Abstract
Background/Aim:
Hirschsprung's disease (HD) is one of the most common causes resulting in lower intestinal obstruction in children with atypical clinical symptoms and inconspicuous morphological findings by barium enema X-ray. Recently, this situation has been largely ameliorated by improvement of instrument for measurement of anorectal pressure. By now, anorectal manometry has been regarded as a routine means for functional assessment and diagnosis of HD. It is accurate in nearly all cases of HD with characteristic absence of rectoanal inhibitory reflex. Different surgical modalities of treatment are available and Swenson's operation is one of the surgical procedures done for HD. Anorectal manometric findings may change after Swenson's operation with improvement of rectoanal inhibitory reflex in some cases. We aimed to evaluate functional results after Swenson's operation for HD using anorectal manometry.
Patients and Methods:
Between 1996 and 2005, 52 patients were diagnosed with HD and operated upon by Swenson's operation in Gastroenterology Center, Mansoura University. There were 33 males (63.46%) and 19 females (36.54%) with a mean age of 3.29 ± 1.6, (range 2-17 years). Anorectal manometry and rectal muscle biopsy were done preoperatively for diagnosis but after operation anorectal manometry was done after every six months and then yearly.
Results:
All of the 52 patients showed absent rectoanal inhibitory reflex on manometric study with relatively higher resting anal canal pressure and within normal squeeze pressure. Postoperatively, there were 35 continent patients (67.31%) with 11 patients (21.15%) showing minor incontinence and six (11.54%) with major incontinence. On the other side, there were five patients (9.62%) with persistent constipation after operation (three due to anal stricture and two due to residual aganglionosis). Postoperative manometric study showed some improvement in anal sensation with the rectoanal inhibitory reflex becoming intact in six patients (11.54%) four years after operation.
Conclusion:
Anorectal manometry is a more reliable method for diagnosis of HD than barium enema X-ray but for final diagnosis, it is reasonable to combine anorectal manometry with tissue biopsy. Functional outcome after Swenson's operation for HD may improve in some patients complaining of incontinence or constipation. Anorectal manometry may show improvement of the parameters after Swenson's operation.
Keywords: Hirshsprung's disease, Swenson's operation, anorectal manometry
Hirshsprung's disease (HD) occurs in one out of 5,000 births,[1]caused by absence of parasympathetic innervation of the distal intestine leading to chronic constipation that characterizes the disease.[2]The distal colon is unable to relax causing functional colonic obstruction over time. The aganglionic segment usually begins at the anus and extends proximally.[3] Short-segment disease is most common and is confined to the rectosigmoid region of the colon but may affect the entire colon. However, rarely, the small and large intestine are involved.[4] Most patients are admitted in the infancy stage where early diagnosis is important to avoid complications. Symptoms range from neonatal intestinal obstruction to chronic progressive constipation in older children.[5] Approximately 80% of the patients present in the first few months of life with difficult bowel movements, poor feeding, and progressive abdominal distension.[6] Patients with HD may present with enterocolitis-related diarrhea rather than constipation.[6] Rectal examination may demonstrate empty rectum, tight anal sphincter, and explosive discharge of stool and gas. Imaging can help diagnose HD, plain films of the abdomen show distension of the distal colon with gas. Contrast enema radiographs of the colon are normal for the first three-months of life.[7]After the dilatation process begins, the diseased portion of the colon will appear normal and the more proximal colon will be dilated.[8]Anorectal manometry is useful to distinguish HD from chronic constipation and megacolon due to other causes. Diagnosis is possible with the absence of internal anal sphincter relaxation upon rectal distension (characteristic for HD).[9] Manometry has been shown to accurately exclude or diagnose HD in 90-100% of the patients with a specificity of 97% and sensitivity of 79%. Barium enema is not conclusive in most of the patients, especially younger children. The diagnosis can be confirmed with a rectal suction biopsy or full thickness biopsy which shows absence of ganglion cells and presence of hypertrophic nerve trunks.[10] If HD is diagnosed, then surgery is normally the only option for treatment. There are several pull-through techniques, with complication rates ranging from 4-16%. Swenson's operation involves removing the rectum, pulling the healthy ganglionated colon through, and connecting it to the anus.[5] Newer techniques as Duhamel and Soave operation help preserve the intricate nerve supply to the rectum and bladder.[11]Most of the patients treated for HD do not have complications and less than 1% may have faecal incontinence.[12]Recently transanal pull-through technique is associated with lower complication rate.
PATIENTS AND METHODS
Our study included 52 patients with HD for whom Swenson's operation was done in the Gastroenterology Center, Mansoura University between 1996 and 2005. There were 33 males (63.46%) and 19 females (36.54%) with a mean age of (3.26 ± 1.6), ranging from 2-17 years.
Preoperatively, all patients underwent clinical examination, routine laboratory investigations, plain X-ray abdomen, and barium enema to see if there is megacolon or cone-shaped transitional zone. Anorectal manometry was done for the 52 patients preoperatively and the results were compared to those obtained with follow-up of patients after surgery.
Anorectal manometry was done using 8-lumen water prefused catheter with latex balloon connected via water filled transducer. This was connected to a polygraph recorder and visual display unit (polygraph ID, Medtronic, USA) and Polygram Net™ (version 4.01.525.45) software to analyze the data.
The anorectal measurements included: Functional anal canal length. Resting anal pressure which is the function of the internal sphincter supplemented with the external sphincter. Squeeze pressure which is the function of the voluntary control pathways and external sphincter. Rectoanal inhibitory reflex: In normal individuals, distension of the rectal ampulla causes relaxation of the internal anal sphincter. This effect is mediated by the intrinsic nerves of the intestine and it is absent in patients with HD [Figure 1]. Finally, the rectal sensation is tested by gradually inflating the rectal balloon to test for the first rectal sensation, the urge to defecate and the maximum tolerable volume. In younger children, rectal sensation could not be obtained.
Figure 1.
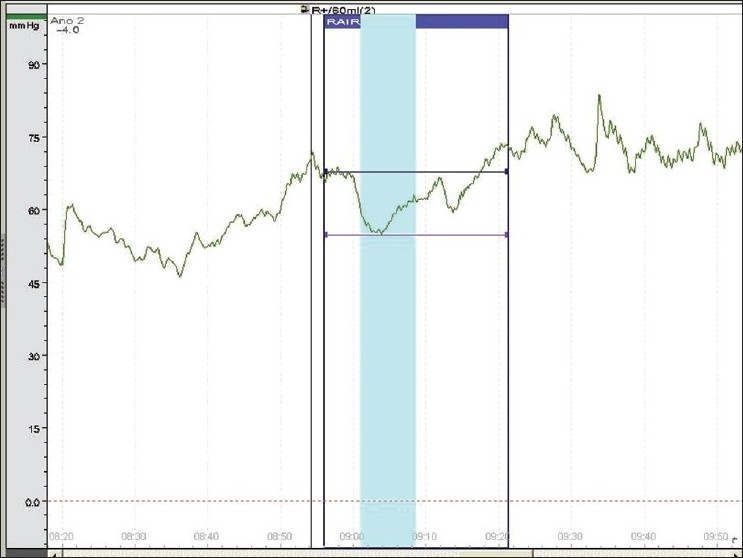
Absent RAIR trace in HD patient
Preoperatively, rectal muscle biopsy was mandatory to prove aganglionosis, even though the rectoanal inhibitory reflex was absent.
Anorectal manometry measurements were obtained before operation and at six months and yearly post operatively. This was done to compare pre and postoperative data in addition to history taking and clinical examination. If constipation or faecal incontinence developed after operation, investigations were done to reveal the cause and treated accordingly.
Patients with minor incontinence were trained with biofeedback therapy by a water-perfused manometry catheter attached to transducers and an amplifier to perform biofeedback. Changes in pressure within the anal canal were displayed on a computer screen situated in front of the patient. Increments in anal squeeze pressure were displayed by the rise in height of a bar chart. The patients were instructed to achieve a maximal squeeze of the voluntary anal sphincter initially, and later to hold a squeeze for as long as possible and improve rectal sensation by gradually deflating balloon and help coordination of pelvic floor and gluteal muscles. The process was repeated several times for 30 minutes in two sessions per week for an average of ten sessions. Patients were requested to perform squeeze efforts at home. Patients were over an age quite enough to understand the procedure. A total of 11 patients improved by biofeedback training but three of them required additional sessions after the end of training course. Biofeedback training was provided by a trained technician and a nurse.
RESULTS
Preoperative anorectal manometry study
Anorectal manometry was carried out for the 52 patients and the results were as follows: Mean resting pressure (61.3 ± 16.2 mmHg); mean maximum squeeze pressure (112.5 ± 32.9 mmHg).
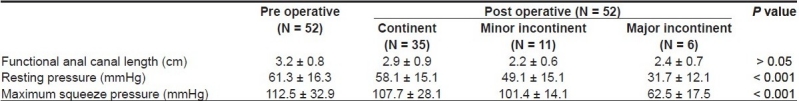
The rectoanal inhibitory reflex was absent in all patients, while the functional anal canal length was (3.2 ± 0.8 cm) [Table 1]. There was diminished rectal sensation in patients for whom this test could be done. None of our older patients could expel the rectal balloon.
Table 1.
Pre and postoperative anorectal manometry study
Functional results
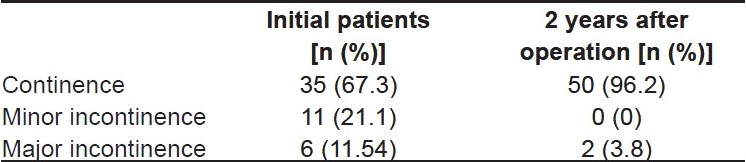
With respect to faecal incontinence, after Swenson's operation and according to Miller′s score,[13]the patients were classified as: continent in 35 cases (67.31%), minor incontinence in 11 cases (21.15%), and major incontinence in 6 cases (11.54%).
On follow-up of faecal incontinence parameter during the first two years postoperatively, the number of patients with major incontinence reduced from 6 to 2 (P< 0.005) [Table 2]. Additionally, the 11 patients with minor incontinence were trained with biofeedback therapy in a twice-a-week session, with patients showing improvement after 10-12 sessions.
Table 2.
Functional continence status after Swenson's operation according to Miller's score in 52 patients
Anorectal manometry was carried out for the 52 cases, resulting in continence in 35 cases, minor incontinence in 11 cases and major incontinence in 6 cases. Functional anal canal length was 2.9 ± 0.9 cm among continent cases, 2.2 ± 0.6 cm among minor incontinent cases, and 2.4 ± 0.7 cm among major incontinent cases with no significant difference between any groups. Resting pressure: The mean pressure was 58.1 ± 15.1 mmHg among continent cases, 49.1 ± 15.1 mmHg among minor incontinent cases, and 37.1 ± 12.1 mmHg among major incontinent cases with a highly significant difference between continent and major incontinent groups (P < 0.001) [Table 1].
The maximum squeeze pressure: The mean pressure was 107.7 ± 28.5 mmHg among continent cases, 101.4 ± 14.1 mmHg among minor incontinent cases, and 62.5 ± 17.5 mmHg among major incontinent cases with a highly significant difference between major and minor incontinent groups (P < 0.001).
The results of the anorectal manometry study are in line with the history and physical findings; both the resting and maximum squeeze pressures are higher in continent cases, lower in minor incontinent cases, and the lowest in major incontinent ones. This suggests that incontinence may be related to a weakened internal anal sphincter.
Meanwhile recurrent constipation developed in six patients (11.54%), three of them due to anal stricture after surgery for whom repeated anal dilatation solved the problem. While in the other two patients, the cause of constipation was due to residual aganglionosis (revealed by postoperative pathology), inspite of being ganglionic in frozen biopsy. This was treated with a redo of the Swenson procedure resulting in improvement of the constipation.
Anorectal manometry was done for five such patients with recurrent constipation and the functional anal canal length was measured at 2.9 ± 0.9 cm, the resting pressure was 70.1 ± 10.1 mmHg, and the maximum squeeze pressure was (110.8 ± 20.5 mmHg).
There were five patients with intact rectoanal inhibitory reflex, after at least four years post- surgery.
DISCUSSION
HD is characterized by absence of myenteric and submucosal ganglion cells in the distal alimentary causing tract constipation, recurrent enterocolitis, failure to pass meconium, and distension. Clinical outcome for affected patients is improved much after the operative treatment. Swenson's operation is one of the operative procedures used to treat such patients in our center. However, specific problems as recurrent constipation and faecal incontinence may occur after Swenson's operation.
Anorectal manometry is a valuable and easy procedure for diagnosis of HD. It is particularly helpful in cases of short segment aganglionosis.[7] It is an extremely valuable screening diagnostic tool in the evaluation of constipated infant.[14]The infant should be completely calm, if he is irritated, the external sphincter contracts irregularly, thereby influencing the anal pressure, which no longer reflects the internal sphincter activity alone.[15]In our study we have to wait until the child is calm to measure the resting pressure. Also, the response may be absent in the severely constipated infants with normal ganglia.[15]In our laboratory, anorectal manometry was conclusive in 52 patients (proved later on by rectal muscle biopsy to have aganglionosis) but in the series of Kekomaki et al. (1979),[16] manometry was inconclusive in 22% of the cases and 20% of the normal children gave a false negative response in the series of Morikawa et al. (1979).[14]
Nagasaki et al. (1984)[17] included the recto-anal reflex electrically in normal children and in children with idiopathic constipation but in cases of HD, however, no reflex was obtained. The advantage of this method is that it does not depend on balloon dilatation of the anal canal, in which case a shift of the probe will occur. Thus, no false positive reflex is elicited. In our anorectal laboratory we have the normal anorectal manometry parameters of population of different age groups. When this is compared with patients with HD, there was slightly higher, albeit insignificant, resting pressure in patients with HD than controls. There was no significant difference in squeeze pressures between controls and patients with HD. The functional length of anal canal was slightly shorter among patients with HD. Postoperative manometric study showed some improvement in anal sensation as late as four years after the pull-through surgery.[18] In our study, we had five patients with intact rectoanal inhibitory reflex, after at least four years post-surgery. This is an intramural local axon reflex controlled by spinal and higher centers but it persists even after loss of extrinsic control. The ganglionic colon anastomosed to the anal canal acquires the function of the rectum after years of operation, though Mya, 1994, demonstrated that rectoanal inhibitory reflex is not restored after corrective surgery.[19]
Faecal incontinence may develop after pull-through due to decreased neural sensation or a natural correlate of aganglionosis, weakened anal sphincter making it impossible to expel flatus selectively without passage of liquid stool. [20]Incidence of incontinence among our cases is relatively high, with minor incontinence in 21.15% cases and major incontinence in 11.54% cases. This is higher than the incontinence reported by Marty et al.[21](12.6%).
Postoperative manometry of the incontinent cases revealed a relatively low mean resting pressure (42.9 ± 16.2 mmHg) and maximum squeeze pressure (87 ± 28.7 mmHg), suggesting that incontinence may be related to a weakened internal anal sphincter. Follow-up of the incontinent cases revealed a significant improvement within two years (decreased from 56.3% down to 18.8%). Some cases gained benefit from biofeedback therapy. Chronic constipation may be due to residual aganglionosis or postoperative stricture. In our study constipation was observed among five cases (9.62%). This is relatively higher than that of Marty, 1995[21](5.7%). In our study, there were three cases of constipation due to anal stricture and two cases due to residual aganglionosis. For the former, repeated anal dilatation succeeded and for the latter, re-Swenson's operation was done with resultant good outcome after surgery. Anorectal manometry in patients with recurrent constipation revealed a high mean resting pressure (70.1 ± 10.1 mmHg) and maximum squeeze pressure (110 ± 20.5mmHg).
CONCLUSION
HD is a devastating problem in infancy and childhood characterized by absence of myenteric and submucosal ganglion cell in the distal alimentary tract. Swenson's operation is the original curative pull-through procedure but some complications as constipation and faecal incontinence may occur. However, incontinence improves with time or with biofeedback training. Anorectal manometry is a valuable investigative tool and may show improvement in some anorectal measurements with possibility of development of intact recto-anal inhibitory reflex. Therefore, we conclude that the functional outcome after Swenson's technique is unsatisfactory due to a high rate of fecal incontinence (iatrogenic in origin) in children (33%), which is inappropriately higher than that reported previously.[19]As such we believe that other surgical procedures, such as the more recent transanal pull-through technique, are a more valid option.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Amiel J, Lyonnet S. Hirschsprung disease, associated syndromes, and genetics: A review. J Med Genet. 2001;38:729–39. doi: 10.1136/jmg.38.11.729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Fishein RH, Handelsman JC, Schuster MM. Surgical treatment of Hirschsprung's disease in adults. Surg Gynecol Obstet. 1986;163:458–64. [PubMed] [Google Scholar]
- 3.Feldmen M, Friedman LS, Sleisenger MH. Sleisenger and Fordtran's Gastrointestinal and Liver Disease: Pathophysiology, Diagnosis, Management. 7th ed. Saunders: Pa:Philadelphia; 2002. Hirschsprung's disease: Congenital megacolon; pp. 2131–5. [Google Scholar]
- 4.Stewart DR, von Allmen D. The genetics of Hirschsprung disease. Gastroenterol Clin North Am. 2003;32:819–37. doi: 10.1016/s0889-8553(03)00051-7. [DOI] [PubMed] [Google Scholar]
- 5.Holschneider AM, Puri P. 2nd ed. Amsterdam: Harwood Academic Publishers; 2000. Hirschsprung's Disease and Allied Disorders. [Google Scholar]
- 6.Khan AR, Vujanic GM, Huddart S. The constipated child: How likely is Hirschsprung's disease? Pediatr Surg Int. 2003;19:439–42. doi: 10.1007/s00383-002-0934-9. [DOI] [PubMed] [Google Scholar]
- 7.Lanfranchi GA, Bazzocchi G, Federici S, Brignola C, Campieri M, Rossi F, et al. Anorectal manometry in the diagnosis of Hirschsprung's disease.Comparison with clinical and radiological criteria. Am J Gastroenterol. 1984;79:270. [PubMed] [Google Scholar]
- 8.Weidner BC, Waldhausen JH. Swenson revisited: A one-stage, transanal pull-through procedure for Hirschsprung's disease. J Pediatr Surg. 2003;38:1208–11. doi: 10.1016/s0022-3468(03)00269-0. [DOI] [PubMed] [Google Scholar]
- 9.Diseth TH, Egeland T, Emblem R. Effects of anal invasive treat-ment and incontinence on mental health and psychological func-tioning of adolescents with Hirschsprung's disease and low anorectal anomalies. J Pediatr Surg. 1998;33:468–75. doi: 10.1016/s0022-3468(98)90090-2. [DOI] [PubMed] [Google Scholar]
- 10.de Lorijn F, Reitsma JB, Voskuijl WP, Aronson DC, Ten Kate FJ, Smets AM, et al. Diagnosis of Hirschsprung's disease: A prospective, comparative accuracy study of common tests. J Pediatr. 2005;146:787–92. doi: 10.1016/j.jpeds.2005.01.044. [DOI] [PubMed] [Google Scholar]
- 11.Hadidi A. Transanal endorectal pull-through for Hirschsprung's disease: Experience with 68 patients. J Pediatr Surg. 2003;38:1337–40. doi: 10.1016/s0022-3468(03)00392-0. [DOI] [PubMed] [Google Scholar]
- 12.Coran AG, Teitelbaum DH. Recent advances in the management of Hirschsprung's disease. Am J Surg. 2000;180:382–7. doi: 10.1016/s0002-9610(00)00487-6. [DOI] [PubMed] [Google Scholar]
- 13.Miller R, Bartolo DC, Roe AM, Mortensen NJ. Assessment of microtransducers in anorectal manometry. Br J Surg. 1988;75:40–3. doi: 10.1002/bjs.1800750115. [DOI] [PubMed] [Google Scholar]
- 14.Morikawa Y, Donahoe PK, Hendren WH. Manometry and histochemistry in the diagnosis of Hirschsprung's disease. Ped. 1979;63:865–71. [PubMed] [Google Scholar]
- 15.Frenckner B. Anorectal manometry in the diagnosis of Hirschsprung's disease in infants. Acta Ped Scand. 1987;67:187. doi: 10.1111/j.1651-2227.1978.tb16301.x. [DOI] [PubMed] [Google Scholar]
- 16.Kekomaki M, Rapola J, Louhimo I. Diagnosis of Hirschsprung's disease. Acta Ped Scand. 1979;68:893. doi: 10.1111/j.1651-2227.1979.tb08229.x. [DOI] [PubMed] [Google Scholar]
- 17.Nagasaki A, Ikeda K, Suita S, Sumitomo K. Induction of the rectoanal reflex by electric stimlulation a diagnostic aid for Hirschsprung's disease. Dis Colon Rectum. 1984;27:598–601. doi: 10.1007/BF02553850. [DOI] [PubMed] [Google Scholar]
- 18.Rescorla FJ, Morrison AM, Engles D, West KW, Grosfeld JL. Hirschsprung's disease: Evaluation of mortality and long-term function in 260 cases. Arch Surg. 1992;127:934–42. doi: 10.1001/archsurg.1992.01420080068011. [DOI] [PubMed] [Google Scholar]
- 19.Mya GH, Ng W, Cheng W, Saing H. Colonic hyperaganglionosis presenting as neonatal enterocolitis and multiple strictures. J Pediatr Surg. 1994;29:1628–30. doi: 10.1016/0022-3468(94)90245-3. [DOI] [PubMed] [Google Scholar]
- 20.Quinn FM, Surana R, Puri P. The influence of trisomy 21 on outcome in children with Hirschsprung's disease. J Pediatr Surg. 1994;29:781–3. doi: 10.1016/0022-3468(94)90369-7. [DOI] [PubMed] [Google Scholar]
- 21.Marty TL, Seo T, Sullivan JJ, Matlak ME, Black RE, Johnson DG. Rectal irrigations for the prevention of postoperative enterocolitis in Hirschsprung's disease. J Pediatr Surg. 1995;30:652–4. doi: 10.1016/0022-3468(95)90681-9. [DOI] [PubMed] [Google Scholar]


