Abstract
Introduction
Cavernous hemangiomas represent the most common benign primary hepatic neoplasm, often being incidentally detected. Although the majority of hepatic hemangiomas remain asymptomatic, symptomatic hepatic hemangiomas can present with abdominal pain, hemorrhage, biliary compression, or a consumptive coagulopathy. The optimal surgical management of symptomatic hepatic hemangiomas remains controversial, with resection, enucleation, and both deceased donor and living donor liver transplantation having been reported.
Case Report
We report the case of a patient found to have a unique syndrome of multiorgan cavernous hemangiomatosis involving the liver, lung, omentum, and spleen without cutaneous involvement. Sixteen years following her initial diagnosis, the patient suffered from intra-abdominal hemorrhage due to her giant cavernous hepatic hemangioma. Evidence of continued bleeding, in the setting of Kasabach-Merritt Syndrome and worsening abdominal compartment syndrome, prompted MELD exemption listing. The patient subsequently underwent emergent liver transplantation without complication.
Conclusion
Although cavernous hemangiomas represent the most common benign primary hepatic neoplasm, hepatic hemangioma rupture remains a rare presentation in these patients. Management at a center with expertise in liver transplantation is warranted for those patients presenting with worsening DIC or hemorrhage, given the potential for rapid clinical decompensation.
Keywords: Hepatic hemangioma, Kasabach-Merritt syndrome, Liver transplantation
Introduction
Cavernous hemangiomas represent the most common benign primary hepatic neoplasm, with a reported prevalence of 3% to 20% based upon autopsy series.1 These congenital vascular malformations are microscopically composed of cavernous vascular channels that are lined by single layers of flattened endothelium separated by fibrous septae. The majority of hepatic hemangiomas are less than 5 cm in size, solitary, and rarely symptomatic. There is a reported female-to-male ratio of up to 6:1, and most hepatic hemangiomas frequently present within the fourth to fifth decade of life. In 1970, Adam et al. reported a series of 106 hemangioma resections over a 30-year period and delineated hemangiomas >4 cm as “giant”.2 Giant hepatic hemangiomas represent <10% of all hepatic hemangiomas.3 We describe here a report of emergent liver transplantation for a ruptured giant hepatic hemangioma in a patient with a unique syndrome of multiorgan cavernous hemangiomatosis.
Case Report
In September of 2003, a 32-year-old Caucasian female presented to an outside institution with a chief complaint of increasing abdominal fullness for 2 months. The patient reported mild abdominal discomfort during her daily activities, as well as decreased appetite and early satiety. Her past medical history was significant for an incidentally diagnosed liver mass in 1994 when she had undergone an abdominal computed tomographic (CT) scan as part of a workup for amenorrhea. At that time, the 10-cm well-marginated hypodense mass in the right lobe of the liver was confirmed to be a hemangioma by subsequent nuclear scan, and no further treatment was initiated. On her subsequent presentation in 2003, the patient was found to have massive hepatomegaly and thus underwent laparoscopic biopsy of the hepatic lesion. Pathology revealed a benign cavernous hemangioma, and the patient was then transferred to our institution for further evaluation.
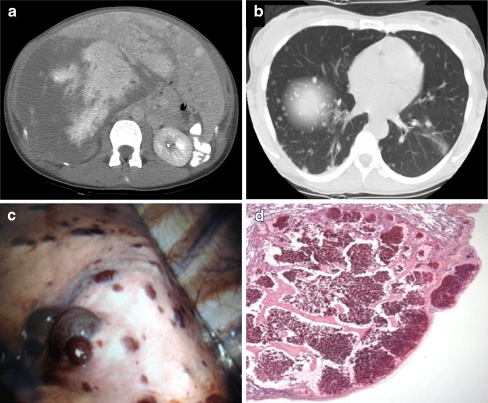
On admission, the patient's laboratory values were notable for a total bilirubin of 2.1 mg/dL (normal range, 0.3–1.3) and an international normalized ratio (INR) of 1.4. Serum tumor markers were all within normal limits. CT scan of the abdomen and chest showed numerous, large hypervascular liver masses, the largest measuring 18 × 23 cm (Fig. 1a), splenic hemangiomas, as well as innumerable bilateral pulmonary nodules (Fig. 1b). Given the multiorgan presentation raising concern for a metastatic neoplasm, the patient underwent video-assisted thoracoscopic surgery which demonstrated diffuse, purple, raised, subpleural nodules (Fig. 1c). The lung biopsy demonstrated pulmonary cavernous hemangiomas (Fig. 1d). Additional stains for both CD34 and CD31 highlighted the benign endothelial cell lining of the vascular spaces. In addition, HMB-45 staining was negative, ruling out lymphangioleiomyomatosis. The patient was discharged from the hospital and started on interferon alpha-2b in an attempt to shrink her hepatic and pulmonary lesions; this resulted in mild radiological and symptomatic improvement. Given the size and number of her lesions, it was felt that curative liver resection was not technically possible and that ultimately she might require liver transplantation. The patient was listed for transplantation, but over the ensuing years she remained stable.
Fig. 1.
a Initial abdominal CT at presentation in 2003 showing the largest lesion (18.1 × 15.9 cm) measured at level of the right portal vein and the second largest lesion was 4.3 × 3.5 cm. b Initial chest CT in 2003 revealing innumerable pulmonary nodules. c Video-assisted thoracoscopic surgery (VATS). Diffuse hemorrhagic, purple/red, raised nodules are seen on the surface of the lung. Biopsy of these lesions revealed benign cavernous hemangiomas. d Photomicrograph of an H&E-stained section of cavernous hemangioma in a lung biopsy specimen (40×). The lung lesions were small and well-circumscribed with benign endothelial cells and thin vessel walls and septa composed predominantly of fibrous tissue.
In January of 2010, the patient developed severe mid-abdominal pain while riding a horse. She subsequently suffered a syncopal episode and was taken to the emergency room where she was found to be hypotensive with a hematocrit of 22%. She was transfused 4 units of blood and transferred to our facility. On arrival, she was in no distress and hemodynamically stable. Her exam was significant for markedly increased abdominal distension (Fig. 2a). Her admission weight was 84 kg. Laboratory values demonstrated a hematocrit of 24.6%, INR of 2.1, fibrinogen of 78 mg/dL, platelets of 99,000 × 106/L (decrease from her baseline of 180,000 × 106/L), creatinine of 0.61 mg/dL, and a total bilirubin of 4.4 mg/dL. Her admission Model for End-Stage Liver Disease (MELD) score was 20. A CT scan demonstrated a large amount of intra-peritoneal blood in addition to the known hepatic hemagiomas. Over the course of the subsequent 48 h, her abdominal distension worsened, and she developed progressive lower extremity edema. Despite resuscitation with blood products, as well as the use of aminocaproic acid, she continued to demonstrate a consumptive coagulopathy with evidence of ongoing bleeding. Her abdominal compartment syndrome worsened, with evidence of decreased urinary output and rising creatinine levels. A petition to the United Network for Organ Sharing Regional Review Board requesting a high initial MELD to ensure life-saving emergent transplantation was submitted and approved.
Fig. 2.
a Intra-operative photo prior to start of liver transplantation demonstrating the patient's massive abdominal distension. b Giant cavernous hepatic hemangioma occupying the entire abdominal cavity. c Posterior aspect of gross liver specimen following resection and complete decompression (the white ruler on the specimen measures 15 cm in length and is on top of the left lobe). d Intra-operative photo at the completion of liver transplantation demonstrating the patient's abdomen.
On hospital day 14, a suitable donor became available. The recipient was brought to the operating room and explored. Four liters of old blood, with no evidence of clot, were evacuated. There were no immediate signs of active bleeding. The liver occupied her entire abdomen, the majority of which showed the appearance of a massive cavernous hemangioma (Fig. 2b). The omentum contained innumerable berry-sized hemangiomas. The patient had a conventional main hepatic artery, as well as replaced right and left hepatic arteries. These were individually ligated and divided. Clamps were then placed on the supra-hepatic inferior vena cava (IVC), infra-hepatic IVC, and portal vein. The liver was then drained of a large volume of blood to facilitate the completion of the posterior dissection under improved visualization. The liver was excised (Fig. 2c), and the donor allograft was brought to the operative field. A bicaval anastomosis, followed by a portal vein anastomosis, was performed. Given the small caliber size of each of the recipient's hepatic arteries, the arterial anastomosis was done directly to the supraceliac aorta. Biliary drainage was achieved by choledochocholedochostomy. Following completion of the liver transplant (Fig. 2d), the patient was extubated in the operating room and transferred to the intensive care unit. She was subsequently transferred to the transplant ward on post-operative day 1 and discharged home on post-operative day 11 following an uneventful post-operative course. On outpatient follow-up, the patient remains well and has begun to resume a normal level of activity.
The patient's weight at the time of discharge was 46 kg, a net loss of 38 kg from her pre-transplant weight. Histological examination of the liver revealed multiple areas of dilated blood-filled spaces lined by a layer of flattened endothelial cells, thus confirming the diagnosis of cavernous hepatic hemangioma. These changes occupied the entire right lobe and the majority of the left lobe of the liver.
Discussion
The majority of hepatic hemangiomas are asymptomatic and require no intervention. Indeed, advances in imaging technology, as well as the widespread application of diagnostic imaging, has resulted in the more frequent detection of hepatic hemangiomas.4 For those with symptomatic lesions, right upper quadrant pain or fullness is the most common complaint. Whereas 40% of patients with 4-cm hemangiomas are symptomatic, 90% of patients with 10-cm hemangiomas are symptomatic.5 Giant hemangiomas can present with abdominal fullness or pain, hemorrhage within the hemangioma or within the abdominal cavity with associated hemodynamic compromise, jaundice due to compression of the biliary tree, cardiac failure from massive arteriovenous shunting, or as a consumptive coagulopathy (Kasabach-Merritt Syndrome). The latter syndrome of profound thrombocytopenia, microangiopathic hemolytic anemia, a consumptive coagulopathy, and an enlarging vascular lesion was first reported in 1940 as a case of thrombocytopenic purpura in a 2-month-old child who presented with a rapidly growing cutaneous hemangioma.6
The optimal surgical management of giant hepatic hemangiomas remains controversial with resection, enucleation, and both deceased donor and living donor liver transplantation having been reported.7–13 Surgical resection or enucleation has often been reserved for symptomatic, single-lobe lesions. Symptomatic patients with unresectable lesions, multiple bi-lobar hemangiomas, or those involving the hepatic hilum, have often been referred for consideration for liver transplantation. Our patient's clinical course was unique as she was monitored for years without change in clinical presentation and without limitations in her daily activities. Furthermore, the size and diffuse nature of her hepatic hemangiomas precluded liver resection. Consideration for living donor liver transplant prior to her acute presentation was deferred given her continued stability as an outpatient. Furthermore, our patient's rapid decline following presentation prevented the ability for timely living donor evaluation and thus required petition for MELD exemption to allow for emergent liver transplantation. Patients with hepatic hemangiomas who present with evidence of worsening DIC and/or hemorrhage should be referred emergently to centers with expertise in liver transplantation, given the potential for rapid decompensation.
Although previous reports on liver transplantation for giant hepatic hemangiomas have documented reversal of Kasabach-Merritt Syndrome,7–13 we believe this to be the first report of transplantation in the setting of hemorrhage from a giant hepatic hemangioma. Rupture of a hepatic hemangioma remains an extremely rare event, with a reported incidence of 1% to 4% 14 and a reported high rate of mortality (60–75%).15 A report from 2003 identified 32 published cases of spontaneous hepatic hemangioma rupture in adults, of which 27 cases were available for review.16 In the latter study, the mean hemangioma size was 14.8 cm. Four of the 27 patients died from hemorrhage without surgical intervention. Twenty-two of the remaining 23 patients underwent surgery (59% resection, 23% suture ligation, and 18% tamponade). Transcatheter arterial embolization was undertaken in 31% of patients prior to hepatic resection. Mortality for the different forms of surgical interventions was 23% for resection, 40% for suture ligation, and 75% for tamponade, with an overall mortality of 36%.16 There were no documented cases of hepatic hemangioma rupture managed with emergent liver transplantation.
Non-surgical treatment of giant hepatic hemangiomas in stable patients has been reported with mixed results and includes interferon administration, transarterial catheter embolization, and hepatic radiation therapy. Interferon has known anti-angiogenic properties, and a few case reports have described its efficacy in the treatment of vascular malformations and neoplasms.17 Our patient demonstrated minimal symptomatic and radiological improvement with interferon-alpha-2b administration. Small case series have reported radiotherapy as an effective means to limit or regress hemangioma growth, as well as decrease associated symptoms. Radiotherapy has often been administered at a dose ranging from 15 to 30 Gy in 15 to 22 fractions over a few weeks with minimal morbidity.18,19 It should be noted that the efficacy of radiation therapy in reversing the DIC associated with Kasabach-Merritt Syndrome has yet to be demonstrated. Hepatic arterial embolization has been reported to be the second most common form of treatment of symptomatic giant hemangiomas, with surgical resection being the most common.20 Transarterial embolization has been reported to provide symptomatic relief, as well as a reduction in hemangioma size.21,22 Indeed, the ability to perform catheter-directed therapy has circumvented the need for open hepatic artery ligation as a form of management for hepatic hemangiomas. However, the role of transarterial catheter embolization in the management of cavernous hepatic hemangiomas in the setting of Kasabach-Merritt Syndrome remains limited.23 Complications associated with embolization include liver infarction with associated abscess formation, as well as treatment failure associated with vessel recanalization following embolization.7 Superselective arterial embolization has been used for patients with hemorrhage from hepatic hemangioma rupture; however, this modality has been employed as a bridge to successful hepatic resection, rather than as a permanent treatment for ongoing hemorrhage.24
Conclusion
Herein, we describe a patient with massive hepatomegaly found to have what appears to be a unique syndrome of multiorgan cavernous hemangiomatosis of the liver, lung, omentum, and spleen without cutaneous involvement. Although the majority of hepatic hemangiomas remain asymptomatic, and thus require no intervention, symptomatic focal lesions can be addressed surgically by either enucleation or resection. More extensive symptomatic disease, as demonstrated in our patient, necessitates liver transplantation. Our patient suffered from ongoing intra-abdominal hemorrhage in the setting of Kasabach-Merritt Syndrome, with associated abdominal compartment syndrome. Her continued clinical decompensation required MELD exemption listing and thus allowed for emergent liver transplantation.
Acknowledgments
Open Access
This article is distributed under the terms of the Creative Commons Attribution Noncommercial License which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
Contributor Information
Parsia A. Vagefi, Phone: +1-415-3531888, FAX: +1-415-3532102, Email: parsia.vagefi@ucsfmedctr.org
Ingo Klein, Email: ingo.klein@ucsfmedctr.org.
Bruce Gelb, Email: Bruce.Gelb@ucsfmedctr.org.
Bilal Hameed, Email: Bilal.Hameed@ucsf.edu.
Stephen L. Moff, Email: smoff@alumni.duke.edu
Jeff P. Simko, Email: jeff.simko@ucsf.edu
Oren K. Fix, Email: oren.fix@ucsf.edu
Helge Eilers, Email: eilersh@anesthesia.ucsf.edu.
John R. Feiner, Email: feinerj@anesthesia.ucsf.edu
Nancy L. Ascher, Email: Nancy.Ascher@ucsfmedctr.org
Chris E. Freise, Email: Chris.Freise@ucsfmedctr.org
Nathan M. Bass, Email: nathan.bass@ucsf.edu
References
- 1.Choi BY, Nguyen MH. The diagnosis and management of benign hepatic tumors. J Clin Gastroenterol. 2005;39(5):401–12. doi: 10.1097/01.mcg.0000159226.63037.a2. [DOI] [PubMed] [Google Scholar]
- 2.Adam YG, Huvos AG, Fortner JG. Giant hemangiomas of the liver. Ann Surg. 1970;172:239–245. doi: 10.1097/00000658-197008000-00010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lopez-Arce G, Barahona-Garrido J, Tellez-Avila F, et al. A giant hepatic hemangioma treated successfully with hepatic enucleation. Ann Hepatol. 2009;8(4):377–378. [PubMed] [Google Scholar]
- 4.Assy N, Nasser G, Djibre A, et al. Characteristics of common solid liver lesions and recommendations for diagnostic workup. World J Gastroenterol. 2009;15(26):3217–3227. doi: 10.3748/wjg.15.3217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Goodman Z. Benign tumors of the liver. In: Okuda K, Ishak KG, editors. Neoplasms of the liver. Tokyo: Springer-Verlag; 1987. pp. 105–125. [Google Scholar]
- 6.Kasabach HH, Merritt KK. Capillary hemangioma with extensive purpura. American Journal of Diseases in Children; 1940;59:1063–1070. [Google Scholar]
- 7.Hochwald SN, Blumgart LH. Giant hepatic hemangioma with Kasabach-Merritt syndrome: is the appropriate treatment enucleation or liver transplantation? HPB Surg. 2000;11(6):413–419. doi: 10.1155/2000/25954. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Longeville JH, de la Hall P, Dolan P, et al. Treatment of a giant haemangioma of the liver with Kasabach-Merritt syndrome by orthotopic liver transplant: a case report. HPB Surg. 1997;10(3):159–162. doi: 10.1155/1997/10136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Klompmaker IJ, Sloof MJ, van der Meer J, et al. Orthotopic liver transplantation in a patient with a giant cavernous hemangioma of the liver and Kasabach-Merritt syndrome. Transplantation. 1989;48(1):149–151. doi: 10.1097/00007890-198907000-00035. [DOI] [PubMed] [Google Scholar]
- 10.Ferraz AA, Sette MJ, Maia M, et al. Liver transplant for the treatment of giant hepatic hemangioma. Liver Transpl. 2004;10(11):1436–1437. doi: 10.1002/lt.20250. [DOI] [PubMed] [Google Scholar]
- 11.Concejero AM, Chen CL, Chen TY, et al. Giant cavernous hemangioma of the liver with coagulopathy: adult Kasabach-Merritt syndrome. Surgery. 2009;145(2):245–247. doi: 10.1016/j.surg.2007.07.039. [DOI] [PubMed] [Google Scholar]
- 12.Meguro M, Soejima Y, Taketomi A, et al. Living donor liver transplantation in a patient with giant hepatic hemangioma complicated by Kasabach-Merritt syndrome: report of a case. Surg Today. 2008;38(5):463–468. doi: 10.1007/s00595-007-3623-4. [DOI] [PubMed] [Google Scholar]
- 13.Kumashiro Y, Kasahara M, Nomoto K, et al. Living donor liver transplantation for giant hepatic hemangioma with Kasabach-Merritt syndrome with a posterior segment graft. Liver Transpl. 2002;8(8):721–724. doi: 10.1053/jlts.2002.33689. [DOI] [PubMed] [Google Scholar]
- 14.Cappellani A, Zanghì A, Di Vita M, et al. Spontaneous rupture of a giant hemangioma of the liver. Ann Ital Chir. 2000;71(3):379–383. [PubMed] [Google Scholar]
- 15.Brouwers MA, Peeters PM, de Jong KP, et al. Surgical treatment of giant haemangioma of the liver. Br J Surg. 1997;84(3):314–316. doi: 10.1002/bjs.1800840310. [DOI] [PubMed] [Google Scholar]
- 16.Corigliano N, Mercantini P, Amodio PM, et al. Hemoperitoneum from a spontaneous rupture of a giant hemangioma of the liver: report of a case. Surg Today. 2003;33(6):459–463. doi: 10.1007/s10595-002-2514-z. [DOI] [PubMed] [Google Scholar]
- 17.Wu JM, Lin CS, Wang JN, et al. Pulmonary cavernous hemangiomatosis treated with interferon alfa-2a. Pediatric Cardiology. 1996;17:332–334. doi: 10.1007/s002469900074. [DOI] [PubMed] [Google Scholar]
- 18.Gaspar L, Mascarenhas F, da Costa MS, et al. Radiation therapy in the unresectable cavernous hemangioma of the liver. Radiother Oncol. 1993;29(1):45–50. doi: 10.1016/0167-8140(93)90172-5. [DOI] [PubMed] [Google Scholar]
- 19.Biswal BM, Sandhu M, Lal P, et al. Role of radiotherapy in cavernous hemangioma liver. Indian J Gastroenterol. 1995;14(3):95–98. [PubMed] [Google Scholar]
- 20.Hobbs KE. Hepatic hemangiomas. World J Surg. 1990;14:468–471. doi: 10.1007/BF01658669. [DOI] [PubMed] [Google Scholar]
- 21.Zeng Q, Li Y, Chen Y, et al. Gigantic cavernous hemangioma of the liver treated by intra-arterial embolization with pingyangmycin-lipiodol emulsion: a multi-center study. Cardiovasc Intervent Radiol. 2004;27(5):481–485. doi: 10.1007/s00270-003-2754-2. [DOI] [PubMed] [Google Scholar]
- 22.Srivastava DN, Gandhi D, Seith A, et al. Transcatheter arterial embolization in the treatment of symptomatic cavernous hemangiomas of the liver: a prospective study. Abdom Imaging. 2001;26(5):510–514. doi: 10.1007/s00261-001-0007-x. [DOI] [PubMed] [Google Scholar]
- 23.Malagari K, Alexopoulou E, Dourakis S, Kelekis A, Hatzimichail K, Sissopoulos A, et al. Transarterial embolization of giant liver hemangiomas associated with Kasabach-Merritt syndrome: a case report. Acta Radiol. 2007;48(6):608–612. doi: 10.1080/02841850701326917. [DOI] [PubMed] [Google Scholar]
- 24.Soyer P, Levesque M. Haemoperitoneum due to spontaneous rupture of hepatic haemangiomatosis: treatment by superselective arterial embolization and partial hepatectomy. Australas Radiol. 1995;39(1):90–92. doi: 10.1111/j.1440-1673.1995.tb00243.x. [DOI] [PubMed] [Google Scholar]