Abstract
Thrombocytopenia is a common clinical problem in HCV-infected cases. Multiple studies have consistently shown a rise in platelet count following a successful HCV treatment thus proving a cause-effect relationship between the two. Although, many therapeutic strategies have been tried in the past to treat HCV-related thrombocytopenia (e.g. interferon dose reductions, oral steroids, intravenous immunoglobulins, splenectomy etc), the success rates have been variable and not always reproducible. After the cessation of clinical trials of PEG-rHuMGDF due to immunogenecity issues, the introduction of non-immunogenic second-generation thrombopoietin-mimetics (eltrombopag and Romiplostim) has opened up a novel way to treat HCV-related thrombocytopenia. Although the data is still sparse, eltrombopag therapy has shown to successfully achieve the primary endpoint platelet counts of ≥50,000/μL in phase II & III, randomized, double-blind, placebo-controlled trials. Likewise, though it is premature to claim safety of this drug especially in high-risk patient groups, reported side effects in the published literature were of insufficient severity to require discontinuation of the drug. Based on the current and emerging evidence, a review of the pharmacologic basis, pharmacokinetics, therapeutic efficacy, safety profile and future considerations of eltrombopag in the context of HCV-related thrombocytopenia is given in this article. A MEDLINE search was conducted (1990 to August 2009) using the search terms eltrombopag, HCV, thrombocytopenia.
Keywords: Eltrombopag, hepatitis C virus, thrombocytopenia
Hepatitis C virus (HCV) infection, even in the absence of overt hepatic disease, is a well-established cause of chronic immune thrombocytopenic purpura (CITP).[1,2] Six cross-sectional studies have reported positive HCV serology in almost 20% patients with a clinical diagnosis of CITP.[3,4] Pockros et al., retrospectively estimated that the prevalence of CITP among their HCV patients was much greater than would be expected by chance ( P < 0.00001). [5,6] The severity of thrombocytopenia can be highly variable ranging from a transient, isolated finding to a severe, life-threatening condition. Multiple treatment strategies have been employed to treat HCV-related thrombocytopenia but due to the heterogeneous nature of the disease, the response rates are variable, often disappointing and associated with high risks.[7] After the cessation of clinical trials of PEG-rHuMGDF due to immunogenecity issues, the introduction of non-immunogenic second-generation thrombopoietin (TPO) mimetics has opened up a novel way to treat thrombocytopenia. In 2008, FDA approved using eltrombopag and Romiplostim in patients with CITP who are refractory to at least one standard treatment.
DISCUSSION
Cause-effect relationship between hepatitis C virus infection and thrombocytopenia
It is suggested that all thrombocytopenia patients with risk factors for HCV (h/o multiple blood transfusions, hemodialysis, unexplained abnormal aminotransferase levels, needle stick injury or mucosal exposure to HCV-positive blood, I/V drug abusers, recipients of organ transplant, children born to HCV-infected mothers, current sexual partners of HCV-infected persons or persons having multiple sexual partners) be screened for the virus, especially in regions with high rates of infection.[8,9] Improvement in platelet counts that follow successful treatment of HCV clearly demonstrate the cause-effect relationship between the two.[10,11] HCV-related thrombocytopenia (defined as a platelet count of 20,000 to < 70,000/mm3) is typically less severe than primary (idiopathic) CITP, but the affected patients are more vulnerable to major bleeding. Possible causes include decreased platelet production (due to decreased hepatic production of thrombopoietin[12,13] and virus-induced bone marrow suppression),[14,15] increased peripheral destruction of platelets (immune-mediated5and hypersplenism leading to increased splenic platelet sequestration),[16,17] deranged clotting profile, portal hypertension (predisposing to variceal bleeding) etc. HCV binding to platelet membrane with consequent binding of anti-HCV antibody and phagocytosis of platelets, and derangement of host immune system triggering the production of autoantibodies against platelet glycoproteins are the two most frequently postulated immune mechanisms explaining increased peripheral platelet destruction in HCV-infected cases.[5,14,18,19] Interferon (IFN) therapy is also known to cause a 10-50% fall in the platelet count. It is more severe with pegylated interferon/ribavirin (PEG-IFN/RBV) combination therapy as compared to non-pegylated IFN/RBV therapy. It is worst with PEG-IFN monotherapy,[20] suggesting that some reactive thrombocytosis may be occurring secondary to RBV-induced anemia. Since successful treatment of HCV infection has clearly shown to improve the platelet counts,[5,21] the therapeutic protocols for managing HCV-related thrombocytopenia ought to significantly differ from those of primary (idiopathic) thrombocytopenic purpura.
Different therapeutic strategies to treat hepatitis C virus-related thrombocytopenia
Multiple therapeutic strategies including a reduction in the dose of IFN,[22] oral steroids,[4,10,23,24] intravenous immunoglobulin (IVIG)[3] or anti-RhD Ig,[9] splenectomy [4,10] and partial splenic embolization have been tried to treat HCV-related thrombocytopenia.[25] Unlike CITP, use of steroid therapy in the management of HCV-related thrombocytopenia has never gained popularity because despite conflicting reports of variable increases in platelet counts, steroid therapy has shown to cause a rise in transaminase levels and HCV viral load, and worsening of liver damage.[9] Steroids have even shown to cause an elevation in serum bilirubin levels and development of overt jaundice, though rarely.[9] Splenectomy has shown to produce comparable responses in HCV-positive and HCV-negative CITP cases.[4,10]
The most practical strategy in treating HCV-related thrombocytopenia is based on the principle that eradication of HCV infection should result in remission of thrombocytopenia. Thus the usual protocol to treat HCV-related thrombocytopenia is to continue with IFN therapy but reduce its dose if platelet count falls to < 30 × 109/L or discontinue if it falls to < 20 × 109/L. [22,26] The minimum effective dose of PEG-IFN appears to be 1 µg/kg/week. If platelet counts of < 30 × 109/L persist even after reducing PEG-IFN dose to the minimum effective level, initiating some adjunct therapy like Eltrombopag may be considered.
Use of 1st-generation thrombopoietic growth factors in treating hepatitis C virus-related thrombo cytopenia-A historical note
Thrombopoietin (Tpo), a glycoprotein primarily produced in the liver, is the major regulator of both megakaryopoiesis and platelet production in human body. It is the key endogenous ligand for thrombopoietin receptor (TpoR) found on the surface of megakaryocytes, and megakaryocytic precursors.[27,28] Tpo binding to its receptor activates the Janus Kinase/Signal Transducer and Activator of Transcription (JAK-STAT) pathway ultimately leading to the release of platelets in the circulation.[29–31] Although, the use of first-generation thrombopoietic growth factors (recombinant human thrombopoietin [TPO] and pegylated recombinant human megakaryocyte growth and development factor [PEG-rHuMGDF]) clearly showed improvement in platelet counts in multiple clinical trials,[32–35] their use was abruptly abandoned in 1998 when some patients paradoxically developed thrombocytopenia as a result of treatment with PEG-rHuMGDF.[36–39] The underlying mechanism was development of antibodies against PEG-rHuMGDF, which cross-reacted with and neutralized endogenous TPO, producing thrombocytopenia. Some nonimmunogenic second-generation thrombopoietic growth factors have been tried since, the most extensively investigated being romiplostim [AMG-531, Nplate(R)] and eltrombopag [SB-497115, Promacta(R), Revolade(R)].[40]
Role of eltrombopag (2nd-generation thrombopoietic growth factor) in treating hepatitis C virus-related thrombocytopenia
Mechanism of action
Eltrombopag is a first-in-class, nonpeptide, orally bioavailable, thrombopoietin-receptor (TpoR) agonist, human platelets growth factor.[41–43] It interacts with the transmembrane domain of the thrombopoietin receptor, activating JAK2/STAT signaling pathways and inducing increased proliferation and differentiation of human bone marrow progenitor cells into megakaryocytes and thus increased platelet production.[44] It appears that eltrombopag binds the TPO receptor at a distance from the binding site for TPO and appears to initiate signal transduction by a mechanism different from rhTPO.[45] The two thus have an additive (and not competitive) effect on platelet production.
Pharmacokinetics
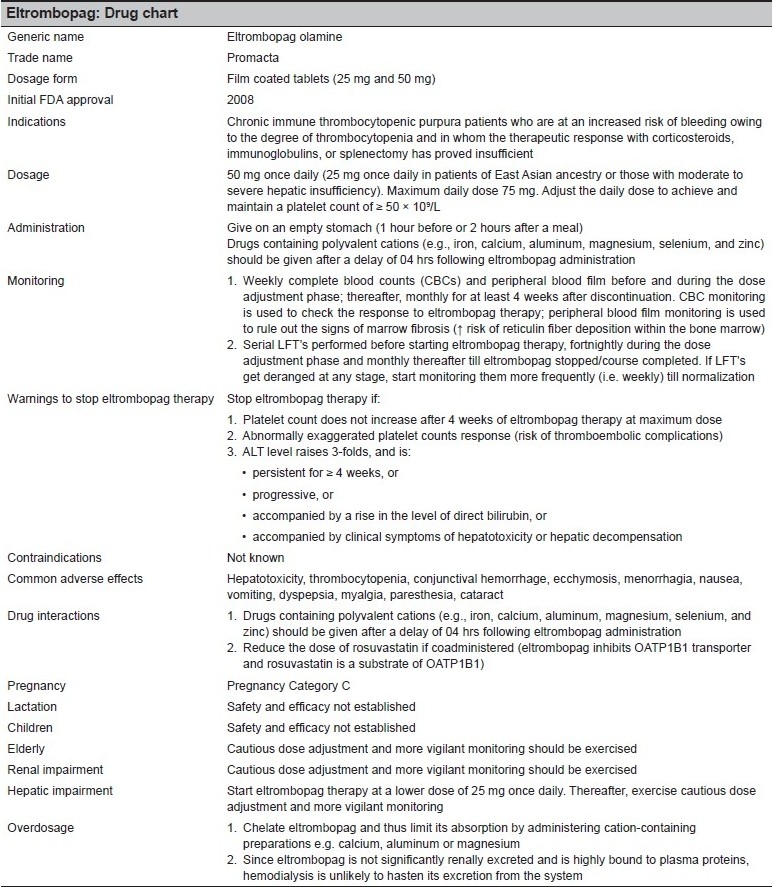
It appears that the pharmacokinetics of Eltrombopag (average T1/2> 12 hours) is linear and therefore it produces a dose-dependent increase in platelet proliferation and differentiation in CITP cases[42,46–49] with no rebound thrombocytopenia following discontinuation of treatment. [50] In one study,[51] subjects receiving 75 mg of eltrombopag once daily started to show a rise in platelet [SUPPORTING:1] count at day 7, which peaked on day 16. Eltrombopag therapy has not been shown to produce any negative effect on platelet function, as measured by platelet aggregation and activation.[52,53]
Eltrombopag.
Drug chart
In a phase 2 study,[54] whereas only 6% of HCV-related cirrhotics in the placebo group completed the 12 weeks antiviral course, the same was completed by 36%, 53%, and 65% of patients receiving 30 mg, 50 mg, and 75 mg of eltrombopag, respectively. Moreover, 75 to 95% of patients in the eltrombopag groups achieved the primary end point (a platelet count 100,000/mm3at week 4) in a dose-dependent manner.
Evidence of therapeutic efficacy
In a recent phase III, randomized, double-blind, placebo- controlled study,[55] CITP patients from 63 sites in 23 countries having platelet counts of < 30,000/µL received once-daily eltrombopag 50 mg (n = 76) or placebo (n = 38) for up to six weeks. The primary endpoint in this study was the determination of the proportion of patients who successfully achieve platelet counts of ≥50,000/µL at day 43. It was shown that compared to 16% placebo patients, 59% eltrombopag patients successfully achieved the primary endpoint (odds ratio [OR] 9.61 [95% CI 3.31-27.86]; P < 0.0001). Consequent to a rise in the platelet count, eltrombopag patients had less bleeding at any given time during the study than did those receiving placebo (OR 0.49 [95% CI 0.26-0.89]; P = 0.021). The effect in rise of platelet count was, however, transient with platelet counts generally falling back to the baseline levels within two weeks of halting eltrombopag therapy. The frequency of grade 3-4 adverse events leading to the discontinuation of the study were similar in both groups (eltrombopag 4% and placebo 5%).
Results from another phase II placebo controlled, double-blind, dose-ranging study,[56] done in patients with chronic hepatitis C liver disease with concomitant thrombocytopenia (platelet counts ranging from 20-70 × 109/L) showed median platelet counts in eltrombopag arm at week 4 of 53 × 109/L, 137 × 109/L, 214 × 109/L, and 209 × 109/L. This rise in platelet counts helped initiate a twelve week long interferon therapy, which was successfully completed by 6%, 36%, 53%, and 65% of the subjects, respectively.
Safety profile of eltrombopag
Although more studies are needed to ascertain the safety of eltrombopag therapy, the most commonly reported side effects in the published literature (headache, dry mouth, abdominal pain, and nausea) were of insufficient severity to require discontinuation of the drug.[53] Additionally, one study showed a significant reduction in the incidence of WHO-defined bleeding with six weeks eltrombopag therapy compared with the placebo.[57] Our knowledge whether a rise in eltrombopag-induced platelet count will increase the rate of thrombosis - vascular outcome data-is limited.[58] What we know from the data from studies of the first-generation thrombopoietic growth factors is that a rise in platelet count did not increase the rate of thrombosis, even when patients had cancer.[59–61] But notably, all those studies excluded patients with active cardiac or cerebrovascular disease or a history of thrombosis. Thus we don′t exactly know at this stage, how unsafe or risky eltrombopag administration would be in these high-risk patients. It is sound to say that worsened cardiovascular and stroke outcomes may be the major obstacle to the success of this otherwise promising agent. A recent encouraging study by Erhardt JA et al.,[62] demonstrated that in contrast to rhTPO, which significantly primed platelet activation, eltrombopag showed little or no effect on overall platelet function.
Another worrisome safety issue is the possible long-term exposure effect/s of eltrombopag therapy on bone marrow function. Studies have shown that when megakaryocytes are stimulated, they release TGF-β, which in turn causes a reversible increase in reticulin deposition.[63,64] Animal studies have shown, administration of second-generation thrombopoeitic growth factors of causing extensive bone marrow fibrosis, osteosclerosis and extramedullary hematopoiesis-a picture similar to human myelofibrosis.[65,66] In the only study[67] in human subjects in which routine bone marrow analysis was performed to determine the effects of first-generation thrombopoietic growth factors, 8 of 9 rhTPO-treated patients and two of six control patients had increased bone marrow reticulin staining. Because of the almost lack of experience with first-generation thrombopoietic growth factors, more long-term exposure studies are needed to specifically explore the effects of second-generation thrombopoietic growth factors on bone marrow function in human subjects. [68] It is pertinent to mention here that both, thromboembolic events in high risk patients, and potentially reversible increases in bone marrow reticulin have been reported with romiplostim (AMG-531), another TPO peptide mimetic.[69] There are reports of rebound worsening of thrombocytopenia as well as increased blast formation, upon discontinuation.[70] Some avoidable interactions with concomitant administration of antacids (containing aluminum and magnesium) and high-calcium food-both causing significant reductions in systemic absorption of eltrombopag have also been reported in the literature.[71]
CONCLUSION
The ultimate aim of treating thrombocytopenia in HVC-positive cases is not to normalize the platelet counts,[72] but to attain and maintain a safe hemostatic level that avoids hemorrhage on one hand and thrombosis on the other. Although more studies are needed to validate true indications, dosage schedule, therapeutic efficacy and safety profile of eltrombopag adjunct therapy, it appears that it is an effective[73] and relatively safe treatment modality (at least in short-term usage) for managing thrombocytopenia in HVC-positive CITP cases. Its main advantage being possible avoidance of interferon dose reductions or interruptions.[74]
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Pyrsopoulos NT, Reddy KR. Extrahepatic manifestations of chronic viral hepatitis. Curr Gastroenterol Rep. 2001;3:71–8. doi: 10.1007/s11894-001-0044-1. [DOI] [PubMed] [Google Scholar]
- 2.Cacoub P, Renou C, Rosenthal E, Cohen P, Loury I, Loustaud-Ratti V, et al. Extrahepatic manifestations associated with hepatitis C virus infection: A prospective multicenter study of 321 patients. Medicine. 2000;79:47–56. doi: 10.1097/00005792-200001000-00005. [DOI] [PubMed] [Google Scholar]
- 3.Garcia-Suarez J, Burgaleta C, Hernanz N, Albarran F, Tobaruela P, Alvarez-Mon M. HCV-associated thrombocytopenia: Clinical characteristics and platelet response after recombinant alpha2b- interferon therapy. Br J Haematol. 2000;110:98–103. doi: 10.1046/j.1365-2141.2000.02132.x. [DOI] [PubMed] [Google Scholar]
- 4.Sakuraya M, Murakami H, Uchiumi H, Hatsumi N, Akiba T, Yokohama A, et al. Steroid-refractory chronic idiopathic thrombocytopenic purpura associated with hepatitis C virus infection. Eur J Haematol. 2002;68:49–53. doi: 10.1034/j.1600-0609.2002.00509.x. [DOI] [PubMed] [Google Scholar]
- 5.Pockros PJ, Duchini A, McMillan R, Nyberg LM, McHutchison J, Viernes E. Immune thrombocytopenic purpura in patients with chronic hepatitis C virus infection. Am J Gastroenterol. 2002;97:2040–5. doi: 10.1111/j.1572-0241.2002.05845.x. [DOI] [PubMed] [Google Scholar]
- 6.Danish FA. Current Standards in the Pharmacotherapy of Chronic Hepatitis C and Local Practices. Infect Dis J. 2008;17:93–7. [Google Scholar]
- 7.Nurden AT, Viallard JF, Nurden P. New-generation drugs that stimulate platelet production in chronic immune thrombocytopenic purpura. Lancet. 2009;373:1562–9. doi: 10.1016/S0140-6736(09)60255-5. [DOI] [PubMed] [Google Scholar]
- 8.Stasi R. Therapeutic strategies for hepatitis- and other infection-related immune thrombocytopenias. Semin Hematol. 2009;46:S15–25. doi: 10.1053/j.seminhematol.2008.12.006. [DOI] [PubMed] [Google Scholar]
- 9.Rajan SK, Espina BM, Liebman HA. Hepatitis C virus-related thrombocytopenia: Clinical and laboratory characteristics compared with chronic immune thrombocytopenic purpura. Br J Haematol. 2005;129:818–24. doi: 10.1111/j.1365-2141.2005.05542.x. [DOI] [PubMed] [Google Scholar]
- 10.Zhang L, Li H, Zhao H, Ji L, Yang R. Hepatitis C virus-related adult chronic idiopathic thrombocytopenic purpura: Experience from a single Chinese centre. Eur J Haematol. 2003;70:196–7. doi: 10.1034/j.1600-0609.2003.00032.x. [DOI] [PubMed] [Google Scholar]
- 11.Iga D, Tomimatsu M, Endo H, Ohkawa S, Yamada O. Improvement of thrombocytopenia with disappearance of HCV RNA in patients treated by interferon-alpha therapy: Possible aetiology of HCV-associated immune thrombocytopenia. Eur J Haematol. 2005;75:417–23. doi: 10.1111/j.1600-0609.2005.00524.x. [DOI] [PubMed] [Google Scholar]
- 12.Peck-Radosavljevic M, Wichlas M, Pidlich J, Sims P, Meng G, Zacherl J, et al. Blunted thrombopoietin response to interferon alfa-induced thrombocytopenia during treatment for hepatitis C. Hepatology. 1998;28:1424–9. doi: 10.1002/hep.510280535. [DOI] [PubMed] [Google Scholar]
- 13.Adinolfi LE, Giordano MG, Andreana A, Tripodi MF, Utili R, Cesaro G, et al. Hepatic fibrosis plays a central role in the pathogenesis of thrombocytopenia in patients with chronic viral hepatitis. Br J Haematol. 2001;113:590–5. doi: 10.1046/j.1365-2141.2001.02824.x. [DOI] [PubMed] [Google Scholar]
- 14.Bordin G, Ballaré M, Zigrossi P, Bertoncelli MC, Paccagnino L, Baroli A, et al. A laboratory and thrombokinetic study of HCV-associated thrombocytopenia: A direct role of HCV in bone marrow exhaustion? Clin Exp Rheumatol. 1995;13:S39–43. [PubMed] [Google Scholar]
- 15.Ballard HS. Hematological complications of alcoholism. Alcohol Clin Exp Res. 1989;13:706–20. doi: 10.1111/j.1530-0277.1989.tb00408.x. [DOI] [PubMed] [Google Scholar]
- 16.McCormick PA, Murphy KM. Splenomegaly, hypersplenism and coagulation abnormalities in liver disease. Baillieres Best Pract Res Clin Gastroenterol. 2000;14:1009–31. doi: 10.1053/bega.2000.0144. [DOI] [PubMed] [Google Scholar]
- 17.Weksler BB. Review article: The pathophysiology of thrombocytopenia in hepatitis C virus infection and chronic liver disease. Aliment Pharmacol Ther. 2007;26:13–9. doi: 10.1111/j.1365-2036.2007.03512.x. [DOI] [PubMed] [Google Scholar]
- 18.Hamaia S, Li C, Allain JP. The dynamics of hepatitis C virus binding to platelets and 2 mononuclear cell lines. Blood. 2001;98:2293–300. doi: 10.1182/blood.v98.8.2293. [DOI] [PubMed] [Google Scholar]
- 19.Nagamine T, Ohtuka T, Takehara K, Arai T, Takagi H, Mori M. Thrombocytopenia associated with hepatitis C viral infection. J Hepatol. 1996;24:135–40. doi: 10.1016/s0168-8278(96)80021-3. [DOI] [PubMed] [Google Scholar]
- 20.Fried MW, Shiffman ML, Reddy KR, Smith C, Marinos G, Goncales FL, Jr, et al. Peginterferon alfa-2a plus ribavirin for chronic hepatitis C virus infection. N Engl J Med. 2002;347:975–82. doi: 10.1056/NEJMoa020047. [DOI] [PubMed] [Google Scholar]
- 21.Rajan S, Liebman HA. Treatment of hepatitis C related thrombocytopenia with interferon alpha. Am J Hematol. 2001;68:202–9. doi: 10.1002/ajh.1180. [DOI] [PubMed] [Google Scholar]
- 22.Sherman M, Shafran S, Burak K, Doucette K, Wong W, Girgrah N, et al. Management of chronic hepatitis C: Consensus guidelines. Can J Gastroenterol. 2007;21:25C–34C. [PMC free article] [PubMed] [Google Scholar]
- 23.Hernandez F, Blanquer A, Linares M, Lopez A, Tarin F, Cervero A. Autoimmune thrombocytopenia associated with hepatitis C virus infection. Acta Haematol. 1998;99:217–20. doi: 10.1159/000040842. [DOI] [PubMed] [Google Scholar]
- 24.Ramos-Casals M, García-Carrasco M, López-Medrano F, Trejo O, Forns X, López-Guillermo A, et al. Severe autoimmune cytopenias in treatment-naive hepatitis C virus infection: Clinical description of 35 cases. Medicine (Baltimore) 2003;82:87–96. doi: 10.1097/00005792-200303000-00003. [DOI] [PubMed] [Google Scholar]
- 25.Giannini EG, Savarino V. Thrombocytopenia in liver disease. Curr Opin Hematol. 2008;15:473–80. doi: 10.1097/MOH.0b013e32830a9746. [DOI] [PubMed] [Google Scholar]
- 26.Danish FA, Koul SS, Subhani FR, Rabbani AE, Yasmin S. Role of hematopoietic growth factors as adjuncts in the treatment of chronic hepatitis C patients. Saudi J Gastroenterol. 2008;14:151–7. doi: 10.4103/1319-3767.41739. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kuter DJ, Begley CG. Recombinant human thrombopoietin: Basic biology and evaluation of clinical studies. Blood. 2002;100:3457–69. doi: 10.1182/blood.V100.10.3457. [DOI] [PubMed] [Google Scholar]
- 28.Kaushansky K, Drachman JG. The molecular and cellular biology of thrombopoietin: The primary regulator of platelet production. Oncogene. 2002;21:3359–67. doi: 10.1038/sj.onc.1205323. [DOI] [PubMed] [Google Scholar]
- 29.Ezumi Y, Takayama H, Okuma M. Thrombopoietin, c-mpl ligand, induces tyrosine phosphorylation of Tyk2, JAK2, and STAT3, and enhances agonist-induced aggregation in platelets in vitro. FEBS Letters. 1995;374:48–52. doi: 10.1016/0014-5793(95)01072-m. [DOI] [PubMed] [Google Scholar]
- 30.Rojnuckarin P, Drachman JG, Kaushansky K. Thrompoietin-induced activation of the mitogen-activated protein kinase (MAPK) pathway in normal megakaryocytes: Role in endomitosis. Blood. 1999;94:1273–82. [PubMed] [Google Scholar]
- 31.Drachman JG, Millet KM, Kaushansky K. Thrombopoietin signal transduction requires functional JAK2, not Tyk2. J Biol Chem. 1999;274:13480–4. doi: 10.1074/jbc.274.19.13480. [DOI] [PubMed] [Google Scholar]
- 32.de Sauvage FJ, Hass PE, Spencer SD, Malloy BE, Gurney AL, Spencer SA, et al. Stimulation of megakaryocytopoiesis and thrombopoiesis by the c-mpl ligand. Nature. 1994;369:533–8. doi: 10.1038/369533a0. [DOI] [PubMed] [Google Scholar]
- 33.Kaushansky K, Lok S, Holly RD, Broudy VC, Lin N, Bailey MC, et al. Cloning and expression of murine thrombopoietin cDNA and stimulation of platelet production. Nature. 1994;369:565–8. doi: 10.1038/369565a0. [DOI] [PubMed] [Google Scholar]
- 34.Kaushansky K, Lok S, Holly RD, Broudy VC, Lin N, Bailey MC, et al. Promotion of megakaryocyte progenitor expansion and differentiation by the c-mpl ligand thrombopoietin. Nature. 1994;369:568–71. doi: 10.1038/369568a0. [DOI] [PubMed] [Google Scholar]
- 35.Wendling F, Maraskovsky E, Debili N, Florindo C, Teepe M, Titeux M, et al. C-mpl ligand is a humoral regulator of megakaryocytopoiesis. Nature. 1994;369:571–4. doi: 10.1038/369571a0. [DOI] [PubMed] [Google Scholar]
- 36.Li J, Yang C, Xia Y, Bertino A, Glaspy J, Roberts M, et al. Thrombocytopenia caused by the development of antibodies to thrombopoietin. Blood. 2001;98:3241–8. doi: 10.1182/blood.v98.12.3241. [DOI] [PubMed] [Google Scholar]
- 37.Basser RL, O'Flaherty E, Green M, Edmonds M, Nichol J, Menchaca DM, et al. Development of pancytopenia with neutralizing antibodies to thrombopoietin after multicycle chemotherapy supported by megakaryocyte growth and development factor. Blood. 2002;99:2599–602. doi: 10.1182/blood.v99.7.2599. [DOI] [PubMed] [Google Scholar]
- 38.Bartley TD, Bogenberger J, Hunt P, Li YS, Lu HS, Martin F, et al. Identification and cloning of a megakaryocyte growth and development factor that is a ligand for the cytokine receptor mpl. Cell. 1994;77:1117–24. doi: 10.1016/0092-8674(94)90450-2. [DOI] [PubMed] [Google Scholar]
- 39.Harker LA, Roskos LK, Marzec UM, Carter RA, Cherry JK, Sundell B, et al. Effects of megakaryocyte growth and development factor on platelet production, platelet life span, and platelet function in healthy human volunteers. Blood. 2000;95:2514–22. [PubMed] [Google Scholar]
- 40.Panzer S. Eltrombopag in chronic idiopathic thrombocytopenic purpura and HCV-related thrombocytopenia. Drugs Today. 2009;45:93–9. doi: 10.1358/dot.2009.45.2.1322479. [DOI] [PubMed] [Google Scholar]
- 41.Erickson-Miller CL, DeLorme E, Tian SS, Hopson CB, Stark K, Giampa L, et al. Discovery and characterization of a selective, nonpeptidyl thrombopoietin receptor agonist. Exp Hematol. 2005;33:85–93. doi: 10.1016/j.exphem.2004.09.006. [DOI] [PubMed] [Google Scholar]
- 42.Luengo JI, Duffy KJ, Shaw AN, Delorme E, Wiggall KJ, Giampa L, et al. Discovery of SB-497115, a small-molecule thrombopoietin (TPO) receptor agonist for the treatment of thrombocytopenia. Blood. 2004;104:2910–0. [Google Scholar]
- 43.Kalota A, Brennan K, Erickson-Miller C, Danet G, Carroll M, Gewirtz A. Effects of SB559457, a novel small molecule thrombopoietin receptor agonist, on haematopoietic cell growth and differentiation. Blood. 2004;104:2913. [Google Scholar]
- 44.Erickson-Miller C, Delorme E, Giampa L, Hopson C, Valoret E, Tian SS, et al. Biological activity and selectivity for Tpo receptor of the orally bioavailable, small molecule Tpo receptor agonist, SB-497115 [abstract] Blood. 2004;104:796a–2912. [Google Scholar]
- 45.Erickson-Miller CL, Delorme E, Tian SS, Hopson CB, Landis AJ, Valoret EI, et al. Preclinical Activity of Eltrombopag (SB-497115), an Oral, Nonpeptide Thrombopoietin Receptor Agonist. Stem Cells. 2009;27:424–30. doi: 10.1634/stemcells.2008-0366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Jenkins JM, Williams D, Deng Y, Uhl J, Kitchen V, Collins D, et al. Phase I clinical study of eltrombopag, an oral, nonpeptide thrombopoietin receptor agonist. Blood. 2007;109:4739–41. doi: 10.1182/blood-2006-11-057968. [DOI] [PubMed] [Google Scholar]
- 47.Sellers T, Hart T, Semanik M, Murthyl K. Pharmacology and safety of SB-497115-GR, an orally active small molecular weight TPO receptor agonist, in chimpanzees, rats and dogs. Blood. 2004;104:2063–3. [Google Scholar]
- 48.Erickson-Miller CL, Luengo JI, Nicholl R, Williams D, Baidoo C, Phillips J, et al. In vitro and in vivo biology of a small molecular weight TPO receptor agonist, SB-497115. Poster presented at the 96th American Association for Cancer Research Annual Meeting, Anaheim, CA, April. 2005 Apr;:16–20. [Google Scholar]
- 49.Bussel JB, Cheng G, Saleh MN, Psaila B, Kovaleva L, Meddeb B, et al. Eltrombopag for the treatment of chronic idiopathic thrombocytopenic purpura. N Engl J Med. 2007;357:2237–47. doi: 10.1056/NEJMoa073275. [DOI] [PubMed] [Google Scholar]
- 50.Jenkins JM, Williams D, Deng Y, Uhl J, Kitchen V, Collins D, et al. Phase 1 clinical study of eltrombopag, an oral, nonpeptide thrombopoietin receptor agonist. Blood. 2007;109:4739–41. doi: 10.1182/blood-2006-11-057968. [DOI] [PubMed] [Google Scholar]
- 51.Jenkins JM, Williams D, Deng Y, Uhl J, Kitchen V, Collins D, et al. An oral, non-peptide, small molecule thrombopoietin receptor agonist increases platelet counts in healthy subjects. Blood. 2004;104:2916. [Google Scholar]
- 52.Erhardt J, Erickson-Miller CL, Tapley P. SB 497115-GR, a low molecular weight TPOR agonist, does not induce platelet activation or enhance agonist-induced platelet aggregation in vitro. Blood. 2004;104:3888. [Google Scholar]
- 53.Provan D, Saleh M, Goodison S, Rafi R, Stone N, Hamilton JM, et al. The safety profile of eltrombopag, a novel, oral platelet growth factor, in thrombocytopenic patients and healthy subjects. J Clin Oncol. 2006;24:18S–18S. Suppl. [Google Scholar]
- 54.McHutchison JG, Dusheiko G, Shiffman ML, Rodriguez-Torres M, Sigal S, Bourliere M, et al. Eltrombopag for Thrombocytopenia in Patients with Cirrhosis Associated with Hepatitis C. N Engl J Med. 2007;357:2227–36. doi: 10.1056/NEJMoa073255. [DOI] [PubMed] [Google Scholar]
- 55.Bussel JB, Provan D, Shamsi T, Cheng G, Psaila B, Kovaleva L, et al. Effect of eltrombopag on platelet counts and bleeding during treatment of chronic idiopathic thrombocytopenic purpura: A randomized, double-blind, placebo-controlled trial. Lancet. 2009;373:641–8. doi: 10.1016/S0140-6736(09)60402-5. [DOI] [PubMed] [Google Scholar]
- 56.McHutchison JG, Afdhal NH, Dusheiko G, Shiffman ML, Rodriguez-Torres M, Sigal S, et al. Eltrombopag, an oral platelet growth factor, facilitates initiation of interferon therapy in subjects with HCV associated thrombocytopenia: Results from a phase II placebo controlled, double-blind, dose-ranging study [abstract] Hepatology. 2006;44:692a. [Google Scholar]
- 57.Garnock-Jones KP, Keam SJ. Eltrombopag. Drugs. 2009;69:567–76. doi: 10.2165/00003495-200969050-00005. [DOI] [PubMed] [Google Scholar]
- 58.Serebruany VL, Eisert C, Sabaeva E, Makarov L. Eltrombopag (Promacta), a Thrombopoietin Receptor Agonist for the Treatment of Thrombocytopenia: Current and Future Considerations. Am J Ther. 2009 May 15; doi: 10.1097/MJT.0b013e318199d6b7. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 59.Vadhan-Raj S, Verschraegen CF, Bueso-Ramos C, Broxmeyer HE, Kudelkà AP, Freedman RS, et al. Recombinant human thrombopoietin attenuates carboplatin-induced severe thrombocytopenia and the need for platelet transfusions in patients with gynaecologic cancer. Ann Intern Med. 2000;132:364–8. doi: 10.7326/0003-4819-132-5-200003070-00005. [DOI] [PubMed] [Google Scholar]
- 60.Fanucchi M, Glaspy J, Crawford J, Garst J, Figlin R, Sheridan W, et al. Effects of polyethylene glycol-conjugated recombinant human megakaryocyte growth and development factor on platelet counts after chemotherapy for lung cancer. N Engl J Med. 1997;336:404–9. doi: 10.1056/NEJM199702063360603. [DOI] [PubMed] [Google Scholar]
- 61.Basser RL, Underhill C, Davis I, Green MD, Cebon J, Zalcberg J, et al. Enhancement of platelet recovery after myelosuppressive chemotherapy by recombinant human megakaryocyte growth and development factor in patients with advanced cancer. J Clin Oncol. 2000;18:2852–61. doi: 10.1200/JCO.2000.18.15.2852. [DOI] [PubMed] [Google Scholar]
- 62.Erhardt JA, Erickson-Miller CL, Aivado M, Abboud M, Pillarisetti K, Toomey JR. Comparative analyses of the small molecule thrombopoietin receptor agonist eltrombopag and thrombopoietin on in vitro platelet function. Exp Hematol. 2009;37:1030–7. doi: 10.1016/j.exphem.2009.06.011. [DOI] [PubMed] [Google Scholar]
- 63.Ulich TR, del Castillo J, Senaldi G, Kinstler O, Yin S, Kaufman S, et al. Systemic hematologic effects of PEG-rHuMGDF-induced megakaryocyte hyperplasia in mice. Blood. 1996;87:5006–15. [PubMed] [Google Scholar]
- 64.Yanagida M, Ide Y, Imai A, Toriyama M, Aoki T, Harada K, et al. The role of transforming growth factor-beta in PEG-rHuMGDF-induced reversible myelofibrosis in rats. Br J Haematol. 1997;99:739–45. doi: 10.1046/j.1365-2141.1997.4843288.x. [DOI] [PubMed] [Google Scholar]
- 65.Yan XQ, Lacey D, Fletcher F, Hartley C, McElroy P, Sun Y, et al. Chronic exposure to retroviral vector encoded MGDF (mpl-ligand) induces lineage-specific growth and differentiation of megakaryocytes in mice. Blood. 1995;86:4025–33. [PubMed] [Google Scholar]
- 66.Villeval JL, Cohen-Solal K, Tulliez M, Giraudier S, Guichard J, Burstein SA, et al. High thrombopoietin production by hematopoietic cells induces a fatal myeloproliferative syndrome in mice. Blood. 1997;90:4369–83. [PubMed] [Google Scholar]
- 67.Douglas VK, Tallman MS, Cripe LD, Peterson LC. Thrombopoietin administered during induction chemotherapy to patients with acute myeloid leukemia induces transient morphologic changes that may resemble chronic myeloproliferative disorders. Am J Clin Pathol. 2002;117:844–50. doi: 10.1309/09NP-3DFG-BLM9-E5LE. [DOI] [PubMed] [Google Scholar]
- 68.Arnold DM, Nazi I, Kelton JG. New treatments for idiopathic thrombocytopenic purpura: Rethinking old hypotheses. Expert Opin Investig Drugs. 2009;18:805–19. doi: 10.1517/13543780902905848. [DOI] [PubMed] [Google Scholar]
- 69.Cohn CS, Bussel JB. Romiplostim: A second-generation thrombopoietin agonist. Drugs Today (Barc) 2009;45:175–88. doi: 10.1358/dot.2009.45.3.1343793. [DOI] [PubMed] [Google Scholar]
- 70.Kuter DJ. Thrombopoietin and thrombopoietin mimetics in the treatment of thrombocytopenia. Annu Rev Med. 2009;60:193–206. doi: 10.1146/annurev.med.60.042307.181154. [DOI] [PubMed] [Google Scholar]
- 71.Williams DD, Peng B, Bailey CK, Wire MB, Deng Y, Park JW, et al. Effects of food and antacids on the pharmacokinetics of eltrombopag in healthy adult subjects: Two single-dose, open-label, randomized-sequence, crossover studies. Clin Ther. 2009;31:764–76. doi: 10.1016/j.clinthera.2009.04.010. [DOI] [PubMed] [Google Scholar]
- 72.Vizcaíno G, Diez-Ewald M, Vizcaíno-Carruyo J. Treatment of chronic immune thrombocytopenic purpura.Looking for something better. Invest Clin. 2009;50:95–108. [PubMed] [Google Scholar]
- 73.Ikeda Y, Miyakawa Y. Development of thrombopoietin receptor agonists for clinical use. J Thromb Haemost. 2009;7:239–44. doi: 10.1111/j.1538-7836.2009.03440.x. [DOI] [PubMed] [Google Scholar]
- 74.Tillmann HL, Patel K, McHutchison JG. Role of growth factors and thrombopoietic agents in the treatment of chronic hepatitis C. Curr Gastroenterol Rep. 2009;11:5–14. doi: 10.1007/s11894-009-0002-x. [DOI] [PubMed] [Google Scholar]


