Abstract
Background/Aim:
The role of laparoscopic appendectomy is still not well defined in the literature. This study was conducted to evaluate the feasibility of laparoscopic appendectomy at a university hospital in a developing country.
Patients and Methods:
Patients undergoing laparoscopic appendectomy (LA) from August 2002 to August 2006 were identified. For each case, a control was selected from patients undergoing open appendectomy (OA) during the same year by systematic sampling. The groups were compared in terms of duration of surgery, requirement of narcotic analgesia, length of hospital stay, postoperative complications and the overall cost for each patient.
Results:
A total of 68 patients underwent laparoscopic appendectomy during the study period. Median duration of surgery was 82 minutes in LA group and 70 minutes in OA group (P < 0.001). Forty-five patients in LA group and 64 in OA group required narcotic analgesia (P < 0.001). Median length of hospital stay (P = 0.672) and postoperative complications (P = 0.779) were comparable in both groups. Median cost of hospital stay was Pakistani Rupees (PKR) 47121/in LA group and PKR 39318/in OA group, the difference being significant (P = 0.001).
Conclusions:
Laparoscopic appendectomy is feasible in developing countries with similar postoperative outcome and less requirement of narcotic analgesia. The duration of surgery and overall cost were significantly higher and efforts should be made to develop expertise and reduce operative time with resultant decrease in cost. Development of standardized protocols for discharge of patients from the hospital after LA may further reduce the cost and benefit patients in developing countries.
Keywords: Appendicitis, laparoscopic appendectomy, open appendectomy
Since its first description by Reginald Fitz in 1886,[1] acute appendicitis remains the most common intraabdominal condition requiring emergency surgery, with a lifetime risk of about 8%.[2] Open appendectomy (OA), as described by McBurney in 1894, remained the gold standard for the treatment of acute appendicitis for more than a century. [3] The surgical approach of OA combines therapeutic efficacy with low and desirable morbidity and mortality rates. [4] The advent and rapid acceptance of laparoscopic surgery led to the idea of performing laparoscopic appendectomy (LA). In 1983 Semm, a German gynecologist performed the first LA.[5] More than two decades later, the benefits of LA are still controversial. Despite numerous randomized trials,[6–8] several meta-analyses,[9–12] and systematic critical reviews[13,14] comparing the two techniques, the relative advantages of each procedure have yet to be established.
Our hospital is a tertiary care hospital in a developing country where laparoscopic procedures are frequently performed. We are a private university and due to lack of insurance system or government support for healthcare, the cost of medical treatment is directly borne by the patient. We sought to analyze and compare the outcomes of LA vs. OA in terms of duration of surgery, requirement of narcotic analgesia, length of hospital stay, postoperative complications and cost of the procedure.
PATIENTS AND METHODS
All consecutive patients undergoing laparoscopic appendectomy (LA) at our hospital from August 2002 to August 2006 were identified using ICD-9-CM coding system. For each case during the year, a control was selected from patients undergoing OA through systematic sampling. The medical records of the patients were reviewed for demographic data, co-morbidities, clinical presentation, physical findings and investigations performed. Operative time was calculated as time from incision to dressing. Peroperative findings were noted from the procedure note transcribed at the time of surgery. The presence and degree of inflammation were determined by reports of histopathology. Requirement for narcotic analgesia, postoperative complications, total length of hospital stay and follow up were recorded. Total cost of the hospital stay which included emergency room charges, bed charges, professional charges, operating room and supply charges, anesthesia charges and pharmacy charges was obtained from the financial department. The patients in our study were counseled about the risks and benefits of each approach, and the final decision was made in consultation with the patient.
For the laparoscopic approach, a 5 mm trocar was placed at the umbilicus and pneumoperitoneum created with carbon dioxide. Two additional ports were placed in lower abdomen as per individual surgeon′s preference. The appendix was identified and the mesoappendix was divided with harmonic scalpel. Base of the appendix was secured by using vicryl endo-loop. The specimens were retrieved through a 10 mm port in a specimen retrieval bag.
The open approach used a traditional oblique or transverse incision over McBurney's point. All patients received a preoperative dose of antibiotics. Postoperative antibiotics administration varied and was determined by the surgeon according to the surgical findings. The patients were given non-narcotic analgesia as first medication for postoperative pain control, but narcotic analgesics were liberally used if pain was not optimally controlled. They were given oral liquids a few hours after surgery. Gradually, once they were fully awake and showed no signs of nausea or abdominal pain, the diet was progressed as tolerated. Patients were discharged home once they were afebrile, had good pain control and tolerated soft diet.
The data were analyzed by using SPSS version 16. Descriptive data are given as median and range. The groups were compared by using Chi-square test for categorical variables and student t-test for continuous variables. The P value of < 0.05 was considered as significant.
RESULTS
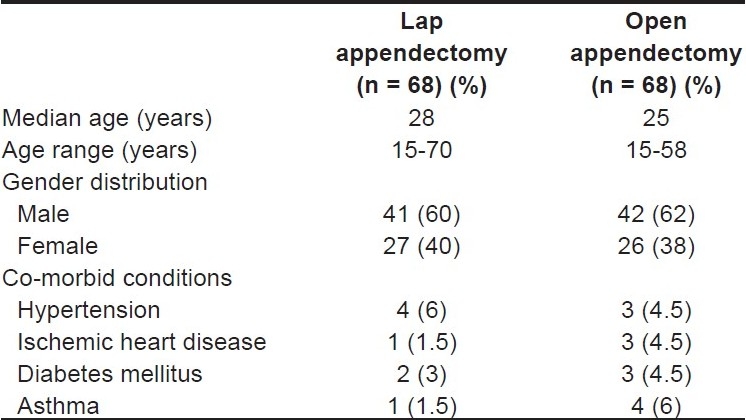
A total of 742 patients underwent appendectomy during the four years of study period. Laparoscopic appendectomy was performed in 68 (9.2%) patients, 10 (14.7%) required conversion to open approach. These patients were included in the LA group for comparison with OA group, based on an intention-to-treat principle. Median age of the patients was 28 years in the LA group and 25.5 years in OA group. Majority of the patients were males and the distribution of co-morbid conditions was comparable in both the groups, as shown in Table 1.
Table 1.
Demographic features and co-morbid conditions in both groups
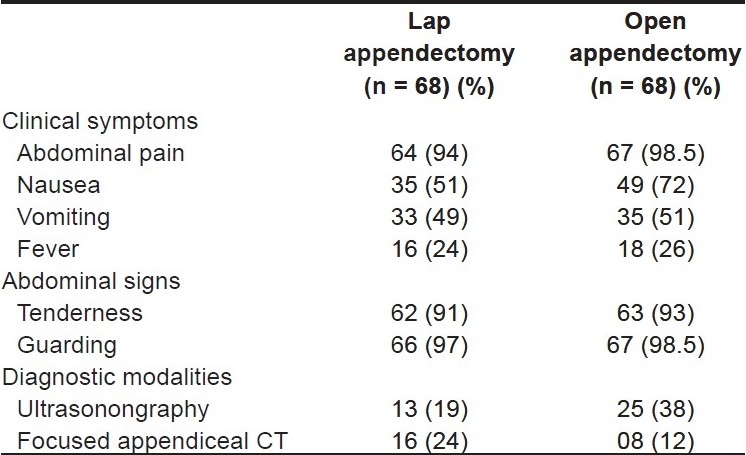
As shown in Table 2, majority of the patients presented with abdominal pain, followed by nausea and vomiting. Preoperative investigations included a blood count and urinalysis for each patient. The radiological investigations were advised by the attending surgical team and is outlined in Table 2. During surgery, the appendix was noted to be grossly ‘normal’ looking in 11 (16%) patient in LA group and 5 (7%) patients in OA group. Final histopathology reported 13 (19%) appendices as ‘normal’ in LA group as compared to 7 (10%) in OA group. This included four patients in LA group and one in OA group who had their surgery done as interval appendectomy. All other patients explored with a clinical suspicion of acute appendicitis had their appendices removed irrespective of the operative findings. Peroperatively, 12 patients in LA group were found to have perforated and/or gangrenous appendix as compared to 14 patients in OA group. Three patients in LA group were found to have appendicular abscesses and they were converted to open laparotomy for optimal drainage and washout.
Table 2.
Clinical features and diagnostic modalities used in both groups
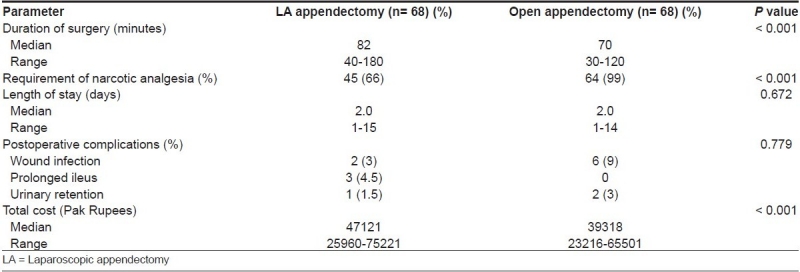
Median operative time was 82 (range: 40-180) minutes in LA group as compared to 70 (range: 30-120) minutes in OA group, the difference was statistically significant (P value < 0.001). Forty-five patients in LA group and 64 patients in OA group required narcotic analgesia, the difference being statistically significant (P value < 0.001). Median length of hospital stay (P value: 0.672) and postoperative complications (P = 0.779) were comparable in both groups. There was a trend towards lower wound infection rate with LA (3% vs. 9%), but the difference was not statistically significant. The cost was calculated in Pakistani Rupees for each patient and the median cost of hospital stay was significantly higher for LA group (P < 0.001). The results are summarized in Table 3. Most of the patients in both groups were followed-up at an interval of one to six weeks after surgery. There were no readmissions or significant symptoms noted during follow-up visits.
Table 3.
Comparison of major clinical outcomes
DISCUSSION
The enormous continuous development of minimally invasive surgery is justified by the many advantages this method provides: Minimal surgical trauma, less postoperative pain, rapid postoperative recovery, exploration of entire abdominal cavity, management of unexpected findings, and better cosmetic results with rapid return to normal activities. Despite all these proposed advantages and increasing popularity, LA has not yet been demonstrated to have a clear advantage over its open counter-part over the past two decades.[14] On the other hand, it has also been argued that the advantages of LA are marginal compared to OA performed by an experienced surgeon through a short, cosmetically acceptable incision, which is associated with minimal complications and short hospital stay.[15–19] The results of our study indicate that patients who underwent LA had significantly lesser requirement for narcotic analgesics, with similar postoperative outcome.
Analysis of our data demonstrated that despite the availability of equipment and expertise for both techniques, large number of patients underwent open appendectomy as compared to laparoscopic procedure. This reflects the personal preference of the staff surgeon in our set-up, probably in view of lesser cost for the patient. The median operative time in our study was 82 minutes for LA, which is relatively longer than that reported by other studies.[20–22] This is probably related to the surgical practices in our university hospital where most of the procedures are performed by the surgical trainee under the direct supervision of the attending surgeon.
The hospital cost was also influenced by the duration of surgery in our hospital, which shows parallel increase for LA. The issue of residents′ training resulting in increasing healthcare cost remains an area of great concern in academic institutions.[23]This is particularly relevant in developing countries without proper healthcare support like ours where it has direct impact on the patient.
In accordance with other studies,[24–26] there were fewer wound infections in the laparoscopy group in our study, but this difference was not statistically significant. A reduction in wound infection can be achieved by extraction of the specimen through a port, or by using an endobag. This finding has also been highlighted in the recent Cochrane review which consisted of more than 5000 patients. [14] According to their findings, patients undergoing LA were half as likely to have wound infection as after OA. This seems to be a significant advantage because wound infection is the commonest complication after open appendectomy. On the other hand, the same reviewers noted that the incidence of intraabdominal abscesses was threefold higher after LA, as compared to OA.[14]We didn′t have any postoperative intraabdominal abscess in our study population.
The question of whether laparoscopic appendectomy decreases the length of hospitalization has been a matter of great debate over the past decade.[24–26] In our study, the length of stay was comparable in both the groups and the results are in keeping with the other studies.[20,21] Broadly speaking, the length of hospital stay has declined dramatically in the recent years, and the differences between open and laparoscopic cases are only marginal.[27] The duration of stay is mainly determined by the pathological status of the appendix and the clinical status of the patient, rather than the open or laparoscopic access used for the procedure. [21]It seems that pathological status of the appendix also contributes to the postoperative septic complications. This is reflected in the fact that five out of 6 patients who developed wound infection in OA group and two out of 3 patients with prolonged ileus in laparoscopic group had perforated appendix at the time of surgery. Development of standardized protocols for discharge of patients from the hospital after LA may further optimize the care and reduce the cost at our hospital.
Although suggested by other studies[14] we were not able to assess the cosmetic results and time to return to normal activity due to limitation of the available data. It has also been suggested that beside the therapeutic effects of LA, laparoscopy per se may offer valuable diagnostic opportunities. The issue of removal of an uninflamed, normal looking appendix has also been debated and it has been proposed not to remove the appendix in those situations where other pathologies can be diagnosed during laparoscopy. Some surgeons, therefore, have used laparoscopy as a diagnostic tool only, and perform conventional appendectomy after laparoscopy in those patients, where the appendix macroscopically has an abnormal appearance. However, it is not yet clarified in which situations a normal looking appendix should be left in place, although non-randomized studies indicate this.[28]
Another issue that remains yet to be conclusively answered is the appropriateness of the laparoscopic approach for complicated appendicitis. A number of studies in the past have recommended open surgery for perforated appendicitis.[29,30]In keeping with these recommendations, the patients in our study who were found to have perforated appendix with abscess formation at the time of laparoscopy were converted to open laparotomy for better drainage and wash-out. A number of recent reports, however, question this approach and the results indicate that patients with complicated appendicitis may be as effectively managed by laparoscopic approach.[31–33]Further randomized trials might help resolve this issue.
CONCLUSION
The results of our study indicate that the requirement of narcotic analgesia was significantly less for patients undergoing LA as compared to OA. There was no significant difference in the incidence of complications and duration of hospital stay between the two groups. There was a trend towards lower wound infection rate with LA (3% vs 9%), but the difference was not statistically significant. On the other hand, the duration of surgery and procedure-related cost were significantly higher for the laparoscopic group. We suggest that laparoscopic approach for appendectomy is at least as safe and effective as its open counterpart. More frequent use of this procedure may lead to reduction in operating time and hospital cost for our patients. It should be continued as a therapeutic option for patients with suspected appendicitis.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Fitz RH. Perforating inflammation of the vermiform appendix with special reference to its early diagnosis and treatment. Am J Med Sci. 1886;92:321. [Google Scholar]
- 2.Addiss DG, Shaffer N, Fowler BS, Tauxe RV. The epidemiology of appendicitis and appendectomy in the United States. Am J Epidemiol. 1990;132:910–25. doi: 10.1093/oxfordjournals.aje.a115734. [DOI] [PubMed] [Google Scholar]
- 3.Mc Burney C. The incision made in the abdominal wall in case of appendicitis with a description of a new method of operating. Ann Surg. 1894:20–38. doi: 10.1097/00000658-189407000-00004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Eriksson S, Granström L. Randomized controlled trial of appendicectomy versus antibiotic therapy for acute appendicitis. Br J Surg. 1995;82:166–9. doi: 10.1002/bjs.1800820207. [DOI] [PubMed] [Google Scholar]
- 5.Semm K. Endoscopic appendectomy. Endoscopy. 1983;15:59–64. doi: 10.1055/s-2007-1021466. [DOI] [PubMed] [Google Scholar]
- 6.Katkhouda N, Mason RJ, Towfigh S, Gevorgyan A, Essani R. Laparoscopic versus open appendectomy: A prospective randomized double-blind study. Ann Surg. 2005;242:439–48. doi: 10.1097/01.sla.0000179648.75373.2f. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Omli S, Magnone S, Bertolinin A, Croce E. Laparoscopic versus open appendectomy in acute appendicitis: A randomized prospective study. Surg Endosc. 2005;19:1193–5. doi: 10.1007/s00464-004-2165-8. [DOI] [PubMed] [Google Scholar]
- 8.Moberg AC, Berndsen F, Palmquist I, Petersson U, Resch T, Montgomery A. Randomized clinical trial of laparoscopic versus open appendicectomy for confirmed appendicitis. Br J Surg. 2005;92:298–304. doi: 10.1002/bjs.4842. [DOI] [PubMed] [Google Scholar]
- 9.Sauerland S, Lefering R, Holthausen U, Neugebauer EA. Laparoscopic vs.conventional appendectomy - a meta-analysis of randomised controlled trials. Langenbecks Arch Surg. 1998;383:289–95. doi: 10.1007/s004230050135. [DOI] [PubMed] [Google Scholar]
- 10.Chung RS, Rowland DY, Li P, Diaz J. A meta-analysis of randomized controlled trials of laparoscopic versus conventional appendectomy. Am J Surg. 1999;177:250–6. doi: 10.1016/s0002-9610(99)00017-3. [DOI] [PubMed] [Google Scholar]
- 11.Garbutt JM, Soper NJ, Shannon WD, Botero A, Littenberg B. Meta-analysis of randomized controlled trials comparing laparoscopic and open appendectomy. Surg Laparosc Endosc. 1999;9:17–26. [PubMed] [Google Scholar]
- 12.Golub R, Siddiqui F, Pohl D. Laparoscopic versus open appendectomy: A meta-analysis. J Am Coll Surg. 1998;186:545–53. doi: 10.1016/s1072-7515(98)00080-5. [DOI] [PubMed] [Google Scholar]
- 13.Fingerhut A, Millat B, Borrie F. Laparoscopy versus open appendectomy: Time to decide. World J Surg. 1999;23:835–45. doi: 10.1007/s002689900587. [DOI] [PubMed] [Google Scholar]
- 14.Sauerland S, Lefering R, Neugebauer EA. Laparoscopic versus open surgery for suspected appendicitis. Cochrane Database Syst Rev. 2007;4:CD001546. doi: 10.1002/14651858.CD001546.pub2. [DOI] [PubMed] [Google Scholar]
- 15.Klingler A, Henle KP, Beller S, Rechner J, Zerz A, Wetscher GJ, et al. Laparoscopic appendectomy does not change the incidence of postoperative infectious complications. Am J Surg. 1998;175:232–5. doi: 10.1016/s0002-9610(97)00286-9. [DOI] [PubMed] [Google Scholar]
- 16.Long KH, Bannon MP, Zietlow SP, Helgeson ER, Harmsen WS, Smith CD, et al. A prospective randomized comparison of laparoscopic appendectomy with open appendectomy: Clinical and economic analyses. Surgery. 2001;29:390–400. doi: 10.1067/msy.2001.114216. Lapaoscopic Appendectomy Interest group. [DOI] [PubMed] [Google Scholar]
- 17.Kum CK, Ngoi SS, Goh PM, Tekant Y, Isaac JR. Randomized controlled trial comparing laparoscopic and open appendicectomy. Br J Surg. 1993;80:1599–600. doi: 10.1002/bjs.1800801236. [DOI] [PubMed] [Google Scholar]
- 18.Ortega AE, Hunter JG, Peters JH, Swanstrom LL, Schirmer B. A prospective, randomized comparison of laparoscopic appendectomy with open appendectomy.Laparoscopic Appendectomy Study Group. Am J Surg. 1995;169:208–12. doi: 10.1016/s0002-9610(99)80138-x. [DOI] [PubMed] [Google Scholar]
- 19.Hansen JB, Smithers BM, Schache D, Wall DR, Miller BJ, Menzies BL. Laparoscopic versus open appendectomy: Prospective randomized trial. World J Surg. 1996;20:17–20. doi: 10.1007/s002689900003. [DOI] [PubMed] [Google Scholar]
- 20.Moberg AC, Berndsen F, Palmquist I, Petersson U, Resch T, Montgomery A. Randomized clinical trial of laparoscopic versus open Appendicectomy for confirmed appendicitis. Br J Surg. 2005;92:298–304. doi: 10.1002/bjs.4842. [DOI] [PubMed] [Google Scholar]
- 21.Kurtz RJ, Heimann TM. Comparison of open and laparoscopic treatment of acute appendicitis. Am J Surg. 2001;182:211–4. doi: 10.1016/s0002-9610(01)00694-8. [DOI] [PubMed] [Google Scholar]
- 22.Maxwell JG, Robinson CL, Maxwell TG, Maxwell BG, Smith CR, Brinker CC. Deriving the indications for laparoscopic appendectomy from a comparison of the outcomes of laparoscopic and open appendectomy. Am J Surg. 2001;182:687–92. doi: 10.1016/s0002-9610(01)00798-x. [DOI] [PubMed] [Google Scholar]
- 23.Cothren CC, Moore EE, Johnson JL, Moore JB, Ciesla DJ, Burch JM. Can we afford to do laparoscopic appendectomy in an academic hospital? Am J Surg. 2005;190:950–4. doi: 10.1016/j.amjsurg.2005.08.026. [DOI] [PubMed] [Google Scholar]
- 24.Frazee RC, Roberts JW, Symmonds RE, Snyder SK, Hendricks JC, Smith RW, et al. A prospective randomized trial comparing open versus laparoscopic appendectomy. Ann Surg. 1994;219:725–8. doi: 10.1097/00000658-199406000-00017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Henle KP, Beller S, Rechner J, Zerz A, Szinicz G, Klingler A. Laparoscopic versus conventional appendectomy: A prospective randomized study. Chirurg. 1996;67:526–30. [PubMed] [Google Scholar]
- 26.Cox MR, McCall JL, Toouli J, Padbury RT, Wilson TG, Wattchow DA, et al. Prospective randomized comparison of open versus laparoscopic appendectomy in men. World J Surg. 1996;20:263–6. doi: 10.1007/s002689900041. [DOI] [PubMed] [Google Scholar]
- 27.Pedersen AG, Petersen OB, Wara P, Rønning H, Qvist N, Laurberg S. Randomized clinical trial of laparoscopic versus open appendicectomy. Br J Surg. 2001;88:200–5. doi: 10.1046/j.1365-2168.2001.01652.x. [DOI] [PubMed] [Google Scholar]
- 28.van den Broek WT, Binjen AB, De Ruiter P, Gouma DJ. A normal appendix found during diagnostic laparoscopy should not be removed. Br J Surg. 2002;88:251–4. doi: 10.1046/j.1365-2168.2001.01668.x. [DOI] [PubMed] [Google Scholar]
- 29.Paik PS, Towson JA, Anthone GJ, Ortega AE, Simons AJ, Beart RW., Jr Intra-abdominal abscesses following laparoscopic and open appendectomies. J Gastrointest Surg. 1997;1:188–92. doi: 10.1016/s1091-255x(97)80108-4. [DOI] [PubMed] [Google Scholar]
- 30.Krisher SL, Browne A, Dibbins A, Tkacz N, Curci M. Intra-abdominal abscess after laparoscopic appendectomy for perforated appendicitis. Arch Surg. 2001;136:438–41. doi: 10.1001/archsurg.136.4.438. [DOI] [PubMed] [Google Scholar]
- 31.Yau KK, Siu WT, Tang CN, Yang GP, Li MK. Laparoscopic versus open appendectomy for complicated appendicitis. J Am Coll Surg. 2007;205:60–5. doi: 10.1016/j.jamcollsurg.2007.03.017. [DOI] [PubMed] [Google Scholar]
- 32.Pokala N, Sadhasivam S, Kiran RP, Parithivel V. Complicated appendicitis- is the laparoscopic approach appropriate? A comparative study with the open approach: Outcome in a community hospital setting. Am Surg. 2007;73:737–41. [PubMed] [Google Scholar]
- 33.Korlacki W, Dzielicki J. Laparoscopic appendectomy for simple and complicated appendicitis in children-safe or risky procedure. Surg Laparosc Endosc Percutan Tech. 2008;18:29–32. doi: 10.1097/SLE.0b013e31815b2de0. [DOI] [PubMed] [Google Scholar]


