Beyond the milestone in transplantation represented by the introduction of cyclosporine as an immunosuppressant, other factors have continued to operate to enhance survival rates for liver recipients. Previous studies have stressed the importance of venous bypass,1 the proper use of retransplantation,2 and refinements in the use of cyclosporine along with antilymphocyte preparations in effecting these additional improvements.3 Each of these factors is reviewed in detail elsewhere in this issue of Seminars.
At the same time, better overall survival rates have served to underscore the need to develop criteria that might aid in defining a population of patients upon whom the effects of better immunosuppression and better technique have had little or no impact. The purpose of the present study is to determine whether an assessment of certain recognizable and measurable patient characteristics might aid in predicting survival (Fig. 1). More specifically, the primary interest is to elucidate those factors other than rejection itself or technical failures that seriously hinder survival. Only adults will be considered, since a preliminary examination of data suggested that such preoperative patient characteristics are much less important in predicting survival among children. Only 6-month survival will be examined because the few patients who die after that date seldom die from causes related to their preoperative status.
FIG. 1.
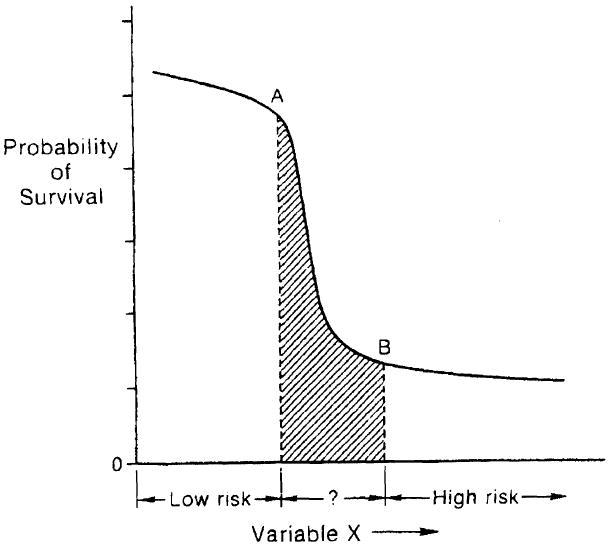
Sigmoid curve showing proposed relationship between prospective patient variables and probability of survival following liver transplantation.
METHODS
A total of 160 adult patients received primary, orthotopic liver transplantation at the University of Pittsburgh Health Center between July 1, 1981, and December 31, 1984. Of these, 35 eventually required retransplantation and seven were considered operative deaths. For survival calculations, only those 118 patients surviving at least 1 day and not requiring more than one graft were included. For consideration of factors that influence blood loss during the first transplant operation, all 160 patients were included.
Clinical Variables
Patient variables considered included age, diagnosis, race, sex, date of transplantation, number of transplants, duration of survival, measurements of serum bilirubin, creatinine, albumin, and the prothrombin time. All patients were given scores (based on a retrospective review of their preoperative records) in the following categories:
Coma (COMA): A score of 2 was assigned for those patients experiencing episodes of stage 3 or 4 coma; a score of 1, for those with intermittent episodes of moderate to severe confusion or frequent problems with mild to moderate confusion; and a score of 0, for those with no gross evidence of encephalopathy.
Malnutrition (MALN): A score of 2 was assigned for those with severe muscle wasting and obvious evidence of generalized malnutrition; a score of 1, for those with less severe malnutrition; and a score of 0 for those with no obvious signs of poor nutrition.
Ascites (ASCI): A score of 2 was assigned for those with massive, uncontrollable ascites; a score of 1, for those with moderate or controllable ascites; and a score of 0, for those with no evidence of ascites.
Miscellaneous: If a history of recurrent variceal bleeding, biliary sepsis, or spontaneous bacterial peritonitis, was present, a score of 1 was assigned, 0 if absent.
Previous Surgery: In addition, each patient was assigned an index of previous operative procedures (IOP), which was an additive score as follows: multiple previous biliary reconstructions, 2; and a single attempt, 1; portosystemic shunt procedure, 2; splenectomy, open liver biopsy, cholecystectomy, or other procedures in the upper abdomen, 1 for each separate laparotomy.
Operative blood losses (RBC) were determined by a review of the records of the Central Blood Bank of Pittsburgh and are expressed in terms of the units of packed red blood cells administered to the patient during the transplant operation.
Statistical Methods
Complete survival data were available for all patients to 6 months. Life-table analysis was used to calculate survival probabilities for intervals beyond 6 months. Multiple linear regression was used initially to examine the effects of the different variables on 6-month survival. Simple two-way linear regression was used to examine the isolated effect of each variable on survival and on RBC.
Unpaired sample means were compared using the unpaired t test, and proportions compared with the chi-square test, using Yates correction when indicated. Risk ratios, which are an estimate of the relative risk associated with a variable, were calculated for different score groups and 95% confidence intervals were calculated using the standard error of the risk ratio.
Disease Scoring System
Finally, a disease scoring system was developed based on an examination of those factors most often associated with an eventual poor outcome. The scoring system was extensively modified by trial and error to allow a maximum separation between those patients who survived for 6 months and those who did not.
RESULTS
Table 1 shows the results of a simple two-way analysis of the variables using linear regression. Survival at 6 months was found to correlate inversely and to a significant degree (see p values in Table 1) with RBC, COMA, MALN, bilirubin, and prothrombin time, and directly with the date of the transplant operation. It did not correlate to a significant degree with the patients’ age, sex, race, or diagnosis, or with IOP or ASCI scores. Stepwise multiple linear regression analysis revealed RBC to have the highest inverse correlation with survival (p < 0.0001), followed by COMA (p = 0.0001). However, because of multicolinearity, the addition to the equation of the remaining scores of disease severity did not improve the correlation. Further work with various combinations of COMA, ASCI, and MALN scores revealed the best inverse correlation with survival was that obtained by adding COMA and MALN scores.
TABLE 1.
Survival After Orthotopic Liver Transplantation: Two-Way Regression Analysis
| p Value | R2 | |
|---|---|---|
| Survival at 6 months is highly correlated with | ||
| 1. Operative blood loss | 0.0005 | 0.097 |
| 2. Coma score | 0.010 | 0.055 |
| 3. Malnutrition score | 0.025 | 0.042 |
| 4. Serum bilirubin | 0.026 | 0.042 |
| 5. Prothrombin time | 0.024 | 0.043 |
| 6. Date of transplant | 0.037 | 0.037 |
| Survival at 6 months does not correlate with | ||
| 1. History of previous surgery | 0.716 | 0.001 |
| 2. Ascites score | 0.555 | 0.003 |
| 3. Diagnosis | 0.419 | 0.061 |
| 4. Age | 0.382 | 0.007 |
The effect of RBC on survival in patients with different scores in the COMA, MALN, and ASCI categories was examined (Table 2). In those patients with marked encephalopathy (COMA = 2), the negative correlation of blood loss with survival was significant (p = 0.045) but less pronounced than in those with minimal or no encephalopathy (p = 0.0004). The negative correlation of RBC with survival was significant (p = 0.001) in patients with fair to good nutritional status (MALN = 1 or 0), but not (p = 0.063) in those patients with severe malnutrition (MALN = 2). This may have been an effect of colinearity between RBC and MALN in the analysis, since mean RBC in the MALN = 2 group (50.2 ± 58.6 units) was markedly higher than in the lower MALN score group (23.4 ± 24.6 units). Finaily, the correlation of better survival with lower blood loss was more pronounced in those patients with massive ascites (ASCI = 2) than in those with low ASCI scores p < 0.0001, F = 20.50 versus p = 0.027, F = 5.12, respectively).
TABLE 2.
Correlation of Operative Blood Loss with Survival in Different Score Categories
| Variable | Score | Correlation of RBC with Survival | p Value |
|---|---|---|---|
| Coma | 2 | Significant | 0.0450 |
| Coma | 1 or 0 | Highly significant | 0.0004 |
| Malnutrition | 2 | Not significant | 0.063 |
| Malnutrition | 1 or 0 | Significant | 0.001 |
| Ascites | 2 | Significant | 0.0265 |
| Ascites | 1 or 0 | Highly significant | <0.0001 |
Figures 2 through 4 show life-table curves for the COMA and MALN score groups and for various RBC groups. The correlation of high RBC with high scores in MALN, COMA, or ASCI categories as well as with other variables was also examined with linear regression analysis (Table 3). A high degree of correlation was found between high blood loss (RBC the dependent variable) and COMA score (p < 0.001), MALN score (p = 0.0005), ASCI score (p = 0.0001), and prothrombin time (p = 0.006). A significant negative correlation was found between RBC and the use of venous bypass (p = 0.040) and the date of transplantation (p = 0.002), a more recent transplant date correlating with lower blood losses. Total RBC did not correlate with diagnosis, bilirubin, age, or a history of previous variceal bleeding. The correlation of high RBC with IOP, the index of previous surgical procedures, was also not significant (although p = 0.066).
FIG. 2.
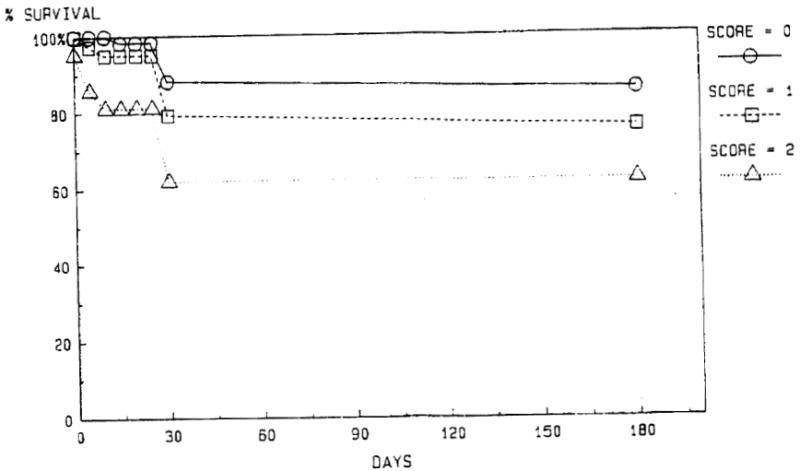
Actuarial survival after liver transplantation based on preoperative coma score.
FIG. 4.
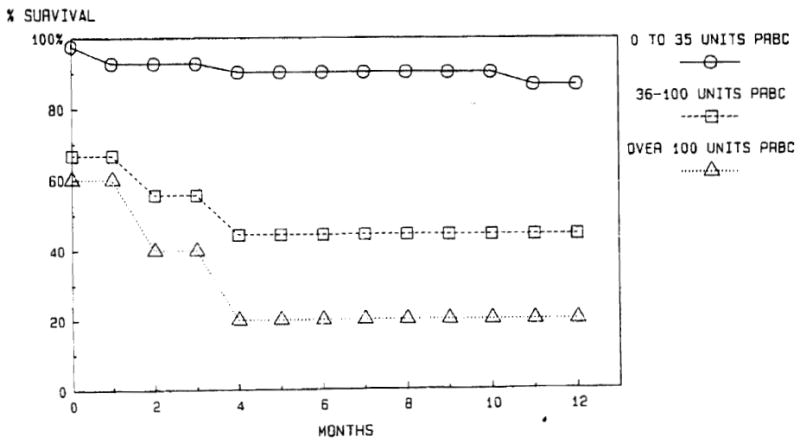
Actuarial survival after liver transplantation based on operative blood loss.
TABLE 3.
Survival after Orthotopic Liver Transplantation: Correlation of Operative Blood Loss with Other Variables
| p Value | R2 | |
|---|---|---|
| Operative blood loss correlates with | ||
| 1. Coma score | <0.00001 | 0.140 |
| 2. Ascites score | =0.0001 | 0.090 |
| 3. Malnutrition score | =0.0005 | 0.070 |
| 4. Date of transplant | =0.0023 | 0.057 |
| 5. Prothrombin time | =0.0060 | 0.046 |
| Operative blood loss does not correlate with | ||
| 1. Age | =0.879 | 0.020 |
| 2. Diagnosis | =0.660 | 0.010 |
| 3. History of variceal bleeding | =0.660 | 0.001 |
| 4. Serum bilirubin | =0.135 | 0.014 |
| 5. Index of previous surgery | =0.066 | 0.020 |
An examination of the various values of R2 (R = correlation coefficient) for the different regressions revealed that most were less than 10%. This suggests that a linear model is not appropriate for defining the relationship between the variables. In fact, in a scatterplot of different variables on the X axis versus survival probabilities on the Y axis, the curves defined for each metric variable (such as bilirubin levels, RBC, or prothrombin times) were sigmoid in shape (Fig. 1). This suggests that the relationship between survival and many of these patient variables might best be described by a third order equation, that is, y = f(x).3
An examination of the sigmoid curve in Figure 1 demonstrates how the probability of survival falls off sharply at a certain value of each patient variable. This observation was the basis for constructing a disease scoring system that would allow one to place patients into one of the three groups delineated by the two inflection points along the sigmoid curve. Those with a disease score in the flat, upper left part of the curve would represent relatively low-risk patients, and those in the flat portion of the lower right section of the curve would clearly be high-risk patients. Those patients with scores placing them between the inflection points of the curve would represent a group for whom the relative risks for transplantation would be difficult to estimate, since small errors in scoring (motion along the X axis in Figure 1) would drastically alter estimates of survival probability (position along the Y axis).
Development of the Disease Scoring System
The scoring procedure developed was that which proved most useful in defining a clear separation between the highest and lowest risk groups. This was accomplished mainly by trial and error. During this process, patients who had low-risk scores but died from causes related to surgical or immunologic factors and not to their preexisting liver disease were eliminated from consideration. This represented 7 of the 22 patients who died by 6 months. They are listed in Table 4 along with the causes of death.
TABLE 4.
Causes of Death in Patients Excluded During Creation of Disease Scoring System
| Age (Yr) | Sex | Score | Cause af Death |
|---|---|---|---|
| 33 | F | 3 | Accelerated acute rejection* |
| 43 | F | 1 | Arterial thrombosis* |
| 29 | F | 0 | Sepsis secondary to preexisting biliary tract sepsis |
| 24 | F | 0 | Colon perforation |
| 23 | M | 0 | Multiple agent sepsis, probable AIDS |
| 42 | M | 4 | Ruptured hepatic artery, 82 days |
| 28 | M | 4 | Recurrent hepatitis B, hemorrhage, sepsis |
Donor livers were not located in time for retransplantation.
The disease score is determined by adding the COMA, MALN, and ASCI scores together, with the following modifications: (1) If the patient is in a deep coma at the time of going to the operating room for the transplant, the COMA score is increased to 6; (2) an additional 1 point is given if the patient’s age is more than 40 years; (3) 2 additional points are given if the serum bilirubin level is higher than 30 mg/dl; (4) 1 point is subtracted if the prothrombin time is less than 15 seconds; (5) an additional 1 point is subtracted if the bilirubin level is less than 10 mg/dl; (6) if the resulting score is 5 or greater, 2 points should be subtracted if the patient’s age is less than 25 years; and (7) the marked effect on survival of the RBC is accounted for as follows: for patients with a total score of 5 or more, 1 point can be subtracted if RBC is 10 units or less; for all patients, if RBC is 40 units or more, an additional 1 point should be added to the total score.
Patients with a resultant score of 0 to 3 represent relatively low-risk patients. Those with a score of 7 or more are at high risk. Those with scores from 4 to 6 are located between the inflection points of the sigmoid curve and thus represent patients whose relative risks are difficult to estimate.
REVIEW OF RETROSPECTIVE SCORING
The mean score of those patients who died by 6 months (except those patients listed in Table 4) was 6.3 ± 3.1, compared with 2.1 ± 1.9 for those who survived at least 6 months (p < 0.0001). Mean scores before and after April 1, 1983, were 4.0 ± 5.6 and 3.3 ± 8.2, respectively (p > 0.50). Thus, the improvement in survival occurring after that date does not appear to be the result of selection of lower risk patients (Table 5).
TABLE 5.
Disease Scores and 6-Month Survival: A Retrospective Analysis
| No. | Mean Score* | p Value | |
|---|---|---|---|
| All patients, primary grafting | |||
| Dead < 6 months | 15 | 6.3 ± 3.1 | |
| Alive > 6 months | 96 | 2.1 ± 1.9 | <0.0001 |
| Before April, 1983 | 33 | 4.0 ± 5.6 | |
| After April, 1983 | 78 | 3.3 ± 8.2 | >0.50 |
| All patients undergoing retransplantation | |||
| Dead < 6 months | 18 | 9.2 ± 1.8 | |
| Alive > 6 months | 15 | 2.3 ± 1.7 | < 0.0001 |
Mean ±SD of different groups of patients.
Causes of Death After 6 Months
Eight of the 96 patients who survived 6 months subsequently died during the follow-up period. Recurrence of tumor was the cause of death in four of these patients (all whose disease scores were 1 or 0), at intervals of 265, 480, 490, and 617 days after transplantation. Two men, ages 53 and 38 years with scores of 0 and 2, died in foreign countries, at 426 and 905 days, respectively, of causes that were unclear but thought to be of cardiac origin. A fifth patient, a 44-year-old man whose preoperative score would have been 7, died after 439 days with hepatic failure and sepsis related to recurrent hepatitis B. Finally, a 20-year-old man, (disease score = 3), died 339 days postoperatively following massive gastrointestinal hemorrhage.
High-Risk Patients Surviving More Than 6 Months
Only 2 of the 96 patients who survived beyond 6 months had scores in the high-risk range. One was a 45-year-old woman with primary biliary cirrhosis who is a remarkable exception to the rule. Her preoperative score would have been 9. The second patient was the 44-year-old man mentioned in the preceding discussion. Both patients required extended rehabilatation periods, particularly the woman.
Five other patients had preliminary scores ranging from 5 to 8 that were reduced by 2 points because of ages less than 25 years. All are alive and well after recovery periods that were relatively short when compared with the group of older patients with scores of 6 to 9. This experience is the basis for the reduction of score related to age less than 25 years.
Low-Risk Patients Surviving Less Than 6 Months
Besides the exceptions listed in Table 4, two other patients who died in less than 6 months had scores of 0 and 3. One was a 19-year-old girl who died of disseminated herpes zoster, and the other was a 52-year-old woman who required multiple surgical reexplorations for intra-abdominal bleeding and sepsis.
Patients with Scores Between the Inflection Points
Five patients who did not survive at least 6 months and 14. who did had scores between 4 and 6. One of those who died had a score of 8 before reduction to 6 for an age of 18 years. Death in two was related to opportunistic infection arising at 1 and 4 months following discharge, most likeiy related to overimmunosuppression. Two others died largely as the result of surgical complications.
Three of the surviving patients (with scores of 5, 5, and 4), required prolonged hospitalization (4 months to more than 1 year) for rehabilitation and for treatment of various surgical complications. The others experienced rather uneventful recoveries that were free of surgical complications.
Scoring of Retransplanted Patients
A group of 33 out of 35 patients who required retransplantation were scored subsequent to development of the system (Table 5). (Two patients were eliminated from consideration because they underwent transplantation using venous bypass with full systemic heparinization.) Four of these patients required three transplants, of whom two are still alive at 2 and 3 years. Blood loss at the first transplant operation only was considered for scoring purposes. Coma scores were given on the basis of mental status at the time of reoperation. All other variables were scored on the basis of their values prior to the first transplant operation.
Among the 18 retransplanted patients who died within 6 months of the first transplant operation, scores ranged from 6 to 12, with the exception of one patient with a score of 0. That patient died 176 days after the first transplant from acute colchicine toxicity. The mean score of the remaining 17 patients was 9.2 ± 1.8). The major factor contributing to high scores for 16 of these patients was that of coma scores of 6, indicating stage III or IV coma at the time of retransplantation.
Of the remaining 15 patients who were retransplanted, 14 are alive from 14 to 43 months following their first transplant. The one patient who died had an arterial thrombosis in the second graft and was not transplanted a third time. Scores in this group ranged from 0 to 6, with a mean of 2.3 ± 1.7). None of these patients were in a coma at the time of retransplantation, although four were retransplanted urgently, two for accelerated acute rejection and two for primary nonfunction.2
Estimation of Relative Risks
Table 6 summarizes the scoring for those 111 patients used in developing the disease scoring system. Relative risk ratios were calculated from a chi-square table (with Yates correction when indicated) and 95% confidence limits estimated. A score of 7 or higher carries a 41 (95% confidence range 7.29 to 231) times greater risk of dying within the first 6 months following transplantation than does a lower score. The risk ratios and confidence limits for other scores, along with chi-square values, are shown in Table 6. Another way of interpreting each ratio is to use the inverse argument. Thus, not only are patients with a score of 7 or higher 41 times more likely to die within 6 months of transplantation, but those with a score of 6 or less are 41 times more likely to survive the first 6 months than are patients with a higher score. Of course, the 95% confidence intervals for all scores are quite wide in range. For example, the relative risk for a patient with a score of 7 or above has a 95% chance of being as high as 231 times greater or as low as 7.29 times greater than the relative risk for a patient with a score of 6 or less.
TABLE 6.
Chi-Square and Risk Ratios for Score Values
| Score | A/D* | Chi-Square | Yares Chi-Square | p Value | Risk Ratio | 95% Confidence Interval |
|---|---|---|---|---|---|---|
| 7 or above | 2/7 | 34.6 | 28.9 | <0.0001 | 41.1 | 7.29–231 |
| 6 or above | 5/9 | 35.3 | 30.5 | <0.0001 | 27.3 | 6.96–107 |
| 5 or above | 10/10 | 27.8 | 24.1 | <0.0001 | 17.2 | 4.90–60.3 |
| 4 or above | 17/12 | 26.1 | 23.0 | <0.0001 | 18.6 | 4.71–73.0 |
| 3 or above | 40/14 | 13.9 | 11.9 | <0.001 | 19.6 | 2.48–154 |
Number of patients in scoring group alive and dead at 6 months.
Effect of Previous Surgery on Blood Loss
The mean RBC loss for patients with various operations and the comparison with that for patients with no history of prior surgery is shown in Table 7. Several comparisons were made. A group of 31 patients who had had either bile duct reconstructions, cholecystectomies, or any kind of shunt procedure were compared with the 129 patients who had undergone either no perihepatic surgery or minimal procedures, such as open liver biopsy or exploratory laparotomy. Mean blood loss of the former group (35.4 ± 35.5 units) was not significantly more (p > 0.10) than that of the latter (28.7 ± 34.8 units). A second comparison between 14 patients with duct surgery only and the 129 without surgery also revealed no significant differences in RBC (31.4 ± 33.8 units, (p > 0.50). However, the mean RBC for patients with shunts (70.5 ± 46.0 units) was greater (p < 0.01) than for the other groups. (The range of blood loss for shunt patients was 7 to 143 units.)
TABLE 7.
Influence of Previous Surgery on Mean Operative Blood Loss during Orthotopic Liver Transplantation
| Group | No. | Mean RBC (units)* | p Value |
|---|---|---|---|
| No perihepatic surgery | 129 | 28.7 ± 34.8 | |
| Gallbladder, duct, or shunt surgery | 31 | 35.4 ± 35.5 | >0.10 |
| Duct procedure only | 14 | 31.4 ± 33.8 | >0.50 |
| Shunt procedure only | 6 | 70.5 ± 46.0 | <0.01 |
Mean ± SD.
DISCUSSION
Perhaps more so than for most surgical procedures, candidates for liver transplantation present in a wide range of physiologic conditions. Although the most important reasons for failure in these patients are still related to rejection, with the introduction of cyclosporine and following major improvements in surgical technique, the overall physiologic condition of the individual patient has assumed an even greater role in influencing the eventual outcome following transplantation. This became particularly evident when, in a previous study, we examined the overall impact of venous bypass on survival and discovered that, although the probability of surviving to 30 days was markedly improved, by 6 months patients transplanted with he use of bypass no longer appeared to have an advantage over those transplanted without bypass. Further investigation revealed that the bulk of the patients in the bypass group who died between 30 and 180 days could be classified, based on physiologic characteristics that they had before surgery, as belonging to a particularly high-risk category. The major purpose of the current study, then, was to determine whether a scoring system could be developed that would allow easier recognition of those patients for whom the probability of survival, despite all of the recent improvements in immunosuppression and technique, is still unacceptably low.
A key to developing the scoring system was the definition of a population of patients for whom death or survival was related more to preoperative condition than to technical failures or failure of the hepatic allograft related to poor procurement, rejection, or surgical erorrs. Restricting the analysis to those patients who had only one liver transplant went a long way toward accomplishing this goal, largely because of an aggressive attitude in the Pittsburgh program toward early retransplantation of patients with a failing graft (see accompanying article “Retransplantation of the Liver” in this issue of Seminars). Other patients were eliminated from consideration solely for the purpose of developing the scoring system. The causes of failure in these patients are no 1ess.important to examine. As far as the accuracy of the scoring system is concerned, patients who fail to follow predicted courses may truly represent exceptions that prove the rule. Examination of the causes of failure in these patients may, in fact, reveal lessons ultimately more important than those provided by the scoring system itself. This is because, by and large, the scoring system can only make predictions that most physicians experienced in the field already know to be true.
Nevertheless, some important findings are worth reiterating.
Many patient variables, which in the overall analysis have no significant impact, do make a difference among certain groups. For example, overall, age itself is not a factor that correlates with survival. However, patients younger than 25 years of age who otherwise have high scores appear to have an advantage over those who are older. An age over 40 years does not influence the probability of survival in the overall group, or in all of the diagnostic categories, with the exception of cirrhosis. In the latter group, however, the correlation of poor survival with age over 40 years appears to be more related to the coexistence of other risk factors in these older patients than to age itself. The extra 1 point added to scores for an age over 40 years, then, is largely to account for the observation that most older patients have had their liver disease for a longer period of time. Ultimately, its inclusion appeared to provide greater score separation of the survivors from non-survivors.
The most striking finding of the study is that of all the factors studied, survival at 6 months correlates most strongly with RBC. In a sense, RBC is probably a kind of metric scoring system in itself. This is suggested by the observation that RBC correlates most strongly with those other factors with which survival also correlates, namely, the COMA and MALN scores and serum bilirubin and prothrombin time. At the same time, RBC clearly can play an active role in altering the eventual outcome. This is suggested by the observations that patients with high scores who have low blood losses appear to obtain an advantage over those with high scores and higher blood loss, and all patients, regardless of score, appear to have a lower survival probability if RBC exceeds 40 units.
In this series of patients, neither RBC nor survival correlated with a history of previous surgery. This was rrue if one included any history of surgery around the liver, such as a cholecystectomy, open liver biopsy, one or multiple bile duct procedures, or shunt procedures. With one exception, it was also true when the larger group was broken down into smaller groups and individual procedures were considered.
The one exception was the group of six patients who had had portosystemic shunts. Mean blood loss in these six was 70.5 units, but it was accounted for almost entirely by four patients. Three of these four patients died on the operating table. The fourth survived surgery and an operative blood loss of 104 units, but died 4 months later, at home, of an opportunistic infection. Two other patients had RBC less than 20 units and have survived for 9 and 10 months. These last two patients and the other one who survived surgery were all three transplanted using venous bypass, whereas the three who died during surgery were not.
The study makes several other things quite clear. It adds statistical confirmation to notions most surgeons in the field already hold.
-
Patients taken to the operating room in deep coma from chronic liver disease almost never survive. Their score places them on the flat, high-risk portion of the sigmoid curve. If the status of these patients can be improved to the point that they are awake and able to breath without ventilatory support, and if they undergo a technically smooth operation with low blood loss and without surgical complications, then they probably begin their recovery period between the inflection points, perhaps even high up toward the lower risk portion of the curve. The same holds true for patients undergoing retransplantation. No one in a deep coma and requiring a second or third liver has survived long term.
The example of the one patient in this series in stage IV coma from acute hepatic necrosis who survived long term underscores the need to act quickly, if at all, in the setting of acute and fulminant hepatic failure. Long-term support, beyond a few days, of a patient in stage IV coma with an extreme coagulopathy, hypoglycemia, and other profound metabolic derangements will seldom result in a successful outcome. The decision to transplant must be made with little hesitation and a suitable donor found quickly.
The negative influence that a history of perihepatic surgery has had in previous reports has become much less important in recent years. The routine use of venous bypass may have had an important role in minimizing the specter of previous surgery.
Poor surgical technique or errors in surgical judgment can quickly obliterate the significance of any preoperative scoring system. In general, patients in better overall physiologic condition will tolerate most complications better than their less resilient counterparts. However, the health of all of these patients is compromised to begin with, and the additional burden of long operative procedures and immunosuppression leaves little room for errors.
The improvement in survival correlating with a transplant date later than the spring of 1983 reflects several developments. One is the full-scale use of venous bypass, introduced about 6 weeks before. The other is most likely the creation of a liver transplant team by the anesthesiologists in Pittsburgh and the evolvement of a more uniform and informed approach to the operative management of these patients.4,5
Finally, emphasis must be placed on the empirical nature of the scoring system. A much larger population of patients to study might allow more accurate mathematical description of the relationship between the variables and the survival probability. In addition, the system may not apply very well to other centers where differences in surgical technique or pre- and postoperative management of patients may drastically alter eventual outcome in some or even all patients. In the final analysis, one of the most exciting prospects of the present study would be to discover that such things really will make a difference.
SUMMARY
A group of 118 adults who underwent primary, orthotopic transplantation of the liver over a 4-year period served as the subjects of a detailed examination of their ability to survive the first 6 months as a function of their preoperative condition. As a result, a scoring system was developed empirically in an attempt to separate very high-risk from relatively low-risk patients. The scoring method is based on the high degree of correlation between survival probability and various patient characteristics. It allows for additional scoring to account for the dramatic effect of operative blood loss on the eventual outcome. The curve that best describes the relationship between patient scores and survival probability is sigmoidal in shape. Many patients will have scores located on the curve between the inflection points. They represent a group whose relative risk is difficult to estimate but for whom operative blood loss or the occurrence of surgical complications may prove particularly telling.
FIG. 3.
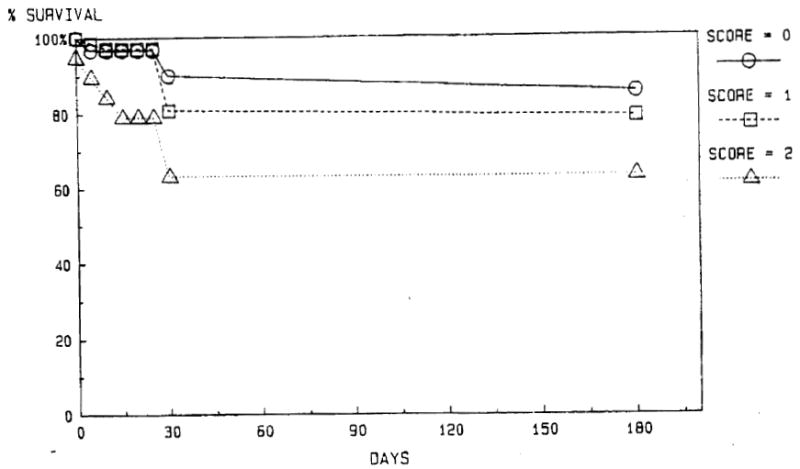
Actuarial survival after liver transplantation based on preoperative malnutrition score.
Acknowledgments
Supported by Research Grants from the Veterans Administration and Project Grant No. AM-29961 from the National Institutes of Health, Bethesda, Maryland.
References
- 1.Shaw BW, Jr, Martin DJ, Marquez JM, et al. Venous bypass in clinical liver transplantation. Ann Surg. 1984;200:524–534. doi: 10.1097/00000658-198410000-00013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Shaw BW, Jr, Gordon RD, Iwatsuki S, et al. Hepatic retransplantation. Transplant Proc. 1985;17:264–271. [PMC free article] [PubMed] [Google Scholar]
- 3.Starzl TE, Iwatsuki S, Shaw BW., Jr Orthotopic liver transplantation in 1984. Transplant Proc. 1985;17:250–258. [PMC free article] [PubMed] [Google Scholar]
- 4.Kang YG, Martin DJ, Marquez JM, et al. Intraoperative changes in blood coagulation and thromboelastographic monitoring in liver transplantation. Aneoth Analg. 1985;64:888–896. [PMC free article] [PubMed] [Google Scholar]
- 5.Marquez JM, Martin DJ, Kang YG, et al. Cardiovascular depression secondary to citrate intoxication during hepatic transplantation in man. Submitted. [Google Scholar]


