Abstract
Objectives. SSc-associated gastrointestinal tract involvement (SSc-GIT) is an important predictor of depressive symptoms. University of California at Los Angeles Scleroderma Clinical trial Consortium Gastrointestinal Tract 2.0 (UCLA SCTC GIT 2.0) is a 34-item valid instrument that captures GIT symptom severity and impact on quality of life. It has seven GI-specific scales and a total GIT score. The objectives were to assess: (i) whether there is an association between depressed mood with GI symptom scales as assessed by the UCLA SCTC GIT 2.0 instrument; and (ii) to explore which GI-specific symptom scales are associated with depressed mood in patients with SSc.
Methods. One hundred and fifty-two patients with SSc completed the UCLA SCTC GIT 2.0 and the Center for Epidemiologic Studies Short Depression scale (CES-D10). Patients were divided into depressed (CES-D ≥ 10) or non-depressed group (CES-D < 10) and compared using t-test or chi-square test. Multiple linear regression was used to determine associations between GI scales and depressed mood (CES-D).
Results. Study participants were 84% female, 78% Caucasian and 40% had depressed mood (CES-D10 ≥ 10). Patients with depressed mood had statistically worse GI scale scores (except fecal soilage) and worse total GIT score (P < 0.05). In the multivariable model reflux and constipation scales were independently associated with worse CES-D scores (P = 0.01–0.06)
Conclusion. SSc-GIT involvement is associated with depressed mood. Reflux and constipation scales of UCLA-SCTC GIT 2.0 were independently associated with CES-D. Future studies should assess if treatment of GIT symptoms will improve depressed mood in patients with SSc-GIT.
Keywords: Scleroderma, Systemic sclerosis, Depression, Center for Epidemiologic Studies Short Depression scale, Gastrointestinal involvement, Reflux, Constipation, University of California at Los Angeles Scleroderma Clinical trial Consortium Gastrointestinal Tract 2.0
Introduction
SSc is a rare, chronic, autoimmune disorder associated with gastrointestinal tract (GIT) involvement [1, 2] and depressed mood [3]. GIT affects ∼90% of patients with SSc [2]. Recent studies have shown that the prevalence of clinically significant depressive symptoms in SSc ranges from 36 to 65% [4] and GIT involvement is an important predictor of depressive symptoms [1, 5].
We have recently developed a validated patient-reported outcome measure to assess health-related quality of life (HRQOL) and GIT severity in SSc—the University of California at Los Angeles Scleroderma Clinical Trial Consortium GIT 2.0 instrument (UCLA SCTC GIT 2.0; available free at http://uclascleroderma.researchcore.org/) [6]. This instrument is feasible, reliable and valid and has seven scales— reflux, distension/bloating, diarrhoea, fecal soilage, constipation, emotional well-being and social functioning.
The objectives of this study were: (i) to assess whether there is an association between depressed mood with GI symptoms as assessed by the UCLA SCTC GIT 2.0 instrument; and (ii) to explore which GI-specific symptom scales are associated with depressed mood in patients with SSc.
Patients and methods
Patient sample
One hundred and fifty-two patients with SSc participated in this cross-sectional study at the following three Scleroderma centres in the USA: UCLA, Los Angeles, CA, USA; University of Texas Houston Medical School, Houston, TX, USA; and University of Michigan, Ann Arbor, MI, USA, to develop the UCLA SCTC GIT 2.0 [6]. The study was approved by local institutional review boards (IRBs of UCLA, University of Texas at Houston and University of Michigan) and all patients signed a written informed consent form. Patients underwent clinical history and physical examination, provided sociodemographic information (age, sex, ethnicity and level of education) and completed the short form-36 (SF-36) version 2 [6]. In addition, we asked a single-item question on global self-rated GIT severity [‘In the past week, how severe were your gastrointestinal (gut, GI) symptoms overall?’ Answers were given as none, very mild, moderate, severe and very severe]. Physician physical exams were used to determine the type of SSc (limited SSc, diffuse SSc or overlap syndrome) and GIT diagnoses.
HRQOL instrument
UCLA SCTC GIT 2.0 is a validated, patient-reported outcome measure to assess HRQOL and GIT severity in SSc [6, 7]. This 34-item instrument has seven scales: reflux, distention/bloating, diarrhoea, fecal soilage, constipation, emotional well-being and social functioning and a total GI score. All scales are scored from 0 (better HRQOL) to 3 (worse HRQOL) except diarrhoea and constipation scales, which range from 0 to 2 and 0 to 2.5, respectively. The total GI score is the average of six of seven scales (excludes constipation) and total GI score are scored from 0 (better HRQOL) to 3 (worse HRQOL). This instrument was found to be feasible, reliable and valid in an observational study [6].
Center for Epidemiologic Studies Short Depression scale
Depressive symptoms were measured by the Center for Epidemiologic Studies Short Depression scale (CES-D10), a 10-item instrument that assesses depressive symptoms [8]. The occurrence of each depressive symptom during the past week is rated on a scale of 0–3 (‘Rarely or none of the time’ to ‘All of the time’), and total scores range from 0 to 30. A score of ≥10 indicates depressed mood [8].
Statistical analysis
Descriptive statistics and differences for demographic variables, type of SSc, UCLA SCTC GIT 2.0 scales and SF-36 physical and mental component scores between the depressed (CES-D ≥ 10) and the non-depressed groups (CES-D < 10) were assessed using Student’s t-test for normally distributed variables and Wilcoxon rank sum test for non-normally distributed variables. The distribution was assessed using Shapiro–Wilk test.
A multiple linear regression model was developed to determine the association between GI scales and CES-D (the outcome variable). CES-D was modelled as a log-transformed continuous variable (since CES-D was not normally distributed). Other covariates included age, gender, race (White, Black and other ethnicity), type of SSc (limited SSc, diffuse SSc and overlap syndrome), marital status (high-school graduate or less, some college/college graduate or post-graduate training) and UCLA SCTC GI 2.0 scales (reflux, distention/bloating, diarrhoea, fecal soilage, constipation and social functioning). Emotional well-being scale was not included among the covariates since it theoretically measures the same construct as CES-D.
For the CES-D model, variables that had non-significant t-statistics were dropped, based on the Wald test [9]. For the CES-D model, age, gender, race, marital status and type of SSc had no significant associations with outcome variables (P < 0.05). Therefore, these non-significant variables were dropped from final model. Covariates that remained in the model included reflux, indigestion, diarrhoea, soil and social functioning scale scores. Statistical analysis was performed using Stata 10.1 (College Station, TX) and P ≤ 0.05 was indicative of statistical significance.
Results
The details of the patient population have been published elsewhere [6]. Of the 152 patients in the study, the majority of participants were female (84%) and Caucasian (78%); 54% had diffuse SSc and 40% had depressed mood (CES-D ≥ 10; Table 1). Self-rated severity of GIT ranged from no symptoms/very mild (39%), to mild (21%), to moderate (31%), to severe/very severe (9%). SF-36 physical component summary (PCS) scores were 1.3 s.d. below US general population, whereas SF-36 mental component summary (MCS) scores were 0.3s.d. below US general population. The majority of patients had a diagnosis of gastroesophageal reflux disease (GERD) (91%), followed by small intestinal bacterial overgrowth, gastroparesis and diarrhoea (11% each) [6]. There were no differences in the demographics and GI medications in patients with and without depressed mood (Table 1).
Table 1.
Baseline characteristics of the patients
| Variables | All patients (n = 152) | CES-D score <10 (n = 91) | CES-D score ≥10 | P-value* |
|---|---|---|---|---|
| (n = 61) | ||||
| Age, mean (s.d.), years | 50.8 (12.3) | 51.07 (12.01) | 50.52 (12.98) | 0.79 |
| Gender: female, n (%) | 128 (84.1) | 77 (84.6) | 51 (83.6) | 0.87 |
| Race, n (%) | 0.85 | |||
| Caucasian | 118 (81.4) | 71 (79.78) | 48 (85.71) | |
| African-American | 11 (7.6) | 8 (8.99) | 2 (3.57) | |
| Asian | 9 (6.2) | 6 (6.74) | 3 (5.36) | |
| Others | 7 (4.8) | 4 (4.49) | 3 (5.37) | |
| Disease duration, mean (s.d.), years | 6.9 (7.2) | 7.5 (7.9) | 6.1 (6.1) | 0.34 |
| Type of SSc, n (%) | 0.31 | |||
| Diffuse | 81 (55.3) | 46 (50.55) | 37 (60.66) | – |
| Limited | 62 (40.7) | 41 (45.05) | 21 (34.43) | – |
| Overlap syndrome | 6 (4.0) | 4 (4.40) | 3 (4.92) | – |
| CES-D, mean (s.d.) | 9.27 (6.77) | 4.73 (2.42) | 16.05 (5.33) | – |
| GI medications | ||||
| Proton-pump inhibitors | 116 (76.8) | 71 (78.0) | 45 (75.0) | 0.697 |
| H-2 blockers | 18 (11.9) | 12 (13.2) | 6 (10.0) | 0.617 |
| Promotility drugs | 24 (15.9) | 13 (14.3) | 11 (18.3) | 0.505 |
| Chronic antibiotic therapy | 10 (6.6) | 3 (3.3) | 7 (11.7) | 0.052 |
| Laxatives | 2 (1.3) | 0 (0.0) | 2 (3.3) | 0.156 |
| Anti-diarrhoeal agents | 3 (2.0) | 1 (1.1) | 2 (3.3) | 0.563 |
| Others | 14 (9.3) | 5 (5.5) | 9 (15.0) | 0.082 |
| UCLA SCTC GIT 2.0, mean (s.d.) | ||||
| Reflux | 0.69 (0.54) | 0.58 (0.47) | 0.86 (0.59) | 0.002 |
| Distension/bloating | 1.07 (0.82) | 0.92 (0.78) | 1.28 (0.81) | 0.006 |
| Constipation | 0.43 (0.49) | 0.36 (0.49) | 0.55 (0.50) | 0.003 |
| Diarrhoea | 0.47 (0.56) | 0.38 (0.49) | 0.61 (0.63) | 0.02 |
| Fecal soilage | 0.29 (0.67) | 0.22 (0.49) | 0.41 (0.86) | 0.4 |
| Emotional well-being | 0.49 (0.65) | 0.30 (0.48) | 0.78 (0.77) | <0.0001 |
| Social functioning | 0.26 (0.51) | 0.15 (0.39) | 0.43 (0.63) | 0.0002 |
| Total GIT score | 0.65 (0.46) | 0.53 (0.38) | 0.84 (0.51) | 0.0001 |
| SF-36 PCS | 36.7 (9.3) | 39.17 (8.66) | 33.48 (8.97) | 0.0002 |
| SF-36 MCS | 47.1 (12.5) | 53.51 (9.00) | 37.65 (10.89) | <0.0001 |
| Self-rated GI severity, n (%) | 0.04 | |||
| No symptoms | 29 (19.2) | 20 (20.2) | 9 (14.7) | – |
| Very mild | 30 (19.7) | 21 (23.3) | 9 (14.7) | – |
| Mild | 33 (21.7) | 17 (18.9) | 15 (24.6) | – |
| Moderate | 47 (30.9) | 29 (32.2) | 18 (29.5) | – |
| Severe/very severe | 13 (8.0) | 3 (3.33) | 10 (16.4) | – |
| GIT hospitalization, n (%) | ||||
| Yes | 34 (22.7) | 19 (21.1) | 15 (25.0) | 0.58 |
*P-value: comparison between depressed (CES-D score ≥10) and non-depressed (CES-D score <10) patients.
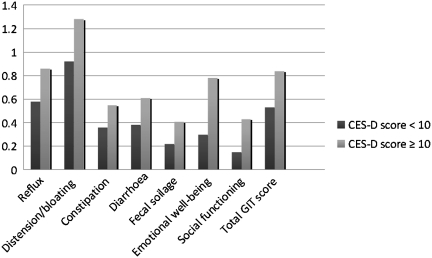
In the univariate comparisons, patients with depressed mood (CES-D ≥ 10) had statistically higher (worse) GI scale scores (except for fecal soilage), total GIT score and lower SF-36 PCS and MCS scores (Table 1 and Fig. 1). GI severity was defined by self-reported severity and hospitalizations due to GI illness. Patients who were depressed rated their GI disease as significantly more severe compared with those without depressed mood (Table 1). There was no difference in hospitalizations due to GI illness (Table 1).
Fig. 1.
UCLA SCTC GIT 2.0 scale scores in patients with and without depressed mood.
In the multivariable model, the constipation (β = 0.31, P = 0.013) and reflux scales (β = 0.23, P = 0.057) had positive association with CES-D (R2 = 0.1935, P ≤ 0.0001); patients with greater scores in reflux and constipation scales had worse depressed mood. After controlling for covariates, an increase of 1 U in constipation/reflux scale scores resulted in a 36.5/25.9% increase in CES-D.
Discussion
GI involvement is associated with depressed mood in patients with SSc [1, 5]. Our study demonstrates a positive association between GI involvement and depressive symptoms; patients with depressed mood had worse scores on self-reported GI symptoms. In addition, the reflux and constipation scales of the UCLA SCTC GIT 2.0 were independently associated with depressed mood.
Previous studies have shown a positive association between depressed mood and GI involvement in patients with SSc. In a cross-sectional study of 72 patients in a university setting, Nietert et al. [1] showed a significant association between worse upper GI involvement and depressed mood (assessed using CES-D scores). However, their GI instrument did not differentiate reflux from distension/bloating scales. In another cross-sectional study with 376 patients with SSc in a community setting, Thombs et al. [5] reported that patients with greater GI symptoms had significantly higher total CES-D scores (more depressed). Our results corroborate these studies in showing a strong association between GI involvement and depressive symptoms in patients with SSc.
We found independent associations of reflux and constipation symptoms with depressive mood, controlling for covariates including other UCLA SCTC GIT 2.0 scales. An association between reflux symptoms and depressed mood in the general population was previously shown by Jansson et al. [10] in a large population-based cross-sectional case–control study consisting of 65 333 participants. In another prospective observational cohort study (n = 6215), GERD patients had lower HRQOL (as assessed by SF-36 and a disease-specific GI instrument) compared with the general population, and was similar to that in patients after acute coronary events [8]. Literature on constipation and depression is sparse but one study in patients with irritable bowel syndrome found that patients with constipation subtype had greater psychological distress compared with diarrhoea subtype [11].
Based on our and other studies [1, 5], reflux symptoms should be recognized and aggressively treated. Large studies in the general population have shown that treatment of GERD significantly improves HRQOL [8]. As an example, in a large cohort study of 6215 patients with reflux disease who were treated with esomeprazole for 2 weeks, there was a clinically meaningful improvement in the SF-36 PCS (improved from 43 to 49) and SF-36 MCS (improved from 45 to 50) [8].
Our study has noteworthy strengths. It included a large number of patients with SSc prospectively recruited to develop UCLA SCTC GIT 2.0. In addition, this is the first study to assess the associations of GI-specific symptom scales with depressed mood.
The study is not without limitations. It employed a cross-sectional design and, therefore, causal inferences cannot be made. It is plausible that presence of depressed mood may lead to greater GI symptoms or presence of GI symptoms may lead to depressed mood. In our current study, we developed multivariable regression model with CES-D as an outcome measure based on prior research showing that GIT involvement is a predictor of depressed mood [1, 5]. Since both GI involvement and depressed mood are very common in SSc, future longitudinal studies should assess the direction of relationship and if treatment of one or both lead to better patient outcomes. We recommend aggressive screening for depressed mood and GI involvement in clinical practice. Secondly, as in previous studies, depressed mood was based on self-report questionnaires, rather than a standard clinical interview by a trained psychologist. Thirdly, we did not capture the specific treatments for the depressed mood.
In conclusion, we show that the GI involvement in SSc is associated with depressed mood. Future research should assess causal relationship between GI involvement and depressed mood. It remains to be seen if treatment of reflux and constipation will improve depressive symptoms in patients with SSc.
Acknowledgements
Funding: Development of UCLA SCTC GIT 2.0 was funded by Scleroderma Clinical Trial Consortium. D.E.F. and D.K. were also supported by U01 National Institutes of Health/National Institute of Arthritis, Musculoskeletal, and Skin Diseases (NIH/NIAMS) AR055057.
Disclosure statement: M.D.M. serves on the Speaker’s Bureau for Actelion, Gilead and United Therapeutics; has received research grants from Actelion, United Therapeutics and MedImmune; and has received honoraria from Actelion, Gilead and United Therapeutics. D.K. was supported by a National Institutes of Health Award (NIAMS K23 AR053858-04). D.E.F. has received grants and been on advisory boards for Actelion and Gilead. All other authors have declared no conflicts of interest.
References
- 1.Nietert PJ, Mitchell HC, Bolster MB, Curran MY, Tilley BC, Silver RM. Correlates of depression, including overall and gastrointestinal functional status, among patients with systemic sclerosis. J Rheumatol. 2005;32:51–7. [PubMed] [Google Scholar]
- 2.Khanna D. Gastrointestinal involvement in systemic sclerosis. In: Font J, Ramos-Casals M, Rodes J, editors. Digestive involvement in systemic autoimmune diseases. Vol. 8. New York: Elsevier; 2008. pp. 51–61. [Google Scholar]
- 3.Thombs BD, Taillefer SS, Hudson M, Baron M. Depression in patients with systemic sclerosis: a systematic review of the evidence. Arthritis Rheum. 2007;57:1089–97. doi: 10.1002/art.22910. [DOI] [PubMed] [Google Scholar]
- 4.Khanna D, Ahmed M, Furst DE, et al. Health values of patients with systemic sclerosis. Arthritis Rheum. 2007;57:86–93. doi: 10.1002/art.22465. [DOI] [PubMed] [Google Scholar]
- 5.Thombs BD, Hudson M, Taillefer SS, Baron M. Prevalence and clinical correlates of symptoms of depression in patients with systemic sclerosis. Arthritis Rheum. 2008;59:504–9. doi: 10.1002/art.23524. [DOI] [PubMed] [Google Scholar]
- 6.Khanna D, Hays RD, Maranian P, et al. Reliability and validity of the University of California, Los Angeles Scleroderma Clinical Trial Consortium Gastrointestinal Tract Instrument. Arthritis Rheum. 2009;61:1257–63. doi: 10.1002/art.24730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Khanna D, Hays RD, Park GS, et al. Development of a preliminary scleroderma gastrointestinal tract 1.0 quality of life instrument. Arthritis Rheum. 2007;57:1280–6. doi: 10.1002/art.22987. [DOI] [PubMed] [Google Scholar]
- 8.Kulig M, Leodolter A, Vieth M, et al. Quality of life in relation to symptoms in patients with gastro-oesophageal reflux disease–an analysis based on the ProGERD initiative. Aliment Pharmacol Ther. 2003;18:767–76. doi: 10.1046/j.1365-2036.2003.01770.x. [DOI] [PubMed] [Google Scholar]
- 9.Kutner M, Nachtsheim C, Neter J, Li W. New York: McGraw-Hill; 2004. Applied linear statistical models, 5th edition. chap 7.3. [Google Scholar]
- 10.Jansson C, Nordenstedt H, Wallander MA, et al. Severe gastro-oesophageal reflux symptoms in relation to anxiety, depression and coping in a population-based study. Aliment Pharmacol Ther. 2007;26:683–91. doi: 10.1111/j.1365-2036.2007.03411.x. [DOI] [PubMed] [Google Scholar]
- 11.Muscatello MR, Bruno A, Pandolfo G, et al. Depression, anxiety and anger in subtypes of irritable bowel syndrome patients. J Clin Psychol Med Settings. 2010;17:64–70. doi: 10.1007/s10880-009-9182-7. [DOI] [PubMed] [Google Scholar]