Abstract
The purpose of the study, conducted in Pennsylvania, USA, was to assess the prospective effect of parental encouragement of physical activity (PA) for weight loss on adolescent girls' concern about weight, Body Mass Index (BMI) and objectively-measured PA. Non-Hispanic White girls (N =177) and their parents were assessed when girls were 9, 11, 13 and 15 years old. At each age, girls' concern about their weight, pubertal development, BMI, and dietary intake were measured along with mothers' and fathers' encouragement of PA for weight loss, modeling of PA, and logistic support for PA. At ages 13 and 15 years, girls' PA was assessed using accelerometry. At age 11, girls' PA was measured using a combination of self-report measures and a standardized assessment of cardiovascular fitness. Parents of obese girls reported the highest encouragement of PA for weight loss; however, girls from all weight categories were exposed to encouragement of PA for weight loss and showed similar age-related increases in parental encouragement. Encouragement of PA for weight loss was prospectively associated with higher concern about weight and higher BMI, independent of pre-existing levels of these constructs and covariates. Encouragement of PA for weight loss was not associated with girls' objectively-measured PA. Parental encouragement of PA for weight loss was therefore not an effective strategy in this sample. Findings are consistent with research on parental child feeding practices, where parental control has been linked with unintended negative dietary and psychosocial outcomes among children.
Keywords: girls, adolescent, USA, obesity, physical activity, parents, family, social support, weightless
A considerable body of research documents the important role that parents play in promoting active lifestyles among children. As outlined in reviews by Gustafson and Rhodes (2006) and Pugliese and Tinsley (2008), children and adolescents are more physically active when their parents are active, encourage them to be active, are active with them, and tell them that being active is good for their health. Parents also facilitate children's physical activity (PA) by taking them to places where they can be active and enrolling them in organized activities and paying the associated fees. One form of parental support that has not been addressed to date is parental encouragement of PA for weight loss. Given that approximately 1 in 3 children in the US are overweight or at risk of overweight (Hedley, Ogden, Johnson, Carroll, Curtin, & Flegal, 2004), it is important to examine the effectiveness of this strategy for promoting PA and reducing children's risk of overweight.
Childhood obesity is recognized as a serious public health problem (Evans, Finkelstein, Kamerow, & Renaud, 2005; Napier, 2006). With regard to the origins of obesity, there is widespread belief that parents are responsible for obesity among children (Evans, et al., 2005). This perspective reflects the strong emphasis in the American culture placed on individual responsibility over one's own lifestyle and that of their children. The willingness to prescribe blame to parents places them in a defensive position and may increase the likelihood that they actively encourage weight loss in their children. Promoting PA for weight loss is a likely strategy in this situation given its known health benefits (U.S. Department of Health and Human Services and Healthier U.S.Gov, 2008). Encouraging children to be active to induce weight loss or retard weight gain may also be a message that is reinforced by health professionals (American Academy of Pediatrics, 2003). Although encouragement of PA for weight loss may be well-intentioned and seemingly justified, there is little information on the potential impact of this message on children's health and well-being. Therefore, this study examines the effect of parental encouragement of PA for weight loss on girls' subsequent concern about weight, objectively-measured PA and BMI.
In the absence of prior research on this topic, the expected effect of parental encouragement of PA for weight loss on child health outcomes can be extrapolated from research on parental child feeding practices. While research in general supports the positive role that parental involvement can play in the treatment of childhood obesity (Golan, 2006), research from non-clinical samples indicates that parenting strategies that promote dieting or restrict access to specific foods have counterproductive effects. For example, parental encouragement of dieting has been linked with increased body concerns among adolescent girls and boys, including increased drive for thinness and increased body dissatisfaction (Wertheim, Martin, Prior, Sanson, & Smart, 2002). Similarly, research indicates that restricting children's access to specific foods to promote weight loss or prevent weight gain is associated with greater consumption of the restricted foods when control is removed (e.g., when parents are not present), negative self-perceptions when eating the target foods, and accelerated weight gain (Birch & Fisher, 2000; Carper, Fisher, & Birch, 2000; Fisher, Mitchell, Smiciklas-Wright, & Birch, 2002; Savage, Fisher, & Birch, 2007). Furthermore, there is evidence that pressuring children to eat specific foods (e.g., vegetables) is linked with decreased consumption of such foods and higher dietary fat intake (Savage, et al., 2007). This research suggests that parental child feeding strategies that are controlling or coercive and which center around children's body weight are linked with negative psychosocial outcomes among children, particularly girls, and further increase their risk of overweight. Extrapolating these findings to PA-related parenting, it is predicted that encouraging girls to be active for the explicit purpose of weight loss will be associated with higher concern about body weight, lower PA, and higher BMI among girls.
In summary, the current study examines the impact of parental encouragement of PA for weight loss on girls' subsequent weight concerns, BMI and PA in a longitudinal sample of girls assessed at ages 9, 11, 13, and 15 years. The objectives of the study are to (1) assess girls' age and weight status as predictors of parental encouragement of PA for weight loss and (2) assess the lagged, prospective effect of encouragement of PA for weight loss on girls' concern about weight, objectively-measured PA and BMI. In order to make full use of the data available, the research questions are addressed using individual growth modeling. Based on research on parental child feeding strategies, it is anticipated that girls who are encouraged to be active for weight loss will exhibit greater concern about their weight, higher BMI, and lower moderate-to-vigorous PA (MVPA) independent of important covariates.
Methods
Participants
Families were part of a longitudinal study examining girls' health and development across ages 5- to 15-years. The study began in 1996 and concluded in 2007. Families residing in Central Pennsylvania, USA, were recruited for the longitudinal study using flyers and newspaper advertisements. Families with age-eligible female children within a 5-county radius also received mailings and follow-up phone calls. Participants for this study include 183 non-Hispanic white girls and their mothers and fathers who were assessed when girls were 9 years old (M age 9.34 ± 0.3) and invited to complete follow-up assessments when girls were ages 11, 13, and 15 years old. The number of families who participated in each follow-up assessment was as follows: 177 families at age 11 (M age 11.34 ± 0.3); 168 families at age 13 (M age 13.33 ± 0.3); and 165 families at age 15 (M age 15.34 ± 0.3). Girls and their families who did not participate in the study beyond age 9 (N = 15) were not included in the analyses, resulting in a final sample size of 177 families. No differences in parental encouragement of PA for weight loss or girls' BMI, or weight concerns were identified for girls who did and did not participate in the study beyond age 9.
This study was part of a larger longitudinal study examining familial influences on girls' evolving dietary patterns and health-related outcomes. In addition to encouraging PA for weight loss, more positive forms of parental support for girls' PA were also assessed. Encouraging PA for weight loss was not a focus of the study. The Institutional Review Board of Pennsylvania State University approved all study procedures. Parents completed informed consent forms for themselves and their daughters at study onset and at each time of assessment as necessary due to modifications to the study protocol (i.e., the inclusion of new measures). Starting at age 11, girls also provided written assent.
Procedures
During summer of the years girls turned 9, 11, 13, and 15 years old, parents and girls visited the General Clinical Research Center at Pennsylvania State University to complete self-report questionnaires and have their height and weight measured. Parents completed the questionnaires independently. Girls were individually administered the questionnaires by trained assistants at age 9 and completed the questionnaires independently at ages 11, 13, and 15 with guidance from research assistants. In addition, when girls were 13 and 15 years old, research personnel visited girls during early fall (i.e., September and October) at their homes or at their schools to explain the accelerometer protocol and distribute the monitors. Monitors were returned by registered mail. All accelerometer data were collected between September and mid November to ensure that cold weather did not prevent girls from being active outdoors.
Measures: Independent Variable
Encouragement of Physical Activity for Weight Loss
In the absence of a previously validated questionnaire of encouragement of PA for weight loss, a measure was developed for this study. At each time of assessment, mothers and fathers were asked to respond to each of the following questions using a 4-point response scale (0=definitely not; 3=a lot/definitely): (1) Have you ever talked to your daughter about how to exercise to lose weight?; (2) Have you ever encouraged your daughter to exercise more in order to lose weight; and (3) Have you ever put your daughter on an exercise program to lose weight? Scores for the three items were averaged at each age. Results from preliminary analyses showed few differences in the relationship between maternal and paternal encouragement of PA for weight loss and key outcomes of interest. In addition, mothers' and fathers' reports were significant correlated at each age (r = .60 or higher, p < .001). Therefore, scores for mothers and fathers were averaged at each age to create a single parental encouragement score. The internal consistency coefficient for parental encouragement of PA for weight loss was α =.85 or higher at all times of assessment.
Measures: Dependent Variables
Concern about Weight
At each time of assessment, girls' concern about their weight was assessed using the Weight Concerns scale (Killen, Taylor, Hayward, Wilson, Haydel, Hammer et al., 1994). This scale includes five items which assess girls' fear of weight gain, worry about weight and body shape, and perceived fatness. Girls responded to each item using a 5-point response scale, with high scores indicating high concern about weight. Previous research supports the scale's concurrent and predictive validity in adolescent populations (Killen, et al., 1994). Given that the Weight Concerns Scale was originally developed for preadolescent and adolescent populations, a simplified version of the scale was administered to girls at age 9. In the amended version, the response scale was reduced from a 5-point scale to a 3-point scale. The internal consistency coefficients in this sample were α = .63 (age 9), α =. 78 (age 11), α = .84 (age 13), and α = .88 (age 15).
Body Mass Index (BMI)
Girls' height and weight were measured in triplicate at each age by a trained research assistant using a wall-mounted stadiometer and a calibrated electronic scale. Average height and weight were used to calculate BMI (weight (kg)/height (m)2) at each age. BMI values were converted to age- and sex-specific BMI percentiles and z-scores using the 2000 growth charts from the Centers for Disease Control and Prevention (Kuczmarski & Flegal, 2000). Girls with a BMI percentile ≥ 85 and < 95 were defined as overweight and girls with a BMI percentile ≥ 95 were defined as obese. All remaining girls were defined as normal weight.
Physical Activity: Objective Monitoring
An objective assessment of girls' PA was obtained when girls were 13 and 15 years old using the ActiGraph 7164 accelerometer (Shalimar, FL), which has been shown to be a valid and reliable tool for assessing PA in children and adolescents (Trost, Ward, Moorehead, Watson, Riner, & Burke, 1998). Accelerometer data, which are output as “counts”, were compiled over 30s intervals (or epochs). Girls were instructed to wear the ActiGraph at all times, except when bathing and swimming, for 7 consecutive days. Consistent with previous studies, the ActiGraph was worn on the right hip. Non-wearing time for each monitoring day was calculated by counting the number of zero counts accumulated in strings of 20 minutes or longer. Girls were included in the analyses if they had 4 or more days with 10 or more hours of wearing time (Trost, McIver, & Pate, 2005). Of the 148 girls who completed the accelerometer protocol at age 13, 140 girls had valid data based on the criteria above and were used in the analyses. Of the 113 girls who completed the accelerometer protocol at age 15, 96 girls had valid data. Raw accelerometer counts were converted to minutes per day spent in moderate-to-vigorous PA (MVPA) using age-specific count thresholds (Freedson, Pober, & Janz, 2005; Trost, Pate, Sallis, Freedson, Taylor, Dowda et al., 2002).
Physical Activity: Other Measures
Because an objective measure of girls' PA was not available prior to age 13, data for surrogate measures of PA that were obtained at age 11 were used in the analyses to control for pre-existing levels of PA. Three measures of PA were obtained including girls' general inclination toward activity, participation in organized sports, and cardiovascular fitness. The Children's Physical Activity scale (CPA) was used to assess girls' general inclination toward activity (e.g., “I would rather watch TV or play in the house than play outside” (reverse scored); “I participate in sports almost every day”) (Tucker, Seljaas, & Hager, 1997). This measure includes 15 items and uses a 4-point response scale ranging from 1 = completely true to 4 = completely false. Scores on the measure were inversely associated with 1-mile run/walk time, body fat percentage, and BMI in a sample of 9 and 10 year old children, supporting the validity of the scale (Tucker, et al., 1997). Girls' participation in team sports and organized activities was assessed using an activity checklist. Girls were presented with a list of 24 activities (e.g., rollerblading, soccer, cheerleading) and asked to indicate if they participated in each activity at an organized level (i.e., on a team or took lessons). The total number of activities selected was summed to reflect the total number of sports and organized activities in which girls participated.
Finally, girls' cardiovascular fitness, an indirect measure of PA, was measured using the Progressive Aerobic Cardiovascular Endurance Run (PACER; Leger, Mercier, Gadoury, & Lambert, 1988). Previous research illustrates the test-retest reliability of the PACER and has shown that the number of laps completed is significantly and positively correlated with measured VO2 Max (Liu, Plowman, & Looney, 1992). Scores for the three measures of PA obtained at age 11 were combined using principal component analysis to create a more reliable, valid, and multidimensional assessment of girls' PA (Wood, 2000). A single score was created using weights (or factor loadings) reflecting the intercorrelations between the measures. The resulting score (a z-score with a mean of 0 and standard deviation of 1) was correlated with each individual measure of PA with correlations ranging between r = .57 and r = .79, p < .0001.
Measures: Covariates
Parental Support for Children's Physical Activity
In order to examine whether links identified between encouragement of PA for weight loss were independent of other forms of support for PA, parents completed the Activity Support scale (ACTS; Davison, Cutting, & Birch, 2003) at each time of assessment. This is a 7-item scale that assesses two domains of parental support including logistic support (e.g., taking girls to places where they can be active, enrolling them in activities) and modeling (e.g., being active with girls, using their own behavior to show girls how to be active). Previous research supports the factorial structure, predictive validity, and internal consistency of this scale (Davison, et al., 2003). Similar to encouragement of PA for weight loss, scores for mothers and fathers were combined to create a parent modeling and a parent logistic support score at each age. The internal consistency coefficients ranged between α = .70 and α = .77 across all times of assessment.
Pubertal Development
Girls' pubertal development was examined as a potential covariate given prior links between visible aspects of pubertal development and girls' concern about weight and their PA (Baker, Birch, Trost, & Davison, 2007; Davison, Werder, Trost, Baker, & Birch, 2007; Dorn, Dahl, Woodward, & Biro, 2006). At each time of assessment, girls' breast development was determined by physical examination of the breasts using Tanner breast staging (Marshall & Tanner, 1969). Ratings were conducted in a clinical setting by a nurse and a nurse's assistant. Each breast was directly observed by both raters, who jointly determined a breast stage score ranging from 1 (no development) to 5 (mature development). Scores for each breast were averaged to create a total breast development score. In cases where ratings of the two breasts were not equal, the lower stage was used because the girl had not fully attained the higher stage.
Dietary Intake
At ages 9, 11, and 13, girls' dietary intake was assessed using 24 hour recall telephone interviews. At each age, average values from three recalls were calculated (including 2 weekday and 1 weekend day). The Nutrition Data System for Research (NDS-R) software (food database version 12A, nutrient database version 28, 1996, University of Minnesota Nutrition Coordinating Center, Minneapolis) was used for data collection and analysis. A multiple pass procedure was used facilitate recall and improve the reliability and validity of girls' reports (Johnson, Driscoll, & Goran, 1996). Only data for girls' total energy intake (kcal) was of interest in this study.
Statistical Analyses
The objectives of this study were assessed using individual growth models (Singer & Willett, 2003) using SAS PROC MIXED in SAS version 9. This analytic method makes full use of the data available at each assessment, accounts for the within-person correlation across time, reduces the number of analyses performed, and increases the number of data points – thereby increasing the statistical power and reducing the likelihood of a type I error. PROC MIXED supports a host of goodness-of-fit (residual), leverage, and influence diagnostics for multilevel growth models (Bryk & Raudenbush, 1992) and conventional model diagnostics for the detection of model misspecification and influential outliers (Belsley, Kuh, & Welsch, 1980; Cook & Weisberg, 1982). Residual diagnostics unequivocally supported the assumption of normality level-1 regression errors and homogeneity of variances in the growth models reported below. Furthermore, subject-based deletion diagnostics did not evidence undue influence on estimates of the fixed effects or their estimated standard errors reported for objectives 1 or 2, or in estimates of the level-2 random effects.
Objective 1
This focused on changes in encouragement of PA for weight loss across ages 9 to 15 years and differences in such trajectories for non-overweight, overweight, and obese girls. Initial analyses indicated that encouragement of PA for weight loss exhibited linear change between ages 9 and 15 years and that an unstructured error covariance matrix provided the most appropriate fit with the data. To examine girls' weight status as a predictor of parents' encouragement of PA for weight loss, encouragement was regressed onto time (i.e., age), girls' weight status, and the interaction between time and weight status. The intercept and slope for encouragement were modeled as random effects and weight status and the interaction between weight status and time were modeled as fixed effects. Girls' weight status was modeled as a categorical variable (non-overweight, overweight, obese), with obese as the referent category. To account for the fact that girls can move back and forth between weight status categories, weight status was modeled as a time-varying covariate.
Objective 2
Individual growth modeling was also used to examine the lagged effect of encouragement of PA for weight loss on girls' concern about weight, BMI, and MVPA. All outcome variables, including BMI, were modeled as continuous variables. Girls who were never overweight and girls who were never exposed to encouragement of PA for weight loss were excluded from the analyses for this objective (N = 39). Thus, analyses focused on girls for whom encouragement of PA for weight loss was relevant, including girls who were classified as overweight at least once and girls whose parents reported some level of encouragement of PA for weight loss, regardless of girls' weight status, across the 4 assessment occasions (N = 138).
In an initial series of analyses, unconditional growth models (i.e., a simple two-level model) were fit to the data. In these models, the level-1 regression modeled the individuals' trajectories of an outcome variable, and the level-2 regression modeled variation in parameters from the growth model as random effects unrelated to any person-level covariates for each outcome variable to (a) determine if there was sufficient variability in the intercepts and slopes to warrant the inclusion of level 2 covariates, (b) determine whether the outcome variable exhibited linear or nonlinear change across time, (c) identify the appropriate structure of the error covariance matrix, and (d) establish baseline cross-level exploratory analyses for level-1 residuals and level-2 outliers (Bryk & Raudenbush, 1992). Model fit for the error covariance structures was compared using the AIC fit index, with smaller values indicating better fit. Results from these analyses indicated that there was statistically significant variability in the intercepts and slopes for all outcome variables. In addition, all outcome variables exhibited linear change across ages 11 to 15 years (weight concerns, BMI) or ages 13 to 15 years (MVPA), the ages across which change in the outcome variables were modeled. An unstructured error covariance matrix was most appropriate when modeling weight concerns and BMI. Because MVPA was assessed at two occasions only, it was necessary to specify a random intercepts model with an independent error covariance structure.
To assess the second objective, individual growth models assessing the lagged effect of encouragement, and relevant covariates, were then examined for each outcome. Examining lagged effects reduces the likelihood of reciprocal causation (e.g., that the outcome variables predicted or led to encouragement of PA for weight loss) and increases the ability to assess the temporal sequence of the growth model (Singer & Willett, 2003). Given well-documented links between early pubertal development (Davison, Susman, & Birch, 2003; Davison, Werder, Trost, Baker, & Birch, 2007), weight status (Trost, Kerr, Ward, & Pate, 2001), dietary intake (Astrup, Ryan, Grunwald, Storgaard, Saris, Melanson et al., 2000; Berkey, Rockett, Field, Gillman, Frazier, Camargo et al., 2000), parental support for PA (Gustafson & Rhodes, 2006) and one or more of the outcome variables, these variables were entered into the models as covariates (dietary intake was only entered into the model predicting BMI). With the exception of early pubertal development (i.e., breast development at age 9), all covariates were time-varying. In addition, to control for pre-existing levels of the outcome variable, the outcome measure at baseline (i.e., age 9 for weight concerns and BMI and age 11 for MVPA) was entered into the appropriate model as a time-invariant covariate.
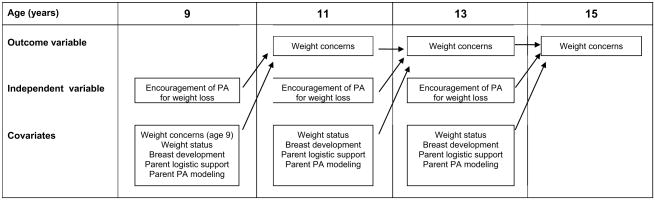
Figure 1 illustrates the sequencing of effects in the analytic model using girls' weight concerns as an example. As indicated, encouragement of PA for weight loss at age 9 affected weight concerns at age 11, encouragement at age 11 affected weight concerns at age 13, and encouragement at age 13 affected weight concerns at age 15. In addition, Figure 1 shows that girls' weight concerns (at baseline), weight status, and breast development and parents' logistic support of girls' PA and modeling of PA also exerted lagged effects on girls' weight concerns – as covariates. Similar models with slight modifications were utilized for BMI and MVPA. For BMI, total caloric intake was included as an additional a time-varying covariate. For MVPA, the outcome was modeled across ages 13 to 15 years (rather than 11 to 15 years) and baseline PA was measured at age 11. To facilitate interpretation of the results continuous covariates were mean-centered at 0. Rather than mean centering girls' BMI, their BMI z-score at baseline (age 9) was included as a covariate given that it has a population reference mean of 0 and is readily interpretable. For breast development, Tanner staging was recoded to have a lower bound of 0 rather than 1.
Figure 1.
Summary of the analytic model for objective 2 using weight concerns as an example
Note; With the exception of baseline weight concerns and breast development (assessed at age 9), all covariates were time-varying and assessed concurrently with encouragement of PA for weight loss. Baseline weight concerns was included in the model as a time invariant covariate to control for pre-existing levels of concern about weight. Similar models predicting BMI and MVPA were run with the exception that the model predicting BMI also included caloric intake as a time-varying covariate and the model for MVPA predicted MVPA at ages 13 and 15 only with baseline PA measured at age 11.
Results
Descriptive Statistics
At age 9, 15% of girls were from families with a total family income of less than < $35,000, 28% had a family income of $35,000 - $50,000, and 57% had a family income of > $50,000. At age 9, 17% of girls were overweight. This figure declined with age to 10% at age 15. Similarly, 14% of girls were obese at age 9, which declined to 8% by age 15. Parents were in general well-educated; mothers and fathers completed a mean of 15 ± 2 (range = 12 - 20) and 15 ± 3 (range = 12 - 20) years of education respectively. Parents were on average overweight with a mean BMI of 27.5 ± 6.3 for mothers and 29.0 ± 4.5 for fathers. As shown in Table 1, parents reported low encouragement of PA for weight loss, with scores increasing slightly with age. In contrast, parents reported moderate to high levels of modeling of PA and logistic support for girls' PA, with mean scores for both forms of support decreasing with age. On average, girls participated in 35 minutes of MVPA per day at age 13 and 26 minutes per day at age 15. Girls' weight concerns were low at age 9 but then increased with time.
Table 1. Means (SD) for parent and child measures at each time of assessment.
| Girls' Age | |||||
|---|---|---|---|---|---|
| MEASURES | Scale range | 9 | 11 | 13 | 15 |
| Parents' support of girls' PA | |||||
| Encouragement of PA for weight loss | 0-3 | 0.40 (.60) | 0.49 (.65) | 0.59 (.72) | 0.57 (.69) |
| Modeling of PA | 0-3 | 1.56 (.48) | 1.49 (.55) | 1.41 (.56) | 1.28 (.54) |
| Logistic support for PA | 0-3 | 2.00 (.59) | 2.11 (.57) | 1.96 (.64) | 1.81 (.70) |
| Girls' outcome measures | |||||
| Weight concerns | 0-4 | .38 (.34) | .72 (.60) | 1.11 (.78) | 1.34 (.90) |
| BMI | NA | 18.5 (3.4) | 20.0 (4.0) | 21.4 (4.5) | 22.3 (4.4) |
| MVPA (average mins/day) | 0+ | 35.9 (14.8) | 26.3 (15.1) | ||
PA = physical activity; MVPA = moderate to vigorous physical activity; Modeling of PA and logistic support for PA are general measures of parental encouragement of PA that do not focus on weight loss.
Objective 1: Weight status as a Predictor of Encouragement of PA for Weight Loss
Age, weight status, and their interaction were examined as predictors of parents' encouragement of PA for weight loss. Results showed that encouragement of PA for weight loss increased linearly with age (b = .128, t = 3.45, p < .0001). A significant effect for weight status revealed that parents of obese girls reported significantly higher encouragement of PA for weight loss compared with parents of normal weight (b = -.90, t = -11.56, p < .001) and overweight (b = -.36, t = -4.04, p < .001) girls. The interaction between time and weight status was not significant indicating that the rate of change in encouragement did not differ significantly for normal weight, overweight and obese girls (F = 1.10, p = .34). Additional analyses showed that normal weight (b = .31, t = 9.47, p <.001), overweight (b = .89, t = 17.17, p <.001), and obese (b = 1.29, t = 20.34, p <.001) girls had a mean encouragement score across ages 9 to 15 that was significantly different than 0, indicating that girls in all weight status categories were exposed to some level of encouragement of PA for weight loss.
Objective 2: Lagged Effect of Encouragement of PA for Weight Loss on Girls' Concern about Weight, MVPA and BMI
Results from the individual growth models for objective 2 are reported in Table 2. Initial model diagnostics unambiguously preferred the linear growth model over non-linear alternatives. Thus, all models showed a linear change in the outcome measure (reported as the slope of the “age” covariate). Given that covariates were mean-centered at 0, the parameters in Table 2 can be interpreted as follows; the “intercept” and “age” correspond to the mean for the outcome variable at time = 0 (age 11 for BMI, weight concerns; age 13 for MVPA) and the rate of change in the outcome when all covariates are 0 (i.e., no encouragement of PA for weight loss, not obese, no breast development at age 9, and average scores for the outcome at baseline, logistic support, modeling, and caloric intake). “Encourage PA for weight loss” reflects the differential in the outcome with a one unit difference in encouragement and “Age * Encourage PA for weight loss” reflects the differential in the rate of change in the outcome for a one unit increase in encouragement, controlling for the effects of the covariates.
Table 2. Results from the growth models examining the lagged effect of encouragement of PA for weight loss on (a) girls' concern about weight, (b) BMI and (c) MVPA, controlling for covariates.
| Outcome Measures | Weight Concerns | BMI | MVPA | |||
|---|---|---|---|---|---|---|
| b (SE) | t-value | b (SE) | t-value | b (SE) | t-value | |
| Intercept 1 | .53 (.08) | 6.03 *** | 17.92 (.30) | 59.91*** | 39.77 (3.41) | 11.67*** |
| Age 2 | .19 (.0) | 7.72** | 0.66 (.09) | 7.68*** | -12.25 (5.25) | -2.33* |
| Encourage PA for weight loss | .27 (.10) | 2.65** | 1.02 (.30) | 3.39** | -1.47 (2.57) | -0.57 |
| Age* Encourage PA for weight loss | -.05 (.03) | -1.52 | -.18 (.10) | -1.83 | -0.20 (3.32) | -0.06 |
| Covariates: 3 | ||||||
| Obese (yes, no) | .40 (.18) | 2.16* | 2.17 (.53) | 4.10*** | 2.52 (4.77) | 0.53 |
| Obese* Age | -.01 (.06) | 0.19 | -.13 (.21) | -0.63 | 4.29 (6.44) | 0.67 |
| Outcome at baseline | .35 (.15) | 2.29* | 2.91 (.31) | 9.39*** | 2.23 (1.10) | 2.02* |
| Breast development | .09 (.06) | 1.37 | 0.06 (.28) | 0.22 | -2.24 (1.63) | -1.37 |
| Parent logistic support for PA | .01 (.06) | 0.72 | .25 (.19) | 1.31 | 0.72 (2.07) | 0.35 |
| Parent modeling of PA | -.06 (.08) | -0.78 | -.09 (.26) | -0.33 | 2.35 (2.14) | 1.10 |
| Total energy intake (kcal) | .0003 (.0002) | 1.50 | ||||
b = unstandardized beta weight.
p <.05,
p<.01,
p<.001
The intercept was initialized at age 11 for weight concerns (WC) and BMI and at age 13 for MVPA.
“Age” represents the slope in the outcome variable across ages 11 to 15 years for WC and BMI and across ages 13 to 15 years for MVPA.
Covariates were measured concurrently with encouragement of PA for weight loss.
Girls' concern about weight increased significantly at a rate of 0.19 units per year. Parents' encouragement of PA for weight loss at age 9 had a significant positive effect on girls' concern about weight at age 11, independent of covariates. Girls' weight concern at age 11 increased by .27 units for each unit increase in encouragement at age 9. Similarly, parent encouragement at age 11 had a significant positive effect on girls' weight concerns at age 13 (b = .18, t = 2.51, p < .05). In contrast, the effect of encouragement at age 13 on weight concerns at age 15 was not significant (b = .08, t = .93, p > .05). Differential lagged effects of encouragement on girls' weight concerns at each age are illustrated in Figure 2. The interaction between age and encouragement was not significant indicating that while there was some suggestion that girls exposed to low versus high encouragement reported more similar concern about weight with increasing age, this effect was not significant.
Figure 2.
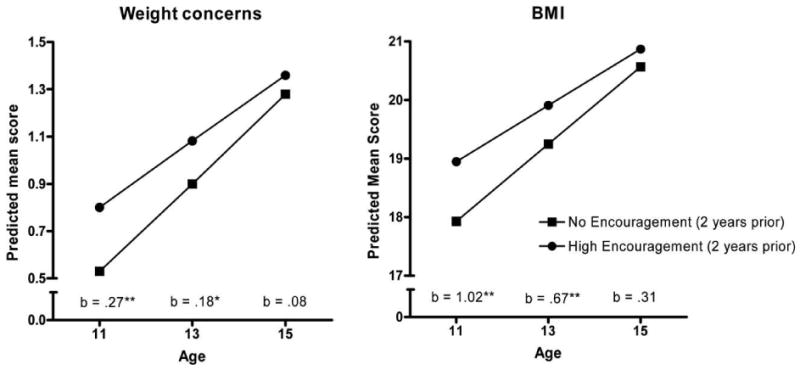
Differential lagged effects of encouragement of PA for weight loss on girls' weight concerns and BMI by age.
Note: The unstandardized beta weights (b) reflect the expected differential in the outcome variable for girls exposed to low (score=0) versus high (score = 1) encouragement of PA for weight loss, controlling for covariates. * p <.05 ** p < .01
BMI also increased significantly with age at a rate of 0.66 BMI units per year. After controlling for covariates, encouragement of PA for weight loss at age 9 had a significant positive lagged effect on girls' BMI at age 11; a one unit difference in encouragement at age 9 was associated with a 1.02 unit difference in BMI at age 11. Similar to girls' weight concerns, encouragement had a significant positive lagged effect on girls' BMI at age 13 (b = .67, t = 2.77, p <.01) but not at age 15 (b = .31, t = .97, p >.05) (see Figure 2). The interaction between age and encouragement was not significant indicating that encouragement of PA for weight loss did not have a significant effect on the rate of change in BMI.
Girls' MVPA declined significantly between ages 13 and 15; girls recorded 12.25 fewer minutes of MVPA each year. In contrast to concern about weight and BMI, encouragement of PA for weight loss did not have a significant lagged effect on girls' MVPA after taking covariates into consideration. In addition, there was no interaction between age and encouragement.
Discussion
Parental support of children's PA, which has been linked with higher PA among youth, has been operationalized to include modeling active behaviors, participating in activities with children, providing transportation to recreational areas, and enrolling children in activities (Gustafson & Rhodes, 2006). One form of support that has not been considered to date is parental encouragement PA for weight loss. This study examined changes in parental encouragement of PA for weight loss across ages 9 to 15 years in a longitudinal sample of girls and the prospective effect of encouragement of PA for weight loss on girls' concern about weight, BMI and objectively-measured MVPA. Results showed that while parents of obese girls were most likely to report encouraging PA for weight loss, encouragement increased linearly between ages 9 and 15 years among girls in all weight status groups. Girls whose parents encouraged them to be active for weight loss reported higher subsequent concern about weight and higher BMI independent of covariates. These effects were observed at age 11 and 13, but not age 15. Encouraging PA for weight loss did not predict girls' MVPA. Thus, contrary to parents' intentions, encouraging PA for weight loss did not lead to increases in girls' MVPA and was linked with negative psychosocial and health outcomes among girls.
Although mechanisms of effect were not explicitly examined in this study, there are a number of possible reasons why encouraging PA for weight loss might be a counterproductive strategy. First, girls may have received contradictory messages. Prior analyses with this sample showed that encouragement of PA for weight loss was not correlated with parents' general encouragement of PA (Davison, Trost, & Birch, 2007). That is, parents who encouraged girls to be active for weight loss did not report higher levels of more positive forms of support that have been linked with higher PA among children including modeling active behaviors and taking girls to places where they can be active. Second, encouraging PA for weight loss, by for example putting children on a weight loss exercise program, reduces children's autonomy to determine the circumstances under which they are active and their ability to self-regulate their behavior. Research from the child feeding literature shows that controlling parenting practices whereby parents control what, when and how much children eat have counterproductive effects on children's consumption of the target foods, their evaluation of their eating behaviors, and their body weight (Savage, et al., 2007). A third explanation for findings in the current study is a possible link between encouraging PA for weight loss and unhealthy dieting practices in girls. Such a relationship could explain the seemingly counterintuitive effect of encouraging PA for weight loss on girls' BMI in the absence of significant effects for PA. It is possible that parents who encouraged PA for weight loss also encouraged girls to diet. Research shows that parental encouragement of weight loss is linked with a greater likelihood of dieting among girls (Wertheim, et al., 2002). This in turn could be linked with unhealthy eating patterns such as skipping meals and binge eating, which may not be evident in a measure of dietary intake, but which have been associated with accelerated weight gain among adolescent girls (Stice, Cameron, Killen, Hayward, & Taylor, 1999). The negative impact of encouragement of PA for weight loss on girls' subsequent concern about weight lends credibility to this suggestion.
Lagged effects of encouraging PA for weight loss on girls' concern about weight and BMI were observed at ages 11 and 13, but not at age 15. Girls' exposure to parental encouragement of PA for weight loss increased linearly with age. It is possible that girls were particularly sensitive to such feedback from their parents at ages 11 and 13 years because it was developmentally atypical. That is, at these ages few other girls received such feedback from their parents. In addition, regulating body weight through exercise may not have been a key topic of conversation among peers prior to age 13. Given the rapid social transitions that take place after age 13, including the transition into high school, the increase in cross-sex friendships, and the onset of romantic relationships (Savin-Williams & Berndy, 1990), encouraging PA for weight loss or weight maintenance may have been be more normative for girls and may have been consistent with similar feedback from peers. These ideas are purely speculative and require additional research.
Contrary to expectations, encouraging PA for weight loss did not predict lower MVPA among girls. The lack of an effect for MVPA may be explained by the fact that this outcome was measured at ages 13 and 15 years only. Links between encouragement of PA for weight loss and girls' MVPA may be limited to the earlier ages in this sample, as was observed for concern about weight and BMI. If this is the case, the absence of a measure of MVPA at age 11 would prevent the identification of this time-dependent effect. Future research could assess this possibility by measuring encouragement of PA for weight loss and MVPA repeatedly during preadolescence and early adolescence.
The current study fills an important knowledge gap and provides much needed information on the potential consequences of encouraging children to be active for the purpose of weight loss in a non-clinical setting. Additional strengths of this study include the use of a longitudinal design with data collected at regular intervals across ages 9 to 15 years, the assessment of mothers' and fathers' encouragement of PA for weight loss, the use of an objective measure of PA, the assessment of psychosocial and behavioral outcomes among girls, and the use of an analytic procedure that capitalizes on the strengths of the longitudinal design.
This study also has a number of limitations. First, some measures were not available at all times of assessment. In the case of MVPA, it was necessary to use a surrogate measure to account for pre-existing differences in PA. While using the same objective measure of PA at all times of assessment would have been more appropriate, the surrogate measure combined three measures of PA and, therefore, provides a reasonable estimate of girls' general levels of PA prior to age 13. Second, this study utilized a non-validated measure of encouragement of PA for weight loss. In the absence of a previously validated measure, it was necessary to develop a scale specifically for this study. Results from the study, however, provide preliminary evidence of the scale's reliability and validity. Finally, findings from this study are only applicable to white Non-Hispanic girls from generally middle class families. Future research could explore this topic in greater detail by examining mechanisms that explain the observed effects.
In conclusion, results from this sample of girls suggest that parental encouragement of physical activity for weight loss may have unintended negative outcomes for girls, particularly during early adolescence, including increased concern about weight and increased BMI. While it is important that parents seek to promote healthy lifestyles among children, results from this study in conjunction with prior research on child feeding strategies suggest that overly controlling strategies that focus on body weight and which reduce children's autonomy to make healthy choices, should be avoided. Instead parents could promote healthy lifestyles by exposing children to healthy foods and healthy activities and giving them freedom to make choices within such contexts.
Acknowledgments
We would like to thank Stewart Trost for his helpful feedback on earlier versions of this paper. This study was supported by NIH grants RO1 HD32973, RO1 HD46567-01, MO1 RR107. Other
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- American Academy of Pediatrics. Prevention of pediatric overweight and cbesity. Pediatrics. 2003;112(2):424–430. doi: 10.1542/peds.112.2.424. [DOI] [PubMed] [Google Scholar]
- Astrup A, Ryan L, Grunwald G, Storgaard M, Saris W, Melanson E, et al. The role of dietary fat in body fatness: evidence from a preliminary meta-analysis of ad libitum low-fat dietary intervention studies. British Journal of Nutrition. 2000;83:S25–S32. doi: 10.1017/s0007114500000921. [DOI] [PubMed] [Google Scholar]
- Baker B, Birch L, Trost S, Davison K. Advanced pubertal status at age 11 and lower physical activity in adolescent girls. Journal of Pediatrics. 2007;151:488–493. doi: 10.1016/j.jpeds.2007.04.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Belsley D, Kuh E, Welsch R. Regression Diagnostics. New York: Wiley; 1980. [Google Scholar]
- Berkey C, Rockett H, Field A, Gillman M, Frazier A, Camargo C, et al. Activity, dietary intake and weight changes in a longitudinal study of preadolescent and adolescent boys and girls. Pediatrics. 2000;105:e56. doi: 10.1542/peds.105.4.e56. Retrieved 1.12.08 from http://pediatrics.aappublications.org/cgi/reprint/105/4/e56. [DOI] [PubMed]
- Birch L, Fisher J. Mothers' child-feeding practices influence daughters' eating and weight. American Journal of Clinical Nutrition. 2000;71:1054–1061. doi: 10.1093/ajcn/71.5.1054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bryk A, Raudenbush S. Hierarchical linear models for social and behavioral research: Applications and data analysis methods. Newbury Park: Sage Publications; 1992. [Google Scholar]
- Carper J, Fisher J, Birch L. Young girls' emerging dietary restraint and disinhibition are related to parental control in child feeding. Appetite. 2000;35:121–129. doi: 10.1006/appe.2000.0343. [DOI] [PubMed] [Google Scholar]
- Cook R, Weisberg S. Residuals and influence in regression. London: Chapman and Hall; 1982. [Google Scholar]
- Davison K, Cutting T, Birch L. Parents' activity-related parenting practices predict girls' physical activity. Medicine and Science in Sports and Exercise. 2003;35(9):1589–1595. doi: 10.1249/01.MSS.0000084524.19408.0C. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davison K, Susman E, Birch L. Percent body fat at age 5 predicts earlier pubertal development among girls at age 9. Pediatrics. 2003;111(4):815–821. doi: 10.1542/peds.111.4.815. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davison K, Trost S, Birch L. Encouragement of physical activity for weight loss may lead to negative psychological outcomes among girls. Medicine and Science in Sports and Exercise. 2007;39:S86. [Google Scholar]
- Davison KK, Werder JL, Trost SG, Baker BL, Birch LL. Why are early developing girls less active? Links between pubertal development, psychological well-being and physical activity among girls at ages 11 and 13. Social Science and Medicine. 2007;64:2391–2404. doi: 10.1016/j.socscimed.2007.02.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dorn L, Dahl R, Woodward H, Biro F. Defining the boundaries of early adolescence: A user's guide to assessing pubertal status and pubertal timing in research with adolescents. Applied Developmental Science. 2006;10(1):30–56. [Google Scholar]
- Evans W, Finkelstein E, Kamerow D, Renaud J. Public perceptions of childhood obesity. American Journal of Preventive Medicine. 2005;28(1):26–32. doi: 10.1016/j.amepre.2004.09.008. [DOI] [PubMed] [Google Scholar]
- Fisher J, Mitchell D, Smiciklas-Wright H, Birch L. Parental influences on young girls' fruit and vegetable, micronutrient, and fat intakes. Journal of the American Dietetic Association. 2002;102:58–64. doi: 10.1016/s0002-8223(02)90017-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Freedson P, Pober D, Janz K. Calibration of accelerometer output for children. Medicine and Science in Sports and Exercise. 2005;S37(11):S523–530. doi: 10.1249/01.mss.0000185658.28284.ba. [DOI] [PubMed] [Google Scholar]
- Golan M. Parents as agents of change in childhood obesity - from research to practice. International Journal of Pediatric Obesity. 2006;1(2):66–76. doi: 10.1080/17477160600644272. [DOI] [PubMed] [Google Scholar]
- Gustafson S, Rhodes R. Parental correlates of physical activity in children and early adolescents. Sports Medicine. 2006;36(1):79–97. doi: 10.2165/00007256-200636010-00006. [DOI] [PubMed] [Google Scholar]
- Hedley A, Ogden C, Johnson C, Carroll M, Curtin L, Flegal K. Prevalence of overweight and obesity among US children, adolescents, and adults, 1999-2002. Journal of the American Medical Association. 2004;291(23):2847–2850. doi: 10.1001/jama.291.23.2847. [DOI] [PubMed] [Google Scholar]
- Johnson R, Driscoll P, Goran M. Comparison of multiple-pass 24-hour recall estimates of energy intake with total energy expenditure determined by the doubly labeled water method in children. Journal of the American Dietetic Association. 1996;96:1140–1144. doi: 10.1016/S0002-8223(96)00293-3. [DOI] [PubMed] [Google Scholar]
- Killen J, Taylor C, Hayward C, Wilson D, Haydel F, Hammer L, et al. Pursuit of thinness and onset of eating disorder symptoms in a community sample of adolescent girls: A three-year prospective analysis. International Journal of Eating Disorders. 1994;16(3):227–238. doi: 10.1002/1098-108x(199411)16:3<227::aid-eat2260160303>3.0.co;2-l. [DOI] [PubMed] [Google Scholar]
- Kuczmarski R, Flegal K. Criteria for definition of overweight in transition: background and recommendations for the United States. American Journal of Clinical Nutrition. 2000;72:1074–1081. doi: 10.1093/ajcn/72.5.1074. [DOI] [PubMed] [Google Scholar]
- Leger L, Mercier D, Gadoury C, Lambert J. The multistage 20 metre shuttle run test for aerobic fitness. Journal of Sports Sciences. 1988;6:93–101. doi: 10.1080/02640418808729800. [DOI] [PubMed] [Google Scholar]
- Liu N, Plowman S, Looney M. The reliability and validity of the 20-meter shuttle test in American students 12 to 15 years old. Research Quarterly for Exercise and Sport. 1992;63:360–365. doi: 10.1080/02701367.1992.10608757. [DOI] [PubMed] [Google Scholar]
- Marshall W, Tanner J. Variations in the pattern of pubertal changes in girls. Archives of Disease in Childhood. 1969;44:291–303. doi: 10.1136/adc.44.235.291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Napier M. What does America think about childhood obesity? Robert Wood Johnson Research Highlight. 2006 April;(3) Retrieved 11.20.08 from http://www.rwjf.org/files/research/Obesity_ResearchHighlight_3_0604.pdf.
- Pugliese J, Tinsley B. Parental socialization of child and adolescent physical activity: A meta-analysis. Journal of Family Psychology. 2008;21(3):331–431. doi: 10.1037/0893-3200.21.3.331. [DOI] [PubMed] [Google Scholar]
- Savage J, Fisher J, Birch L. Parental influence on eating behavior. Journal of Law, Medicine and Ethics. 2007;35(1):22–34. doi: 10.1111/j.1748-720X.2007.00111.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Savin-Williams R, Berndy T. Friendship and peer relations. In: Feldman S, Elliot G, editors. At the threshold: the developing adolescent. Cambridge, MA: Harvard University Press; 1990. pp. 277–307. [Google Scholar]
- Singer J, Willett J. Applied longitudinal data analysis: Modeling change and event occurrence. New York: Oxford University Press Inc.; 2003. [Google Scholar]
- Stice E, Cameron R, Killen J, Hayward C, Taylor C. Naturalistic weight-reduction efforts prospectively predict growth in relative weight and onset of obesity among female adolescents. Journal of Consulting and Clinical Psychology. 1999;67(6):967–974. doi: 10.1037//0022-006x.67.6.967. [DOI] [PubMed] [Google Scholar]
- Trost S, Kerr L, Ward D, Pate R. Physical activity and determinants of physical activity in obese and non-obese children. International Journal of Obesity. 2001;25:822–829. doi: 10.1038/sj.ijo.0801621. [DOI] [PubMed] [Google Scholar]
- Trost S, McIver K, Pate R. Conducting accelerometer-based activity assessments in field-based research. Medicine and Science in Sports and Exercise. 2005;37:S531–S543. doi: 10.1249/01.mss.0000185657.86065.98. [DOI] [PubMed] [Google Scholar]
- Trost S, Pate R, Sallis J, Freedson P, Taylor W, Dowda M, et al. Age and gender differences in objectively measured physical activity in youth. Medicine and Science in Sports and Exercise. 2002;34:350–355. doi: 10.1097/00005768-200202000-00025. [DOI] [PubMed] [Google Scholar]
- Trost S, Ward D, Moorehead S, Watson P, Riner W, Burke J. Validity of the Computer Science and Applications (CSA) activity monitor in children. Medicine and Science in Sports and Exercise. 1998;30:629–633. doi: 10.1097/00005768-199804000-00023. [DOI] [PubMed] [Google Scholar]
- Tucker L, Seljaas G, Hager R. Body fat percentage of children varies according to their diet composition. Journal of the American Dietetic Association. 1997;97:981–986. doi: 10.1016/S0002-8223(97)00237-X. [DOI] [PubMed] [Google Scholar]
- U.S. Department of Health and Human Services and Healthier U.S.Gov. 2008 Physical Activity Guidelines for Americans. 2008 Retrieved 1.12.09 from http://www.health.gov/paguidelines/guidelines/default.aspx.
- Wertheim E, Martin G, Prior M, Sanson A, Smart D. Parent influences in the transmission of eating and weight-related values and behaviors. Eating Disorders. 2002;10:321–334. doi: 10.1080/10640260214507. [DOI] [PubMed] [Google Scholar]
- Wood T. Issues and future directions in assessing physical activity: An introduction to the conference proceedings. Research Quarterly for Exercise and Sport. 2000;71(2):11–16. doi: 10.1080/02701367.2000.11082779. [DOI] [PubMed] [Google Scholar]