Abstract
Primary immunodeficiencies (PIDs) are characterized by an increased susceptibility to infections due to defects in one ore more components of the immune system. Although most PIDs are relatively rare, they are more frequent than generally acknowledged. Early diagnosis and treatment of PIDs save lives, prevent morbidity, and improve quality of life. This early diagnosis is the task of the pediatrician who encounters the child for the first time: he/she should suspect potential PID in time and perform the appropriate diagnostic tests. In this educational paper, the first in a series of five, we will describe the most common clinical presentations of PIDs and offer guidelines for the diagnostic process, as well as a brief overview of therapeutic possibilities and prognosis.
Keywords: Primary immunodeficiency, Diagnosis, Protocol, Lymphocyte, Immunoglobulin
Introduction
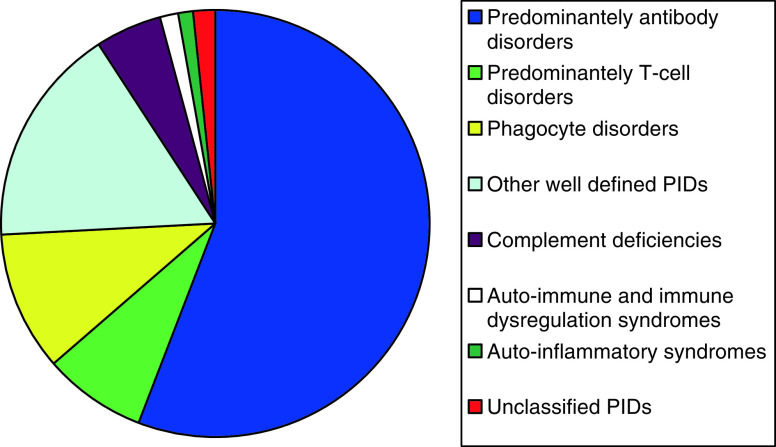
Primary immunodeficiencies (PIDs) are characterized by defects in the development and function of the human immune system. As a result, there is an increased susceptibility to infections, although some PIDs rather present with autoimmunity or lymphoproliferation. To date, the molecular basis of more than 150 PIDs has been unraveled and this number is increasing rapidly [10]. PIDs can be separated into eight categories, depending on which part of the immune system is dysfunctional [10] (Table 1). An overview of the frequency of PID diagnoses in the database of the European Society for Immunodeficiencies (ESID) shows that primary antibody deficiencies constitute more than half of the reported PID diagnoses [7] (Fig. 1). Other frequently reported PID categories are the predominantly T-cell disorders, abnormalities in granulocyte number or function, and the other well-defined immunodeficiency syndromes. The estimated prevalence differs widely per individual PID diagnosis, from approximately 1:500 for IgA deficiency—being the most frequent, but often asymptomatic—to >1:100,000 for very serious forms of severe combined immunodeficiency (SCID), immune dysregulation syndromes, and complement deficiencies. Although most PIDs are relatively rare, they are more frequent than generally acknowledged. There is a lack of awareness of PIDs among the public and health care workers alike, resulting in diagnostic delay. (http://ec.europa.eu/health/ph_projects/2005/action1/docs/action1_2005_exs_01_en.pdf). However, early diagnosis and treatment of PIDs save lives, prevent morbidity, and improve quality of life. In this educational paper, the first in a series of five, we will describe the clinical presentations of PIDs and offer guidelines for the diagnostic evaluation of suspected PID, as well as a brief overview of therapeutic possibilities and prognosis. The different categories of PIDs will be described in more detail in the remainder of the educational reviews in future issues of the Journal. The field of PID is too extensive to cover all different PIDs known to date. Therefore, the subsequent reviews will focus on the four largest PID categories: antibody deficiencies, T-cell disorders, disorders of granulocyte number and/or function, and the category of other well-defined immunodeficiency syndromes.
![]()
Table 1.
The eight pathogenetic categories of PID according to the IUIS
| Disease category | Diagnosesa |
|---|---|
| Combined B- and T-cell immunodeficiencies (predominantly T-cell) | (Severe) combined immunodeficiency, (S)CID; many different genetic defects |
| CD40L deficiency | |
| Predominantly antibody deficiencies | X-linked or AR agammaglobulinemia |
| Common variable immunodeficiency disorders (CVIDs) | |
| Specific antibody deficiencies | |
| IgG-subclass deficiency | |
| Selective IgA deficiency | |
| Other well-defined immunodeficiency syndromes | Wiskott Aldrich syndrome |
| Ataxia telangiectasia and other DNA repair disorders | |
| Hyper-IgE syndromes | |
| Disease of immune dysregulation | Immunodeficiencies with hypopigmentation |
| Familial hemophagocytic lymphohistiocytosis syndromes (HLH) | |
| X-linked lymphoproliferative syndrome | |
| Autoimmune lymphoproliferative syndrome (ALPS) | |
| Congenital defects of phagocyte number, function, or both | Severe congenital neutropenia |
| Cyclic neutropenia | |
| X-linked or AR chronic granulomatous disease (CGD) | |
| Defects in innate immunity | Anhidrotic ectodermal dysplasia with immunodeficiency |
| IL-1 receptor-associated kinase 4 deficiency (IRAK-4 deficiency) | |
| Chronic mucocutaneous candidiasis | |
| Autoinflammatory disorders | Familial Mediterranean fever |
| TNF receptor-associated periodic fever (TRAPS) | |
| Hyper-IgD syndrome | |
| Cryopyrin-associated periodic syndromes | |
| Complement deficiencies | Broad spectrum of deficiencies of classical and alternative pathway complement factors |
| Hereditary angioedema (C1 esterase inhibitor deficiency) |
AR autosomal recessive, IUIS International Union of Immunological Societies Expert Committee on Primary Immunodeficiencies
aThere are >150 primary immunodeficiencies; for the complete list of diagnoses: PID 2009 update, J Allergy Clin Immunol 2009
Fig. 1.
Distribution of PID in Europe according to the ESID patient registry 2010 (http://www.esid.org/statistics.php?sub=2), n = 10,747. PIDs primary immunodeficiencies, ESID European Society for Immunodeficiencies
A diagnostic strategy for PIDs
It is not easy to timely identify potential PID patients among the many children seen in everyday practice by pediatricians; PIDs often present with very common and/or aspecific signs and symptoms [5]. The relative rarity of the individual PIDs also contributes to the diagnostic challenge. As a consequence, diagnostic delay is common [4,15]. An effective diagnostic strategy should be able to quickly identify PIDs with rapidly fatal complications like severe combined immunodeficiency (SCID) and to limit diagnostic delay in children with PIDs with a more protracted course like common variable immunodeficiency disorders (CVIDs), who may develop bronchiectasis with pulmonary disability [15] and decreased life span if treatment is delayed.
The best way to efficiently recognize PIDs in children is to rely on adequate “pattern recognition” of the various clinical presentations, followed by an initial limited set of laboratory examinations, aiming at the exclusion of a PID with rapidly fatal complications. A diagnostic protocol including more detailed investigations can be used when the initial examinations are compatible with a PID or when clinical problems persist despite a normal initial evaluation. For this, the elaborate ESID multistep diagnostic protocol for PIDs is very useful [5]. Eventually, the aim is to establish a genetic diagnosis by sequence analysis of candidate genes, which is important to guide treatment and follow-up of PID patients, as well as genetic counseling of families [16]. However, in a substantial proportion of PID patients, genetic defects have not been found so far.
![]()
Clinical presentation and diagnosis of PID
Analysis of a child with potential PID begins with the history and physical examination like in any other situation in pediatric practice. Symptoms and signs suggestive of PID summarized in Tables 2 and 3 can be used as warning signs (http://www.info4pi.org/aboutPI/pdf/General10WarningSignsFINAL.pdf). PIDs tend to present in clinically recognizable patterns of signs and symptoms, which can be grouped in eight different clinical presentations determined by the underlying pathogenesis (Table 1) [5]. Of these, recurrent ENT and airway infections is by far the most common. It is essential to be familiar with these clinical presentations to be able to recognize potential cases of PIDs; knowledge of the pathogenesis is helpful, but not strictly necessary. In this respect, an important clue for the potential presence of PID is the family history: although most children presenting with recurrent infections do not have PID, this becomes much more likely when it runs in the family or when parents are consanguineous. In those cases, further investigations should not be postponed. In this section, we will discuss the categories of PID in relation to the eight different clinical presentations.
Table 2.
Symptoms and signs that can point towards the presence of PID
| Medical history |
| Recurrent (proven) bacterial infections |
| Two ore more severe infections (pneumonia, sepsis, meningitis, osteomyelitis) |
| Atypical presentation of infection |
| Unusually severe course of infection or impaired response to treatment |
| Infections caused by an unexpected or opportunistic pathogen |
| Recurrent infections with the same type of pathogen |
| Abscesses of internal organs or recurrent subcutaneous abscesses |
| Failure to thrive with prolonged or recurrent diarrhea |
| Generalized long-lasting warts or mollusca contagiosa |
| Extensive prolonged candidiasis (oral/skin) |
| Delayed (>4 weeks) separation of the umbilical cord |
| Delayed shedding of primary teeth |
| Family history of immunodeficiency, unexplained infant deaths, or consanguinity of the parents |
| Difficult-to-treat obstructive lung disease, unexplained bronchiectasis |
| Atypical autoimmune disease and/or lymphoproliferation |
| Physical examination |
| Dysmorphic features, especially facial abnormalities and microcephaly |
| Partial albinism, abnormal hair, severe eczema, dermatitis |
| Telangiectasia, ataxia |
| Gingivitis, oral ulcers/aphthae |
| Abnormal wound healing |
| Absence of immunological tissue (lymph nodes, tonsils) |
| Lymphadenopathy |
| Organomegaly |
| Digital clubbing |
| Vasculitis |
Clin Exp Immunol 2006 and the Jeffrey Modell Foundation warning signs for PID
Table 3.
Clinical presentation, differential diagnosis, and first-line diagnostic work-up of potential PID
| Clinical presentation | Suspected immunodeficiency | Non-immunological differential diagnosis (most frequent on top) | First-line immunologic diagnostic work-up |
|---|---|---|---|
| Recurrent ENT and airway infections | Antibody deficiency | Normal frequency in infants and young children | Full blood count and differential |
| Phagocyte deficiency | Asthma, allergy, bronchial hyperreactivity | IgG, IgA, IgM | |
| HIV | Adenoidal hypertrophy | In case of agammaglobulinemia: lymphocyte subpopulations (B-cells present?) | |
| PID related to eponymous syndrome | Gastro-esophageal reflux | In case of hypogammaglobulinemia or persistent problems: IgG-subclasses, specific antibody responses, CH50, AP50, lymphocyte subpopulations | |
| Wiskott Aldrich Syndrome | Inhaled foreign body | ||
| Complement deficiency | Cystic fibrosis | ||
| Primary ciliary dyskinesia | |||
| Congenital anomaly | |||
| Failure to thrive from early infancy (often combined with intractable diarrhea) | T-lymphocyte deficiency: (S)CID | Wide variety of other causes, see appropriate textbooks | Exclude SCID and HIV infection: |
| HIV | Full blood count and differential, IgG, IgA, IgM | ||
| HIV test | |||
| Lymphocyte subpopulations (decreased T-cells?) | |||
| Recurrent pyogenic infections (e.g., abscesses of internal organs or recurrent subcutaneous abscesses) | Congenital defects of granulocyte number, function, or both | Disrupted skin (eczema, burns) | Full blood count and differential |
| Carriage of virulent strain of Staphylococcus aureus | Perform repeatedly in case of cyclic pattern of fever: | ||
| Drug-related neutropenia | 3×/week for 3–6 weeks | ||
| Alloimmune neutropenia, benign neutropenia of infancy (autoimmune neutropenia) | In case problems persist and there is no neutropenia, antibody or complement deficiency: phagocyte function tests | ||
| Hematological malignancy | |||
| Unusual infections or unusually severe course of infections (e.g., opportunistic infections) | T-lymphocyte deficiency: (S)CID | Secondary immunodeficiency: | Full blood count and differential, |
| HIV | Malignancy, malnutrition, chronic disease, immunosuppressive therapy | IgG, IgA, IgM | |
| Wiskott Aldrich Syndrome | HIV test | ||
| Defects of innate immunity | Lymphocyte subpopulations (decreased T-cells?) | ||
| Recurrent infections with the same type of pathogen | Encapsulated bacteria: antibody deficiency | Increased exposure | Full blood count and differential |
| Meningococci: complement deficiency | Inadequate treatment of first infection | IgG, IgA, IgM, follow diagnostic work-up for recurrent ENT and airway infections | |
| Candida: T-lymphocyte deficiency | Anatomical defects, e.g., CSF fistula in case of recurrent meningitis | In case of meningococcal disease: CH50, AP50 | |
| Mycobacteria: macrophage–T-cell interaction problem | In case of mycobacteria: consult immunologist | ||
| Autoimmune or chronic inflammatory disease; lymphoproliferation | CVIDs | Other systemic autoimmune diseases like autoimmune cytopenias | Initial work-up depends upon clinical presentation |
| Hemophagocytic lymphohistiocytosis (HLH) | SLE | ||
| Autoimmune lymphoproliferative syndrome (ALPS) | |||
| Characteristic combinations of clinical features in eponymous syndromes and PID warning signs | DNA-repair defects | See appropriate textbooks for syndrome characteristics | Initial work-up depends upon the suspected syndromes |
| Hyper-IgE syndromes | |||
| Microdeletion 22q11 (DiGeorge) | |||
| Angioedema | C1 esterase inhibitor deficiency | Allergy, malignancy, autoimmunity, drug-related | C1 esterase inhibitor |
CVID common variable immunodeficiency disorders, PID primary immunodeficiency
Modified from Clin Exp Immunol 2006
Combined B- and T-cell immunodeficiencies (predominantly T-cell)
The fate of a child with severe PID is determined by rapid diagnosis and treatment. This is most urgent for children with SCID [13], who generally present with failure to thrive from early infancy in combination with intractable diarrhea. In addition, unusual (opportunistic) infections or unusually severe course of infections are part of the clinical spectrum. In children who present with a severe interstitial pneumonia, Pneumocystis jiroveci is the most likely opportunistic pathogen. The hallmark of SCID is T-cell lymphopenia in combination with hypo- or agammaglobulinemia. T-cell lymphopenia is reflected in low lymphocyte counts in the leukocyte differential. Determination of the immunoglobulins in serum shows decreased levels of IgG, IgA, and IgM. Pitfalls are the relative lymphocytosis of young infants and the presence of maternal immunoglobulins in the first months of life. It is therefore essential to use age-matched reference values for interpretation of laboratory results [3]. Also, the presence of maternal T-cells in the patient’s peripheral blood can obscure the T-cell lymphopenia. Further analysis consists of lymphocyte subpopulation analysis and subsequent genetic analysis of candidate genes. In any child with unusual (opportunistic) infections, or unusually severe course of infections, and who does not have abnormalities in this initial work-up, further diagnostic steps should be undertaken considering other PIDs mentioned in Table 3. Also, HIV infection has to be excluded at this stage.
Antibody deficiencies
Congenital agammaglobulinemias generally present with recurrent ENT and airway infections, but may also present with severe bacterial infections in other organ systems [18]. The differential diagnosis is extensive (Table 3). However, they represent emergencies which are relatively easy to detect by the determination of immunoglobulin levels. These basic laboratory tests should not be postponed until other possibilities have been ruled out. Agammaglobulinemia usually presents after the age of 3 months to 2 years because of an increased susceptibility to bacterial infections once the infant’s protection by maternal antibodies is weaning. All three immunoglobulin isotypes are severely decreased. Analysis of lymphocyte subpopulations will show the near absence of B-lymphocytes. Determination of the exact nature of the defect is possible by analysis of genes that affect early B-cell development. A defect in Bruton’s tyrosine kinase, causing X-linked agammaglobulinemia, is present in 85% of agammaglobulinemic patients.
Infants with a (moderate) decrease of IgG and IgA, but with normal B-lymphocyte numbers, most likely suffer from transient hypogammaglobulinemia, which is a self-limiting condition with a mild clinical course. If the hypogammaglobulinemia is profound in the presence of normal or elevated IgM levels, a CD40L deficiency (Table 1) is part of the differential diagnosis.
Less urgent, but still important in the light of preventing future damage and decreased quality of life and life span, is the recognition of the more subtle or late-onset forms of antibody deficiency like specific antibody deficiencies and CVID. The latter is defined by a decrease of at least two of the three immunoglobulin isotypes and a decreased response to immunization (ESID–PAGID criteria) in a child older than 2 years of age. These patients generally present with recurrent ENT and airway infections [4]. However, most young children with this clinical presentation do not have PID. Especially in children below 2 years of age, a high frequency of upper respiratory tract infections in an otherwise healthy child is very common. An increased exposure to infections in day care centers, increased susceptibility to infections secondary to cigarette smoke exposition, adenoidal hypertrophy, and bronchial hyperreactivity and/or atopy all contribute to a high frequency of respiratory complaints. Simple measures and a wait-and-see approach are fully justified in most cases. However, when more than one pneumonia occurs, further investigations into immunological as well as non-immunological causes are mandatory (Table 3). Also, the frequency of respiratory infections should decrease when the child grows older. When this is not the case, PID becomes more likely, and further investigations such as repeated serum IgG, IgA, IgM, and IgG subclasses, specific antibody responses to vaccination, and a lymphocyte subpopulation screen may be warranted using age-matched reference values for the interpretation of the results [3].
Well-defined immunodeficiency syndromes
The occurrence of signs and symptoms that point towards PID in children with syndromic features is suggestive of the presence of a well-defined immunodeficiency syndrome. Recognition of these syndromes requires detailed immunological and clinical genetic knowledge and warrants further evaluation for immunodeficiency and examination by a specialist in clinical genetics. The immunological work-up depends on the expected syndrome. In case of DNA repair disorders, analysis should include the determination of immunoglobulin levels, whereas patients with hyper-IgE syndromes may suffer from a disorder of granulocyte function.
Diseases of immune dysregulation
PID syndromes with immune dysregulation form a separate category of patients in which the increased susceptibility to infections is not the main problem. A life-threatening immune dysregulation syndrome is hemophagocytic lymphohistiocytosis (HLH). HLH is characterized by an exaggerated but ineffective immune response which leads to severe hyperinflammation. Many cases are triggered by an infection, but the basis is often an inherited defect in immune effector cells [11,12]. The presentation of familial HLH is clinically indistinguishable from the HLH associated with lymphoproliferative syndromes, which are mostly X-linked and induced by an EBV infection. The major diagnostic pitfall in HLH is to misdiagnose children as having sepsis because fever and severe inflammation are almost invariably present. In any critically ill febrile child with negative blood cultures and persistent fever despite antibiotic treatment, HLH should be considered as a potential diagnosis. Apart from fever, the criteria used to diagnose HLH include hepatosplenomegaly, bi-cytopenia, elevated serum ferritin and triglyceride levels, and low fibrinogen. Furthermore, bone marrow examination can reveal the presence of hemophagocytosis. Also, an elevated plasma soluble IL2 receptor level and decreased NK-cell activity are part of the diagnostic criteria for HLH. These tests are available in specialized laboratories. When five of the eight aforementioned diagnostic criteria are present, the diagnosis of HLH can be made [9]. Treatment with high dose dexamethasone, etoposide, and ciclosporin can be life-saving while awaiting hematopoietic stem cell transplantation (HSCT) as a definitive treatment. Several genetic defects underlying familial HLH and lymphoproliferative syndromes are currently known [10], so genetic studies are necessary once the clinical diagnosis has been made.
Apart from HLH, an immune dysregulation syndrome should be considered in children with atypical presentations of autoimmunity, such as autoimmune poly-endocrinopathy and/or enteropathy. In children with autoimmune cytopenia, generalized lymphadenopathy (most prominent in the head and neck region), and splenomegaly, an autoimmune lymphoproliferative syndrome (ALPS) has to be considered. The determination of lymphocyte subpopulations frequently shows an increased proportion of CD4−CD8− double negative T-cells in these patients. ALPS is a disorder of the mediators of lymphocyte apoptosis, of which Fas (CD95) is most often affected. Diagnosis can be made by functional analysis of Fas expression and sequence analysis of the corresponding gene.
![]()
Disorders of granulocyte number or function
Recurrent non-superficial pyogenic infections and recurrent ENT and airway infections can both point towards a granulocyte disorder. A third, much rarer presentation consists of unusual (opportunistic) infections with Aspergillus species or other fungi. Congenital neutropenia is a granulocyte disorder which can be easily identified by a full blood count with differential. In case of neutropenia in the first years of life, the differential diagnosis of benign neutropenia of infancy or autoimmune neutropenia has to be explored because this disease is more common than congenital neutropenia [6]. The presence of auto-antibodies against granulocytes supports this diagnosis. The detection of intermittent episodes of neutropenia suggests cyclic neutropenia. In that case, the determination of the leukocyte differential count has to be performed repeatedly to reveal the cyclic pattern (Table 3). Disorders of granulocyte function should be considered when granulocyte counts are not reduced; the diagnosis can be explored by performing granulocyte function tests.
Defects of innate immunity
Over the last couple of years, several defects in innate immunity have been discovered representing a new group of PIDs characterized by defects in pathogen recognition receptor signaling (e.g., IRAK-4 deficiency), predisposing these patients to pyogenic infections [14] and recurrent ENT and airway infections, mainly in the first decade of life. If there is no evidence for other PIDs such as antibody deficiency or granulocyte disorders in patients with persistent or recurrent severe bacterial infections, it is advisable to explore the possibility of a defect in innate immunity.
Autoinflammatory disorders
Children with autoinflammatory disorders are frequently considered to have recurrent infections because of their febrile episodes, which are characteristically periodic. But these patients do not have an increased susceptibility to infections. Familial Mediterranean Fever (FMF) is by far the most common and is mainly found in populations from the eastern Mediterranean area. Apart from periodic fever, the clinical manifestations consist of abdominal pain secondary to serositis, often misdiagnosed as appendicitis, and acute (mono)arthritis. There is a marked inflammatory response, reflected in a high C-reactive protein level and erythrocyte sedimentation rate. FMF is caused by autosomal recessive mutations in the MEFV gene, coding for pyrin, which is an essential modulator of the inflammatory response. An important long-term complication is renal failure, which can be prevented by prophylactic colchicin treatment. Much rarer autoinflammatory syndromes are tumor necrosis factor receptor-associated periodic syndromes (TRAPS), mevalonate kinase deficiency or hyper IgD syndrome, and the cryopyrin-associated periodic syndromes. For diagnosis and treatment of these disorders, we refer to a recent review [19].
Complement deficiencies
Recurrent meningococcal infections (meningitis/sepsis) are very suggestive of deficiencies of the terminal components of the complement system (C5–C9) and warrant screening of the classical (CH50) and alternative (AP50) complement pathways. If these screening tests are abnormal, analysis of the individual components of the complement system will yield the exact diagnosis. A deficiency of C3, the major opsonin, is associated with recurrent pyogenic infections with encapsulated bacteria. Although complement deficiency increases the host’s susceptibility to respiratory tract infections because of impaired opsonophagocytosis of encapsulated bacteria, a complement deficiency is seldom diagnosed in children with recurrent ENT and airway infections. The main reason for this is the rarity of complement deficiencies compared to antibody deficiencies and granulocyte disorders [7]. Some complement deficiencies do not result in increased susceptibility to infections but to other diseases; a deficiency of complement regulatory proteins factor H, I, and MCP account for approximately 50% of the cases of atypical hemolytic uremic syndrome, whereas a deficiency of the early components of the classical pathway (C1, C2, C4) predispose children to systemic lupus erythematodes. A deficiency of mannose binding lectin, a component of the lectin pathway of the complement cascade, is not considered to be a PID because it often occurs in healthy individuals [9].
Treatment and prognosis
Because infections are the main problem in PIDs, preventing them is the hallmark of treatment. How this is achieved depends on the underlying condition. Vigorous antibiotic treatment of bacterial infections is important. Children with milder antibody deficiencies like specific antibody deficiency may do very well on antibiotic prophylaxis, but it is important to remain vigilant for lung and ear damage which may develop very slowly but irreversibly nonetheless. For more severe forms of antibody deficiency immunoglobulin substitution, administered either subcutaneously or intravenously, is the treatment of choice. Close surveillance is necessary in children who use it. Immunoglobulin substitution reduces the frequency of pneumonia in antibody-deficient patients [2], but cannot prevent pulmonary complications in all patients. Severe forms of PID can generally only be treated by HSCT, which is performed in selected highly specialized centers only. Gene therapy becomes increasingly available for severe forms of PIDs [1], like some forms of SCID. For patients with congenital neutropenia, regular subcutaneous treatment with recombinant granulocyte-colony stimulating factor (G-CSF) is able to restore granulocyte numbers to near normal levels in most patients [17].
The fate of children with PID rests on three pillars: (1) timely recognition, (2) adequate therapy and surveillance, and (3) the nature of the underlying disease. The last item cannot be changed. The first is the task of the pediatrician who encounters the child for the first time, and the second a combined task of the general pediatrician and pediatric immunologist who do the follow-up. With appropriate care, the prognosis of SCID has changed from invariably fatal into >90% survival when HSCT with an HLA-matched donor is performed in time [8]. Immunoglobulin substitution has changed the clinical course of children with agammaglobulinemia dramatically, as has recombinant G-CSF administration for children with congenital neutropenia. The challenge for the future is to achieve an optimal quality of life and increased life span for all children with PID. In this respect, the general pediatrician plays a crucial role: being vigilant and inquisitive, he/she will be able to recognize these patients in time, which is a critical step towards achieving this goal.
Acknowledgments
Conflicts of interest
None to be declared by all authors.
Open Access
This article is distributed under the terms of the Creative Commons Attribution Noncommercial License which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
References
- 1.Aiuti A, Roncarolo MG. Ten years of gene therapy for primary immune deficiencies. Hematology Am Soc Hematol Educ Program. 2009;2009:682–689. doi: 10.1182/asheducation-2009.1.682. [DOI] [PubMed] [Google Scholar]
- 2.Busse PJ, Razvi S, Cunningham-Rundles C. Efficacy of intravenous immunoglobulin in the prevention of pneumonia in patients with common variable immunodeficiency. J Allergy Clin Immunol. 2002;109:1001–1004. doi: 10.1067/mai.2002.124999. [DOI] [PubMed] [Google Scholar]
- 3.Comans-Bitter WM, de Groot R, van den Beemd R, et al. Immunophenotyping of blood lymphocytes in childhood. Reference values for lymphocyte subpopulations. J Pediatr. 1997;130:388–393. doi: 10.1016/S0022-3476(97)70200-2. [DOI] [PubMed] [Google Scholar]
- 4.Cunningham-Rundles C, Bodian C. Common variable immunodeficiency: clinical and immunological features of 248 patients. Clin Immunol. 1999;92:34–48. doi: 10.1006/clim.1999.4725. [DOI] [PubMed] [Google Scholar]
- 5.de Vries E, Clinical Working Party of the European Society for Immunodeficiencies Patient-centred screening for primary immunodeficiency: a multi-stage diagnostic protocol designed for non-immunologists. Clin Exp Immunol. 2006;145:204–214. doi: 10.1111/j.1365-2249.2006.03138.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Donadieu J. [Evaluation of neutropenia in children] Evaluation d’une neutropenie chez l’enfant. Arch Pediatr. 2003;10(Suppl 4):521s–523s. doi: 10.1016/S0929-693X(03)90061-3. [DOI] [PubMed] [Google Scholar]
- 7.Gathmann B, Grimbacher B, Beaute J, et al. The European internet-based patient and research database for primary immunodeficiencies: results 2006–2008. Clin Exp Immunol. 2009;157(Suppl 1):3–11. doi: 10.1111/j.1365-2249.2009.03954.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Grunebaum E, Mazzolari E, Porta F, et al. Bone marrow transplantation for severe combined immune deficiency. JAMA. 2006;295:508–518. doi: 10.1001/jama.295.5.508. [DOI] [PubMed] [Google Scholar]
- 9.Henter JI, Horne A, Arico M, et al. HLH-2004: diagnostic and therapeutic guidelines for hemophagocytic lymphohistiocytosis. Pediatr Blood Cancer. 2007;48:124–131. doi: 10.1002/pbc.21039. [DOI] [PubMed] [Google Scholar]
- 10.International Union of Immunological Societies Expert Committee on Primary Immunodeficiencies. Notarangelo LD, Fischer A, Geha RS, et al. Primary immunodeficiencies: 2009 update. J Allergy Clin Immunol. 2009;124:1161–1178. doi: 10.1016/j.jaci.2009.10.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Janka GE. Familial and acquired hemophagocytic lymphohistiocytosis. Eur J Pediatr. 2007;166:95–109. doi: 10.1007/s00431-006-0258-1. [DOI] [PubMed] [Google Scholar]
- 12.Janka GE, Schneider EM. Modern management of children with haemophagocytic lymphohistiocytosis. Br J Haematol. 2004;124:4–14. doi: 10.1046/j.1365-2141.2003.04726.x. [DOI] [PubMed] [Google Scholar]
- 13.Lipstein EA, Vorono S, Browning MF, et al. Systematic evidence review of newborn screening and treatment of severe combined immunodeficiency. Pediatrics. 2010;125:e1226–e1235. doi: 10.1542/peds.2009-1567. [DOI] [PubMed] [Google Scholar]
- 14.Picard C, Puel A, Bonnet M, et al. Pyogenic bacterial infections in humans with IRAK-4 deficiency. Science. 2003;299:2076–2079. doi: 10.1126/science.1081902. [DOI] [PubMed] [Google Scholar]
- 15.Quinti I, Soresina A, Spadaro G, et al. Long-term follow-up and outcome of a large cohort of patients with common variable immunodeficiency. J Clin Immunol. 2007;27:308–316. doi: 10.1007/s10875-007-9075-1. [DOI] [PubMed] [Google Scholar]
- 16.van der Burg M, van Zelm MC, van Dongen JJ. Molecular diagnostics of primary immunodeficiencies: benefits and future challenges. Adv Exp Med Biol. 2009;634:231–241. doi: 10.1007/978-0-387-79838-7_19. [DOI] [PubMed] [Google Scholar]
- 17.Welte K, Zeidler C, Reiter A, Riehm H. Effects of granulocyte colony-stimulating factor in children with severe neutropenia. Acta Haematol Pol. 1994;25:155–162. [PubMed] [Google Scholar]
- 18.Winkelstein JA, Marino MC, Lederman HM, et al. X-linked agammaglobulinemia: report on a United States registry of 201 patients. Medicine (Baltimore) 2006;85:193–202. doi: 10.1097/01.md.0000229482.27398.ad. [DOI] [PubMed] [Google Scholar]
- 19.Yao Q, Furst DE. Autoinflammatory diseases: an update of clinical and genetic aspects. Rheumatology (Oxford) 2008;47:946–951. doi: 10.1093/rheumatology/ken118. [DOI] [PubMed] [Google Scholar]