Abstract
Introduction. Sports activities play an important role in today’s society. However, as more people become involved in these activities, the number of sports-related injuries also increases. In the Netherlands, 3.5 million sports injuries occur annually. Twenty per cent of these injuries are first seen by a GP. Little is known about the epidemiology of these injuries in general practice. This study has been conducted to determine the incidence and prevalence of sports-related injuries in general practice and to provide information about the nature and treatment of these injuries.
Methods. Survey study conducted in 612 patients with sports-related injuries by 21 GP trainees in as many GP practices. Inclusion of study subjects took place between September 2007 and April 2009.
Results. In total, 694 sports-related injuries were registered. The incidence of sports-related injuries was 23.7 in 1000 patients and prevalence 27.8 in 1000 patients. Soccer-related injuries are most prominent in this population, lower extremities being three times more often involved than upper extremities. GPs often (60.9%) used a symptom-based diagnosis. In 80% of the cases, no additional diagnostic testing took place, while in 36.5% of the cases, only explanation and advice sufficed. Few patients were referred to the hospital (6.6%).
Discussion. Patients with sports-related injuries regularly consult GPs (on average one to two times per week). GPs tend to use non-specific diagnoses in sports-related injuries. In part, this may be due to the lack of specific diagnoses available in the current registration system (International Classification of Primary Care). Most often these injuries require only explanation and medical advice from the GP. Usually, additional tests or hospital referrals are not necessary. Presumably, mostly patients with mild sports-related injuries consult the GP.
Keywords: Epidemiology, general practitioner, sports-related injuries
Introduction
Sporting activities play an important role in current society. In the Netherlands, ∼46% of its 16 million people participate in sports activities at an organized or non-organized level.1 In addition to its health benefits,2 sports activities may lead to injuries. A national survey revealed that 3.5 million new sports injuries occur each year in the Netherlands. Most of these injuries (82%) display a sudden cause and 40% of these injuries require medical attention. Approximately half of the injuries are seen by a GP.3 In this population-based survey, Internet has replaced the telephone as the source for response entry since 2006. After this transition, more than a doubling of the registered number of sports injuries was observed.4 However, research based on population studies only generates information at an aggregated level that cannot be extrapolated to individual patients. To be informed more accurately, research at a patient–physician level is needed.
In one study that took place in Dutch GP practices, an incidence of sports injuries of 23.1 in 1000 patients was found.5 Another study reported that a least 39 patients/year consulted a GP for a new sport injury.6 However, the study populations in both Dutch studies were small and this information may be outdated as nowadays more people are involved in sports.7
Therefore, up-to-date information about the epidemiology of sport injuries in general practices in the Netherlands is needed. However, adequate registration of sports injuries is difficult to materialize because the current registry system of Dutch GPs, the International Classification of Primary Care (ICPC), does not provide an option to register sports injuries.8,9 Moreover, Dutch GPs tend to use symptoms as a ‘working diagnosis’ in this ICPC.10
In addition, the registered diagnosis doesn’t incorporate any elements of ‘severity’ of a sports injury. This information is relevant because of its possible implications. Severity of sports injuries can be described on the basis of six criteria: the nature of the sports injury, the duration and nature of treatment, sporting time lost, working time lost, permanent damage and monetary costs.11 Finally, there is no uniformity in definitions of a sport injury applied in research studies. At present, rather than sports injury, the comprehensive term sports-related injury is used.12–14 This denotes any injury that affects the individuals’ ability to engage into sports activities irrespective of where this injury was sustained (Table 1). It, therefore, also incorporates injuries sustained during non-sports activities.
TABLE 1.
Definition of sports-related injury
| A sports-related injury is defined as:10,11 |
| An injury that has originated during or as a result of sports activities. |
| An injury that interrupts sports practice. |
| An injury, which is caused by a sudden event during sports participation or which originates gradually as a result of sports participation. |
| An injury, which originates during physical education and sports practice during ‘working’ time is also considered a sports injury. |
| An injury that originates during watching sports events is not considered a sports injury. |
A recent study in the Netherlands reports a change in trends of illnesses and symptoms presented to the GP. In particular, an increase in sports injuries is observed by the family physician.15 A literature search (up to April 2009) yielded no other relevant literature on the epidemiology of sports injuries in general practice.
In order to be more accurately informed about the magnitude of sports injuries in GP practices in the Netherlands, we conducted a survey intended to address the following questions:
What are the incidence and prevalence of sports-related injuries in GP practice?
Which diagnosis and treatment of sports-related injuries are registered by GPs?
Methods
Patients and methods
Patients consulting their GP with a sports-related injury were surveyed about their injury. Twenty-one GP trainees registered during their third year of the vocational training programme surveyed all patients with sports-related injuries in the GP trainers office. All participating GP trainers and GP trainees were associated with the department of General Practice of the University Medical Centre of Groningen. The GP trainees completed an Internet-based questionnaire (Appendix A) for each patient with a sports-related injury. The GP trainees used the ICPC diagnosis to register sports-related injuries. The inclusion period started in September 2007 and ended on 1 April 2009.
Results
In total, 694 questionnaires were completed by 612 patients and subsequently analysed, 584 of which involved new sports-related injuries. During the inclusion period, the mean registry period of the 21 GP trainees was 9 months. Most questionnaires contained no missing values. The mean age of the patients was 30.6 years (range: 6–84 years), 56.2% was male.
Incidence and prevalence of sports-related injuries
The incidence of sports-related injuries in this Dutch population consulting their GP was 23.7 per 1000 patients per year; the prevalence of sports-related injuries was 27.8 per 1000 patients per year.
Most of the patients with a sports-related injury experienced an acute origin (75%) of their injury, while 25.0% reported a gradual origin. Of all individuals with a sports-related injury, 58% was involved in organized sports and the remaining individuals in non-organized or during school activities. Almost two-thirds of the people (61.4.%) with a sports-related injury practiced sports between 0 and 3 hours/week and 32% between 3 and 6 hours, while 6.5% practiced >6 hours/week. On average, per week individuals spent 2.9 hours on activities related to sports. In our study population, most injuries occurred in soccer (Table 2). In order to assess season-related fluctuations, injuries sustained during three consecutive periods were registered.
TABLE 2.
“Top 10” injury-prone sports divided over three 6 months periods (N = 584, %)a
| Perioda |
Mean | |||
| 1 | 2 | 3 | ||
| Soccer | 27.4 | 25.0 | 25.6 | 26.2 |
| Running/jogging | 7.1 | 10.3 | 8.5 | 8.6 |
| Fitness | 9.7 | 4.3 | 6.0 | 6.7 |
| Volleyball | 3.5 | 6.0 | 7.3 | 6.3 |
| Speed skating | 4.4 | 0.9 | 9.1 | 6.0 |
| Tennis | 6.2 | 7.8 | 1.6 | 4.1 |
| Skiing | 0.9 | 4.3 | 4.4 | 3.8 |
| Field hockey | 7.1 | 1.7 | 3.5 | 3.6 |
| Walking/Nordic walking | 0.0 | 3.4 | 4.7 | 3.3 |
| Otherwise | 33.7 | 36.3 | 29.3 | 31.4 |
| Total | 100 | 100 | 100 | 100 |
Registration period—1: September 2007 to February 2008; 2: March 2008 to August 2008 and 3: September 2008 to February 2009. Values in bold are scores over the total registration period.
Diagnosis, diagnostic tests and treatment
Diagnosis.
In 92.5% of the registrations, the diagnosis of sports-related injuries (in accordance with ICPC) corresponded to the locomotor apparatus. The remaining groups (each all <1.5%) were registered as, for example, nervous system disorders, such as a commotio cerebri.
When sports-related injuries were categorized according to ICPC either as symptoms or diagnoses, overall 60.9% of sports-related injuries were diagnosed as a symptom, a so-called working diagnosis or symptom diagnosis. Table 3 presents the observed frequency of injury sites for sports-related injuries in our population, as categorized within the tractus locomotorius. An injury can be located at more than one site, for example a knee and muscle injury. A presentation of injury sites based on more ‘specific’ diagnoses, in accordance with the ICPC rubric, is presented in Table 4. Further division of sports-related injuries in upper or lower extremity injuries was made in 414 cases, with 76.8% of the injuries located in the lower extremities and 23.2% in the upper extremities.
TABLE 3.
Injury sites (N = 538, %)a
| Knee | 24.7 |
| Ankle | 18.8 |
| Muscles/not specified | 16.4 |
| Foot/toe | 7.4 |
| Shoulder | 7.2 |
| Back (including neck) | 5.9 |
| Arm (including elbow and wrist) | 5.5 |
| Leg (upper and lower) | 5.3 |
| Hand/finger | 5.0 |
| Hip | 2.4 |
| Rest | 1.5 |
| Total | 100.1 |
Based on only the tractus locomotorius.
TABLE 4.
ICPC (symptom) diagnoses (N = 578, %)
| Symptom diagnosis ‘top 5’ (ICPC L1–L29) | |
| L15: knee symptoms | 16.3 |
| L16: ankle symptoms | 8.3 |
| L17: foot/toe symptoms | 6.9 |
| L08: shoulder ymptoms | 5.7 |
| L14: leg/femur symptoms | 4.3 |
| Diagnosis ‘top 3’ (ICPC L70–L99) | |
| L77: ankle sprains/distorsions | 9.3 |
| L99: other disorders tractus locomotorius | 5.4 |
| L96: acute trauma meniscus/ligaments | 3.8 |
Diagnostic tests.
Table 5 shows the additional tests that the GP requested and registered in relation to ICPC diagnosis. ‘Overall’ represents all information collectively, while the other data pertain to the first consultations only. If tests were requested, X-rays were most common. In the majority of cases, no additional diagnostic test was ordered, while in ankle, hand/finger and foot/toe symptoms, X-ray is the most common diagnostic tool.
TABLE 5.
Additional tests or physiotherapy prescribed in relation to ICPC diagnosis (N = 578, %)
| None | X-ray | Physiotherapya | Laboratory | |
| Over all (N = 694%)b | 80.3 | 17.1 | 0.7 | 1.4 |
| L15: knee symptoms | 89.4 | 9.6 | 1.1 | 0.0 |
| L77: ankle sprains/distortions | 77.8 | 22.2 | 0.0 | 0.0 |
| L16: ankle symptoms | 62.5 | 35.4 | 2.1 | 0.0 |
| L17: foot/toe symptoms | 77.5 | 22.5 | 0.0 | 0.0 |
| L08: shoulder symptoms | 84.8 | 15.2 | 0.0 | 0.0 |
| L99: other diseases tractus locomotorius | 93.5 | 0.0 | 3.2 | 3.2 |
| L96: acute trauma menisci/ligaments | 95.5 | 0.0 | 4.5 | 0.0 |
| L14: leg/femur symptoms | 92.0 | 8.0 | 0.0 | 0.0 |
| L12: hand/finger symptoms | 61.9 | 38.1 | 0.0 | 0.0 |
| L02: back symptoms | 100.0 | 0.0 | 0.0 | 0.0 |
Physiotherapy used in diagnostic procedure.
All consultations.
Treatment.
In our study population, the majority of sports-related injuries did not require a specific treatment besides providing an explanation about injury-specific causes and mechanisms and medical advices (36.5%). If treatment was necessary, most frequently physical and remedial therapy was prescribed in addition to applying bandages (Table 6). Of all patients in this study, 6.6% was referred to a specialist (orthopaedic surgeon or sports physician).
TABLE 6.
Treatment applied to sports-related injuries (N = 578, %)a
| None, excluding advices GP | 36.5 |
| Physical and remedial therapy | 20.9 |
| Bandage/tape | 13.3 |
| Medication | 11.8 |
| Referral to orthopaedic surgeon | 3.8 |
| Referral to sports physician | 2.4 |
| Medication and physiotherapy and remedial therapy | 1.9 |
| Medication and referral to sports physician | 0.2 |
| Physiotherapy or remedial therapy and referral to sports physician | 0.2 |
| Otherwise | 9.0 |
| Total | 100 |
During the first consultation.
Discussion
This is one of the first studies, which has established the incidence and prevalence of sports-related injuries in GP practices in Northern Netherlands. The incidence and prevalence of sports-related injuries in GP practice in this study were 23.7 and 27.8, respectively, per 1000 patients per year. This implies that GPs are regularly consulted (on average one to two times per week) by patients with a sports-related injury. To put this in perspective, on average, a GP in the Netherlands maintains ∼135 to 140 patient contacts each week during regular office hours.16
The incidence we observed is comparable to the incidence reported in an earlier study by Baarveld et al.,5 which is based on the same definition of incidence. The minor difference in proportion between incidence and prevalence suggests that most of the patients with a sport-related injury consult the GP only once for a particular problem. In this study, mainly patients with mild sports-related injuries consult the GP. This presumption is based on the observation that in 80.3% of the cases, no additional tests were needed, not many follow-up consultations were necessary and only few patients were referred to the hospital (6.6%).
Evidently, seasons affect the frequency of type of injuries presented to the GP. During summertime, tennis injuries were more prevalent, while in winter, more injuries related to speed skating were observed. Knee and ankle injuries are the most common sports-related injuries reported in other studies. Muscle and tendon problems are on the rise in professional sports and now gradually predominate the joint injuries,17 but this trend is not observed in our study.
Of all registered diagnoses most are so-called symptom diagnoses. In one-third of the consultations, more specific diagnoses were registered by the GP, even though the registry system only offers few options for specification.
Comparing current epidemiological data of sports-related injuries in the Netherlands with the data in literature from other countries may not be valid as different definitions of sports-related injuries or sport injuries are applied and the variety in health care systems involved could affect the type of care patients receive. The ICPC registry system, used by almost all GPs in the Netherlands, does not allow for an adequate registration of sports-related injuries. The outcome of this study suggests that GPs are comfortable using non-specific diagnoses. Nonetheless, in order to better comprehend the magnitude and effects of these injuries on GP care, epidemiological data based on specific diagnoses are warranted. With the additional registry system used in this study, we obtained more specific information about sports-related injuries, negating the limitations imposed by the current ICPC system.
This study used a clear definition of sports-related injuries. However, even though the survey is easy to complete, it has not been validated. Moreover, generalizability of these results may be limited due to the particular GP trainees and patient population involved in this study.
Conclusions
The incidence and prevalence of sports-related injuries in GP practice were 23.7 and 27.8, respectively, implying that on average, GPs are consulted one to two times each week by a patient with a sports-related injury. Overall, it is fair to say that patients with a sports-related injury that consult a GP are mostly diagnosed non-specifically and receive mainly explanation and medical advice for their injury. Furthermore, this care is characterized by requesting few additional tests and hospital referrals. Presumably, patients with mild sports-related injuries mostly consult the GP. Additional information about the severity of these injuries is needed but the present registration system used by GPs in the Netherlands does not incorporate this option.
Declaration
Funding: none.
Conflict of interest: none.
Appendix A:
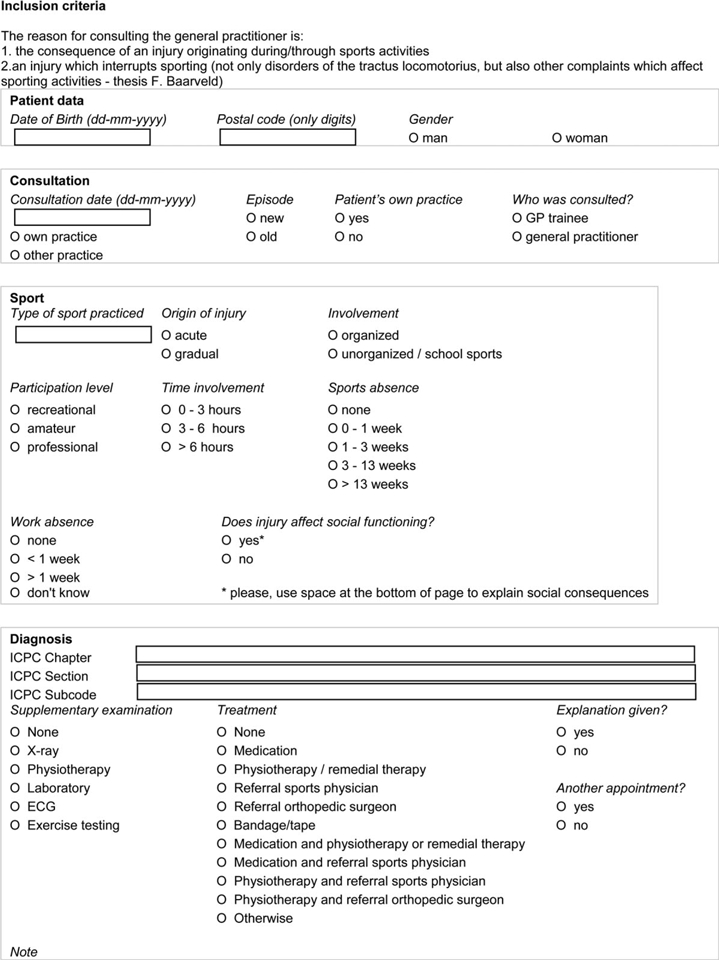 |
References
- 1.Schmikli SL, Schoots W, De Wit MJP. Sports Injuries, the Total Picture. Arnhem, The Netherlands: NOC*NSF; 2002. (Dutch) [Google Scholar]
- 2.Blair SN, Morris JN. Healthy hearts—and the universal benefits of being physically active: physical activity and health. Ann Epidemiol. 2009;19:253–6. doi: 10.1016/j.annepidem.2009.01.019. [DOI] [PubMed] [Google Scholar]
- 3.Schoots W, Vriend I, Stam C, Kloet S. Sports injuries in the Netherlands: a new and current review. Sport & Geneeskunde. 2009;42:16–23. (Dutch) [Google Scholar]
- 4.Vriend I, van Kampen B, Schmikli S, et al. Accidents and Movement and Mobility in the Netherlands 2000-2003. Amsterdam, The Netherlands: Consumer and Safety; 2005. (Dutch) [Google Scholar]
- 5.Baarveld F, van Enst GC, Meyboom-de Jong B, Schuiling J. Sports related injuries in family practice. Sport & Geneeskunde. 2003;36:117–21. (Dutch) [Google Scholar]
- 6.Maarsingh EJ, van Dijk FHM, Backx FJG. Sports injuries in family practice: a registration in the East-Veluwe region. Practitioner. 1992;9:537–44. (Dutch) [Google Scholar]
- 7.Tiessen-Raaphorst A, Breedveld K. Funding in Primary Care: Final Report. The Hague, The Netherlands: The Netherlands Institute for Social Research; 2009. [Google Scholar]
- 8.Lamberts H, Wood M. ICPC International classification of Primary Care. Oxford: Oxford University Press; 1987. [Google Scholar]
- 9.Baarveld F. Epidemiology of sports injuries in family practice. In: Baarveld F, Backx FJG, Voorn TB, editors. Sports Medicine. Houten, The Netherlands: Bohn Stafleu Van Loghum; 2009. (ISBN 978 90 313 4795 7) (Dutch) [Google Scholar]
- 10.Lamberts H. In the Family Physician’s Practice. A Transition Project Report. Lelystad, The Netherlands: Meditekst; 1991. p. 38. (Dutch) [Google Scholar]
- 11.van Mechelen W. The severity of sports injuries. Sports Med. 1997;24:176–80. doi: 10.2165/00007256-199724030-00006. [DOI] [PubMed] [Google Scholar]
- 12.Ministry of Public Health, Welfare and Sports. Sports, Movement and Health. Towards an Active Government’s Policy to Enhance Public Health Through and During Sports and Movement. The Hague, The Netherlands: Ministry of Public Health, Welfare and Sports; 2001. (Dutch) [Google Scholar]
- 13.Baarveld F. Sports Related Injuries in Family Practice (Thesis) Groningen, The Netherlands: UMCG; 2004. (ISBN 90 352 2739 5) (Dutch) [Google Scholar]
- 14.Burt CW, Overpeck MD. Emergency visits for sport-related injuries. Ann Emerg Med. 2001;37:301–8. doi: 10.1067/mem.2001.111707. [DOI] [PubMed] [Google Scholar]
- 15.Donker GA. Continuing Morbidity Registration Gauge stations 2007. Utrecht, The Netherlands: NIVEL; 2007. (Dutch) [Google Scholar]
- 16.Dijk van CE, Verhey RA, van den Hoogen H, de Bakker DH. Funding of Primary Care 2007. Utrecht, The Netherlands: NIVEL; 2009. (ISBN 978 90 6905 955 6) (Dutch) [Google Scholar]
- 17.Ekstrand J, Hägglund M, Waldén M. Injury incidence and injury patterns in professional football—the UEFA injury study. Br J Sports Med. 2009 Jun 23 doi: 10.1136/bjsm.2009.060582. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]


