Abstract
Employing a precise and sensitive double-isotope derivative technique, plasma catecholamine concentration (PCA) was measured in four groups of subjects: (a) long-term diabetics with neuropathy, (b) long-term diabetics without neuropathy, (c) hypophysectomized long-term diabetics with neuropathy, and (d) nondiabetic control subjects. Blood samples were obtained from subjects in the supine and in the standing position.
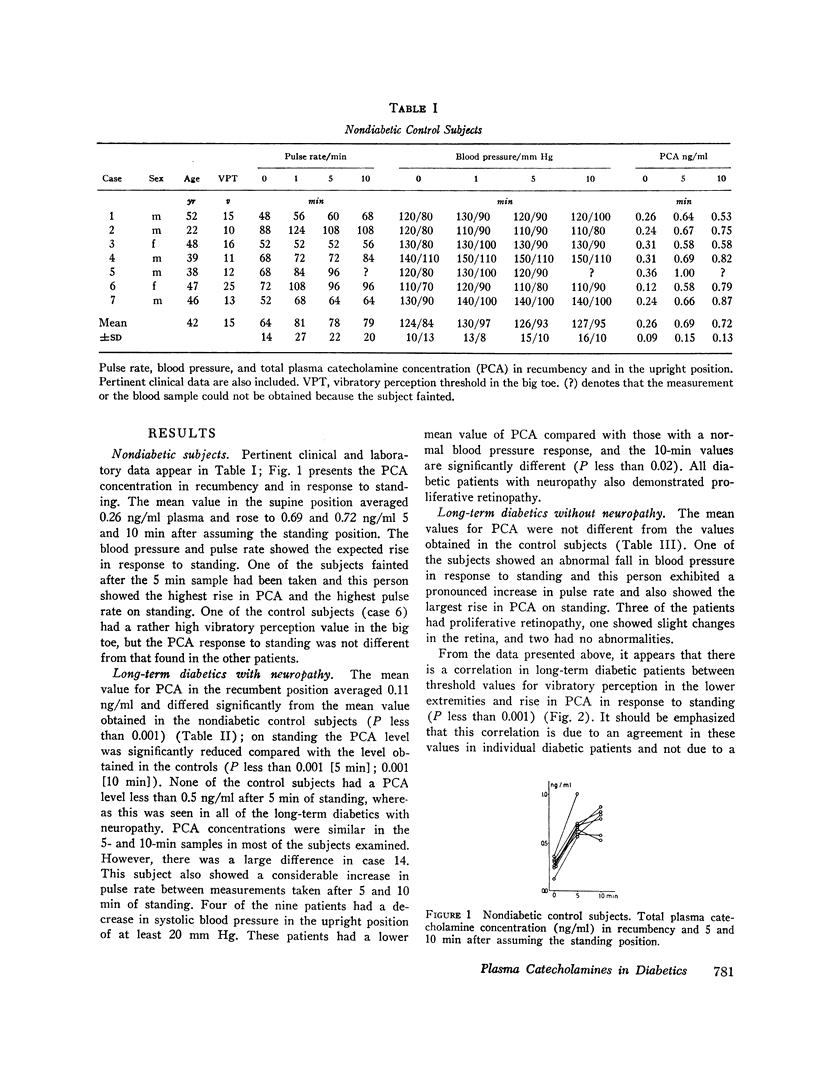
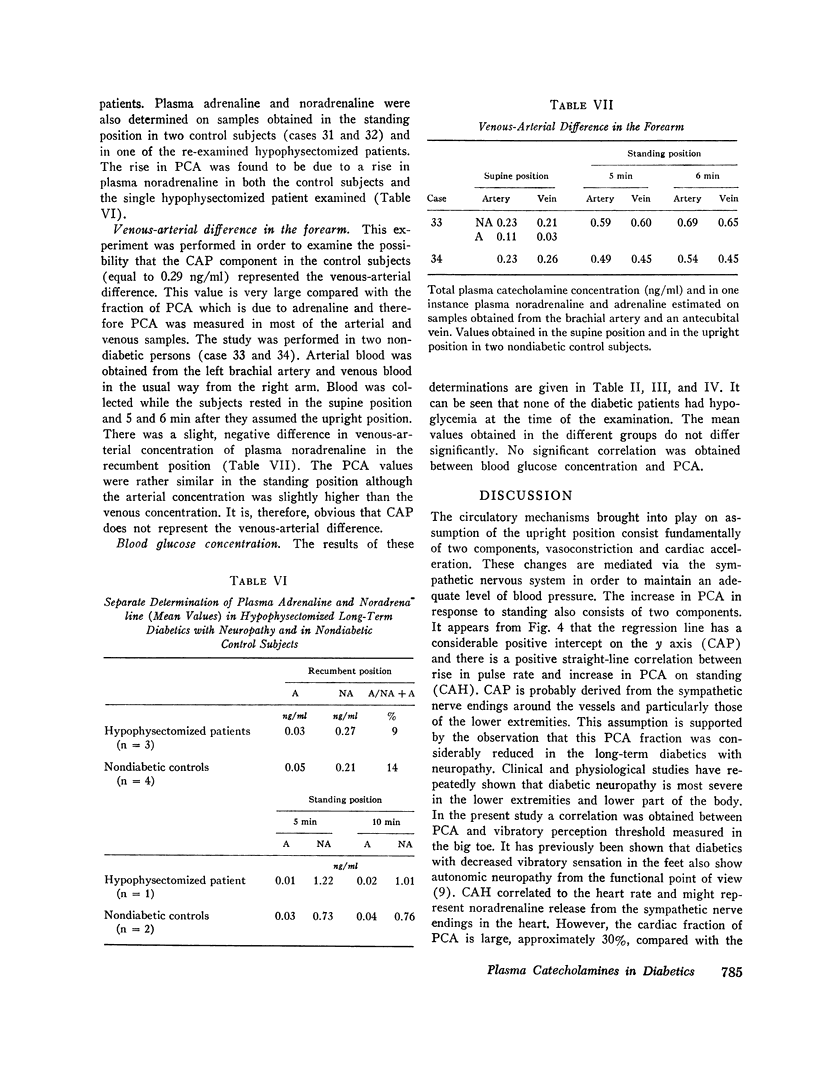
In nondiabetic control subjects, PCA (mainly noradrenaline) increased from 0.26 ng/ml in the supine positon to 0.69 and 0.72 ng/ml 5 and 10 min after assuming the standing position. By plotting this increase in PCA on the y axis in a coordinate system vs. increase in pulse rate, PCA was divided into two components: one of these depended on the rise in pulse rate on standing (called CAH) and the other corresponded to the intercept on the y axis where rise in pulse rate equals zero (CAP).
Long-term diabetics with neuropathy showed a significant reduction in PCA in both the supine and the standing position. Further analysis demonstrated that CAP was considerably reduced whereas CAH was normal. Long-term diabetics without neuropahty showed normal PCA values.
Surprisingly, hypophysectomized diabetics with neuropathy exhibited mean PCA values in both the supine and the standing position which were similar to those found in the nondiabetic subjects and considerably elevated compared with the findings in the nonoperated, long-term diabetics with neuropathy. Further analysis in terms of CAP and CAH demonstrated, however, that CAP was just as abnormally reduced in the hypophysectomized as it was in the nonoperated patients whereas CAH was considerably increased.
In contrast to the findings in the nonoperated diabetics with neuropathy, the hypophysectomized diabetic patients with neuropathy demonstrated a negative correlation between rise in PCA and blood pressure on standing indicating that the increase in PCA was at least partially a compensatory phenomenon in the interest of the maintenance of a normal level of blood pressure.
An increased sympathetic tone (vasoconstriction) is believed to be at least partially responsible for the increased capillary resistance and decreased capillary permeability occuring after hypophysectomy.
Full text
PDF






Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Christensen N. J. Increased skin capillary resistance after hypophysectomy in long-term diabetics. Lancet. 1968 Dec 14;2(7581):1270–1271. doi: 10.1016/s0140-6736(68)91762-5. [DOI] [PubMed] [Google Scholar]
- Christensen N. J. Muscle blood flow, measured by and vascular calcifications in diabetics. Acta Med Scand. 1968 May;183(5):449–454. doi: 10.1111/j.0954-6820.1968.tb10506.x. [DOI] [PubMed] [Google Scholar]
- Christensen N. J. Notes on the glucose oxidase method. Scand J Clin Lab Invest. 1967;19(4):379–384. doi: 10.3109/00365516709090653. [DOI] [PubMed] [Google Scholar]
- Christensen N. J. Spontaneous variations in resting blood flow, postischaemic peak flow and vibratory perception in the feet of diabetics. Diabetologia. 1969 Jun;5(3):171–178. doi: 10.1007/BF01213675. [DOI] [PubMed] [Google Scholar]
- Christensen N. J., Terkildsen A. B. Quantitative measurements of skin capillary resistance in hypophysectomized long-term diabetics. Diabetes. 1971 May;20(5):297–301. doi: 10.2337/diab.20.5.297. [DOI] [PubMed] [Google Scholar]
- Engelman K., Portnoy B. A sensitive double-isotope derivative assay for norepinephrine and epinephrine. Normal resting human plasma levels. Circ Res. 1970 Jan;26(1):53–57. doi: 10.1161/01.res.26.1.53. [DOI] [PubMed] [Google Scholar]
- Isaacs M., Pazianos A. G., Greenberg E., Koven B. J. Renal function after pituitary ablation for diabetic retinopathy. JAMA. 1969 Mar 31;207(13):2406–2410. [PubMed] [Google Scholar]
- Landsberg L., Axelrod J. Influence of pituitary, thyroid, and adrenal hormones on norepinephrine turnover and metabolism in the rat heart. Circ Res. 1968 May;22(5):559–571. doi: 10.1161/01.res.22.5.559. [DOI] [PubMed] [Google Scholar]
- Mellander S., Johansson B. Control of resistance, exchange, and capacitance functions in the peripheral circulation. Pharmacol Rev. 1968 Sep;20(3):117–196. [PubMed] [Google Scholar]



