Abstract
Background
The use of recreational drugs has been observed to have deleterious effects on the heart. The aim of our study was to evaluate the effect of substance abuse on the defibrillation threshold (DFT) in patients with implantable cardioverter-defibrillators (ICDs).
Methods
A retrospective analysis was conducted on patients who had undergone ICD placement at a tertiary university medical center in Detroit, Michigan. Subjects were identified based on self reported drug use and placed into one of the three groups: Controls, Cocaine and Other Illicit Drugs. Due to a disparity in race among groups, the main analysis on DFT value was conducted on African-American patients only. Furthermore, exploratory analyses were conducted to investigate the effects of marijuana use and race on DFT values.
Results
A history of cocaine use(n=17) significantly increases DFT among African-Americans (17.3±8J vs 12.5±5J in cases vs. controls, p<0.05), while previous use of marijuana does not significantly influence DFT. African-American patients with a history of illicit drug use had indications for ICD implantation at an earlier age and that within the control (non-drug using) group, African-Americans(n=73) had higher DFT compared to Caucasians(n=32), (14.5±0.5J vs. 9.7±0.6J, p<0.05).
Conclusions
A history of cocaine use in African-Americans with ICD is a risk factor for high DFT and race itself (being African-American) may be a risk for high DFT. Use of high-energy ICDs and other DFT lowering techniques may be considered for patients who continue to use cocaine or in whom DFT testing cannot be performed at the time of implantation.
Keywords: implantable cardioverter defibrillator, defibrillation threshold, cocaine, marijuana, African-American
INTRODUCTION
The defibrillation threshold (DFT) is the minimum energy required to reliably defibrillate a fibrillating heart. It is determined usually during the implantation of the Implantable Cardioverter-Defibrillators (ICD) or at a later stage. DFT testing involves induction of ventricular fibrillation (VF) or hemodynamically unstable ventricular tachycardia (VT), often under deep sedation or general anesthesia and allowing the ICD to detect and cardiovert the ventricular arrhythmia to normal sinus rhythm. Numerous factors such as temperature, body weight, heart weight (1), anesthetic drugs (2) and a variety of anti-arrhythmic drugs like lidocaine, mexiletine and verapamil (3) in addition to underlying cardiac pathology and configuration of defibrillation leads (4) have been observed to influence DFT. Epstein and colleagues in a large multicenter study attempting to identify the predictors of elevated DFT, established the role of amiodarone as a strong predictor of a high DFT (5).
During ICD implantation, a 10 Joule safety margin between the DFT and the ICD’s maximum deliverable output is considered the standard of care. However, any imminent problem with high DFT is a compromise of this safety margin thus increasing the risk of failed defibrillation. In an effort to maintain the safety margin, several techniques including implantation of subcutaneous shocking coils and device modifications such as changing to high energy ICD or altering the defibrillation vector are performed. Hence, it becomes imperative to elucidate the risk factors for a high DFT.
The abuse of recreational drugs such as cocaine, marijuana and opioids are known to cause adverse effects on the heart including accelerated atherosclerosis, myocarditis, dilated cardiomyopathy and sudden cardiac death (6, 7). A study in 2007 by Chen et al. observed that the habitual cocaine use was associated with an increased DFT in a modest study group consisting of 11 cocaine users (8). A literature search revealed that there have been no further reported studies regarding the effect of other recreational drugs on DFT.
The purpose of this retrospective cohort study was to evaluate the effect of habitual use of recreational drugs such as cocaine, marijuana and opioids on the DFT in patients undergoing ICD placement procedures at an inner city university hospital setting with a predominant African-American patient population.
METHODS
Study Subjects
The study group consisted of patients who had undergone ICD placement at Harper university hospital between January 2006 and December 2008 in the metropolitan area of Detroit, Michigan. An electronic medical record database was used to review patient records and identify those with a positive history of illicit drug use as evidenced by self report. Those with a negative self report of drug use formed the ‘control’ group. In addition, patient demographics, medication profile, co-morbid profile, echocardiographic reports and indications for ICD placement were abstracted from the records (Tables 1 & 2).
Table 1. Distribution of subjects according to illicit drug and race.
Pearson’s Chi-Square analysis showed that controls (non-drug users) had a different racial distribution than cocaine or other illicit drug users (χ2(2)=13.09, p<0.001). Given that this retrospective study was conducted using an inner city Detroit population, which is predominately African-American, this result is not surprising nor meant to imply that only African-Americans are drug users. As a result, of the biased sample population, only African-American controls were used to compare patient profiles and DFT values among study groups.
| Control (N=105) (non-drug users) | Cocaine (N=17) | Other Illicit Drugs (N=16) | |||
|---|---|---|---|---|---|
| Marijuana | Opioids | Polydrug | |||
| African-American | 73 (70%) | 17 (100%) | 8 (100%) | 2 (100%) | 6 (100%) |
| Caucasian | 32 (30%) | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) |
Table 2. Demographics, medication/disease profiles and indications for ICD placement in study groups.
Note that only African-American controls are reported. Pearson-Chi Square (dichotomous variables) and ANOVA (continuous variables) used to assess potential differences among group distribution of demographics and profiles. Dichotomous variables are presented as total and frequency (*p<0.05; Control versus Cocaine or Other Illicit Drugs) and data reflect the number of people that reported medication use or presence of disease. Continuous variables are presented as the mean ± standard error of the mean (#p<0.05; Control versus Other Illicit Drugs).
| Control (N=73) | Cocaine (N=17) | Other Illicit Drugs (N=16) | |
|---|---|---|---|
| Demographics | |||
| Age (years) | 62 ± 2# | 56 ± 1 | 52 ± 2 |
| Gender – male | 35 (48%) | 12 (71%) | 12 (75%) |
| Body Mass Index (BMI, kg/m2) | 30 ± 1 | 26 ± 1 | 28 ± 2 |
| Subcutaneous Coil (present) | 9 (12%) | 3 (18%) | 1 (6%) |
| Ejection Fraction (%) | 30.5 ± 15.2 | 25.6 ± 24.7 | 15.6 ± 15.1 |
| Medications | |||
| Angiotensin-related drugs | 51 (70%) | 15 (88%) | 11 (69%) |
| Anti-arrhythmia drugs | 10 (14%) | 1 (6%) | 4 (25%) |
| Sympathomimetics | 59 (81%) | 14 (82%) | 14 (88%) |
| Anti-thrombosis drugs | 70 (96%) | 16 (94%) | 14 (88%) |
| Aspirin | 38 (54%) | 12 (71%) | 10 (63%) |
| Calcium-Channel blockers | 11 (15%) | 2 (12%) | 4 (25%) |
| Cardiac Glycosides | 13 (18%) | 6 (35%) | 6 (38%) |
| Diuretics | 51 (70%) | 14 (82%) | 13 (81%) |
| HMG-CoA Reductase inhibitors | 36 (49%) | 9 (52%) | 5 (31%) |
| Diseases | |||
| Ischemic Cardiomyopathy | 42 (57.5%) | 10 (58.8%) | 7 (43.7%) |
| Non-ischemic Cardiomyopathy | 31 (42.5%) | 7 (41.2%) | 9 (56.3%) |
| Diabetes | 30 (41%)* | 3 (18%) | 2 (13%) |
| Hypertension | 56 (77%) | 14 (82%) | 14 (88%) |
| Indication for ICD | |||
| Primary prevention | 22 (30.1%) | 2 (11.7%) | 2 (12.5%) |
| Secondary prevention | 51 (69.9%) | 15 (88.3%) | 14 (87.5%) |
ICD implantation and DFT testing
ICDs were implanted in all patients based on the clinical indications recommended by the guidelines available at the time period of the study (9). Standard techniques were used for ICD implantation and all patients received ICD in the left prepectoral region utilizing axillary/subclavian system. All DFT testing was done immediately following ICD implantation. Testing protocol required at least two successful shocks that terminated induced ventricular fibrillation with a minimum of 10 Joules (J) safety margin. A high DFT was defined as the DFT when the safety margin was less than 10 J.
In all cases DFT determination was performed through standard technique including induction of ventricular fibrillation by delivering shock on the ‘T’ wave and DFT testing by a “step-down,” (testing with 5 J decrements/increments) and “step down/step up” (2–3 J increments) protocol. If a subcutaneous coil was added during the implant due to high DFT, the DFT before the coil implantation was recorded as the programmed DFT. If a subcutaneous coil was not used, the lowest therapy, which reverted the patient to sinus rhythm, was recorded as the programmed DFT. Overall among ‘cases’ and ‘controls’, it was noted that 80% of the total number received a single coiled right ventricular(RV) lead (n=110) as compared to 20% who received dual coiled RV lead (n=28).
Statistical Analysis
To determine whether differences in the distribution of data existed between groups, Pearson’s Chi-Square was used for dichotomous variables and one-way analysis of variance (ANOVA) was used for continuous variables, including DFT. In cases where a significant ANOVA was determined, Tukey HSD posthoc test was used for multiple comparisons. For exploratory analyses, a two-tailed t-test or one-way analysis of covariance (ANCOVA) was used to compare between groups. In all cases a 95% confidence interval was used and statistical significance was set at p<0.05. Data were analyzed using SPSS (version 17) and Graphpad Prism (version 4) was used for the pictorial representations.
RESULTS
Patient characteristics
Table 1 shows the number of patients with ICD who were included in this study that had (1) reported no history of drug use (controls), (2) positive self reported history for cocaine use (cocaine group) or (3) positive self reported history for other illicit drug use (other illicit drugs group). Patients with a positive self reported history for other illicit drugs group included marijuana, non-prescription opioids (mainly heroin), or polydrug (use of 2 or more illicit drugs). Since the number of patients having positive self reported history for other illicit drugs besides cocaine was too low for proper statistical analysis, these users were grouped together. During data analysis, it was noticed that nearly all patients were African-American or Caucasian; therefore, no other racial groups were included in this study. Furthermore, a Pearson Chi-Square analysis of race by group, confirmed the obvious disparity among groups that all patients with a history of illicit drug use were African-American, and it showed that controls had a significantly different racial distribution than cocaine or other illicit drug users (χ2(2)=13.09, p<0.001). It is important to note that this finding should not be generalized to indicate erroneously that African-Americans use illicit drugs more than Caucasians or any other racial group. Because of the disparity in racial distribution among groups, only African-American non-drug using controls were used in the remainder of the data analyses to compare to cocaine and other illicit drug user groups and Caucasian controls were excluded (with the exception of the exploratory analysis by race).
Table 2 outlines select patient demographics, medication use, diseases and indication for ICD placement according to the groups. Important factors such as use of cardiovascular medications, and presence of hypertension were not different among groups. Analysis of continuous variables by one-way ANOVA showed that age (but not body mass index (BMI)) was statistically different among groups (F(2, 103)=6.5, p=0.002). Tukey HSD posthoc analysis revealed that the patients with no history of drug use (Controls) were on average older than the patients with a history of other illicit drug use (p=0.004), but not cocaine use (p=0.096). This suggested that among those African-American patients requiring an ICD, patients with a history of illicit drug use required ICD implantation at an earlier age compared to their non-drug using counterparts.
The mean ejection fraction (EF) of the control group was found to be 30.5±15.2% which was comparable to the mean EF of the cocaine group (25.6±24.7%), where as the mean EF for the other illicit drugs group was 15.6±15.1%. With regard to the etiology of cardiomyopathy, it was ischemic in 57.5%, 58.5% and 43.7% in the control, cocaine and other illicit drug group respectively, where as the remaining were classified as non-ischemic. The indication for ICD was more for secondary prevention than primary, across all the three groups. (Table 2). The use of subcutaneous coils in the three groups was 12% (controls), 18% (cocaine) and 6% (other illicit drugs).
Comparison of Defibrillation Threshold values
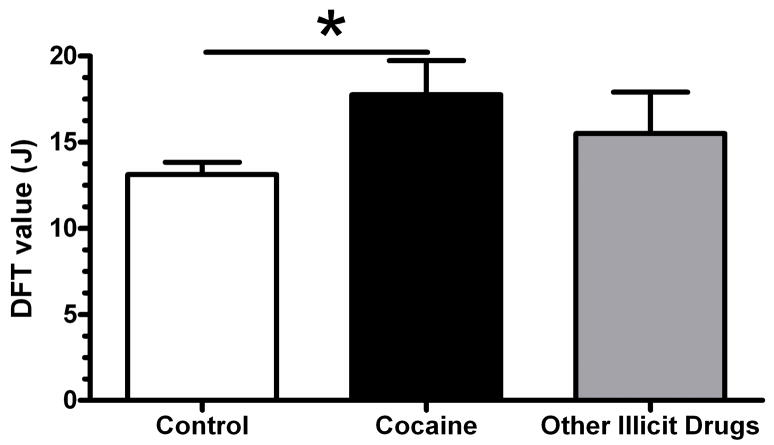
Figure 1 illustrates DFT values among different drug using groups and shows that one-way ANOVA revealed a significant difference among groups (F(2, 100)=3.277, p=0.042). Tukey HSD posthoc analysis showed that a history of cocaine use (p=0.043), but not previous use of other illicit drugs (including marijuana, non-prescription opioids like heroin, and polydrug use; p=0.45), was significantly different from matched no-drug using control group.
Figure 1. A history of cocaine use increases defibrillation threshold (DFT) in African-Americans with implanted cardioverter defibrillator.
One-way ANOVA showed that previous cocaine use, but not previous use of other illicit drugs (including marijuana, non-prescription opioids, and polydrug use) was significantly different from matched non-drug using controls. Data are presented as the mean ± standard error of the mean and *p<0.05 (Tukey HSD multiple comparisons). Samples sizes were Control=73, Cocaine=17, and Other Illicit Drugs=16.
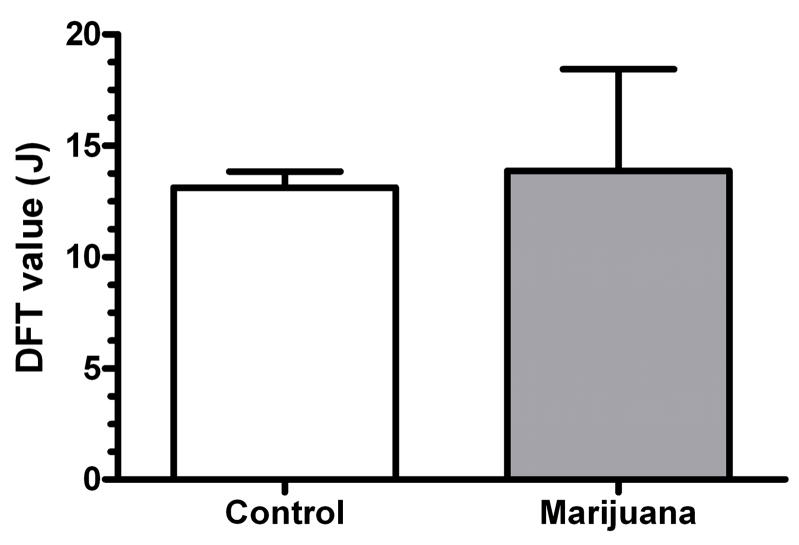
An exploratory analysis comparing the DFT values between patients with ICD that either have no history of drug use (controls) or those with a history of marijuana use was also performed (Figure 2). This was done because the marijuana group size was at the marginal level for proper statistical analysis (N=8). A two-tailed t-test between controls (non-drug users) and marijuana users revealed that no difference existed between the two groups. These data suggest that the non-significant increased trend seen in the other illicit drugs group compared to control group in Figure 1 was likely not due to previous marijuana use.
Figure 2. A history of marijuana use has no effect on defibrillation threshold (DFT) in African-Americans with implanted cardioverter defibrillator.
As an exploratory analysis, a two-tailed t-test showed that previous marijuana use was not significantly different from matched non-drug using controls. Note that the sample size for previous marijuana use was N=8, while the control sample size was N=73. Data are presented as the mean ± standard error of the mean.
As another exploratory analysis, a comparison of DFT values within the control group was made based on race between African-Americans and Caucasians as it was noticed that the DFT values were different within the original data set that included both racial groups. For this analysis, a one-way ANCOVA on DFT by race with BMI as cofactor was used. BMI was used as a covariable here because published data have shown that body weight affects DFT values (2). Figure 3 illustrates that race may play a key factor in DFT values in patients with ICD (F(1,79)=8.532, p=0.005) and that BMI does not account for this difference (F(1,79)=0.449, p=0.505). In patients with ICD and no history of drug use, African-Americans required higher DFT values than Caucasians during ICD testing.
Figure 3. Defibrillation threshold (DFT) values in African-Americans and Caucasians with implanted cardioverter defibrillator.
As an exploratory analysis, a one-way ANCOVA on DFT by race with body mass index as covariable showed that race may play a key factor in DFT in patients with implanted cardioverter defibrillator. African-Americans (N=73) were significantly different from Caucasians (N=32) and had higher DFTs. Data are presented as the mean ± standard error of the mean and *p<0.05 (ANCOVA).
DISCUSSION
Several factors including medications and illicit drugs have been shown to affect the DFT. A previously published study evaluated the role of cocaine use in increasing DFT and found that habitual cocaine use was associated with higher DFT values during ICD implantation (8). This was the first report to show that an illicit, recreational drug could affect DFT; however, the study was limited by lack of control for difference in race between non-drug users and cocaine users.
Among the various deleterious effects of recreational drugs, damage to the cardiovascular system is a well documented one. Cocaine use in particular has been reported to cause extensive cardiovascular complications such as myocardial ischemia, coronary artery spasm, acute myocardial infarction, myocarditis, endocarditis, cardiomyopathy, cardiac arrhythmias and sudden cardiac death (10). A wide range of cardiac electrophysiological abnormalities like bundle branch block, supraventricular arrhythmias, ventricular tachycardia, ventricular fibrillation and torsades de pointes have all been reported (10). Although the precise mechanism by which cocaine increases defibrillation threshold during ICD placement cannot be elucidated at this point, the mechanisms of action of cocaine may provide insight into the pathophysiology. As a sympathomimetic drug, cocaine increases ventricular irritability and may lower thethreshold for fibrillation. Alternatively, the sodium-channel–blockingeffects of cocaine inhibits the generationand conduction of the action potential reflected as a prolongation of the QRS and QT intervals. Cocaine also increasesthe intracellular calcium concentration, which may result in after-depolarizations and trigger the ventricular arrhythmia in the first place (10). Finally, increase in DFT may be due to the cocaine-induced myocardial abnormalities such as left ventricular hypertrophy, dilated cardiomyopathy and myocarditis resulting in leucocytic infiltration with contraction band formations. (7) Additionally, post-mortem histopathology of the conduction system of the heart in chronic cocaine abusers have shown severe thickening of the atrioventricular node artery, intranodal and perinodal fibrosis, and microscopic foci of chronic inflammatory infiltration (11). These diffuse structural changes in the myocardial geometry may facilitate new propagating wave fronts during the post shock isoelectric window period thus perpetuating the ventricular fibrillation culminating in elevated DFT.
Marijuana, on the other hand has been associated with a number of acute effects on the heart such as increased heart rate, increased cardiac output and orthostatic hypotension with tolerance developing with repeated use (12). Although marijuana has the potential to produce cardiac arrhythmias, the chronic effects of marijuana on heart are scant (13). In this study, a history of marijuana use alone did not affect DFT values in African-Americans with ICD. When considering this preliminary finding on the data obtained for the other illicit drugs group, it is tempting to speculate that the non-significant increased trend seen in this group is a result of opioid use or polydrug use. To this end, the synthetic opioid fentanyl has been previously shown to increase the DFT during ICD implantation in humans (14). The effects of opioid use, such as heroin, need to be studied in detail, and such studies should consider polydrug use as a separate group when investigating DFT values and related cardiovascular parameters.
There have been no previous studies showing the association between race and DFT during ICD placement. Although Chen et al. did not explicitly conclude the association between race and high DFT; the majority of patients in the cocaine use group were African Americans. (8) However, on a closer look, it is evident that considerable differences existed in the distribution of race between their ‘cocaine abusers’ (72.7% African American, 18.2% Caucasian and 9.1% Asian) and their control group (24.4% African American, 64.7% Caucasians, 9.2% Hispanics, 1.7% Asians). Additionally, their sample size of the cocaine users was small (N=11) and the study focused only on one illicit drug use. In our study, larger sample sizes were analyzed, included patients with exposure to marijuana and disparities among racial background have been adjusted. Hence, we believe that this is the first report of a statistically significant increased DFT in African-Americans as compared to Caucasians (among our non-drug users). This finding may be viewed as hypothesis generating, with significant scope for future research. Due to a paucity of studies investigating differences in cardiovascular diseases between races, the probable cause of increased DFT in African Americans remains speculative. The presence of intrinsic differences in the myocardial substrate with potential for cardiovascular co-morbidities like cardiomyopathy, coronary artery disease and cardiac failure may account for the increased DFT in African-Americans as compared to Caucasians.
Limitations of the study
Being a retrospective study, one of the possible limitations may be the lack of predefined protocols for the measurement of DFT, configuration of electrodes, or duration of ventricular fibrillation. However, given the probabilistic nature of defibrillation threshold, and the fact that there were no major changes in the methodology or procedures of DFT testing at our center during the course of the study, these factors are not likely to have affected the data. Since self reported drug use was obtained from records and used to establish groups, a few limitations became apparent and unavoidable. For example, a detailed history of drug use was not available, which limited analyses such as acute versus chronic drug use or recent versus past drug use. Furthermore, lack of urine drug screens in all patients may make the control group less clean (i.e. the control group may have contained drug users that did not report use). While greater characterization of groups was desired, the fact that self reported history of drug use was used may be a strength rather than a weakness because potential inclusion of cocaine users in the control group did not weaken the observed effect on DFT between control and cocaine groups.
Conclusions
The most significant finding of this study is that previous cocaine use increases DFT during ICD implantation among African-Americans. However, previous use of marijuana does not significantly influence DFT, although confirmation of this finding is required. It was also found that African-American patients with a history of illicit drug use had an indication for ICD implantation at an earlier age compared to the non-drug using patients. Preliminary findings also indicate that the African-Americans had higher DFT compared to Caucasians among non illicit drug users.
The risk of encountering high DFT should be considered when implanting ICDs in habitual cocaine users. Furthermore, continued use of cocaine in such patients after ICD implantation may further worsen DFT, escalating the chances for ICD failure and hence patients should be counseled for drug abstinence. Additionally, in such patients who could not undergo or need to defer from DFT testing for any clinical reason, possibility of increased DFT should be anticipated and hence counter measures such as use of high energy ICDs, prophylactic additional subcutaneous coil etc should be considered to prevent ICD failure.
Acknowledgments
We hereby acknowledge that the National Institute on Drug Abuse (K01DA024760 and L30DA027397 to SAP) in part, supported this work. The authors thank Brigid R. Waldron-Perrine for help with statistical analyses. This study was approved by the Human Investigation Committee at Wayne State University and complied with the guidelines set forth by the committee.
Abbreviations used
- ICD
implantable cardioverter defibrillator
- DFT
defibrillation threshold
- BMI
body mass index
- ANOVA
analysis of variance
- ANCOVA
analysis of covariance
References
- 1.Geddes LA, Tacker WA, Rosborough JP, Moore AG, Cabler PS. Electrical dose for ventricular defibrillation of large and small animals using precordial electrodes. J Clin Invest. 1974 Jan;53(1):310–9. doi: 10.1172/JCI107552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Jacob S, Abraham AE, McKelvey G. Anaesthetic drugs and defibrillation threshold testing. Drugs. 2008;68(13):1921–2. doi: 10.2165/00003495-200868130-00012. author reply 2–3. [DOI] [PubMed] [Google Scholar]
- 3.Dopp AL, Miller JM, Tisdale JE. Effect of drugs on defibrillation capacity. Drugs. 2008;68(5):607–30. doi: 10.2165/00003495-200868050-00004. [DOI] [PubMed] [Google Scholar]
- 4.Jacob S, Pidlaoan V, Singh J, Bharadwaj A, Patel MB, Carrillo A. High defibrillation threshold: the science, signs and solutions. Indian Pacing Electrophysiol J. 2010;10(1):21–39. [PMC free article] [PubMed] [Google Scholar]
- 5.Epstein AE, Ellenbogen KA, Kirk KA, Kay GN, Dailey SM, Plumb VJ. Clinical characteristics and outcome of patients with high defibrillation thresholds. A multicenter study. Circulation. 1992 Oct;86(4):1206–16. doi: 10.1161/01.cir.86.4.1206. [DOI] [PubMed] [Google Scholar]
- 6.Nagai T, Kurita T, Satomi K, Noda T, Okamura H, Shimizu W, et al. QRS prolongation is associated with high defibrillation thresholds during cardioverter-defibrillator implantations in patients with hypertrophic cardiomyopathy. Circ J. 2009 Jun;73(6):1028–32. doi: 10.1253/circj.cj-08-0744. [DOI] [PubMed] [Google Scholar]
- 7.Kloner RA, Hale S, Alker K, Rezkalla S. The effects of acute and chronic cocaine use on the heart. Circulation. 1992 Feb;85(2):407–19. doi: 10.1161/01.cir.85.2.407. [DOI] [PubMed] [Google Scholar]
- 8.Chen J, Naseem RH, Obel O, Joglar JA. Habitual cocaine use is associated with high defibrillation threshold during ICD implantation. J Cardiovasc Electrophysiol. 2007 Jul;18(7):722–5. doi: 10.1111/j.1540-8167.2007.00834.x. [DOI] [PubMed] [Google Scholar]
- 9.Gregoratos G, Abrams J, Epstein AE, Freedman RA, Hayes DL, Hlatky MA, et al. ACC/AHA/NASPE 2002 Guideline Update for Implantation of Cardiac Pacemakers and Antiarrhythmia Devices--summary article: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (ACC/AHA/NASPE Committee to Update the 1998 Pacemaker Guidelines) J Am Coll Cardiol. 2002 Nov 6;40(9):1703–19. doi: 10.1016/s0735-1097(02)02528-7. [DOI] [PubMed] [Google Scholar]
- 10.Lange RA, Hillis LD. Cardiovascular complications of cocaine use. N Engl J Med. 2001 Aug 2;345(5):351–8. doi: 10.1056/NEJM200108023450507. [DOI] [PubMed] [Google Scholar]
- 11.Michaud K, Augsburger M, Sporkert F, Bollmann M, Krompecher T, Mangin P. Interpretation of lesions of the cardiac conduction system in cocaine-related fatalities. J Forensic Leg Med. 2007 Oct;14(7):416–22. doi: 10.1016/j.jflm.2007.02.003. [DOI] [PubMed] [Google Scholar]
- 12.Jones RT. Cardiovascular system effects of marijuana. J Clin Pharmacol. 2002 Nov;42(11 Suppl):58S–63S. doi: 10.1002/j.1552-4604.2002.tb06004.x. [DOI] [PubMed] [Google Scholar]
- 13.Kosior DA, Filipiak KJ, Stolarz P, Opolski G. Paroxysmal atrial fibrillation following marijuana intoxication: a two-case report of possible association. Int J Cardiol. 2001 Apr;78(2):183–4. doi: 10.1016/s0167-5273(00)00459-9. [DOI] [PubMed] [Google Scholar]
- 14.Weinbroum AA, Glick A, Copperman Y, Yashar T, Rudick V, Flaishon R. Halothane, isoflurane, and fentanyl increase the minimally effective defibrillation threshold of an implantable cardioverter defibrillator: first report in humans. Anesth Analg. 2002 Nov;95(5):1147–53. doi: 10.1097/00000539-200211000-00004. table of contents. [DOI] [PubMed] [Google Scholar]