Summary
The clinical value of therapeutic suggestions during general anaesthesia was assessed in a double-blind randomised placebo-controlled study. 39 unselected patients were allocated to suggestion (n =19) or control (n = 20) groups who were played either recorded therapeutic suggestions or a blank tape, respectively, during hysterectomy. The patients in the suggestion group spent significantly less time in hospital after surgery, suffered from a significantly shorter period of pyrexia, and were generally rated by nurses as having made a better than expected recovery. Patients in the suggestion group, unlike those in the control group, guessed accurately that they had been played an instruction tape.
INTRODUCTION
Evidence increasingly suggests that operating theatre sounds are probably registered in some areas of the cortex during general anaesthesia and these sounds may influence recovery from surgery.1 Cortical auditory evoked responses are not abolished by inhalational anaesthetic agents even at concentrations above those required for surgery2 and, although very few patients can recall intraoperative events,3-6 a more sensitive assessment of learning found significant postoperative recognition of words presented during general anaesthesia.7. Furthermore, patients who are unable to recall instructions made during surgery may still obey them postoperatively: 11 patients who were told during anaesthesia to touch their ears during a subsequent interview did so significantly more frequently than control patients,8 a finding replicated in patients who had cardiac surgery.9 Patients may also respond to therapeutic suggestions made during surgery. Two uncontrolled studies reported that therapeutic suggestions during anaesthesia improved recovery from surgery,10,11 a conclusion supported by two double-blind randomised controlled studies. Pearson12 found that patients who heard tape-recorded therapeutic suggestions left hospital significantly sooner than those played music or blank tapes, but the suggestion and control groups were not matched for type of surgery. Bonke and colleagues13 reported similar findings with cholecystectomy patients but only in older people. We conducted a double-blind randomised controlled study to examine further the hypothesis that the quality and duration of recovery from surgery would be improved by therapeutic suggestions made during general anaesthesia.
PATIENTS AND METHODS
Every patient admitted to St Thomas' Hospital for a total abdominal hysterectomy over a twelve-week period was invited to take part in the study, which was approved by the West Lambeth Health Authority ethics committee. 4 patients declined, 2 failed to complete the questionnaires, and 1 was excluded because a second operation was needed. The characteristics of the remaining 39 subjects are summarised in table I.
TABLE I.
POTENTIAL CONFOUNDING VARIABLES
| — | Control group (n = 20) |
Suggestion group (n = 19) |
|---|---|---|
|
| ||
| Age (yr) | 43·80 (7·1) | 41·79 (6·5) |
| Preoperative anxiety (20–60) | 43·95 (12·9) | 41·00 (9·4) |
| Intraoperative blood loss (ml) | 309·17 (221·2) | 314·80 (181·5) |
| Duration of surgery (min) | 66·31 (16·8) | 70·63 (23·9) |
| Ethnic origin of patient | ||
| Caucasian | 9 | 13 |
| Afro-Caribbean | 11 | 6 |
| Anaesthetist's experience | ||
| Consultant | 8 | 10 |
| Other | 12 | 8 |
| Surgeon's experience | ||
| Consultant | 18 | 12 |
| SR/registrar | 2 | 7 |
Mean (SD).
Patients were randomly played a suggestion tape or a visually indistinguishable blank control tape: the one played to each patient was not known until the end of the study. A waterproof auto-reverse tape player (Sony WM F-63) was used in the operating theatre with purpose-built headphones which made operating theatre sounds inaudible to the patient and prevented the tape being overheard by the anaesthetist. 12 minutes of suggestions were repeated three times on each side of the suggestion tape: the major section described for 9 minutes the normal postoperative procedures with advice on how best to cope with them12 (eg, “How quickly you recover from your operation depends upon you—the more you relax, the more comfortable you will be”); then 2 minutes of direct therapeutic suggestions11,13 (eg, “You will not feel sick, you will not have any pain…”) ; and 1 minute of third person suggestions13 (eg, “The operation seems to be going very well and the patient is fine”). A complete transcript of the suggestion tape is available on request.
On the day before surgery each subject completed a questionnaire: a short form of the profile of mood states questionnaire14,15 which provides six individual mood scores (tension, depression, anger, fatigue, vigour, and confusion) and an overall negative mood score; the Spielberger state-trait anxiety inventory;16 and a 10 cm visual analogue scale17 to assess how distressed the patient felt by admission to hospital. Each patient was randomly allocated to hear a suggestion or control tape which was played from the time of the first incision to the start of wound closure. Normal anaesthetic and clinical procedures were not modified and the anaesthetist recorded the duration of surgery, the intraoperative blood loss, the anaesthetic agents used, and whether the patient showed any signs of consciousness during surgery.
When each patient got up for the first time after surgery, a nurse filled in a six point mobilisation rating scale to assess the amount of help required; any vomiting was recorded. The number of half-days when a temperature exceeded 37.3°C was recorded for the first 5 postoperative days, as was analgesia usage. On the fifth day after surgery, each patient was asked to complete the mood and anxiety questionnaires again, and to make visual analogue scale ratings of: pain intensity; distress caused by pain; difficulty with micturition, flatulence, and defaecation; and severity of nausea. Each patient was asked whether she had any memories or dreams from the time of the operation, and to guess whether she had been played an instruction or a blank tape. The date of discharge was recorded to the nearest half-day, and the nurses were asked to assess patient recovery (worse than expected, as expected, or better than expected).
One-way analyses of variance and covariance were used to compare the mean scores of the suggestion and control groups on all continuous variables. The Fisher exact probability test18 was applied to all 2 × 2 contingency tables for analysis of categorical variables.
RESULTS
There were no significant differences between the preoperative mood and distress scores for the suggestion and control groups. 33 patients were anaesthetised with thiopentone, nitrous oxide, and halothane; 6 were given enflurane (4 from the suggestion group; 2 from the control group). No significant differences between the two groups were found for the distribution of ward or bed (single room vs open bay) or allocation to clinical firms. Table I summarises other potentially confounding variables: no significant differences between the suggestion and control groups were found for age, ethnic origin, preoperative anxiety, intraoperative blood loss, duration of surgery, or anaesthetist's and surgeon's experience.
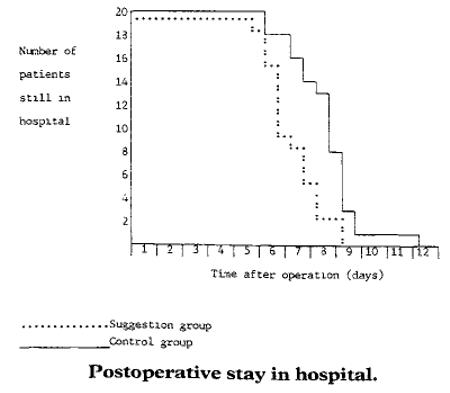
Table II displays the mean scores and the distribution of the main dependent variables for the suggestion and control groups. The mean postoperative stay for the suggestion group was 1.3 days (16%) less than the control group (p <0.002). Patients' age was not significantly associated with the duration of postoperative hospital stay. Postoperative stay for the two groups is shown in the figure. The suggestion group patients also experienced 1.8 (45%) fewer half-days of pyrexia (p <0.005), and reported a significant reduction in gastrointestinal problems (p <0.03). No significant differences were detected between the suggestion and control groups for the quality of mobilisation or difficulty with micturition. 2 patients in each group required catheterisation. Reported nausea, the incidence of vomiting, and analgesia requirement did not differ significantly between the two groups, nor did severity of the distress from pain on the fifth postoperative day. Mood and anxiety scores on the fifth postoperative day did not differ significantly between the two groups and the introduction of the preoperative scores as covariates did not alter this. Almost every member of the suggestion group was rated by nurses as having made a better than expected recovery; in contrast most controls were rated as having made typical or poorer than expected recoveries from surgery (p <0.002). No patient was able to recall any intraoperative events or conversation. All but 1 of the suggestion group patients guessed correctly that they had been played an instruction tape during surgery, whilst the control group guessed no better than chance would predict.
TABLE II.
DEPENDENT VARIABLES
| — | Control group |
Suggestion group |
P |
|---|---|---|---|
|
| |||
| Postoperative stay (d) | 8·4 (1·3) | 7·1 (1·0) | <0·002 |
| Pyrexia (half-days) | 3·9 (2 2) | 2·2 (1·2) | <0·005 |
| Difficulties with bowels (0–100) | 55·7 (34·1) | 31·3 (29·2) | <0 ·03 |
| Flatulence (0–100) | 57·9 (33·1) | 63·4 (36·4) | NS |
| Mobilisation rating (0–5) | 2·6 (1·1) | 3·1 (0·9) | NS |
| Urinary difficulties (0–100) | 26·5 (32·7) | 13·7 (19·6) | NS |
| Nausea (0–100) | 43·4 (40·3) | 28·3 (31·6) | NS |
| Pain intensity (0–100) | 26·5 (25·4) | 23 9 (20·0) | NS |
| Pain distress (0–100) | 20·8 (27·4) | 18·2 (18·2) | NS |
| Record of vomiting | |||
| No vomiting | 12 | 14 | |
| Vomited | 8 | 5 | NS |
| Nurses' assessment of recovery | |||
| *Poorer than or as expected | 14 | 1 | |
| Better than expected | 6 | 16 | <0·002 |
| Patient guess of tape contents | |||
| Blank tape | 11 | 1 | |
| Instruction tape | 9 | 18 | <0·004 |
Only 3 patients were reported to have made a worse than expected recovery; the poorer than and as expected groups were therefore combined because this small cell size prevented the chi-squared test from being used.
DISCUSSION
The results of this study imply that therapeutic suggestions during anaesthesia may significantly reduce the duration and improve the quality of recovery from hysterectomy surgery. This conclusion is consistent with previous controlled research involving different types of surgery.12,13 Many factors determine the quality and duration of recovery and observer error may have affected some of the measures, but these factors should have been equally distributed between the randomly allocated suggestion and control groups who were assessed double-blind. Surgical patients are usually exposed to operating theatre sounds rather than silence and the control condition does not, therefore, represent normal clinical practice. However, earlier studies12,13 found that silence and operating theatre sounds have similar effects upon recovery. The nursing assessments of the quality of recovery also imply that the control condition was equivalent to normal clinical practice and that the patients who were played suggestions during surgery made better recoveries than expected. Furthermore, over 50% of the suggestion group were discharged within a day of suture removal in contrast with only 10% of the control group.
Inappropriate or misinterpreted operating theatre comments may have a harmful effect upon recovery19-23 and suggestions that patients' ears should be plugged during surgery have been made.1,24,25 Our results suggest that auditory perception without awareness may instead be employed to the benefit of the patient. None of our patients was able to recall any intraoperative events or sounds and the ward staff had no access to the visually indistinguishable tapes played in the operating theatre. The accuracy with which the suggestion group patients guessed that they had been played an instruction tape suggests that auditory perception was maintained at some level during general anaesthesia. The stress associated with an operation can affect resistance to infection, rate of blood clotting, and other mechanisms likely to be involved in the physical recovery from surgery.26 Psychophysiological mechanisms27-29 may have accounted for the suggestion group's improved and accelerated recovery. The recommendations on the suggestion tape (eg, frequent mobilisation) may also have contributed to these effects. There is little information about the most effective types of suggestion to use and future studies may find ways of increasing their therapeutic effect; the effectiveness of these therapeutic suggestions may be increased by exposure during induction of anaesthesia and during recovery30,31 in addition to the deepest period of anaesthesia used for this study.
Acknowledgments
Sony UK Ltd kindly donated the cassette players used in the operating theatre. We thank the members of the Departments of Obstetrics and Gynaecology and Anaesthesia and the nurses at St Thomas' Hospital.
REFERENCES
- 1.Editorial Advertising during anaesthesia? Lancet. 1986;ii:1019–20. [PubMed] [Google Scholar]
- 2.Thornton C, Catley DM, Jordan C, Lehane JR, Royston D, Jones JG. Enflurane anaesthesia causes graded changes in the brainstem and early cortical auditory evoked response in man. Br J Anaesth. 1983;55:479–86. doi: 10.1093/bja/55.6.479. [DOI] [PubMed] [Google Scholar]
- 3.Eich E, Reeves JL, Katz RL. Anesthesia, amnesia, and the memory/awareness distinction. Anesth Analg. 1985;64:1143–48. [PubMed] [Google Scholar]
- 4.Dubovsky SL, Trustman R. Absence of recall after general anesthesia: implications for theory and practice. Anesth Analg. 1976;55:696–701. doi: 10.1213/00000539-197609000-00018. [DOI] [PubMed] [Google Scholar]
- 5.Eisenberg L, Taub HA, Burana A. Memory under diazepam-morphine neuroleptanesthesia in male surgical patients. Anesth Analg. 1974;53:488–95. [PubMed] [Google Scholar]
- 6.Browne RA, Catton DV. A study of awareness during anesthesia. Anesth Analg. 1973;52:128–32. [PubMed] [Google Scholar]
- 7.Millar K, Watkinson N. Recognition of words presented during general anaesthesia. Ergonomics. 1983;26:585–94. doi: 10.1080/00140138308963377. [DOI] [PubMed] [Google Scholar]
- 8.Bennett HL, Davis HS, Giannini JA. Non-verbal response to intraoperative conversation. Br J Anaesth. 1985;57:174–79. doi: 10.1093/bja/57.2.174. [DOI] [PubMed] [Google Scholar]
- 9.Goldmann L, Shah MV, Hebden MW. Memory of cardiac anaesthesia. Psychological sequelae in cardiac patients of intra-operative suggestion and operating room conversation. Anaesthesia. 1987;42:596–603. doi: 10.1111/j.1365-2044.1987.tb03082.x. [DOI] [PubMed] [Google Scholar]
- 10.Wolfe LS, Millett JB. Control of post-operative pain by suggestion under general anesthesia. Am J Clin Hypn. 1960;3:109–12. [Google Scholar]
- 11.Hutchings DD. The value of suggestion given under anesthesia: a report and evaluation of 200 cases. Am J Clin Hypn. 1961;4:26–29. [Google Scholar]
- 12.Pearson RE. Response to suggestions given under general anesthesia. Am J Clin Hypn. 1961;4:106–14. [Google Scholar]
- 13.Bonke B, Schmitz PIM, Verhage F, Zwaveling A. Clinical study of so-called unconscious perception during general anaesthesia. Br J Anaesth. 1986;58:957–94. doi: 10.1093/bja/58.9.957. [DOI] [PubMed] [Google Scholar]
- 14.McNair DM, Lorr M, Droppleman LF. Profile of mood states manual. Educational and Industrial Testing Service; San Diego: 1971. [Google Scholar]
- 15.Steptoe A, Cox S. The acute effects of aerobic exercise on mood. Health Psychol. doi: 10.1037//0278-6133.7.4.329. (in press) [DOI] [PubMed] [Google Scholar]
- 16.Spielberger CD, Gorsuch RL, Lushene RE. Manual of the state-trait anxiety inventory. Consulting Psychologists Press; Palo Alto, CA: 1970. [Google Scholar]
- 17.Huskisson EC. Visual analogue scales. In: Melzack R, editor. Pain measurement and assessment. Raven Press; New York: 1983. pp. 33–37. [Google Scholar]
- 18.Finney DJ. Tables for testing in a 2 × 2 contingency table. Cambridge University Press; Cambridge: 1963. [Google Scholar]
- 19.Levinson BW. States of awareness during general anaesthesia. Br J Anaesth. 1965;37:544–46. doi: 10.1093/bja/37.7.544. [DOI] [PubMed] [Google Scholar]
- 20.Levinson BW. States of awareness under general anaesthesia. Med Proc (S Afr) 1965;11:243–45. doi: 10.1093/bja/37.7.544. [DOI] [PubMed] [Google Scholar]
- 21.Cheek DB. Unconscious perception of meaningful sounds during surgical anesthesia as revealed under hypnosis. Am J Clin Hypn. 1959;1:101–13. [Google Scholar]
- 22.Is your anesthetised patient listening? JAMA. 1968;206:1004. Editorial. [Google Scholar]
- 23.Howard JF. Incidents of auditory perception during anaesthesia with traumatic sequelae. Med J Aust. 1987;146:44–46. doi: 10.5694/j.1326-5377.1987.tb120126.x. [DOI] [PubMed] [Google Scholar]
- 24.Davis R. Anaesthesia, amnesia, dreams and awareness. Med J Aust. 1987;146:4–5. doi: 10.5694/j.1326-5377.1987.tb120114.x. [DOI] [PubMed] [Google Scholar]
- 25.Scott DL. Awareness during general anaesthesia. Can Anaesth Soc J. 1972;19:173–83. doi: 10.1007/BF03005047. [DOI] [PubMed] [Google Scholar]
- 26.Mathews A, Ridgeway V. Personality and surgical recovery: a review. Br J Clin Psychol. 1981;20:243–60. doi: 10.1111/j.2044-8260.1981.tb00525.x. [DOI] [PubMed] [Google Scholar]
- 27.Steptoe A. Psychophysiological processes in disease. In: Steptoe A, Mathews A, editors. Health care and human behaviour. Academic Press; London: 1984. [Google Scholar]
- 28.Depression, stress, and immunity. Lancet. 1987:1467–68. Editorial. [PubMed] [Google Scholar]
- 29.Kiecolt-Glaser JK, Glaser R. Psychosocial moderators of immune function. Ann Behav Med. 1987;9:16–20. [Google Scholar]
- 30.Aldrete JA. Cessation of cigarette smoking by suggestion in the perianesthetic period. Anesthesiol Rev. 1987;14:22–24. [Google Scholar]
- 31.Bonnett OT. Effects of positive suggestions on surgical patients. Pac Med Surg. 1966;74:297–300. [PubMed] [Google Scholar]


