Abstract
Introduction
Multiple factors influence the viability of aerosolized bacteria. The delivery of aerosols is affected by chamber conditions (humidity, temperature, and pressure) and bioaerosol characteristics (particle number, particle size distribution, and viable aerosol concentration). Measurement of viable aerosol concentration and particle size is essential to optimize viability and lung delivery. The Madison chamber is widely used to expose small animals to infectious aerosols.
Methods
A multiplex sampling port was added to the Madison chamber to measure the chamber conditions and bioaerosol characteristics. Aerosols of three pathogens (Bacillus anthracis, Yersinia pestis, and Mycobacterium tuberculosis) were generated under constant conditions and their bioaerosol characteristics were analyzed. Airborne microbes were captured using an impinger or BioSampler. The particle size distribution of airborne microbes was determined using an aerodynamic particle sizer (APS). Viable aerosol concentration, spray factor (viable aerosol concentration/inoculum concentration), and dose presented to the mouse were calculated. Dose retention efficiency and viable aerosol retention rate were calculated from the sampler titers to determine the efficiency of microbe retention in lungs of mice.
Results
B. anthracis, Y. pestis, and M. tuberculosis aerosols were sampled through the port. The count mean aerodynamic sizes were 0.98, 0.77, and 0.78 μm with geometric standard deviations of 1.60, 1.90, and 2.37, and viable aerosol concentrations in the chamber were 211, 57, and 1 colony-forming unit (CFU)/mL, respectively. Based on the aerosol concentrations, the doses presented to mice for the three pathogens were 2.5e5, 2.2e4 and 464 CFU.
Discussion
Using the multiplex sampling port we determined whether the animals were challenged with an optimum bioaerosol based on dose presented and respirable particle size.
Keywords: Animal models, Bacillus anthracis, Bioaerosol, Diameter, Dosimetry, Inhalation, Methods, Mycobacterium tuberculosis, Sampling, Yersinia pestis
1. Introduction
The Madison Aerosol Chamber (College of Engineering Shop, University of Wisconsin) is currently used for whole body aerosol exposures at various biocontainment laboratories throughout the country (Basaraba et al. 2006, Agar et al. 2008). The chamber is large enough to expose 180 mice, 18 guinea pigs, or 6 rabbits simultaneously. Priority pathogens in the National Institute of Allergy and Infectious Disease Categories A, B, and C (www.niaid.nih.gov) such as Yersinia pestis (plague) Bacillus anthracis (anthrax), Francisella tularensis (tularemia), Mycobacterium tuberculosis, and influenza can be aerosolized in this chamber. Three of these priority agents were aerosolized in this study for aerosol model development.
The quality of the bioaerosol generated in the chamber is determined by the viability of the pathogens inside the chamber. This viability can be affected by a number of parameters such as the ambient temperature and humidity (Marthi et al. 1990). Marthi et al. have shown that lower temperature and higher humidity conditions increased survival of bacteria during aerosol exposures. Humidity not only affects viability during aerosol exposure but also during sampling (Kim et al. 2007). Viability of microbes can also be affect by parameters such as droplet size, exposure time duration, type of nebulizing media. Larger droplet sizes have shown to assist in increased survivability of microbes (Marthi et al. 1990). Pressures used in the Collison nebulizer can affect the viability of bacteria (Stone & Johnson 2002).
Bioaerosol sampling allows the researcher to optimize the multiple factors determining the quality of the aerosol. However, the Madison chamber as manufactured does not include a sampling port. In order to evaluate the performance of bioaerosol during an exposure, Madison chamber was modified to include a sampling port. 1) Humidity/temperature probe, 2) chamber pressure sensor connector, 3) Aerodynamic Particle Sizer (APS, TSI Inc., Model 3321) and 4) impinger (or BioSampler) were connected to the multiplex sampling port. Impingers and BioSamplers are widely used to determine the viability of bioaerosol (Ching-Wen et al. 1995, Peterson et al. 2007). The devices connected to the sampling port were controlled by the Aerosol Management Platform (Biaera Technologies, LLC).
The APS provides a measure of the particle size distribution in the bioaerosols (Hairston et al. 1997, Tobias et al. 2005, Yoon et al. 2008). The respiratory deposition is a function of aerodynamic particle size in small animal models and in the human respiratory tract (Brown et al. 2005, Schmid et al. 2008). By using the APS, we can optimize the particle size of the bioaerosol to be in the respirable size range for efficient deposition in the lungs of animal model.
B. anthracis, Y. pestis, and M. tuberculosis aerosols has been previously been used to challenge mice in whole body exposure systems (Nuermberger et al. 2004, Heine et al. 2007, Agar et al. 2008). We challenged the animals under similar conditions and did real-time sampling to determine bioaerosol viability and particle size characteristics using the multiplex sampling port.
2. Materials and methods
2.1. Animals
Animals were handled under a protocol approved by the Duke Institutional Animal Care and Use Committee. C57BL/6 and A/J mice from Jackson Labs were used for aerosol exposures. Mice used were 6–8 weeks old. Animals were acclimatized in the Biosafety Level 3 (BSL-3) animal holding area for one week prior to exposure. The animal rooms at Regional Biocontainment laboratory (RBL) at Duke are environmentally controlled at 21°C and 50% relative humidity (RH). The rooms are set to a 12-hour ON/OFF light cycle.
2.2. Aerobiology setup
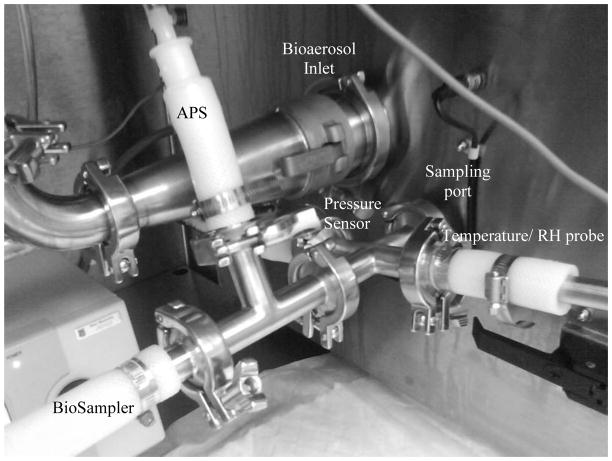
The Madison chamber in the RBL at Duke is connected to a class III biological safety cabinet (BSC, The Baker Company IsoGARD® series Glovebox). The Collison nebulizer which is attached to the front door of the Madison chamber is located inside the class III BSC. This setup enhances the safety of operation. The Baker Company installed a 1″ diameter stainless steel port through the door and the internal baffle of the Madison Chamber to allow sampling of the aerosol at the location of animal exposure. The multiplex sampling port was built around a stainless steel cross (MSC Industrial Co., Catalog No. 04562641). It was connected to a pipe t-fitting (McMaster-Carr, Catalog No. 4322K141) and quick clamp tube fitting hose adapters (McMaster-Carr, Catalog No. 4322K773) with the help of quick clamp tube fitting wing-nut clamps (McMaster-Carr, Catalog No. 4322K152) (Fig. 1).
Figure 1. Multiplex sampling port.
The APS, BioSampler, RH/temperature probe, and chamber pressure sensor are attached to the port. The port penetrates the door of the Madison chamber to sample the aerosol as delivered to animals.
The aerosol exposure was conducted with the turnkey system AeroMP (Aerosol Management Platform, Biaera Technologies, LLC) (Hartings & Roy 2004). The AeroMP controls, monitors, and records the aerobiology parameters. All the aerobiology parameters of nebulizer, dilution, and sampler air flows were programmed into the AeroMP software before the start of the aerosol exposure. The total airflow (aerosol and dilution) entering the Madison chamber was set to 50 lpm by the AeroMP. After the animals were loaded into the chamber, the exposure was initiated by executing the software. Ambient conditions of the chamber were monitored using an RH and temperature probe (Omega Engineering Inc., Model HX94C). The probe was attached to the multiplex sampling port. Humidified air was generated using an Air Bubbler (LabCommerce Inc, Model ZBA2). Humidifier was connected to the AeroMP which regulated is flowrate to set the chamber humidity to 50% RH (Fig. 2).
Figure 2. Whole body exposure system.
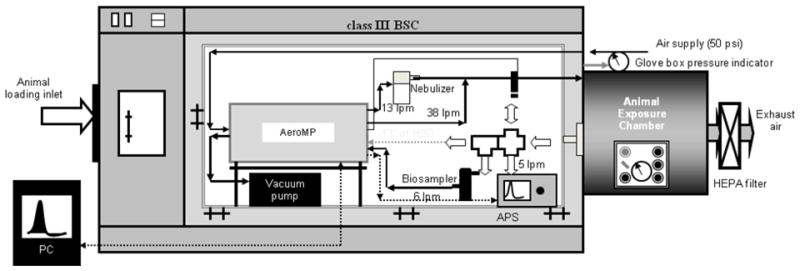
The Madison chamber is connected to a Class III BSC. The AeroMP receives real-time data from the chamber pressure sensor, RH/temperature probe, and APS. It controls the nebulizer flow, dilution air flow, humidifier, BioSampler, and APS.
Exhaust of the Madison chamber was connected to a vacuum pump. The vacuum pump generates exhaust flow while maintaining negative pressure inside the chamber. We used the AeroMP to control the flow rate, and used a control valve located between the two exhaust filters and the vacuum pump (Baker Manual 2006) to maintain chamber pressure at −13±1″WC.
To measure the chamber pressure one of the outlets of the multiplex sampling port was connected to the pressure sensor in the AeroMP. The chamber pressure was displayed in real time during the exposure run on AeroMP software. The software also recorded all the exposure parameters (airflow, chamber pressure, RH, and temperature) every five seconds.
Aerosol concentration and spray factor in the chamber can be reduced if there are any leaks in the sampling port or in the chamber itself. This issue can be resolved by doing a positive pressure decay test on the chamber before generating any aerosol. A positive pressure decay test was performed on the chamber connected to the multiplex sampling port and Collison nebulizer before every aerosol exposure. The end connections of the port were sealed with a sanitary fitting. The chamber was pressurized to 3″ of water column with air flow supplied with the AeroMP at 10 lpm. The chamber was considered to be in an operational condition for aerosol exposure experiments if the positive pressure in the chamber did not drop more than 20% in 30 minutes. Aerosol exposures were conducted once the setup had passed the pressure decay test.
To generate the aerosols, a 6-jet Collision nebulizer (CN25, BGI Incorporation) was used. The nebulizer was operated at 13±1 lpm and 19±1 PSI. For M. tuberculosis aerosols the nebulizer was operated at a higher flow 19±1 lpm corresponding to 35±1 PSI (Baker Manual 2006).
To determine the viability of the aerosol in the chamber, an all-glass impinger (AGI-4) (Ace Glass Inc., Model 7541–10) or BioSampler (SKC Inc., Model 225–9595) was connected to the multiplex sampling port. The AGI-4 was used to capture Y. pestis aerosol operating at a flowrate of 6 lpm while the BioSampler was used for M. tuberculosis operating at 12.5 lpm. A 20 mL volume of Heart Infusion Broth with 0.05% antifoam (Sigma-Aldrich Co., A5758) was used as the capture media solution in the impinger. In the BioSampler, 15 mL of phosphate-buffered saline (PBS) 1X was used. Operation of both the devices was controlled by AeroMP and they were operated full time during the 20 or 60 minute aerosol exposure cycle. The samplers were turned off during the 20-minute purge cycle after the aerosol exposure.
To measure the particle size distributions of various aerosols, the APS was connected to the multiplex sampling port (Fig. 2). No diluter was used along with the APS. The APS operation is controlled by AeroMP. AeroMP was used to set the APS flowrate at 5 lpm and sample for 30 seconds every 5 minutes, starting at 1 minute into the aerosol exposure. Vacuum pump of the APS was kept running during the whole exposure to maintain a constant airflow and stable negative pressure in the Madison chamber. AeroMP software (Version MC01) from Biaera was used to gather and analyze particle diameter and count data. Particle size distribution plots where done using Microsoft Excel.
APS 3321 was calibrated for both size and concentration using the TSI SMPS 3080 classifier and TSI Condensation Particle Counter 3772. The calibration was done by the yearly service contract with the Particle Instrument division of TSI Inc. (St. Paul, MN). Similar, the AeroMP is calibrated for accurate flow, pressure, temperature and RH (%) readings by the yearly service contract with the Biaera, LLC.
2.3. PSL bead sample preparation
Polystyrene latex (PSL) spheres of 1.0 μm size (5100A, Duke Scientific Corp.) were aerosolized in the chamber using the 6-jet Collison nebulizer at 13±1 lpm and 19±1 PSI. PSL beads were diluted 200 times in distilled water. The total volume for nebulization was 15 mL. For each aerosol run a new bead solution was prepared and sonicated for 1 minute prior to aerosolization. The PSL aerosol was sampled at every one minute interval during the 20 minute aerosol.
2.4. B. anthracis spore inocula preparation
To prepare the B. anthracis spores fresh 34F2 was streaked on a blood agar plate and incubated overnight at 37°C. A single colony of B. anthracis was placed into 6 mL Brain Health Infusion broth, and then shaken at 300 RPM at 37°C until turbid. A 1-mL volume of the culture was added to 200 ml Minimal Growth Medium in a 1 L baffled flask. The solution was shaken at 300 RPM at 37°C for 2 days to induce sporulation. The spore preparation was washed three times in sterile water, and incubated for 30 min in a 65°C water bath for 30 min to kill any vegetative anthrax. The spore preparations was pelleted once more, then resuspended in 10 mL sterile water, and stored at room temperature.
2.5. Y. pestis inocula preparation
Frozen stocks of Y. pestis stored at −80° C were used to prepare the culture medium. 1.0 mL of thawed stock solution was added to 100 mL of Heart Infusion Broth containing 100 μM FeCl2 and 1 mL of 50% glycerol. The solution was incubated at 27°C in a shaker incubator at 250 rpm for 24 hours. Y. pestis was grown in log phase overnight; its optical density (OD) was measured using a spectrophotometer at 600 nm. Once the OD was between 0.4–0.7, an 8 fold dilution of the solution was done. Bacteria were collected by centrifugation for 10 min at 2000 rpm (863g) and washed three times, first with HI media, second with 1:1 mix of HI media and diH2O, last with just diH2O. Washed bacteria were resuspended in diH2O at concentration of OD = 2.0 and sonicated using Misonix 2000 (output level 30%; three 10-second pulses with 20-second pause between pulses). Final inoculum preparation of 20 mL was supplemented with 0.2% xylose (Sigma-Aldrich Co, X2126-25G). 0.002% of anti-foam Y-30 (Sigma-Aldrich Co., A5758) was added immediately prior to nebulization. 100 μl of sonicated inoculum was used for determining starting inocula concentrations. The starting, ending inocula, and sampler concentrations were done within 1 hour of aerosol exposure.
2.6. M. tuberculosis inocula preparation
Frozen stocks of M. tuberculosis were used for preparing inocula for aerosolization studies. Frozen stock was thawed, and calculated volume of stock was diluted in 2 mL solution of PBS and tyloxapol. It was then sonicated twice for 15 seconds with two minute interval. The solution was diluted in PBS (containing 0.05% Tween 80) to bring the final volume to 15 mL. 0.002% of antifoam Y-30 was added to the final volume. The solution was poured into the precious liquid jar of the Collison nebulizer. The starting, ending inocula, and sampler concentrations were done within 1 hour of aerosol exposure.
2.7. Lung Homogenates
Lungs were harvested by necropsy within 1 hour of Y. pestis or B. anthracis aerosol exposure and 24 hours of M. tuberculosis aerosol exposure. Lungs were removed from the mice using sterile techniques into WhirlPak bags filled with 2 mL of PBST. Lungs were homogenized in the bags using Stomacher, with two 120 second cycles, and flipping bags in between. Homogenized lungs were plated to an appropriate bacterial medium to determine titer, and to a blood agar plate to screen for contamination. Titer plates were incubated at 37°C (B. anthracis and M. tuberculosis), or 27°C (Y. pestis) until distinct colonies were visualized.
2.8. Dose Presented and Dose Retained
The dose presented (Dp) was calculated using Guyton’s formula (Guyton 1947).
| (1) |
where BW is weight of mice in grams and Vm is minute volume.
| (2) |
where VE is the exposure volume and td is exposure time
| (3) |
where Dp is dose presented and Ca is the viable aerosol concentration
Viable aerosol concentration in the Madison chamber used in dose presented formula (Eq. 3) was calculated as
| (4) |
where Csam is concentration in sampler, VSampler is sampler initial volume, Ec is evaporation rate, td is exposure time duration, and Q Sampler is sampler airflow rate
Spray factor (Swearengen 2005) as shown in Tables 1–3 was calculated as
Table 1.
Aerosol parameters for B. anthracis spores and polystyrene latex beads
| Material | Concentration in chamber | Spray Factor | Dose Presented (mean CFU±SD) | Dose Retained (mean CFU±SD) | Dose Retention Efficiency (%) | Viable Aerosol Retention Rate (mL/min) |
|---|---|---|---|---|---|---|
| B.anthracis | 2.11e2 CFU/mL | 2.13e-7 | 2.50e5± 1.12e4 | 2.14e5±6.7e4 | 84 | 16.9 |
| PSL | 1.60e2 particles/mL | 3.07e-7 | - | - | - | - |
B. anthracis spores at a concentration of 9.90e8 CFU/mL were nebulized using a 6-jet Collison nebulizer at 13 lpm (19 PSI). A/J mice (n = 2) were exposed in the Madison chamber for 60 minutes. The B. anthracis aerosol was sampled using an AGI-4 impinger at 6 lpm. Dose retained in the lungs was measured by culturing a lung homogenate obtained 1 hr after exposure.
PSL beads at a concentration of 9.14e8 beads/mL were aerosolized under similar conditions with no mice in the chamber. The PSL particle concentration was measured with the Aerodynamic Particle Sizer.
Table 3.
Aerosol parameters for M. tuberculosis bacteria
| Starting Inoculum Concentration (CFU/mL) | Ending Inoculum Concentration (CFU/mL) | Viable Chamber Concentration (CFU/mL) | Spray Factor | Dose Presented (mean CFU±SD) | Dose Retained (mean CFU±SD) | Dose Retention Efficiency (%) | Viable Aerosol Retention Rate (ml/min) |
|---|---|---|---|---|---|---|---|
| 1.02e8 | 1.86e6 | 0.40e0 | 0.40e-8 | 172±9 | 119±42 | 69 | 14.9 |
| 3.30e7 | 2.48e6 | 1.22e0 | 3.71e-8 | 526±10 | 210±24 | 40 | 8.75 |
| 1.08e8 | 3.20e6 | 1.33e0 | 1.24e-8 | 574±23 | 168±12 | 29 | 6.45 |
| 2.13e8 | -- | 1.37e0 | 0.64e-8 | 584±25 | 171±18 | 29 | 6.25 |
M. tuberculosis bacteria were nebulized using a 6-jet Collison nebulizer at 19 lpm (35 PSI). C57BL/6 mice (n=4) were exposed in the Madison chamber for 20 minutes. The M. tuberculosis aerosol was sampled using a BioSampler at 12.5 lpm. Dose retained in the lungs was measured by culturing a lung homogenate obtained 24 hours after exposure.
| (5) |
where Fs is spray factor, Ca is concentration of bioaerosol (CFU/mL), Cs is concentration of liquid (CFU/mL)
The dose retained in the lungs (DR) was determined by titering the lung homogenate as described above. The dose retention efficiency was calculated as DR divided by DP.
The viable aerosol retention rate (VARR) was calculated as
| (6) |
To measure the aerosol size characteristics of B. anthracis spores and vegetative B. anthracis, they were aerosolized in the Madison chamber using the 6-jet Collision nebulizer at a flow rate of 13 lpm and 19 PSI. The total system flow was maintained at 50 lpm. APS was connected to the multiplex sampling port to measure particle mean size and standard deviation.
3. Results
3.1. Aerosol generation with PSL beads
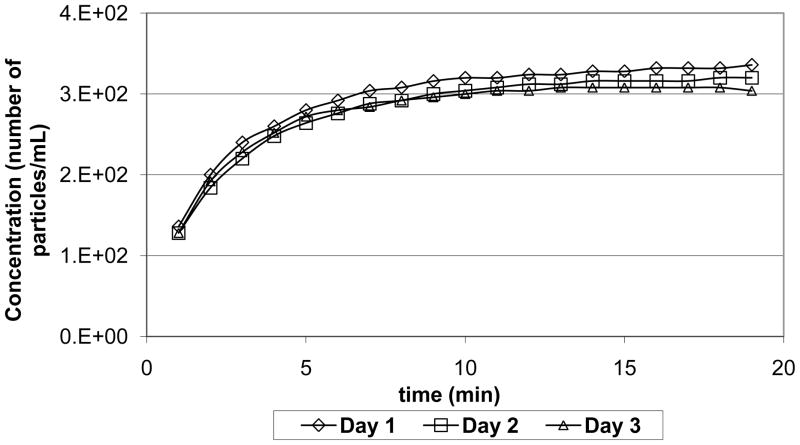
Bead concentration measured by APS is shown in figure 3. The mean concentrations of beads in the chamber measured on three different days were 2.95e2, 2.81e2, and 2.78e2 particles/mL (Fig. 3). The coefficient of variance of the mean concentration aerosolized on three different days was 3.19%. The particle size distribution for aerosolized beads is shown in Fig. 4 by count and in Fig. 5 by mass. The count mean aerodynamic diameter (CMAD) and mass mean aerodynamic diameter (MMAD) of the beads aerosolized on three different days were both 0.96 μm with a geometric standard deviation (GSD) of 1.06. The GSD was calculated using the particle size distribution by mass (Hinds 1999).
Figure 3. Particle concentration measured during aerosol delivery.
Polystyrene latex spheres of 1.0 μm diameter were aerosolized in the chamber for three different days. Each aerosol run was 20 minute duration with one minute sampling interval.
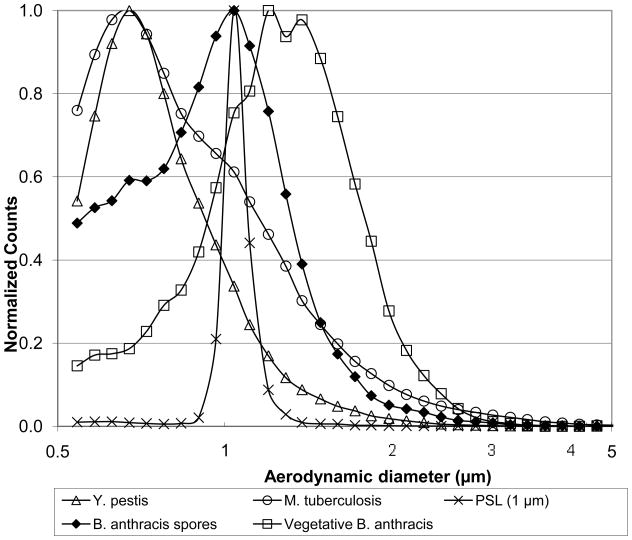
Figure 4. Particle size distributions by count.
Bacteria or polystyrene latex spheres were aerosolized in the Madison chamber using a Collison nebulizer. Aerosols were sampled through the multisampling port and analyzed using the APS. The actual counts were normalized to a peak of 1.0 for this figure.
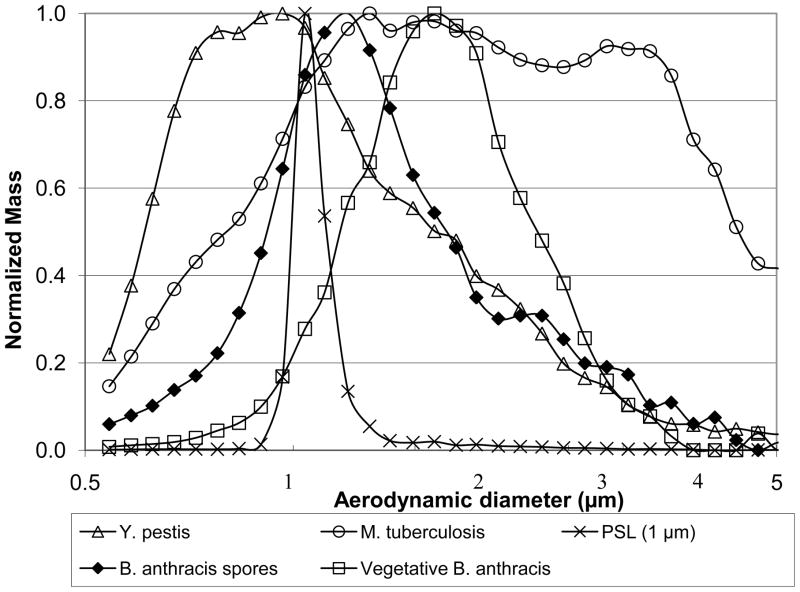
Figure 5. Particle size distributions by mass.
Bacteria or polystyrene latex spheres were aerosolized using a Collison nebulizer. The APS sampled the aerosol inside the Madison chamber through the multisampling port. The APS measured aerodynamic particle sizes, and used this data to estimate particle mass. Mass distributions were normalized to a peak of 1.0 for this figure.
3.2. Aerosol generation and murine challenge with B. anthracis spores
The CMAD and MMAD of anthrax spores were 0.98 and 1.25 microns with a GSD of 1.6 (Figs. 4 and 5). The vegetative B. anthrax CMAD and MMAD were measured to be 1.29 and 1.35 microns with a GSD of 1.33 (Figs. 4 and 5). Theoretically calculated dose presented using the Guyton’s formula was close to the dose retained in the mouse lungs after 1 hr necropsy (Table 1). The spray factor for the spores was higher than Y. pestis or M. tuberculosis, it was close to that of the PSL test particles. Dose retention efficiency and VARR was also highest for B. anthracis spores (Table 1).
3.3. Aerosol generation and murine challenge with Y. pestis bacteria
The Particle size distribution of Y. pestis was measured in real-time during the aerosol exposure. Figs. 4 and 5 show the PSD of Y. pestis when aerosolized in distilled water. The CMAD, MMAD measured by the APS were 0.78, 1.04 microns, respectively and GSD was 1.90 (Fig. 4).
For the study C57BL/6 mice (n = 3) were challenged with aerosol of Y. pestis KIM5 strain on three different days. Starting and ending inocula concentrations measured before and after aerosolization showed slight viability loss in the nebulizer (Table 2). Dose retained in the mouse lungs at 1 hr post exposure had similar counts. The theoretically calculated dose presented using Guyton’s formula was higher (Table 2).
Table 2.
Aerosol parameters for Y. pestis bacteria
| Starting Inoculum Concentration (CFU/mL) | Ending Inoculum Concentration (CFU/mL) | Viable Chamber Concentration (CFU/mL) | Spray Factor | Dose Presented (mean CFU±SD) | Dose Retained (mean CFU±SD) | Dose Retention Efficiency (%) | Viable Aerosol Retention Rate (mL/min) |
|---|---|---|---|---|---|---|---|
| 5.75e9 | 5.10e9 | 6.52e1 | 1.13e-8 | 25500±200 | 4280±335 | 17 | 3.3 |
| 7.90e9 | 7.00e9 | 6.09e1 | 0.83e-8 | 23433±666 | 4270±568 | 18 | 3.5 |
| 5.70e9 | 3.20e9 | 4.59e1 | 0.80e-8 | 17233±493 | 3570±230 | 21 | 3.9 |
Y. pestis bacteria were nebulized using a 6-jet Collison nebulizer at 13 lpm (19 PSI). C57BL/6 mice (n=3) were exposed in the Madison chamber for 20 minutes. The Y. pestis aerosol was sampled using an AGI-4 impinger at 6 lpm. Dose retained in the lungs was measured by culturing a lung homogenate obtained 1 hr after exposure.
The ability of microorganism to undergo the process of nebulization and aerosolize in the Madison chamber was estimated based on the viable aerosol concentration and spray factor (Swearengen 2005). Three different runs of Y. pestis showed similar spray factor values, however, they were less than that of test particles (Table 1). Y. pestis aerosol gave the lowest dose retention efficiency and VARR values (Table 2).
3.4. Aerosol generation and murine challenge with M. tuberculosis bacteria
From the particle size distribution (PSD) of M. tuberculosis measured by the APS, CMAD and MMAD were 0.77 μm and 1.98 μm, respectively and GSD was 2.37 (Figs. 4 and 5). B6 mice (n = 4) were challenged with four different M. tuberculosis aerosols each for 20 minutes. Results of the exposures are shown in Table 3. There was a 100 fold loss between the starting and ending inocula concentrations. The dose retained in mice at 24 hours was in a range of 119–210 CFU/lung. M. tuberculosis aerosol had the lowest viable aerosol concentration and its spray factor was 40 times lower than that of PSL beads (Tables 1 and 3). Theoretically calculated dose retained using the Guyton’s formula was higher than the dose retained in the mouse lungs. M. tuberculosis aerosol gave dose retention efficiency and VARR intermediate between B. anthracis and Y. pestis aerosols.
4. Discussion
This is the first published description of the use of a sampling port with the Madison chamber. By sampling bioaerosol in the chamber we showed that Y. pestis, M. tuberculosis, and B. anthracis aerosols were in the mouse respirable particle size range and of adequate viability to deliver them to mouse lungs. With the assistance of multiplex sampling port it was possible to measure a number of aerobiology parameters such as viable aerosol concentration, spray factor, dose presented, VARR, and particle size characteristics. There aerobiology parameters were used to understand the characteristics of the microbes from the generation to the delivery and retention process, and ultimately to optimize aerosol delivery to murine lungs.
The concept of VARR measured using the multiplex sampling port is being introduced for the first time in this paper (Tables 1–3). VARR is defined as the rate at which the viable aerosol volume is retained in the mouse lungs. It quantifies the ability of the microbe to deposit and survive in the lungs. It is similar to dose retention efficiency, but makes no assumptions on minute ventilation. Retention efficiency uses Guyton’s formula to estimate minute ventilation thereby adjusting to the variations in animal weights (Eq. 1). VARR is based directly on the measured values, but does not include adjustments based on predicted minute ventilation (Eq. 6).
Similar to spray factor, which indicates the viable efficiency of the aerosol that is aerosolized compared to the inocula, VARR indicates the viable efficiency of the aerosol that deposits in the lung compared to viable aerosol concentration in the chamber. VARR can be used in conjunction with spray factor to measure the efficiency of aerosol that was generated and delivered to the animals.
Using the multiplex sampling port, spray factors were calculated for the three microbes and the PSL beads. The PSL bead spray factor was calculated based on the aerosol particle concentration as measured by the APS. In contrast the bacterial spray factors were based on viable bacteria captured by a sampling device (BioSampler or impinger). The bead spray factor was used to estimate the highest achievable spray factor under the present instrument and flow configurations. Bacterial spray factors will be reduced compared to this ideal spray factor if the nebulizer if less efficient in aerosolizing bacteria as compared to beads, if bacterial viability is reduced during the process, or if the capture of microbes in the sampling device is incomplete.
The spray factor for B. anthracis spores was much higher than the other microbial spray factors, and approximated that obtained for PSL beads. B. anthracis spores able to survive for prolonged periods in harsh environmental conditions for a long time. B. anthrax spores also had high dose retention efficiency and VARR followed by M. tuberculosis and then Y. pestis. This could be because spores might be surviving in the mouse lungs better by evading the lung defense mechanisms (Welkos et al. 1986). Dose retention efficiency was lower for Y. pestis and M. tuberculosis. This loss of dose retained might be cleared in the lungs by the pulmonary defense or the pulmonary environment might not be totally friendly to it.
The aerobiology parameters measured for M. tuberculosis showed greater variation as compared to B. anthracis spores and Y. pestis (Table 3). This range of variation is similar to that in other studies (Nuermberger et al. 2004). Mycobacteria possess a waxy capsule that leads to aggregation when grown in liquid media. Microscopic examination has demonstrated significant clumping of mycobacteria even after sonication. Bacterial aggregation may explain the greater variation among experiments, and the greater GSD observed with M. tuberculosis. The greater GSD may also be due to the suspension of M. tuberculosis in PBS, while all other aerosols were suspended in de-ionized water (Fig. 5). This produces a polydisperse particle size distribution of particles not only of M. tuberculosis but also solvent particles of PBS.
The APS measures aerodynamic particle sizes between 0.542 μm to 19.81 μm. Based on the microscopic size of these bacteria, we expected that viable bacteria would have an aerodynamic diameter within this range. Smaller particles are present in these aerosols and are composed of solvent generated particles and debris from bacteria damaged by the Collison nebulizer during aerosolization. We did not consider the smaller particles when calculating CMAD, MMAD, or GSD.
The measured aerodynamic size of vegetative B. anthrax was greater than the B. anthrax spores (Fig. 4).The vegetative B. anthrax also had narrower size distribution compared to the spores (Figs. 4 and 5). Similar size characteristics of spores and vegetative species have been previously reported by microscopic examination (Inglesby et al. 1999).
Impingers and BioSamplers used in this study offer incomplete capture of the viable aerosol. This is a limitation of the sampling devices. We chose devices with reasonable efficiency within the particle size ranges expected for these bacteria. Prior work has shown that the collection efficiency of the impinger and BioSampler are 70–80% and 80–90% in the 0.5 to 2 micron size range, respectively, and >90% for both devices for particle sizes larger than 2 μm (Cox & Wathes 1995, Baron & Willeke 2001). Incomplete capture means that the calculated viable aerosol concentration is an underestimate. Even though the dose presented based on the viable aerosol concentration might have been slightly underestimated the dose retained for all the three microbes (Tables 1–3) was lower than the dose presented. Multiple factors may explain this reduction. Only a fraction of the dose presented is actually deposited in the lungs. Some particles lodge in the upper airways, and some particles may reach the lungs but be exhaled without deposition. Lastly, bacteria deposited in the lungs may be cleared anatomically or killed by host defense mechanisms before necropsy. The measured dose retained may increase over time if bacteria replicate after deposition. We chose the time of necropsy based on the rate of replication of the various bacteria to minimize the effect of replication (one hour after aerosol delivery for B. anthracis and Y. pestis; 24 hours for M. tuberculosis).
The multiplex sampling port provides the user with many advantages. Bioaerosols can be analyzed for their particle size distribution and viability. The use of a biosampler allows the user to optimize the viable aerosol concentration without the need for experimental animals. The effect of humidity, flow rates, and inoculum preparation methods on the viable aerosol concentration can be directly measured.
The multiplex sampling port is built using stainless steel components. This gives it an added advantage to be used in BSL-3 environment where the system exposed to bioaerosol needs to be thoroughly decontaminated with various kinds of chemical agents. Stainless steel offers greater chemical stability and can be easily autoclaved thereby increasing its operational shelf life.
In conclusion, attaching a multiplex port to Madison chamber enhances the functionality of whole body exposure system. The sampling port adds real time sampling capability to the system and assists in gathering valuable information related to the quality of the bioaerosol in the chamber.
Acknowledgments
This work was supported by NIH grants U54 AI057157 (Southeast Regional Center of Excellence for Emerging Infections and Biodefense), P30 AI051445 (Duke Center for Translational Research), and UC6 AI058607 (Regional Biocontainment Laboratory at Duke). The authors also acknowledge Scott Alderman for his assistance providing BSL-3 training.
Footnotes
Author Disclosure Statement
The authors of this article have no conflicting financial interests.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Agar SL, Sha J, Foltz SM, Erova TE, Walberg KG, Parham TE, Baze WB, Suarez G, Peterson JW, Chopra AK. Characterization of a mouse model of plague after aerosolization of Yersinia pestis CO92. Microbiology. 2008;154(Pt 7):1939–48. doi: 10.1099/mic.0.2008/017335-0. [DOI] [PubMed] [Google Scholar]
- Baker Manual. Operating and Maintenance Manual for IsoGARD Isolator S/N 89357. 2006. [Google Scholar]
- Baron PA, Willeke K. Aerosol measurement: Principles, Techniques, and Applications. Wiley-Interscience; 2001. [Google Scholar]
- Basaraba RJ, Smith EE, Shanley CA, Orme IM. Pulmonary lymphatics are primary sites of Mycobacterium tuberculosis infection in Guinea Pigs Infected by Aerosol. Infect Immun. 2006;74(9):5397–5401. doi: 10.1128/IAI.00332-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown JS, Wilson WE, Grant LD. Dosimetric Comparisons of Particle Deposition and Retention in Rats and Humans. Inhalation Toxicology. 2005;17(7–8):355–385. doi: 10.1080/08958370590929475. [DOI] [PubMed] [Google Scholar]
- Ching-Wen C, Grinshpun SA, Willeke K, Macher JM, Donnelly J, Clark S, Juozaitis A. Factors affecting microbiological colony count accuracy for bioaerosol sampling and analysis. Am Ind Hyg Assoc J. 1995;56(10):979–86. doi: 10.1080/15428119591016403. [DOI] [PubMed] [Google Scholar]
- Cox CS, Wathes CM. Bioaerosols Handbook. Boca Raton, FL: CRC Lewis Publishers; 1995. [Google Scholar]
- Guyton A. Analysis of respiratory patterns in laboratory animals. Am J Physiol. 1947;150(1):78–83. doi: 10.1152/ajplegacy.1947.150.1.78. [DOI] [PubMed] [Google Scholar]
- Hairston PP, Ho J, Quant FR. Design of an instrument for real-time detection of bioaerosols using simultaneous measurement of particle aerodynamic size and intrinsic fluorescence. J Aerosol Sci. 1997;28(3):471–82. doi: 10.1016/s0021-8502(96)00448-x. [DOI] [PubMed] [Google Scholar]
- Hartings JM, Roy CJ. The automated bioaerosol exposure system: Preclinical platform development and a respiratory dosimetry application with nonhuman primates. Journal of Pharmacological and Toxicological Methods. 2004;49(1):39–55. doi: 10.1016/j.vascn.2003.07.001. [DOI] [PubMed] [Google Scholar]
- Heine HS, Bassett J, Miller L, Hartings JM, Ivins BE, Pitt ML, Fritz D, Norris SL, Byrne WR. Determination of Antibiotic Efficacy against Bacillus anthracis in a Mouse Aerosol Challenge Model. Antimicrob Agents Chemother. 2007;51(4):1373–1379. doi: 10.1128/AAC.01050-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hinds WC. Aerosol Technology: Properties, Behavior, and Measurement of Airborne Particles. Wiley-Interscience; 1999. [Google Scholar]
- Inglesby TV, Henderson DA, Bartlett JG, Ascher MS, Eitzen E, Friedlander AM, Hauer J, McDade J, Osterholm MT, O’Toole T, Parker G, Perl TM, Russell PK, Tonat K for the Working Group on Civilian B. Anthrax as a Biological Weapon: Medical and Public Health Management. JAMA. 1999;281(18):1735–1745. doi: 10.1001/jama.281.18.1735. [DOI] [PubMed] [Google Scholar]
- Kim S, Ramakrishnan M, Raynor P, Goyal S. Effects of humidity and other factors on the generation and sampling of a coronavirus aerosol. Aerobiologia. 2007;23(4):239–248. doi: 10.1007/s10453-007-9068-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marthi B, Fieland VP, Walter M, Seidler RJ. Survival of bacteria during aerosolization. Appl Environ Microbiol. 1990;56(11):3463–3467. doi: 10.1128/aem.56.11.3463-3467.1990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nuermberger EL, Yoshimatsu T, Tyagi S, Bishai WR, Grosset JH. Paucibacillary Tuberculosis in Mice after Prior Aerosol Immunization with Mycobacterium bovis BCG. Infect Immun. 2004;72(2):1065–1071. doi: 10.1128/IAI.72.2.1065-1071.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peterson JW, Comer JE, Baze WB, Noffsinger DM, Wenglikowski A, Walberg KG, Hardcastle J, Pawlik J, Bush K, Taormina J, Moen S, Thomas J, Chatuev BM, Sower L, Chopra AK, Stanberry LR, Sawada R, Scholz WW, Sircar J. Human monoclonal antibody AVP-21D9 to protective antigen reduces dissemination of the Bacillus anthracis Ames Strain from the Lungs in a Rabbit Model. Infect Immun. 2007;75(7):3414–24. doi: 10.1128/IAI.00352-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schmid O, Bolle I, Harder V, Karg E, Takenaka S, Schulz H, Ferron G. Model for the deposition of aerosol particles in the respiratory tract of the the rat. I. Nonhygroscopic particle deposition. J Aerosol Med Pulm Drug Deliv. 2008;21(3):291–307. doi: 10.1089/jamp.2008.0689. [DOI] [PubMed] [Google Scholar]
- Stone RC, Johnson DL. A Note on the Effect of Nebulization Time and Pressure on the Culturability of Bacillus subtilis and Pseudomonas fluorescens. Aerosol Science and Technology. 2002;36(5):536–539. [Google Scholar]
- Swearengen JR. Biodefense: Research Methodology and Animal Models. CRC Press; 2005. [Google Scholar]
- Tobias HJ, Schafer MP, Pitesky M, Fergenson DP, Horn J, Frank M, Gard EE. Bioaerosol mass spectrometry for rapid detection of individual airborne. Appl Environ Microbiol. 2005;71(10):6086–6095. doi: 10.1128/AEM.71.10.6086-6095.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Welkos SL, Keener TJ, Gibbs PH. Differences in susceptibility of inbred mice to Bacillus anthracis. Infect Immun. 1986;51(3):795–800. doi: 10.1128/iai.51.3.795-800.1986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yoon K-Y, Byeon JH, Park J-H, Ji JH, Bae GN, Hwang J. Antimicrobial Characteristics of Silver Aerosol Nanoparticles against Bacillus subtilis Bioaerosols. Environmental Engineering Science. 2008;25(2):289–294. [Google Scholar]