Abstract
Objectives
Evidence of surgical transmission of sporadic Creutzfeldt–Jakob disease (sCJD) remains debatable in part due to misclassification of exposure levels. In a registry-based case–control study, the authors applied a risk-based classification of surgical interventions to determine the association between a history of surgery and sCJD.
Design
Case–control study, allowing for detailed analysis according to time since exposure.
Setting
National populations of Denmark and Sweden.
Participants
From national registries of Denmark and Sweden, the authors included 167 definite and probable sCJD cases with onset during the period 1987–2003, 835 age-, sex- and residence-matched controls and 2224 unmatched. Surgical procedures were categorised by anatomical structure and presumed risk of transmission level. The authors used logistic regression to determine the odds ratio (OR) for sCJD by surgical interventions in specified time-windows before disease-onset.
Results
From comparisons with matched controls, procedures involving retina and optic nerve were associated with an increased risk at a latency of ≥1 year OR (95% CI) 5.53 (1.08 to 28.0). At latencies of 10 to 19 years, interventions on peripheral nerves 4.41 (1.17 to 16.6) and skeletal muscle 1.58 (1.01 to 2.48) were directly associated. Interventions on blood vessels 4.54 (1.01 to 20.0), peritoneum 2.38 (1.14 to 4.96) and skeletal muscle 2.04 (1.06 to 3.92), interventions conducted by vaginal approach 2.26 (1.14 to 4.47) and a pooled category of lower-risk procedures 2.81 (1.62 to 4.88) had an increased risk after ≥20 years. Similar results were found when comparing with unmatched controls.
Interpretation
This observation is in concordance with animal models of prion neuroinvasion and is likely to represent a causal relation of surgery with a non-negligible proportion of sCJD cases.
Keywords: Creutzfeldt–Jakob disease, epidemiology, aetiology, safety, surgery, prion
Introduction
Creutzfeldt–Jakob disease (CJD) is a rare, fatal neurodegenerative disease characterised by deposition of a pathological isoform of the normal cellular prion protein (PrPC). CJD exists in various forms, namely, genetic, caused by mutations in the gene encoding PrPC, acquired (variant and iatrogenic) and sporadic. Most cases are classified as sporadic (sCJD). Twelve case–control studies1–12 and one meta-analysis13 have examined surgical transmission of sCJD. The outcomes have been partly diverging due to methodological constraints, including problems in selection of control subjects and in particular exposure assessment.9 14 Most studies have relied on surrogate informants and medical records for surgical histories, inevitably prone to recall- and selection-bias. A recent register-based case–control study,9 which by design had a less biased assessment of surgical exposures,15 corroborated that a proportion of sCJD may be transmitted by surgery following long incubation periods (20 years or more). However, a limitation shared by all the above-mentioned studies could be misclassification bias induced by the use of standard categories of surgical procedures (SP).
Case–control studies focussing on surgical transmission of sCJD have been conducted using convenient anatomical references for classification of surgical interventions1–8 10–12 or national body-system classifications of SP.9 However, such a standard classification of surgical exposures may lead to misclassification. For example, in many ophthalmic and neurosurgical procedures, surgical instruments are not likely to encounter potentially high-risk infective tissue.16 In a Swedish dataset, only 27% of ophthalmological SP were included in a risk category in which contact with retina and optic nerve was explicit or likely.17 As neither infectivity, nor cellular prion-protein expression patterns, nor the routes of experimentally transmitted infections fit broad anatomic SP classifications or groups used in prior research, we created a risk-based classification system for surgical exposures.17 Sensitivity analysis corroborated that case–control studies in this field may have been subject to misclassification bias due to the use of SP classifications that were insufficiently specific or sensitive to distinguish between low-risk and high-risk interventions for sCJD transmission.17
The aim of the present study was to apply the risk-based classification system17 to determine the association between surgery and sCJD and thereby quantify effects potentially masked in prior case–control studies.1–12
Methods
Study design and selection of cases and controls
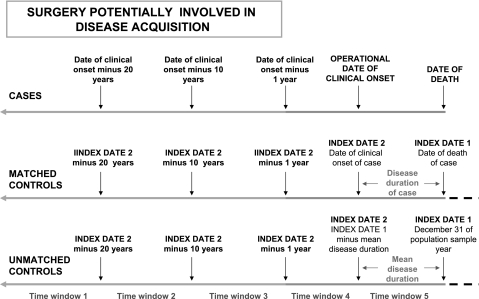
The study was designed9 as a case–control study including 167 probable or definite sCJD cases fulfilling established EUROCJD diagnostic criteria,18 with clinical onset during the period 1987–2003, and resident in Denmark or Sweden. Two sets of randomly selected population controls were included, that is, 835 matched (MC, 5:1 by gender, year, month of birth, and municipality of residence at death of the corresponding case) and 2224 unmatched controls (UMC, sampled from the annual, resident, national study populations aged 40 years and over). For latency analysis purposes, three time windows (TWs) were adopted as described.9 These were based on two operational dates, of death and of clinical onset for cases, and corresponding index dates, denoted index dates 1 and 2 (ID-1 and ID-2), for controls (figure 1).9 Relevant parameters for our design of TWs 1,2 and 3 were onset of surgical procedure registration at hospital discharges in the early 1970s, reported length of latency time in iatrogenic CJD due to dura mater grafts, uncertainties in symptoms onset in sCJD and the study size.
Figure 1.
Schematic illustration of the study design and methodological procedure for life-time-interval definition of the registered surgical history of cases and controls. Time windows included in the present study were those covering surgical history >1 year prior to clinical onset of cases or index-date-2 of controls, namely, windows 1, 2 and 3. Modified from Mahillo-Fernandez et al,9 where details of individuals' life-time references are given.
Exposure ascertainment
The surgical history was obtained from national registers, and assigned, blind to subjects' case or control status, to one of the three TWs, and, where required to all three pooled TWs covering registered hospital stay up to 1 year before clinical onset or ID-2.
For cases and controls, data on past hospital discharges (diagnoses, SP codes, and dates of admission and discharge) were obtained from the National Hospital Discharge Registers in Sweden and Denmark. Personal identifiers and case-status indication were removed before analysing the data with respect to exposure to SP. Reported SP codes were identified and categorised according to Swedish, Danish and Nordic (NOMESCO-NCSP) SP classifications.19–21 Codes describing procedures that were not properly surgical, for example, delivery, and non-specific codes, for example ‘investigative procedures connected with surgery’, were omitted. The 5990 remaining SP were categorised into two major groups, namely: ‘main surgical procedures’, and ‘subsidiary procedures’, a heterogeneous category that included minor surgery (punctures, needle aspiration or biopsy, superficial incision), other non-surgical, potentially invasive procedures, such as transluminal endoscopies (with or without biopsy) and, in a few instances in Denmark, blood transfusion. The selected surgical experience of cases and controls corresponded to 1445 distinct SP codes and 5990 SP associated with 3876 registered discharges during TWs 1–3, that is, dating one or more years before the operational disease onset or ID-2 used in the reported study.9
SP reclassification by risk level
A total of 1445 unrepeated SP codes were decoded, and their 5990 discharge dates were reclassified blindly to individual outcomes according to the reported method.17 The following two attributes were assigned to each SP: (a) probable use of non-disposable instruments involved; and (b) list of up to four (of the 24 reported) tissue types or anatomical structures with the highest assigned risk level most likely contacted by such instruments.22 In total, 4813 repeated or not SP codes with different discharge dates were reclassified into six putative categories of CJD-acquisition risk level16: high risk; diluted high risk; lower risk; diluted lower risk; lowest risk; no risk (when deemed to have been conducted with disposable instruments). Furthermore, 1177 SP were not reclassified, including 865 transluminal endoscopies and 198 minor surgical procedures and blood transfusions. Endoscopies were not reclassified because early registration periods did not discriminate between procedures that were and those that were not associated with invasive procedures such as biopsies.
SP reclassification by tissue/structure
Surgical exposure was defined as tissue/structure-specific by possible contact of non-disposable instruments with up to four assigned tissues/structures.17 The above-mentioned 4813 SP generated up to four of 24 binary categorical variables for 24 different types of tissue or anatomical structure.22
Individual exposure assignment by potential entry site
An individual was assigned to one out of three mutually exclusive exposure categories per window (see figure 2A for examples), namely: exposed to tissue/structure under study; exposed to other tissues/structures; and unexposed.
An individual was assigned as exposed to a specific tissue/structure under study when at least one discharge associated with a SP involving such tissue/structure was found at a date within the limits of a TW.
An individual was deemed as exposed to a tissue/structure other than that under study, during any given TW, when at least one discharge was associated with a tissue/structure other than that under study. Persons solely exposed to no risk and not-reclassified SP were included here.
Finally, unexposed individuals were defined as those who had never been discharged or undergone a discharge associated with any ‘reclassified’ or ‘not-reclassified’ SP during the TW under study.
Figure 2.
(A) Example of individual categories of exposure by tissue/structure under study when focusing on retina and optic nerve, at a specific window, for three different individuals. (B) Surgical procedure risk categories after reclassification, and corresponding individual categories of exposure to surgery.
Individual exposure assignment by putative risk level
Individual levels of exposure were collapsed to five categories, figure 2B. These were: (1) high risk; (2) lower risk; (3) lowest risk; (4) no risk or not-reclassified procedures; and (5) unexposed. The hypothetical risk level of surgical exposure assigned to a given individual during a specific TW was the highest SP risk level found to be associated with the hospital discharges registered during that TW. As done in the preceding report, an individual was classified as exposed to a specific risk category of surgery in a specific TW when at least one discharge associated with at least one code of such surgery had taken place at a date within the limits of the individually designated TW. Multiple exposures to a specific category were determined by the number of surgical discharges with one or more SP codes reclassified in that same category.
Data analysis
We determined the risk of sCJD by presumed risk level and by contacted tissue/structure. Statistical methods with regard to design of variables, choice of reference groups, latency intervals, multivariate models and procedures for calculation of 95% CIs (CI) replicate those used in the preceding analysis.9 Conditional logistic regression was used for comparisons with MCs, and logistic regression with adjustment for age, sex and country of residence at ID-1, for comparisons with UMCs. Exposures during single TWs, 1, 2 and 3, and one combined TW, 1–3, that is, predating onset/ID-2 by ≥1 year, were included in main and complementary analyses. When an association was based on a meaningful number of exposed cases, we explored the presence of a dose–response effect quantifying the linear increase in OR for the number of surgical discharges. We assessed potential confounding by associated tissue/structure types in tissue/structure-specific models, by including, as independent variables, the tissue/structure present in at least 25% of the discharges associated with the repeated or unrepeated tissue/structure-specific SP under study. Since only comparisons related to single one-at-a-time hypotheses were planned, we followed Rothman, Greenland and Last, recommendations to refrain from use of conventional procedures for widening the confidence intervals.23
The study was formally notified to the Danish Data Protection Agency (record No 2003-41-3104) and approved by the Karolinska Institute Ethics Committee (South; report No 452/02).
Results
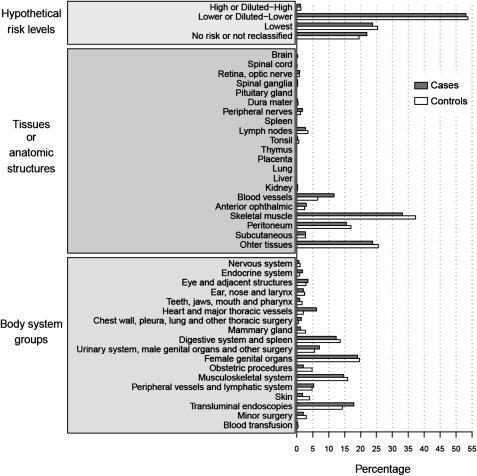
Figure 3 shows, separately for cases and controls, the results of the reclassification of the 5990 selected SP. Surgery on brain, retina, spinal cord and pituitary gland or dura mater accounted for approximately 2% of reclassified procedures.
Figure 3.
Percentage distributions of 5990 selected surgical procedure codes associated with surgical discharges during TWs 1–3, either classified by body-system or reclassified by hypothetical transmission risk level (n=5990) or contacted tissue/structure (n=4813). Three surgical procedure categories yielding Zero values (trigeminal ganglia, olfactory mucosa and cerebrospinal fluid), are not represented. Added percentages by tissue or anatomic structure exceed 100%.
In the analyses of risk factors for sCJD, high-risk surgery among cases was almost absent in all TWs, which made statistical inference less meaningful for these SPs (table 1). However, lower-risk surgery carried out more than 20 years before disease-onset or ID-2 was associated with an increased risk of sCJD (OR for MCs (ORMC) 2.81 and an OR for UMCs (ORUMC) of 2.54). Furthermore, for lower-risk procedures there was a dose–response relation with a linear increase by discharge (ORMC 1.34 and ORUMC 1.33). In addition, point estimates of the OR increased by latency period for lower-risk surgery, and those for latencies 10 years or longer decreased moving from high risk through lower risk to lowest risk.
Table 1.
Associations for surgery by risk level for specific periods predating onset or ID-2
| Putative risk categories after reclassification | ||||||||||
| Unexposed* | High risk | Lower risk | Lowest risk | No risk or not reclassified | ||||||
| Time window | Subject | n (%) | n (%) | OR (95% CI) | n (%) | OR (95% CI) | n (%) | OR (95% CI) | n (%) | OR (95% CI) |
| Time window 1 (≥20 years) | Cases | 134 (80.2) | 0 (0.0) | 25 (15.0) | 7 (4.2) | 1 (0.6) | ||||
| MC | 745 (89.2) | 0 (0.0) | – | 58 (6.9) | 2.81 (1.62 to 4.88)† | 29 (3.5) | 1.70 (0.71 to 4.04) | 3 (0.4) | 2.09 (0.18 to 23.8) | |
| UMC | 1985 (89.3) | 1 (0.0) | – | 162 (7.3) | 2.54 (1.59 to 4.06)‡ | 66 (3.0) | 1.67 (0.72 to 3.86) | 10 (0.4) | 1.35 (0.14 to 12.9) | |
| Time window 2 (10–19 years) | Cases | 110 (65.9) | 2 (1.2) | 44 (26.3) | 10 (6.0) | 1 (0.6) | ||||
| MC | 603 (72.2) | 6 (0.7) | 1.72 (0.34 to 8.59) | 167 (20.0) | 1.49 (1.00 to 2.22) | 48 (5.7) | 1.16 (0.59 to 2.28) | 11 (1.3) | 0.51 (0.07 to 3.96) | |
| UMC | 1569 (70.5) | 10 (0.4) | 2.53 (0.57 to 11.3) | 474 (21.3) | 1.45 (0.99 to 2.12) | 128 (5.8) | 1.20 (0.61 to 2.38) | 43 (1.9) | 0.30 (0.04 to 2.24) | |
| Time window 3 (1–9 years) | Cases | 116 (69.5) | 2 (1.2) | 33 (19.8) | 9 (5.4) | 7 (4.2) | ||||
| MC | 565 (67.7) | 8 (1.0) | 1.22 (0.26 to 5.77 | 192 (23.0) | 0.84 (0.55 to 1.29) | 42 (5.0) | 1.04 (0.50 to 2.18) | 28 (3.4) | 1.22 (0.50 to 2.94) | |
| UMC | 1526 (68.6) | 16 (0.7) | 1.41 (0.33 to 6.10) | 513 (23.1) | 0.74 (0.49 to 1.11) | 115 (5.2) | 0.96 (0.47 to 1.96) | 54 (2.4) | 1.59 (0.69 to 3.66) | |
| All time TWs (≥1 year) | Cases | 72 (43.1) | 4 (2.4) | 81 (48.5) | 7 (4.2) | 3 (1.8) | ||||
| MC | 399 (47.8) | 13 (1.6) | 1.67 (0.50 to 6.51) | 333 (39.9) | 1.35 (0.96 to 1.91) | 68 (8.1) | 0.57 (0.25 to 1.30) | 22 (2.6) | 0.76 (0.21 to 2.74) | |
| UMC | 1056 (47.5) | 27 (1.2) | 1.94 (0.67 to 5.58 | 907 (40.8) | 1.28 (0.91 to 1.79) | 184 (8.3) | 0.56 (0.25 to 1.24) | 50 (2.2) | 0.76 (0.23 to 2.54) | |
OR for comparisons with unmatched controls (UMC) was adjusted by age, sex and country.
Reference category. No registered surgery.
Linear increase per discharge: OR=1.34, 95% CI=1.07 to 1.69.
Linear increase per discharge: OR=1.33, 95% CI =1.09 to 1.61.
MC, matched controls.
For surgery classified by the tissue/structure involved, results from comparisons with matched and unmatched control groups were fairly similar. Findings for surgery conducted at any time throughout the entire study period, TWs 1–3, were negative (table 2), except when instruments contacted retina and optic nerve being in such case associated with an increased risk of sCJD ORMC (95% CI) 5.53 (1.08 to 28.0) (based on three exposed cases and compared with matched controls only). However, 16 of the 23 remaining comparisons yielded statistically non-significant OR point values above the unit. No significant differences were found at 1–9 years before onset (data not shown). For surgery conducted 10–19 years before onset, TW-2 (table 3), point estimates generally exceeded 1, being statistically significantly higher in both comparisons those for surgery in contact with peripheral nerves and, when compared with MCs only, those for surgery on skeletal muscle. Several significant differences were found at TW-1, ≥20 years (table 4), for several categories, including surgery involving blood vessels, peritoneum, skeletal muscle and the group of other tissues.
Table 2.
Associations for surgery by tissue/structure contacted 1 or more years before onset or ID-2
| Unexposed* | Tissue/structure under study | Other surgery† | |||
| Tissue/structure | Subject | n (%) | n (%) | OR (95% CI) | n (%) |
| Retina, optic nerve | Case | 72 (43.1) | 3 (1.8) | 92 (55.1) | |
| MC | 399 (47.8) | 3 (0.4) | 5.53 (1.10 to 27.79) | 433 (51.9) | |
| UMC | 1056 (47.5) | 14 (0.6) | 2.96 (0.66 to 9.62) | 1154 (51.9) | |
| Spinal ganglia | Case | 72 (43.1) | 1 (0.6) | 94 (56.3) | |
| MC | 399 (47.8) | 3 (0.4) | 1.77 (0.18 to 17.04) | 433 (51.9) | |
| UMC | 1056 (47.5) | 8 (0.4) | 1.66 (0.09 to 9.74) | 1160 (52.2) | |
| Dura mater | Case | 72 (43.1) | 1 (0.6) | 94 (56.3) | |
| MC | 399 (47.8) | 10 (1.2) | 0.53 (0.07 to 4.27) | 426 (51.0) | |
| UMC | 1056 (47.5) | 11 (0.5) | 1.19 (0.06 to 6.49) | 1157 (52.0) | |
| Peripheral nerves | Case | 72 (43.1) | 5 (3.0) | 90 (53.9) | |
| MC | 399 (47.8) | 13 (1.6) | 2.10 (0.74 to 6.00) | 423 (50.7) | |
| UMC | 1056 (47.5) | 39 (1.8) | 1.76 (0.58 to 4.31) | 1129 (50.8) | |
| Lymph nodes | Case | 72 (43.1) | 9 (5.4) | 86 (51.5) | |
| MC | 399 (47.8) | 52 (6.2) | 0.97 (0.46 to 2.07) | 384 (46.0) | |
| UMC | 1056 (47.5) | 122 (5.5) | 0.92 (0.41 to 1.81) | 1046 (47.0) | |
| Tonsil | Case | 72 (43.1) | 1 (0.6) | 94 (56.3) | |
| MC | 399 (47.8) | 8 (1.0) | 0.69 (0.09 to 5.60) | 428 (51.3) | |
| UMC | 1056 (47.5) | 21 (0.9) | 0.99 (0.05 to 4.97) | 1147 (51.6) | |
| Kidney | Case | 72 (43.1) | 1 (0.6) | 94 (56.3) | |
| MC | 399 (47.8) | 6 (0.7) | 0.92 (0.11 to 7.72) | 430 (51.5) | |
| UMC | 1056 (47.5) | 5 (0.2) | 2.58 (0.13 to 16.92) | 1163 (52.3) | |
| Blood vessels | Case | 72 (43.1) | 15 (9.0) | 80 (47.9) | |
| MC | 399 (47.8) | 56 (6.7) | 1.51 (0.80-2.85) | 380 (45.5) | |
| UMC | 1056 (47.5) | 109 (4.9) | 1.66 (0.88 to 2.97) | 1059 (47.6) | |
| Anterior olphtalmic | Case | 72 (43.1) | 7 (4.2) | 88 (52.7) | |
| MC | 399 (47.8) | 19 (2.3) | 2.10 (0.83 to 5.32) | 417 (49.9) | |
| UMC | 1056 (47.5) | 52 (2.3) | 1.60 (0.63 to 3.55) | 1116 (50.2) | |
| Skeletal muscle | Case | 72 (43.1) | 63 (37.7) | 32 (19.2) | |
| MC | 399 (47.8) | 257 (30.8) | 1.38 (0.94 to 2.02) | 179 (21.4) | |
| UMC | 1056 (47.5) | 714 (32.1) | 1.33 (0.92 to 1.91) | 454 (20.4) | |
| Peritoneum | Case | 72 (43.1) | 34 (20.4) | 61 (36.5) | |
| MC | 399 (47.8) | 136 (16.3) | 1.44 (0.89 to 2.33) | 300 (35.9) | |
| UMC | 1056 (47.5) | 389 (17.5) | 1.32 (0.85 to 2.04) | 779 (35.0) | |
| Subcutaneous | Case | 72 (43.1) | 6 (3.6) | 89 (53.3) | |
| MC | 399 (47.8) | 26 (3.1) | 1.28 (0.51 to 3.24) | 410 (49.1) | |
| UMC | 1056 (47.5) | 88 (4.0) | 0.89 (0.33 to 1.96) | 1080 (48.6) | |
| Other tissues | Case | 72 (43.1) | 43 (25.7) | 52 (31.1) | |
| MC | 399 (47.8) | 198 (23.7) | 1.22 (0.79 to 1.88) | 238 (28.5) | |
| UMC | 1056 (47.5) | 533 (24.0) | 1.17 (0.78 to 1.74) | 635 (28.6) | |
OR for comparisons with unmatched controls (UMC) was adjusted by age, sex and country.
Reference category. No registered surgery.
Reclassified procedures involving tissues/structures different from that on study only.
MC, matched controls.
Table 3.
Associations for surgery by tissue/structure contacted 10–19 years before onset or ID-2
| Unexposed* | Tissue/structure under study | Other surgery† | |||
| Tissue/structure | Subject | n (%) | n (%) | OR (95% CI) | n (%) |
| Retina, optic nerve | Case | 110 (65.9) | 2 (1.2) | 55 (32.9) | |
| MC | 603 (72.2) | 1 (0.1) | 10.7 (0.91 to 124.9) | 231 (27.7) | |
| UMC | 1569 (70.5) | 6 (0.3) | 3.97 (0.83 to 18.9) | 649 (29.2) | |
| Peripheral nerves | Case | 110 (65.9) | 4 (2.4) | 53 (31.7) | |
| MC | 603 (72.2) | 5 (0.6) | 4.41 (1.17 to 16.6) | 227 (27.2) | |
| UMC | 1569 (70.5) | 16 (0.7) | 3.83 (1.24 to 11.8) | 639 (28.7) | |
| Lymph nodes | Case | 110 (65.9) | 6 (3.6) | 51 (30.5) | |
| MC | 603 (72.2) | 18 (2.2) | 1.87 (0.72 to 4.86) | 214 (25.6) | |
| UMC | 1569 (70.5) | 43 (1.9) | 1.82 (0.77 to 4.27) | 612 (27.5) | |
| Kidney | Case | 110 (65.9) | 1 (0.6) | 56 (33.5) | |
| MC | 603 (72.2) | 3 (0.4) | 1.88 (0.19 to 18.5) | 229 (27.4) | |
| UMC | 1569 (70.5) | 0 (0.0) | 655 (29.5) | ||
| Blood vessels | Case | 110 (65.9) | 5 (3.0) | 52 (31.1) | |
| MC | 603 (72.2) | 24 (2.9) | 1.19 (0.44 to 3.23) | 208 (24.9) | |
| UMC | 1569 (70.5) | 50 (2.2) | 1.40 (0.55 to 3.58) | 605 (27.2) | |
| Anterior ophthalmic | Case | 110 (65.9) | 3 (1.8) | 54 (32.3) | |
| MC | 603 (72.2) | 6 (0.7) | 2.74 (0.67 to 11.2) | 226 (27.1) | |
| UMC | 1569 (70.5) | 15 (0.7) | 2.57 (0.70 to 9.42) | 640 (28.8) | |
| Skeletal muscle | Case | 110 (65.9) | 34 (20.4) | 23 (13.8) | |
| MC | 603 (72.2) | 122 (14.6) | 1.58 (1.01 to 2.48) | 110 (13.2) | |
| UMC | 1569 (70.5) | 385 (17.3) | 1.41 (0.92 to 2.15) | 270 (12.1) | |
| Peritoneum | Case | 110 (65.9) | 19 (11.4) | 38 (22.8) | |
| MC | 603 (72.2) | 67 (8.0) | 1.62 (0.91 to 2.89) | 165 (19.8) | |
| UMC | 1569 (70.5) | 190 (8.5) | 1.65 (0.97 to 2.79) | 465 (20.9) | |
| Subcutaneous | Case | 110 (65.9) | 4 (2.4) | 53 (31.7) | |
| MC | 603 (72.2) | 13 (1.6) | 1.73 (0.50 to 5.96) | 219 (26.2) | |
| UMC | 1569 (70.5) | 35 (1.6) | 1.64 (0.57 to 4.70) | 620 (27.9) | |
| Other tissues | Case | 110 (65.9) | 22 (13.2) | 35 (21.0) | |
| MC | 603 (72.2) | 101 (12.1) | 1.22 (0.72 to 2.06) | 131 (15.7) | |
| UMC | 1569 (70.5) | 286 (12.9) | 1.20 (0.74 to 1.96) | 369 (16.6) | |
OR for comparisons with unmatched controls (UMC) was adjusted by age, sex and country.
Reference category. No registered surgery.
Reclassified procedures involving tissues/structures different from that on study only, shown for clarity.
MC, matched controls.
Table 4.
Associations for surgery by tissue/structure contacted, 20 or more years before onset or ID-2
| Unexposed* | Tissue/structure under study | Other surgery† | ||||
| Time window | Tissue/structure | Subject | n (%) | n (%) | OR (95% CI) | n (%) |
| Time window 1 (≥20 years) | Peripheral nerves | Case | 134 (80.2) | 1 (0.6) | 32 (19.2) | |
| MC | 745 (89.2) | 1 (0.1) | 6.27 (0.50 to 78.1) | 89 (10.7) | ||
| UMC | 1985 (89.3) | 7 (0.3) | 2.12 (0.20 to 21.9) | 232 (10.4) | ||
| Lymph nodes | Case | 134 (80.2) | 2 (1.2) | 31 (18.6) | ||
| MC | 745 (89.2) | 6 (0.7) | 2.18 (0.46 to 10.4) | 84 (10.1) | ||
| UMC | 1985 (89.3) | 9 (0.4) | 2.83 (0.62 to 12.9) | 230 (10.3) | ||
| Tonsil | Case | 134 (80.2) | 1 (0.6) | 32 (19.2) | ||
| MC | 745 (89.2) | 2 (0.2) | 3.59 (0.39 to 32.8) | 88 (10.5) | ||
| UMC | 1985 (89.3) | 4 (0.2) | 6.46 (0.72 to 58.3) | 235 (10.6) | ||
| Blood vessels | Case | 134 (80.2) | 3 (1.8) | 30 (18.0) | ||
| MC | 745 (89.2) | 4 (0.5) | 4.54 (1.01 to 20.3) | 86 (10.3) | ||
| UMC | 1985 (89.3) | 10 (0.4) | 4.15 (1.12 to 15.5) | 229 (10.3) | ||
| Skeletal muscle | Case | 134 (80.2) | 14 (8.4) | 19 (11.4) | ||
| MC | 745 (89.2) | 46 (5.5) | 2.04 (1.06 to 3.92) | 44 (5.3) | ||
| UMC | 1985 (89.3) | 125 (5.6) | 1.87 (1.03 to 3.38) | 114 (5.1) | ||
| Peritoneum | Case | 134 (80.2) | 11 (6.6) | 22 (13.2) | ||
| MC | 745 (89.2) | 32 (3.8) | 2.38 (1.14 to 4.96) | 58 (6.9) | ||
| UMC | 1985 (89.3) | 66 (3.0) | 2.48 (1.26 to 4.88) | 173 (7.8) | ||
| Subcutaneous | Case | 134 (80.2) | 1 (0.6) | 32 (19.2) | ||
| MC | 745 (89.2) | 3 (0.4) | 1.98 (0.19 to 20.6) | 87 (10.4) | ||
| UMC | 1985 (89.3) | 14 (0.6) | 1.06 (0.12 to 9.19) | 225 (10.1) | ||
| Other tissues | Case | 134 (80.2) | 16 (9.6) | 17 (10.2) | ||
| MC | 745 (89.2) | 50 (6.0) | 2.26 (1.14 to 4.47) | 40 (4.8) | ||
| UMC | 1985 (89.3) | 109 (4.9) | 2.24 (1.25 to 4.04) | 130 (5.8) | ||
OR for comparisons with unmatched controls (UMC) was adjusted by age, sex and country.
Reference category. No registered surgery.
Reclassified procedures involving tissues/structures different from that on study only. Shown for clarity
MC, matched controls.
When complementary subgroup analyses by alternative TWs were conducted, we observed a statistically significant excess risk for lower-risk surgery performed at least 15 years before onset in both comparisons, and for putatively high-risk surgery performed 5–14 years before onset using UMCs (table 5). Positive findings similar to those yielded by the core analysis were detected for strata by country, sex, alternative study period and age at CJD onset, or for definite cases, during both TW-1 and TW-2 (data not shown).
Table 5.
Complementary analyses by risk level
| Putative risk categories after reclassification | ||||||||||
| Unexposed* | High risk | Lower risk | Lowest risk | No risk or not reclassified | ||||||
| Time window | Subject | n (%) | n (%) | OR (95% CI) | n (%) | OR (95% CI) | n (%) | OR (95% CI) | n (%) | OR (95% CI) |
| Time window 1 (≥15 years) | Cases | 114 (68.3) | 0 (0.0) | 47 (28.1) | 5 (3.0) | 1 (0.6) | ||||
| MC | 642 (76.9) | 2 (0.2) | – | 132 (15.8) | 2.13 (1.39 to 3.25) | 52 (6.2) | 0.59 (0.22 to 1.55) | 7 (0.8) | 0.84 (0.10 to 6.72) | |
| UMC | 1703 (76.6) | 6 (0.3) | – | 378 (17.0) | 2.05 (1.42 to 2.96) | 117 (5.3) | 0.67 (0.26 to 1.72) | 20 (0.9) | 0.80 (0.10 to 6.62) | |
| Time window 2 (5–14 years) | Cases | 117 (70.1) | 3 (1.8) | 34 (20.4) | 7 (4.2) | 6 (3.6) | ||||
| MC | 571 (68.4) | 8 (1.0) | 1.85 (0.49 to 6.96) | 188 (22.5) | 0.88 (0.59 to 1.33) | 48 (5.7) | 0.71 (0.31 to 1.61) | 20 (2.4) | 1.47 (0.57 to 3.79) | |
| UMC | 1512 (68.0) | 11 (0.5) | 3.43 (1.01 to 11.6) | 531 (23.9) | 0.83 (0.56 to 1.24) | 123 (5.5) | 0.76 (0.34 to 1.68) | 47 (2.1) | 1.57 (0.64 to 3.85) | |
| Time window 3 (1–4 years) | Cases | 136 (81.4) | 1 (0.6) | 22 (13.2) | 7 (4.2) | 1 (0.6) | ||||
| MC | 692 (82.9) | 3 (0.4) | 1.68 (0.17 to 16.3) | 104 (12.5) | 1.07 (0.66 to 1.76) | 21 (2.5) | 1.70 (0.72 to 4.01) | 15 (1.8) | 0.32 (0.05 to 1.84) | |
| UMC | 1831 (82.3) | 12 (0.5) | 0.89 (0.12 to 6.67) | 281 (12.6) | 0.89 (0.55 to 1.43) | 59 (2.7) | 1.46 (0.65 to 3.26) | 41 (1.8) | 0.29 (0.04 to 2.07) | |
OR for comparisons with unmatched controls (UMC) was adjusted by age, sex and country.
Reference category. No registered surgery.
MC, matched controls.
We went on to explore which specific operations among cases might have contributed to the excess risk. The highest risk, observed for surgery on the retina during the combined TWs 1–3, was based on two surgical discharges after retinal detachment and one involving electrocoagulation of choroidea and retina dating back 9, 12 and 13 years before clinical onset. Surgery during TW-1 with a lower but significant risk excess included SP on: blood vessels (n=6, corresponding in all cases to veins); peritoneum (n=15, with four and 11 of them being gynaecological and gastrointestinal, respectively); skeletal muscle (n=23, with seven and five of the SP codes being gynaecological/obstetric- and bone/orthopaedic-related, respectively); and ‘other tissues’ (n=28, with the majority of these being gynaecological SP with vaginal approach, for example, uterus curettage, n=12, and interventions on cervix n=9). Surgery during TW-2 on peripheral nerves among cases (n=4) included two finger and toe phalangeal amputations, one acoustic nerve neurinoma excision and one pyloroplasty+vagotomy, and 10 of 33 SP under the ‘skeletal muscle’ heading were gynaecological procedures.
Discussion
The key features of the present study design enabled us to address novel aspects of the potential of surgical transmission of CJD.9 The additional introduction of an aetiological classification, that is unmasking associations hidden by the body-system approach,17 24 revealed a number of statistically significant associations, associations of higher magnitude and new effects with a particular pattern at 10–19 years' latency. Limitations, which in part are discussed elsewhere,9 comprise: the low statistical power for some latencies and exposure categories; missing information on interventions undergone prior to registration or as outpatients; and lack of control of potential confounders such as blood transfusion, overlooked dura mater implants or hospital hygiene level.
The new SP classification system was built in a tissue/structure classification reported in 200522 combining features of the first WHO Classification on Tissue infectivity25 and of experimental efficiency of prion disease transmission to animals when using different routes of inocula administration.26–29 The plausibility of the risk excess of surgery of retina and peripheral nerves seen here might be supported by studies in experimental scrapie (Sc). PrPSc injected into the eye travelling via defined neuroanatomical connections has been demonstrated to be able to reach larger brain regions.30 31 In hamsters, PrPSc spreads along the vagus nerve to the medulla, pons, midbrain, cerebellum and thalamus via neuroanatomical pathways.32 The increasing risk found for SP involving veins, peritoneal cavity and lymph nodes at longer latencies fits proposals on prion neuroinvasion and transport, suggesting that prions first replicate and accumulate in the lymphoreticular system (LRS) (see Aguzzi and Calella33 for a recent review). In addition, it would appear that risk excess and latency are inversely correlated: for surgery of retina, OR 5.53, at mean 11 years; for surgery of peripheral nerves, OR 4.41, at 10–19 years; and for lower-risk SP OR 2.4, at ≥20 years. In summary, our findings might be consistent with proposed biological mechanisms potentially underlying the rapid access to the CNS by direct contact,34 prion uptake through the skin, neuroinvasion from the spleen and spread of prions along peripheral and CNS pathways.33 35
Compared with other studies, the main contribution of the new methodology may be credibility to consistently positive results from large recent studies covering lifetime surgery and pointing to likewise underlying diluting effects.7 8 In a study with negative results, retina surgery was unfortunately not investigated separately from other ophthalmological surgery.12 Findings for lower-risk procedures at >20 years would correspond to a similar risk excess before reclassification for main surgical procedures.9 However, the association with coronary surgery seen in TW-3 when using unmatched controls as well as the body system approach does not have a corresponding finding here. Since the association of coronary surgery with sCJD has been reported for Alzheimer's disease at a similar latency, confounding from vascular risk factors generating both dementia and coronary disease followed by coronary surgery may be proposed as a potential explanation unrelated to prion transmission consistent with absence of findings after reclassification.36
Unrecorded information potentially determining our results might be the length of the pathway to the brain, short in the case of retina and acoustic nerve. An overlooked autologous dura mater graft, implanted during the above-mentioned acoustic neurinoma intervention, was excluded by direct perusal of the surgeon's report, issued in 1977, by an author, HL, who excluded an accidentally transmitted CJD by dura mater implant. Improved cleaning of instruments in recent times may in part explain decreased excess risk with shorter latencies.
Blood transfusion has not been identified as a risk factor for sCJD; however, Riggs et al warn about the weaknesses of case–control studies frequently reporting protective effects.37 Inability to adjust for blood transfusion is a limitation of the study, since it has been estimated that blood transfusion is present in 50% of all major surgical interventions38; blood thus comprises a potential confounder.39 Since it would appear that the excess risk seen here for some tissues, for instance for retina surgery, is difficult to attribute to simultaneous blood transfusion, some of the present results might be consistent with confounded effects of surgical instruments and blood. This view contradicts observations on variant CJD, where transmission by blood has been demonstrated,40–43 but not risk excess for surgery.44 However, differences between sCJD and vCJD or Kuru are so large that inferences should perhaps be inappropriate. Furthermore, the exposures studied might not be independent phenomena representing either a potential entry site for prions or the above-mentioned uncontrolled confounding. For example, cohorting of surgical instruments occurs, and an instrument used once for retina surgery, for example, has in all likelihood been repeatedly used for retina surgery. It is therefore possible that our findings could in part be explained by infectivity determined by tissue remnants adhered to instruments (not controlled for here) rather than by the putative entry site (ie, tissue contacted). Consequently, the 18%9 to 35%7 proportion of sCJD which has been suggested might be causally related to surgery, while in theory consistent with observations from animal models, would be difficult to ascribe to a single biological mechanism based on these data.
The results might be surprising, since identified iatrogenic events related to surgery appear to be very rare. Surveillance since 1993 by 11 countries at the EUROCJD consortium includes data on more than 6000 sCJD cases (http://www.eurocjd.ed.ac.uk/genetic.htm). The number of iatrogenic cases related to surgery are 53 assigned to dura mater, two to corneal implants and nil to neurosurgery. However, routine surveillance data will usually not recognise surgical risk exposures for iatrogenic CJD other than grafts. Reasons to explain this might be: (1) the overwhelming difference in annual cohort size, that is >100 000 surgical in-patients per million in Sweden 2004 (http://192.137.163.40/epcfs/index.asp?modul=ope), versus approximately 200 dura mater grafts per million in the 1990s in Japan45; (2) the comparatively large attrition by low survival of neurosurgical and dura mater grafted cohorts45–47; (3) surveillance encompasses the end of the iCJD epidemic48; (4) large differences in duration of incubation periods, mean 11 years for iCJD by dura mater reduce differences in cumulative risk48; (5) similar genetic susceptibility might be a strong determinant of surgical risk linked or not to grafts, and is shared by iCJD and sCJD as shown by homozygosity at codon 12948 49 but can be interpreted in different ways. CJD surveillance captures epidemiologically compelling evidences required for correct CJD diagnosis; the OR for exposure to cadaveric dura mater for CDJ in Japan50 was 32.5 95% CI (2.6 to infinity). Our three cases with history of retina surgery were first discharged with CJD diagnosis from three different hospitals, at different years, in two countries, and most probably diagnosed by different clinicians. Views for iCJD from surveillance and results of this study are perhaps not so difficult to reconcile when biology, diagnosis, epidemiology and public-health practice51 are simultaneously considered.
The potential applicability of results in prevention is complex. Cautiousness might be recommended for planning of surgical interventions for patients where CJD diagnosis has been considered, and for decontamination and quarantining of such surgical instruments, avoiding reuse during the interval CJD diagnosis has not been excluded. Established instrument-quarantining, -tracking, -cleaning and prion-disinfection policies, which generally target infrequent procedures, such as neurosurgery and ophthalmological, spine and ear surgery,38 52 are based on decontamination of remnants and applied to surgical activity defined by the type of surgeon, that is, by body-system group. Current sterilisation procedures undertaken in hospitals for delicate instrumentation are insufficient to ensure total removal of infectious prion protein, and carriers of infective prions are difficult to detect.52 53 Extension of such measures, after appropriate assessment, to instruments contacting or potentially contacting veins, female genital organs, peritoneal cavity, peripheral nerves and muscle could be a priority. In addition, new decontamination procedures54 may have a wider-than-expected field of application.
To sum up, these results suggest that surgery constitutes a risk factor for sCJD, acting with long incubation periods, and less frequently with shorter latencies when the central- or peripheral nervous system as well as skeletal muscle are implicated. In addition, results are in concordance with animal models of experimental prion transmission through various routes of inoculation that may mimic accidentally transmitted CJD, and might have implications for prevention of CJD spread in medical settings.
Acknowledgments
EUROSURGYCJD group members. Danish team: G Falkenhorst, H Laursen, K Mølbak. Finnish team: J Kovanen. Swedish team: M Cruz, Å Siden. Spanish team: J Almazán, MJ Bleda, M Calero, I Mahillo, P Martínez-Martín, J de Pedro-Cuesta (coordinator), A Rábano. The EUROSURGYCJD group members are grateful: to M Pocchiari, Italy, for contributing to this proposal in respect of the biological plausibility of surgical transmission of prion disorders; to P Sanchez-Juan, Spain, for criticism; and to M Löfdahl (Swedish CJD Surveillance Unit), C-L Spetz, L Forsberg (Socialstyrelsen) and L Caderius (Population Statistics), Sweden, for their help with data collection.
Footnotes
Funding: Funding was obtained from The Research Commission EU, Concerted Action QLRG3-CT-2002-81223, NEUROPRION, and the Spanish RECSP C03-09, CIEN C03-06 and CIBERNED networks.
Competing interests: None.
Ethics approval: Ethics approval was provided by the Danish Data Protection Agency (record No 2003-41-3104) and Karolinska Institute Ethics Committee (South; report No 452/02).
Contributors: JdP-C has full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis. Preliminary results were presented at the EUROCJD/NEUROCJD Public Health EU Meeting, held in Paris on 5 December 2006.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Kondo K, Kuroiwa Y. A case–control study of Creutzfeldt–Jakob disease: association with physical injuries. Ann Neurol 1982;11:377–81 [DOI] [PubMed] [Google Scholar]
- 2.Davanipour Z, Alter M, Sobel E, et al. Creutzfeldt–Jakob disease: possible medical risk factors. Neurology 1985;35:1483–6 [DOI] [PubMed] [Google Scholar]
- 3.Harries-Jones R, Knight RSG, Will RG, et al. Creutzfeldt–Jakob disease in England and Wales, 1980–1984: a case–control study of potential risk factors. J Neurol Neurosurg Psychiatry 1988;51:1113–19 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.van Duijn CM, Delasnerie-Lauprêtre N, Masullo C, et al. Case–control study of risk factors of Creutzfeldt–Jakob disease in Europe during 1993–95. Lancet 1998;351:1081–5 [DOI] [PubMed] [Google Scholar]
- 5.Zerr I, Brandel J-P, Masullo C, et al. European surveillance on Creutzfeldt–Jakob disease: a case–control study for medical risk factors. J Clin Epidemiol 2000;53:747–54 [DOI] [PubMed] [Google Scholar]
- 6.Collins S, Law MG, Fletcher A, et al. Surgical treatment and risk of sporadic Creutzfeldt–Jakob disease: a case–control study. Lancet 1999;353:69. [DOI] [PubMed] [Google Scholar]
- 7.Ward HJT, Everington D, Croes EA, et al. Sporadic Creutzfeldt–Jakob disease and surgery: a case–control study using community controls. Neurology 2002;59:543–8 [DOI] [PubMed] [Google Scholar]
- 8.Ward HJ, Everington D, Cousens SN, et al. Risk factors for sporadic Creutzfeldt–Jakob disease. Ann Neurol 2008;63:347–54 [DOI] [PubMed] [Google Scholar]
- 9.Mahillo-Fernandez I, de Pedro-Cuesta J, Bleda MJ, et al. Surgery and risk of sporadic Creutzfeldt–Jakob disease in Denmark and Sweden: registry-based case–control studies. Neuroepidemiology 2008;31:229–40 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Riegger J, Stoeck K, Amsler L, et al. A case–control study of sporadic Creutzfeldt–Jakob disease in Switzerland: analysis of potential risk factors with regard to an increased CJD incidence in the years 2001-2004. BMC Public Health 2009;9:18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hamaguchi T, Noguchi-Sinohara E, Nozaki I, et al. Medical procedures and risk for sporadic Creutzfeldt–Jakob disease, Japan, 1999-2008. Emerg Infect Dis 2009;15:265–71 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.S-Juan P, Ward HJ, De Silva R, et al. Ophthalmic surgery and Creutzfeldt–Jakob disease. Br J Ophthalmol 2004;88:446–9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Wientjens DPWM, Davanipour Z, Hofman A, et al. Risk factors for Creutzfeldt–Jakob disease: a reanalysis of case–control studies. Neurology 1996;46:1287–91 [DOI] [PubMed] [Google Scholar]
- 14.Barash JA, Johnson BT, Gregorio I. Is surgery a risk factor for Creutzfeldt–Jakob disease? Outcome variation by control choice and exposure assessments. Infect Control Hosp Epidemiol 2008;29:212–18 [DOI] [PubMed] [Google Scholar]
- 15.Ward H, Knight R. Surgery and risk of sporadic Creutzfeldt–Jakob disease. Neuroepidemiology 2008;31:241–2 [DOI] [PubMed] [Google Scholar]
- 16.CJD UK Incidents Panel Management of possible exposure to CJD through medical procedures: a consultation paper. London: Department of Health Publications, 2001:11–27 [Google Scholar]
- 17.de Pedro-Cuesta J, Bleda MJ, Rábano A, et al. Classification of surgical procedures for epidemiologic assessment of sporadic Creutzfeldt–Jakob disease transmission by surgery. Eur J Epidemiology 2006;21:595–604 [DOI] [PubMed] [Google Scholar]
- 18.Zerr I, Pocchiari M, Collins S, et al. Analysis of EEG and CSF 14-3-3 proteins as aids to the diagnosis of Creutzfeldt–Jakob disease. Neurology 2000;55:811–15 [DOI] [PubMed] [Google Scholar]
- 19.Klassifikation av operationer, 6:e upplagan Socialstyrelsen. Norstedts T. Stockholm, 1993.
- 20.Operations og Behandlings-Klassifikation, 3 udgave. Sundhedsstyrelsen, Copenhagen Munksgaard, 1988.
- 21.Nordic Medico Statistical Committee N NOMESCO classification of surgical procedures. Copenhagen: NOTEX, 2003 [Google Scholar]
- 22.Rábano A, de Pedro-Cuesta J, Mølbak K, et al. Tissue classification for the epidemiologic assessment of surgical transmission of sporadic Creutzfeldt–Jakob disease. A proposal on hypothetical risk levels. BMC Public Health 2005;5:9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Rothman KJ, Greenland S, Last TL. Modern epidemiology. 3rd edn Philadelphia, PA: Lippincott Williams & Wilkins, 2008:234–7 [Google Scholar]
- 24.Dosemeci M, Wacholder S, Lubin JH. Does non-differenctial misclassification of exposure always bias a true effect toward the null value? Am J Epidemiol 1990;132:746–8 [DOI] [PubMed] [Google Scholar]
- 25.Health Technology and Pharmaceuticals Cluster W WHO guidelines on transmissible spongiform encephalopathies I relation to biological and pharmaceutical products. WHO/BCT/QSD/03.01,1–26 2003
- 26.Kimberlin RH, Walker CA. Pathogenesis of scrapie (strain 263K) in hamsters infected intracerebrally, intraperitoneally or intraocularly. J Gen Virol 1986;67:255–63 [DOI] [PubMed] [Google Scholar]
- 27.Race R, Oldstone M, Chesebro B. Entry versus blockade of brain infection following oral or intraperitoneal scrapie administration: role of prion protein expression in peripheral nerves and spleen. J Virol 2000;74:828–33 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Bradley R. Animal prion diseases. in prion diseases. In: Collinge J, Palmer MS, eds. Oxford: Oxford University Press, 1997 [Google Scholar]
- 29.Scott JR, Foster JD, Fraser H. Conjunctival instillation of scrapie in mice can produce disease. Vet Microbiol 1993;34:305–9 [DOI] [PubMed] [Google Scholar]
- 30.Fraser H. Neuronal spread of scrapie agent and targeting of lesions within the retino-tectal pathway. Nature 1982;295:149–50 [DOI] [PubMed] [Google Scholar]
- 31.Brandner S, et al. Normal host prion protein (PrPC) is required for scrapie spread within the CNS. Proc Natl Acad Sci USA 1996;93:13148–51 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Beekes M, McBride PA, Baldauf E. Cerebral targeting indicates vagal spread of infection in hamsters fed with scrapie. J Gen Virol 1998;79:601–7 [DOI] [PubMed] [Google Scholar]
- 33.Aguzzi A, Calella M. Prions: Protein aggregation and infectious diseases. Physiol Rev 2009;89:1105–52 [DOI] [PubMed] [Google Scholar]
- 34.Bartz JC, Dejoia C, Tucker T, et al. Extraneural prion neuroinvasion without lymphoreticular system infection. J Virol 2005;79:11858–63 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Kimberlin RH, Hall SM, Walker CA. Pathogenesis of mouse scrapie. Evidence for direct neural spread of infection to the CNS after injection of sciatic nerve. J Neurol Sci 1983;61:315–25 [DOI] [PubMed] [Google Scholar]
- 36.Knopman DS, Petersen RC, Cha RH, et al. Coronary artery bypass grafting is not a risk factor for dementia or Alzheimer disease. Neurology 2005;65:986–90 [DOI] [PubMed] [Google Scholar]
- 37.Riggs JE, Moudgil SS, Hobbs GR. Creutzfeldt–Jakob disease and blood transfusions: a meta-analysis of case–control studies. Mil Med 2001;166:1057–8 [PubMed] [Google Scholar]
- 38.Garske T, Ward HT, Clarke P, et al. Factors determining the potential for onward transmission of variant Creutzfeldt–Jakob disease via surgical instruments. J R Dsoc Interface 2006;3:757–66 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Brown P. Creutzfeldt–Jakob disease: reflections on the risk from blood product therapy. Haemophillia 2007;13(Suppl 5):33–40 [DOI] [PubMed] [Google Scholar]
- 40.Llewelyn CA, Hewitt PE, Knight RS, et al. Possible transmission of variant Creutzfeldt–Jakob disease by blood transfusion. Lancet 2004;363:417–21 [DOI] [PubMed] [Google Scholar]
- 41.Peden AH, Head MW, Ritchie DL, et al. Preclinical vCJD after blood transfusion in a codon 129 heterozygous patient. Lancet 2004;364:527–9 [DOI] [PubMed] [Google Scholar]
- 42.Collinge J. Molecular neurology of prion disease. J Neurol Neurosurg Psychiatry 2005;76:906–19 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Wroe SJ, Pal S, Siddique D, et al. Clinical presentation and pre-mortem diagnosis of variant Creutzfeldt–Jakob disease associated with blood transfusion: a case report. Lancet 2006;368:2061–7 [DOI] [PubMed] [Google Scholar]
- 44.Ward HJ, Everington D, Cousens SN, et al. Risk factors for variant Creutzfeldt–Jakob disease: a case–control study. Ann Neurol 2006;59:111–20 [DOI] [PubMed] [Google Scholar]
- 45.Nakamura Y, Aso E, Yanagawa H. Relative risk of Creutzfeldt–Jakob disease with cadaveric dura transplantation in Japan. Neurology 1999;53:218–20 [DOI] [PubMed] [Google Scholar]
- 46.Martinez-Lage JF, Poza M, Brown P, et al. Enfermedad de Creutzfeldt–Jakob en Neurocirugia: una revisión de riesgos y medidas de prevención. Neurocirugia 1997;8:284–93 [Google Scholar]
- 47.Bird SM, Merrall EL, Ward HJ, et al. Survival and re-operation rates after neurosurgical procedures in Scotland: implications for targeted surveillance of sub-clinical variant Creutzfeldt–Jakob disease. Neuroepidemiology 2009;33:1–11 [DOI] [PubMed] [Google Scholar]
- 48.Brown P, Brandel JP, Preese M, et al. Iatrogenic Creutzfeldt–Jakob disease. The waning of an era. Neurology 2006;67:389–93 [DOI] [PubMed] [Google Scholar]
- 49.Kovács GG, Puopolo M, Ladogana A, et al. Genetic prion disease: the EUROCJD experience. Hum Genet 2005;118:166–74 [DOI] [PubMed] [Google Scholar]
- 50.Nakamura Y, Oki I, Tanihara S, et al. A case–control study of Creutzfeldt–Jakob disease in Japan: transplantation of cadaveric dura mater was a risk factor. J Epidemiol 2000;10:399–402 [DOI] [PubMed] [Google Scholar]
- 51.Lenglet A, Hernández Pezzi G. Comparison of the European Union Disease Surveillance Networks' websites. Euro Surveill 2006;11:ii625. [DOI] [PubMed] [Google Scholar]
- 52.Yan Z, Stitz L, Heeg P, et al. Infectivity of prion protein bound to stainless steel wires: a model for testing decontamination procedures for transmissible spongiform encephalopathies. Infect Control Hosp Epidemiol 2004;25:280–3 [DOI] [PubMed] [Google Scholar]
- 53.Baxter RL, Baxter HC, Campbell GA, et al. Quantitative analysis of residual protein contamination on reprocessed surgical instruments. J Hosp Infect 2006;63:439–44 [DOI] [PubMed] [Google Scholar]
- 54.Lemmer K, Mielke M, Kratzel C, et al. Decontamination of surgical instruments from prions. II. In vivo findings with a model system for testing the removal of scrapie infectivity from steel surfaces. J Gen Virol 2008;89:348–58 [DOI] [PubMed] [Google Scholar]