Abstract
Background/Aim:
Dyspepsia is a common gastrointestinal disorder and is the most common indication for upper gastrointestinal endoscopy (UGIE). In recent years, it has been observed in several centers that there is a change in the causes of dyspepsia as revealed by UGIE. Our main objectives were: (1) To study the pattern of upper gastrointestinal pathology in patients with dyspepsia undergoing upper endoscopy; (2) Compare that with the pattern seen 10-15 years earlier in different areas of KSA.
Patients and Methods:
Retrospective study of all UGI endoscopies performed at Aseer Central Hospital, Abha, Southern Saudi Arabia during the years 2005-2007 on patients above 13 years of age. Patients who underwent UGIE for reasons other than dyspepsia were excluded. The analysis was performed using the SPSS 14 statistical package.
Results:
A total of 1,607 patients underwent UGI endoscopy during the three-year study period (age range, 15-100). There were 907 males (56.4%) and 700 female (43.6%). Normal findings were reported on 215 patients (14%) and the majority had gastritis (676 = 42%), of whom 344 had gastritis with ulcer disease. Moreover, 242 patients (15%) had gastro-esophageal reflux (GERD), with or without esophagitis or hiatus hernia. Also, a total of 243 patients had duodenal ulcer (DU) (15%) while only 12 had gastric ulcer (0.7%).
Discussion and Conclusion:
There is clear change in the frequency of UGIE lesions detected recently compared to a decade ago with an increasing prevalence of reflux esophagitis and hiatus hernia. This could be attributed to changes in lifestyle and dietary habits such as more consumption of fat and fast food, increased prevalence of obesity, and smoking. These problems should be addressed in order to minimize the serious complications of esophageal diseases.
Keywords: Dyspepsia, endoscopy, lesions, esophageal disease
Dyspepsia is defined as a chronic or frequently recurring epigastric pain or discomfort, which is believed to originate in the gastroduodenal region.[1] This may be associated with other upper gastro-intestinal (GI) symptoms, such as heartburn, postprandial fullness, and early satiety.
Dyspepsia is a common problem.[2,3]It is a frequent reason for attending primary care consultations[4,5]and it has a great impact on the patient′s quality of life.[6]
In the UK, 3% of the population takes long-term prescribed drugs for dyspepsia at an annual cost of £500 million, and 450,000 patients have upper gastrointestinal endoscopy each year.[7] Previous studies from Saudi Arabia have shown a low frequency of esophageal diseases such as reflux esophagitis and hiatus hernia.[8,9] and high prevalence of helicobacter associated gastritis.
Recently, there is a clinical impression among clinicians and endoscopists that a change has occurred in the endoscopic causes of dyspepsia with increasing frequency of esophageal diseases, in particular gastro-esophageal reflux disease (GERD).[10,11]Since this trend has significant consequences to clinical practice due to the serious complications of GERD, this matter should be further studied. Thus, the aim of this study was to determine if such changes in the pattern of endoscopic findings have actually occurred during the last 15 years in Abha, Southern Saudi Arabia.
PATIENTS AND METHODS
This was a retrospective study of all upper gastro- intestinal endoscopies (UGIE) performed at the endoscopy department at Aseer Central Hospital, Abha, Southern region of the kingdom of Saudi Arabia between 2005 and 2007. Consecutive patients over the age of 13 years, referred because of dyspepsia, were included. Patients who underwent UGIE for reasons other than dyspepsia such as dysphagia, upper GI bleeding, or strong suspicion of cancer were excluded. Also patients who were taking antihelicobacter treatment or proton pump inhibitors for a month prior to the study were also excluded. Endoscopy was performed by one of the authors (SMA, MEKA, AA) according to standard protocols. Esophageal diseases in this study referred to GERD, no-erosive reflux, hiatus hernia, and peptic esophagitis. Age, sex, and endoscopic findings of patients were tabulated and analyzed using the SPSS 14 statistical package. Simple descriptive statistics were used with a significance level of less than 5% taken as significant.
RESULTS
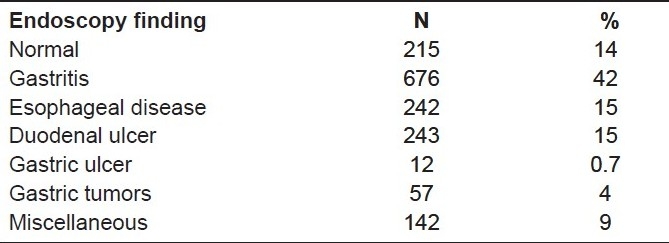
A total of 1,607 patients who underwent UGIE during the three-year study period were analyzed. (age range, 15- 100; mean, 48.5 SD 18). There were 907 males (56.4%) and 700 female (43.6%). None of the patients were taking aspirin or other nonsteroidal antiinflammatory drugs or proton pump inhibitors on regular basis. Table 1 summarizes the endoscopy findings. Normal findings were reported on 215 patients (14%), while 676 (42%) patients had gastritis, of whom 344 had gastritis with ulcer disease. Moreover, 242 (15%) patients had GERD, with or without esophagitis or hiatus hernia. Also, a total of 243 patients had DU (15%) while only 12 had gastric ulcer (0.7%), and 57 (4%) had tumors. Miscellaneous lesions (for example, esophageal varices, gastric erosions, pyloric obstruction, vasculitic legions, etc.) were detected in 142 (9%) patients.
Table 1.
Upper gastroduodenoscopy findings of 1,067 patient
DISCUSSION
We have demonstrated in the current study that a change has occurred in endoscopic findings in our area compared to that seen more than a decade ago. Namely, normal findings decreased by 32%, most likely due to better selection of patients for endoscopy. Also, gastritis has increased by 21% possibly due to increasing use of non-steroidal anti-inflammatory drugs; but most importantly, there was a 15% rise in the frequency of esophageal diseases, particularly reflux esophagitis (GERD).
Previous studies a decade ago in our own area have found a lower frequency of esophageal diseases[12,13] and a higher rate of normal findings. This has been supported by a study by Laajam et al. reporting similar findings in Riyadh area in 1988 with lower frequency of esophageal disease.[14] However, in 1996 a report from the same area have found that in patients above 60 years of age, esophagitis, hiatus hernia and esophageal varices were the most frequently diagnosed.[15]
Regionally, a study from Iran has documented a higher prevalence of reflux esophagitis among Iranian.[16]Even in some European countries such as Greece,[17]it has been found that there was a changing pattern of UGIE indications and findings in the years 1990, 1995, 2000 and 2005 with dyspepsia in 24.4%, 33.6%, 54.3% and 51.3% of cases, respectively (P = 0.002), and reflux in 1.8%, 1.3%, 5.1% and 10.8% of cases, respectively (P = 0.005). With these cases having more frequent indications for upper endoscopy and increasing frequency of reflux esophagitis to 16% in 2005, it lends more support to the fact that esophageal disease is increasing in frequency. In contrast to our findings, Taye in Ethiopia, reported in their findings in the year 2004,[18]that the most common abnormal endoscopic findings were duodenal ulcer (41%), esophageal varices (9%), acute gastritis (6%), duodenitis (3.4%), and reflux esophagitis (only 2.3%), while reports from Sudan demonstrated lower frequency of esophageal diseases.[19]Such differences in prevalence can be attributed to different dietary and lifestyle patterns.
So, what is the explanation for the increasing frequency of esophageal disorders, in particular GERD, as shown in our study? Most likely this may be attributed to the changes in socio-economic status in the Kingdom of Saudi Arabia and other rapidly developing countries where there is a high consumption of fat and fast food, increasing prevalence of obesity and overweight (with an overall obesity prevalence of 35.5% in Saudi Arabia), accompanied by lack of exercise.[20–22]
Moreover, issues have arisen regarding H pylori infection and GERD that have caused confusion among practicing physicians. Some studies have suggested that colonization with H pylori, particularly Cag A strains, may be protective against the more severe forms of GERD, and that the incidence of new GERD-type symptoms or endoscopic esophagitis was greater in cases where successful eradication was achieved.[23] However, the link between GERD and H pylori is complex and remains poorly defined till better evidence is available.[24,25] The main limitation of this study is being a retrospective one. This makes detailed data gathering and analysis difficult.
CONCLUSION
We have demonstrated an increased frequency of endoscopic lesions, in particular esophageal diseases such as GERD and a decline in the frequency of normal findings compared to a decade ago. Possible causes for such change could be related to changes in lifestyle and/or a high fat diet with lack of exercise, leading to obesity.
Preventive measures should be adopted to cope with the situation and to prevent the serious complications of esophageal diseases especially GERD.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Veldhuyzen van Zanten SJ, Flook N, Chiba N, Armstrong D, Barkun A, Bradette M, et al. An evidence-based approach to the management of patients with dyspepsia in the era of Helicobacter pylori. Can Med Assoc J. 2000;162:S3–23. [PMC free article] [PubMed] [Google Scholar]
- 2.McCormick A, Fleming D, Charlton J. Morbidity statistics from general practice: Fourth national morbidity study 1991-1992. 1995 London: Office of Population Censuses and Surveys. [Google Scholar]
- 3.Jones RH, Lydeard SE, Hobbs FD, Kenkre JE, Williams EI, Jones SJ, et al. Dyspepsia in England and Scotland. Gut. 1990;31:401–5. doi: 10.1136/gut.31.4.401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Knill-Jones RP. Geographical differences in the prevalence of dyspepsia.Scand J Gastroenterol Suppl. 1991;182:17–24. doi: 10.3109/00365529109109532. [DOI] [PubMed] [Google Scholar]
- 5.Talley NJ, Silverstein MD, Agreus L, Nyren O, Sonnenberg A, Holtmann G. AGA technical review: Evaluation of dyspepsia.American Gastroenterological Association. Gastroenterology. 1998;114:582–95. doi: 10.1016/s0016-5085(98)70542-6. [DOI] [PubMed] [Google Scholar]
- 6.Talley NJ, Weaver AL, Zinsmeister AR. Impact of functional dyspepsia on quality of life. Dig Dis Sci. 1995;40:584–9. doi: 10.1007/BF02064375. [DOI] [PubMed] [Google Scholar]
- 7.Delaney BC, Moayyedi P. Health care needs assessment. In: Stevens A, Raftery J, Mant J, editors. Dyspepsia. 3rd series. Oxford: Routledge; 2006. [Google Scholar]
- 8.Al-Quorain A, Satti MB, Al-Hamdan A, Al-Gassab G, Al-Freihi H, Al-Gindan Y. Pattern of upper gastrointestinal disease in the eastern province of Saudi Arabia: Endoscopic evaluation of 2982 patients. Trop Geogr Med. 1991;43:203–8. [PubMed] [Google Scholar]
- 9.Satti MB, Twum-Danso K, Al-Freihi HM, Ibrahim EM, Al-Gindan Y, Al-Quorain A, et al. Helicobacter pylori-associated upper gastrointestinal disease in Saudi Arabia: a0 pathologic evaluation of 298 endoscopic biopsies from 201 consecutive patients. Am J Gastroenterol. 1990;85:527–34. [PubMed] [Google Scholar]
- 10.El-Serag HB. Time trends of gastroesophageal reflux disease: A systematic review. Clin Gastroenterol Hepatol. 2007;5:17–26. doi: 10.1016/j.cgh.2006.09.016. [DOI] [PubMed] [Google Scholar]
- 11.Kerrigan BD, Brown SR, Hutchinson GH. Open access gastroscopy; Too much to swallow? BMJ. 1990;300:374–6. doi: 10.1136/bmj.300.6721.374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Tiwari I, Uddin W, Mazhar Z. Impact of open access endoscopy on early diagnosis, treatment and gastrointestinal radiology service. Saudi J Gastroenterol. 1997;3:130–2. [PubMed] [Google Scholar]
- 13.Morad NA, Ahmed ME, Al-Wabel A, Foli AK. Helicobacter pylori associated dyspepsia in patients from southern Saudi Arabia. Ann Saudi Med. 1993 Jul;13:340–3. doi: 10.5144/0256-4947.1993.340. [DOI] [PubMed] [Google Scholar]
- 14.Laajam MA, Al-Mofleh IA, Al-Faleh FZ, Al-Aska AK, Jessen K, Hussain J, et al. Upper gastrointestinal endoscopy in Saudi Arabia: a0 nalysis of 6386 procedures. Q J Med. 1988;66:21–5. [PubMed] [Google Scholar]
- 15.Ayoola EA, al-Rashed RS, al-Mofleh IA, al-Faleh FZ, Laajam M. Diagnostic yield of upper gastrointestinal endoscopy in relation to age and gender: a0 study of 10112 Saudi patients. Hepatogastroenterology. 1996;43:409–15. [PubMed] [Google Scholar]
- 16.Rezailashkajani M, Roshandel D, Shafaee S, Zali MR. High prevalence of reflux agitis among upper endoscopies of Iranian patients. Eur J Gastroenterol Hepatol. 2007;19:499–506. doi: 10.1097/MEG.0b013e32811ebfec. [DOI] [PubMed] [Google Scholar]
- 17.Assimakopoulos SF, Thomopoulos KC, Louvros E, Theocharis G, Giannikoulis C, Katsakoulis E, et al. Changes in the indications of upper gastrointestinal tract endoscopy and endoscopic findings during the last 15 years in South-Western Greece. Am J Med Sci. 2008;336:21–6. doi: 10.1097/MAJ.0b013e31815adeea. [DOI] [PubMed] [Google Scholar]
- 18.Taye M, Kassa E, Mengesha B, Gemechu T, Tsega E. Upper gastrointestinal endoscopy.A review of 10,000 cases. Ethiop Med J. 2004;42:97–107. [PubMed] [Google Scholar]
- 19.Hamo IM. Esophageal disease in Sudan diagnosed by fiberoptic endoscopy. Trop Geogr Med. 1993;45:22–4. [PubMed] [Google Scholar]
- 20.Wildner-Christensen M, Hansen JM, De Muckadell OB. Risk factors for dyspepsia in a general population: n0 onsteroidal anti-inflammatory drugs, cigarette smoking and unemployment are more important than Helicobacter pylori infection. Scand J Gastroenterol. 2006;41:149–54. doi: 10.1080/00365520510024070. [DOI] [PubMed] [Google Scholar]
- 21.Cremonini F, Locke GR, 3rd, Schleck CD, Zinsmeister AR, Talley NJ. Relationship between upper gastrointestinal symptoms and changes in body weight in a population-based cohort. Neurogastroenterol Motil. 2006;18:987–94. doi: 10.1111/j.1365-2982.2006.00816.x. [DOI] [PubMed] [Google Scholar]
- 22.Al-Nozha MM, Al-Mazrou YY, Al-Maatouq MA, Arafah MR, Khalil MZ, Khan NB, et al. Obesity in Saudi Arabia. Saudi Med J. 2005;26:82. [PubMed] [Google Scholar]
- 23.Fallone CA, Barkun AN, Friedman G, Mayrand S, Loo V, Beech R, et al. Is Helicobacter pylori eradication associated with gastroesophageal reflux disease? Am J Gastroenterol. 2000;95:914–20. doi: 10.1111/j.1572-0241.2000.01929.x. [DOI] [PubMed] [Google Scholar]
- 24.Nogueira-de Rojas JR, Jimenez-Gonzalez A, Cervantes-Solis C. Helicobacter pylori gastric infection is a protection factor for gastroesophageal reflux disease. Rev Gastroenterol Mex. 2002;67:22–7. [PubMed] [Google Scholar]
- 25.Werdmuller BFM, Loffeld RJ. Helicobacter pylori infection has no role in pathogenesis of reflux esophagitis. Dig Dis Sci. 1997;42:103–5. doi: 10.1023/a:1018841222856. [DOI] [PubMed] [Google Scholar]


