s0196-0644(05)81025-x. [DOI] [PubMed] [Google Scholar]
- 10.McNamara RM, Rousseau E, Sanders AB. Geriatric emergency medicine: a survey of practicing emergency physicians. Ann Emerg Med. 1992;21:796–801. doi: 10.1016/s0196-0644(05)81024-8. [DOI] [PubMed] [Google Scholar]
- 11.Vaccarino V, Rathore SS, Wenger NK, et al. Sex and racial differences in the management of acute myocardial infarction, 1994 through 2002. N Engl J Med. 2005;353:671–682. doi: 10.1056/NEJMsa032214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Schulman KA, Berlin JA, Harless W, et al. The effect of race and sex on physicians' recommendations for cardiac catheterization. N Engl J Med. 1999;340:618–626. doi: 10.1056/NEJM199902253400806. [DOI] [PubMed] [Google Scholar]
- 13.Blomkalns AL, Chen AY, Hochman JS, et al. Gender disparities in the diagnosis and treatment of non-ST-segment elevation acute coronary syndromes: large-scale observations from the CRUSADE (Can Rapid Risk Stratification of Unstable Angina Patients Suppress Adverse Outcomes With Early Implementation of the American College of Cardiology/American Heart Association Guidelines) National Quality Improvement Initiative. J Am Coll Cardiol. 2005;45:832–837. doi: 10.1016/j.jacc.2004.11.055. [DOI] [PubMed] [Google Scholar]
- 14.Rathore SS, Berger AK, Weinfurt KP, et al. Race, sex, poverty, and the medical treatment of acute myocardial infarction in the elderly. Circulation. 2000;102:642–648. doi: 10.1161/01.cir.102.6.642. [DOI] [PubMed] [Google Scholar]
- 15.McLaughlin TJ, Soumerai SB, Willison DJ, et al. Adherence to national guidelines for drug treatment of suspected acute myocardial infarction: evidence for undertreatment in women and the elderly. Arch Intern Med. 1996;156:799–805. [PubMed] [Google Scholar]
- 16.Di Carlo A, Lamassa M, Baldereschi M, et al. Sex differences in the clinical presentation, resource use, and 3-month outcome of acute stroke in Europe: data from a multicenter multinational hospital-based registry. Stroke. 2003;34:1114–1119. doi: 10.1161/01.STR.0000068410.07397.D7. [DOI] [PubMed] [Google Scholar]
- 17.Glader EL, Stegmayr B, Norrving B, et al. Sex differences in management and outcome after stroke: a Swedish national perspective. Stroke. 2003;34:1970–1975. doi: 10.1161/01.STR.0000083534.81284.C5. [DOI] [PubMed] [Google Scholar]
- 18.Holroyd-Leduc JM, Kapral MK, Austin PC, et al. Sex differences and similarities in the management and outcome of stroke patients. Stroke. 2000;31:1833–1837. doi: 10.1161/01.str.31.8.1833. [DOI] [PubMed] [Google Scholar]
- 19.Simpson CR, Wilson C, Hannaford PC, et al. Evidence for age and sex differences in the secondary prevention of stroke in Scottish primary care. Stroke. 2005;36:1771–1775. doi: 10.1161/01.STR.0000173398.99163.9e. [DOI] [PubMed] [Google Scholar]
- 20.Becker RC, Terrin M, Ross R, et al. Comparison of clinical outcomes for women and men after acute myocardial infarction. The Thrombolysis in Myocardial Infarction Investigators. Ann Intern Med. 1994;120:638–645. doi: 10.7326/0003-4819-120-8-199404150-00003. [DOI] [PubMed] [Google Scholar]
- 21.Earle CC, Venditti LN, Neumann PJ, et al. Who gets chemotherapy for metastatic lung cancer? Chest. 2000;117:1239–1246. doi: 10.1378/chest.117.5.1239. [DOI] [PubMed] [Google Scholar]
- 22.Hawker GA, Wright JG, Coyte PC, et al. Differences between men and women in the rate of use of hip and knee arthroplasty. N Engl J Med. 2000;342:1016–1022. doi: 10.1056/NEJM200004063421405. [DOI] [PubMed] [Google Scholar]
- 23.Covinsky KE, Palmer RM, Fortinsky RH, et al. Loss of independence in activities of daily living in older adults hospitalized with medical illnesses: increased vulnerability with age. J Am Geriatr Soc. 2003;51:451–458. doi: 10.1046/j.1532-5415.2003.51152.x. [DOI] [PubMed] [Google Scholar]
- 24.Dukas L, Staehelin HB, Schacht E, et al. Better functional mobility in community-dwelling elderly is related to D-hormone serum levels and to daily calcium intake. J Nutr Health Aging. 2005;9:347–351. [PubMed] [Google Scholar]
- 25.Fortinsky RH, Covinsky KE, Palmer RM, et al. Effects of functional status changes before and during hospitalization on nursing home admission of older adults. J Gerontol A Biol Sci Med Sci. 1999;54:M521–M526. doi: 10.1093/gerona/54.10.m521. [DOI] [PubMed] [Google Scholar]
- 26.Fenyo G. Acute abdominal disease in the elderly: experience from two series in Stockholm. Am J Surg. 1982;143:751–754. doi: 10.1016/0002-9610(82)90052-6. [DOI] [PubMed] [Google Scholar]
- 27.Social Security Death Index. [Accessed March 25, 2006]; www.ancestry.com. [Google Scholar]
- 28.Chang HJ, Mehta PS, Rosenberg A, et al. Concerns of patients actively contemplating total knee replacement: differences by race and gender. Arthritis Rheum. 2004;51:117–123. doi: 10.1002/art.20073. [DOI] [PubMed] [Google Scholar]
- 29.Karlson EW, Daltroy LH, Liang MH, et al. Gender differences in patient preferences may underlie differential utilization of elective surgery. Am J Med. 1997;102:524–530. doi: 10.1016/s0002-9343(97)00050-8. [DOI] [PubMed] [Google Scholar]
- 30.O'Connor GT, Morton JR, Diehl MJ, et al. Differences between men and women in hospital mortality associated with coronary artery bypass graft surgery. The Northern New England Cardiovascular Disease Study Group. Circulation. 1993;88:2104–2110. doi: 10.1161/01.cir.88.5.2104. [DOI] [PubMed] [Google Scholar]
- 31.Walter LC, de Garmo P, Covinsky KE. Association of older age and female sex with inadequate reach of screening flexible sigmoidoscopy. Am J Med. 2004;116:174–178. doi: 10.1016/j.amjmed.2003.09.030. [DOI] [PubMed] [Google Scholar]
- 32.Giacomini MK. Gender and ethnic differences in hospital-based procedure utilization in California. Arch Intern Med. 1996;156:1217–1224. [PubMed] [Google Scholar]
- 33.Rathore SS, Wang Y, Radford MJ, et al. Sex differences in cardiac catheterization after acute myocardial infarction: the role of procedure appropriateness. Ann Intern Med. 2002;137:487–493. doi: 10.7326/0003-4819-137-6-200209170-00008. [DOI] [PubMed] [Google Scholar]
- 34.Cooper GS, Yuan Z, Rosenthal GE, et al. Lack of gender and racial differences in surgery and mortality in hospitalized Medicare beneficiaries with bleeding peptic ulcer. J Gen Intern Med. 1997;12:485–490. doi: 10.1046/j.1525-1497.1997.00087.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Bell MR, Berger PB, Holmes DR, Jr, et al. Referral for coronary artery revascularization procedures after diagnostic coronary angiography: evidence for gender bias? J Am Coll Cardiol. 1995;25:1650–1655. doi: 10.1016/0735-1097(95)00044-5. [DOI] [PubMed] [Google Scholar]
- 36.Epstein SK, Vuong V. Lack of influence of gender on outcomes of mechanically ventilated medical ICU patients. Chest. 1999;116:732–739. doi: 10.1378/chest.116.3.732. [DOI] [PubMed] [Google Scholar]
- 37.Cydulka RK, Rowe BH, Clark S, et al. Gender differences in emergency department patients with chronic obstructive pulmonary disease exacerbation. Acad Emerg Med. 2005;12:1173–1179. doi: 10.1197/j.aem.2005.06.025. [DOI] [PubMed] [Google Scholar]
- 38.Walker JW. Abdominal and pelvic pain. Emerg Med Clin North Am. 1987;5:425–428. [PubMed] [Google Scholar]
- 39.Kamin RA, Nowicki TA, Courtney DS, et al. Pearls and pitfalls in the emergency department evaluation of abdominal pain. Emerg Med Clin North Am. 2003;21:61–72. doi: 10.1016/s0733-8627(02)00080-9. vi. [DOI] [PubMed] [Google Scholar]
- 40.Lukens TW, Emerman C, Effron D. The natural history and clinical findings in undifferentiated abdominal pain. Ann Emerg Med. 1993;22:690–696. doi: 10.1016/s0196-0644(05)81849-9. [DOI] [PubMed] [Google Scholar]
- 41.King KE, Wightman JM. Abdominal Pain. In: MJ A, editor. Rosen's Emergency Medicine: Concepts and Clinical Practice. St. Louis: Mosby, Inc.; 2002. pp. 190–193. [Google Scholar]
- 42.Newton E, Mandavia S. Surgical complications of selected gastrointestinal emergencies: pitfalls in management of the acute abdomen. Emerg Med Clin North Am. 2003;21:873–907. doi: 10.1016/s0733-8627(03)00087-7. viii. [DOI] [PubMed] [Google Scholar]
- 43.Sanson TG, O'Keefe KP. Evaluation of abdominal pain in the elderly. Emerg Med Clin North Am. 1996;14:615–627. doi: 10.1016/s0733-8627(05)70270-4. [DOI] [PubMed] [Google Scholar]
- 44.Dixon JM, Elton RA, Rainey JB, et al. Rectal examination in patients with pain in the right lower quadrant of the abdomen. Bmj. 1991;302:386–388. doi: 10.1136/bmj.302.6773.386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Muris JW, Starmans R, Wolfs GG, et al. The diagnostic value of rectal examination. Fam Pract. 1993;10:34–37. doi: 10.1093/fampra/10.1.34. [DOI] [PubMed] [Google Scholar]
- 46.Charlson ME, Pompei P, Ales KL, et al. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40:373–383. doi: 10.1016/0021-9681(87)90171-8. [DOI] [PubMed] [Google Scholar]