Abstract
Background
The treatment of fractures in children and adolescents must be based on an adequate knowledge of the physiology of the growing skeleton. Treatment failures usually do not result from technical deficiencies, but rather from a misunderstanding of the special considerations applying to the treatment of fractures in this age group.
Methods
We selectively reviewed recent publications on the main types of long bone fracture occurring in the period of skeletal development.
Results
Alleviating pain is the first step in fracture management, and due attention must be paid to any evidence of child abuse. The goals of treatment are to bring about healing of the fracture and to preserve the function of the wounded limb. The growth that has yet to take place over the remaining period of skeletal development also has to be considered. Predicting the growth pattern of fractured bones is a basic task of the pediatric traumatologist. During the period of skeletal development, conservative and surgical treatments are used in complementary fashion. Particular expertise is needed to deal with fractures around the elbow, especially supracondylar humeral fractures, displaced fractures of the radial condyle of the humerus, radial neck fractures, and radial head dislocations (Monteggia lesions). These problems account for a large fraction of the avoidable cases of faulty fracture healing leading to functional impairment in children and adolescents.
Conclusion
The main requirements for the proper treatment of fractures in children and adolescents are the immediate alleviation of pain and the provision of effective treatment (either in the hospital or on an outpatient basis) to ensure the best possible outcome, while the associated costs and effort is kept to a minimum. Further important goals are a rapid recovery of mobility and the avoidance of late complications, such as restriction of the range of motion or growth disorders of the fractured bone. To achieve these goals, the treating physician should have the necessary expertise in all of the applicable conservative and surgical treatment methods and should be able to apply them for the proper indications.
Fractures occur more often in the pediatric age group than in healthy adults (1, e1). One reason for this is that children and adolescents are less skilled at risk assessment (e2, e3). Furthermore, bone is less stable—albeit much more elastic—during skeletal development than in adulthood. These properties explain both the higher incidence and the more rapid healing of fractures in children and adolescents. The skeleton is a dynamically growing organ whose growth characteristics and reactions to trauma are well known (2– 4, e4). Treatment of fractures in young patients demands precise knowledge of the radiographic anatomy and growth characteristics of healthy and damaged bones as well as the specific fracture dynamics in this age group (e5). Nevertheless, a glance at the figures from the arbitration committees of the German Medical Associations clearly shows that children are too often treated as though they were simply small adults. A higher than average proportion of complaints connected with treatment of fractures occurring during the period of skeletal development are sustained. Confirmed errors include:
Imprecise clinical assessment
Misinterpretation of the radiographic findings
Inappropriate choice of conservative or surgical treatment
Absent or inadequate follow-up.
The highest error rate (77%) was found for fractures in the region of the elbow joint.
In this article we review the epidemiology, diagnosis, treatment, and aftercare of fractures in children and adolescents, analyzing published reports and drawing on our own data and experience. We focus on fractures of the long bones of the upper limb. The article is intended to acquaint its readers with the specific characteristics of fractures in the pediatric age group and enable them to recognize cases in which specialized treatment is necessary.
Method
This article is based on our own personal experience and on a selective review of the literature. The Medline and Cochrane databases were searched for publications featuring various combinations of relevant terms. Documents published in the past 10 years were preferred (89%), but fundamental studies from the second half of the 20th century were also included. Evidence-based clinical studies on the treatment of fractures during the period of skeletal development often focus on pain management, plaster configuration, or surgical technique (5– 7). Randomized studies and meta-analyses on these aspects of treatment are less common (e6– e11). Most publications are treatment studies with level IV evidence.
Results
Epidemiological data and classification
Comparison of epidemiological data from historical studies with our own data shows a similar distribution of the various fractures (table 1) (8). Male children and adolescents are affected more frequently, linked with their higher levels of activity and risk-taking (1, e2). There are higher than average rates of metaphyseal and diaphyseal fractures (90%). The customary classifications were used (AO, Arbeitsgemeinschaft Osteosynthese—Association for the Study of Internal Fixation; Li-La, Light and Laughter for Sick Children—Efficiency in Medicine) (2, 4, 9, 10).
Table 1. Distribution of fractures of the long tubular bones during the period of skeletal development.
| Two-digit fracture site code | Region | Number | Percentage |
| 1.1. | Proximal humerus | 73 | 4.1 |
| 1.2. | Humeral diaphysis | 20 | 1.1 |
| 1.3. | Distal humerus | 278 | 15.6 |
| 2.1. | Proximal forearm | 68 | 3.8 |
| 2.2. | Diaphyseal forearm | 193 | 10.8 |
| 2.3. | Distal forearm | 728 | 40.8 |
| Sum | Upper extremity | 1360 | 76.3 |
| 3.1. | Proximal femur | 11 | 0.6 |
| 3.2. | Femoral diaphysis | 57 | 3.2 |
| 3.3. | Distal femur | 25 | 1.4 |
| 4.1. | Proximal lower leg | 36 | 2.0 |
| 4.2. | Diaphyseal lower leg | 128 | 7.2 |
| 4.3. | Distal lower leg | 166 | 9.3 |
| Sum | Lower extremity | 423 | 23.7 |
| Total | 1783 | 100 |
The two-digit fracture site codes are identical in the AO and Li-La classifications. The data are modified from (9). AO, Arbeitsgemeinschaft Osteosynthese—Association for the Study of Internal Fixation; Li-La, Light and Laughter for Sick Children—Efficiency in Medicine
Circumstances of injury
The case history must reveal an adequate explanation for the fracture. It is particularly important in young patients to distinguish accidents from non-accidental injuries (pathological fracture, child abuse). If trivial trauma results in broken bones, pathological fractures (e.g., in the presence of juvenile bone cysts), albeit rare, have to be excluded. Delayed presentation, shaft fractures in infants who are not yet walking, and inconsistent or contradictory accounts of what happened point to child abuse. Typical patterns of injury in child abuse are metaphyseal fractures or bone fragments, subperiosteal hematomas, and fractures of different ages (11, e12– e14).
Diagnosis and fracture types
Clinical examination is initially restricted to inspection. Testing for the primary signs of fracture (abnormal mobility, crepitation) would cause the child unnecessary pain and must therefore be dispensed with (4). The periphery must be investigated for accompanying injuries (blood supply, sensation, and mobility).
The workhorse of fracture diagnosis in pediatric traumatology remains conventional radiography (12). In every case radiographs of the injured site including the neighboring joints are obtained in two projections. The images must be painstakingly analyzed and the fractures examined for signs of instability (e15). Some shaft fractures can be diagnosed reliably by sonography (compression fractures) (e16). Computed tomography and magnetic resonance imaging have no place in acute diagnosis (e17– e19).
Fractures in children and adolescents show typical maturation-dependent characteristics (table 2). The epiphyseal cartilages act as buffers to axial trauma. Additional torsion or shear forces lead to injury of these growth plates (table 3) (13, 14).
Table 2. Typical fracture types during the period of skeletal development and their characteristics.
| Fracture type | Location | Mechanism | Characteristics | Stability |
| Compression fracture | Metaphysis | Compression | Principally in distal forearm | Stable |
| Greenstick fracture | Metaphysis, diaphysis | Compression and bending | Cortex interrupted on convex side but preserved on concave side (angulation) | Stable |
| Bowing fracture | Metaphysis, diaphysis | Bending | As for greenstick fracture, only plastic deformation with no fracture separation | Stable |
| Complete fracture | Metaphysis | Bending/ torsion | Angulation and complete displacement | Unstable |
| Transverse and oblique fractures (with/without bending wedge) | Diaphysis | Direct trauma with torsion | Complete displacement, angulation, shortening | Unstable |
| Torsion fracture (with/without bending wedge) | Diaphysis | Indirect trauma with torsion | Displacement, shortening, angulation | Unstable |
Assessment of stability, together with the prognosis for growth, determines the treatment plan
Table 3. Classification of growth plate injuries.
| Fracture type | Location | Mechanism | Characteristics | Metaphysis: shaft (S); epiphysis: articular (A) |
| Harris-Salter I | Metaphysis | Bending/torsion | Physeal separation | S |
| Harris-Salter II, Aitken I | Metaphysis | Bending/torsion | Physeal separation with metaphyseal wedge | S |
| Harris-Salter III, Aitken II | Epiphysis | Bending/torsion | Epiphyseal fracture | A |
| Harris-Salter IV, Aitken III | Epiphysis and metaphysis | Bending/torsion | Fracture across growth plate | A |
| Harris-Salter V | Epiphyseal growth plate | Crush | Never proved | S |
Classification of injuries involving the growth plates according to Aitken (14) and Salter und Harris (15). These are the most commonly used classifications for this region. In the German-language literature, the terms Fugenschaftfraktur (growth plate–shaft fracture) and Fugengelenkfraktur (growth plate–articular fracture) (4) highlight the involvement of the metaphyseal or epiphyseal portion of the growth plate
Growth prognosis
Before planning the treatment of a fracture during the period of skeletal development it is essential to draw up a growth prognosis, so that in the case of displaced fractures both the potential for spontaneous correction and the risk of growth disorder can be assessed (e5). Both of these developments—spontaneous correction and growth disorder—are possible only if the remaining growth period is sufficiently long, and both depend on:
Age
Sex
Stage of development
Fracture location
Direction of displacement
Extent of displacement (4).
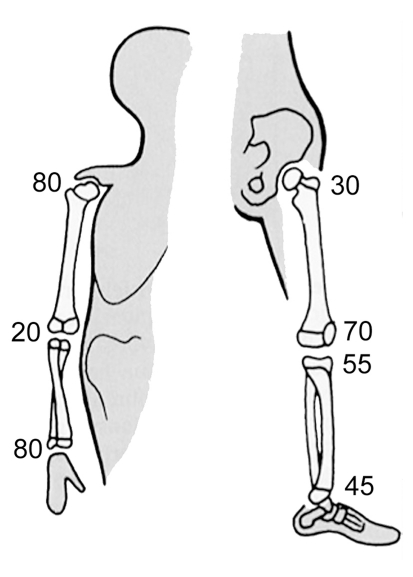
The growth dynamics and times of fusion of the various growth plates are known. In the upper extremity, the proximal growth plate of the humerus and the distal plates of the forearm are each responsible for 80% of longitudinal growth in their respective segments of the limb and are late to fuse (at the ages of 14 to 16 and 14 to 18 years, respectively) (3, 4). In the lower limb the growth plates at the knee joint contribute 40% to 60% of longitudinal growth (figure 1).
Figure 1.
The growth plates of the long bones do not contribute equally to longitudinal growth. The numbers in this illustration show the percentage contributions of each growth plate. Plates that contribute a higher proportion of growth also fuse later (from: v. Laer L, Kraus R, Linhart W: Frakturen und Luxationen im Wachstumsalter. 5th edition 2007. Stuttgart, New York: Thieme 2007; reproduced by kind permission of Thieme-Verlag, Stuttgart)
If a growth plate contributes intensively to growth over a long period of time, it has a higher potential for spontaneous correction of posttraumatic malalignment, but also higher vulnerability to growth disorders. The growth plates of the upper limb are less prone to growth disorders and are more likely to correct malalignments (e5, e10, e20– e24). The physes in the lower limb are much more vulnerable to growth disorders. Malalignments in the sagittal plane are corrected better than those in the coronal plane. Rotational deformities are compensated only non-specifically in the context of physiological changes in torsion (4).
Treatment principles
The primary goal of treatment is freedom from pain. Provisional immobilization of the injured limb even before diagnostic investigation provides pain relief and can be supported by medication (non-steroidal antirheumatics, opiates) (6, e6, e7, e25). Any painful manipulations, particularly reduction and correction of malalignment, must be carried out with the patient under anesthesia.
Once it has been decided to anesthetize the patient, management must be definitive. Unplanned changes in procedure and repeat interventions should be regarded as complications of treatment. Fragile vital signs or endangered viability of the affected limb require urgent intervention (e26– e28). All other measures can be carried out with less urgency, provided adequate pain treatment is initiated (e29).
Children in unforeseen situations can suffer great distress if separated from their attachment figures (parents), so there should be provision for a parent to stay in hospital with an injured child. Outpatient or short inpatient treatment enables a swift return to the familiar social environment and minimizes stress for the child and the family. The treatment should be designed to support rather than suppress the child’s natural urge to be active (e30).
Treatment methods
Conservative and surgical treatment options are available. The choice of method depends on the extent of primary displacement and on the age, location, and stability of the fracture (e30). Undisplaced or acceptably displaced fractures are treated conservatively. An acceptable displacement is one that will definitely be corrected by the anticipated growth in length and thickness of the injured bone. The literature contains ample information on the correction that can be expected depending on fracture location and patient age (2– 4, e5, e22, e23).
If reduction is required, a manipulation technique must be selected that excludes any risk of redisplacement (e31, e32). If this is not possible with immobilization alone, operative stabilization is necessary (e24).
In the epiphysis, joint surface reconstruction can be achieved by means of Kirschner wires or compression screws, usually after open reduction (e33– e37). Arthroscopic monitoring of reduction is also possible. Metaphyseal fragments can usually be reduced well in closed technique, but fixation is often required. This can be attained with Kirschner wires (in which case additional plaster cast immobilization is required) (e11, e38– e40), with screws, or in individual cases by insertion of an intramedullary rod (19, e41– e43). Diaphyseal fractures are nowadays mostly treated surgically (e30). The method of choice for longitudinally stable transverse fractures is elastic stable intramedullary nailing (ESIN) (e44– e50). The external fixator is an alternative for longitudinally unstable oblique, spiral, or multifragmentary fractures (e5– e53).
Plate fixation is used only occasionally, in adolescents with fractures in close proximity to joints. Interlocking nails are used solely for diaphyseal fractures in patients just before the end of growth (table 4).
Table 4. Treatment of pediatric fractures.
| Method | Remarks |
| Functional | Redression (e.g., collar-and-cuff bandage), functional bandage (Desault, Gilchrist) with acceptable degree of deformity |
| Immobilization | Plaster cast, conventional (white) or synthetic (rigid or semirigid; if necesary, correction by cast wedging |
| Adaptation osteosynthesis (Kirschner wires) | Metaphyseal fractures: additional plaster cast immobilization necessary (unstable) |
| Screw fixation | Epiphyseal fractures or physeal separations with metaphyseal wedge after precise reduction |
| ESIN (elastic stable intramedullary nailing) | In longitudinally stable (transverse) diaphyseal fractures (also greenstick fractures of forearm shaft; as intramedullary rod in proximal upper arm fractures, supracondylar humeral fractures, and radial neck fractures |
| External fixator | In longitudinally unstable diaphyseal fractures |
| Plate fixation | As an exception, in fractures close to joints in adolescents |
| Medullary or locking nail | In diaphyseal fractures in adolescents |
Summary of the standard treatment methods for fractures during the period of skeletal development. In selected individual cases, any methods or implants used in general traumatology (arthroscopy, bone replacement materials, angle-stable plates, etc.) may be employed
Each method has its own indications. The burden for the patient, the extent and duration of temporary function-limiting malalignments, and individual preferences must always be taken into account.
Follow-up
Compression fractures do not involve displacement, so follow-up radiography is unnecessary (e23). Conservative treatment of unstable fractures can be followed by secondary displacement; therefore, radiographs should be obtained 7 and 28 days after treatment.
Fractures treated by fixation undergo radiological examination 4 weeks after operation and before planned metal removal. Bone healing, range of motion, and load-bearing capacity are assessed by clinical examination. As soon as mobility is almost back to normal, the patient can resume sporting activity.
Overview of fractures
In the following summary of the principal fractures of the long bones of the upper limb particular attention is paid to the most frequently occurring errors in treatment.
Proximal upper arm
Intra-articular epiphyseal fractures during the period of skeletal development represent a rare occurrence (3, 4). Injuries of this region are mostly physeal separations and metaphyseal fractures with considerable potential for spontaneous correction of up to 40° before adulthood (15, e5, e21, e51). More severely angulated unstable fractures and those displaced by more than the width of the shaft are treated by reduction and ESIN (15, e41, e45). Internal fixation by means of Kirschner wires (instability) or plates (invasiveness) is inappropriate (e54).
Upper arm shaft
Fractures of the shaft of the upper arm are rare. Long oblique or spiral fractures can be treated with plaster or a brace with early resumption of function (15). Axial malalignments of more than 10° will not resolve spontaneously and must be dealt with (4, e4, e54). Transverse fractures are ideal for management with ESIN (e53, e55). The occasionally occurring primary radial nerve palsy does not constitute an indication for surgery per se, as the rate of spontaneous remission is high (e53, e54, e56– e59). Nevertheless, the patients benefit from early physiotherapy after surgical stabilization.
Distal upper arm
The fractures of the distal upper arm most likely to involve complications during the period of skeletal development include supracondylar humerus fracture and radial condyle fracture (16). Because growth at the plates above and below the elbow joint is only slight, residual malalignments are compensated only in the plane of motion (antecurvation) up to the 7th year of life (4, 17) and may result in severe restrictions of movement (e39, e40, e60, e61).
Supracondylar humerus fractures are classified by their degree of displacement (grades I–IV [18]). Up to 10% of cases are complicated by primary vascular and neural damage, and 20% of these patients require additional surgical treatment (e62, e63). The goal of reduction is to deal with axial deviations that cannot be corrected spontaneously (varus, valgus, and rotational deformities) (4, e29, e38). Because of the shortness of the joint-bearing fragment, fixation is always indicated in the case of displacement (grade III and IV) (2– 4, 7, 19, e38, e64, e65). The options are K-wire osteosynthesis (more stable crossed than unilateral), descending ESIN, and radial external fixator (e39, e45, e52, e64– e73). K-wire fixation involves a 10% risk of damaging the ulnar nerve (e74– e76). The arm must also be immobilized in plaster. In contrast, the technically far more demanding descending ESIN (19) or, as an alternative, the radial external fixator offers primary stability of movement (e72, e77).
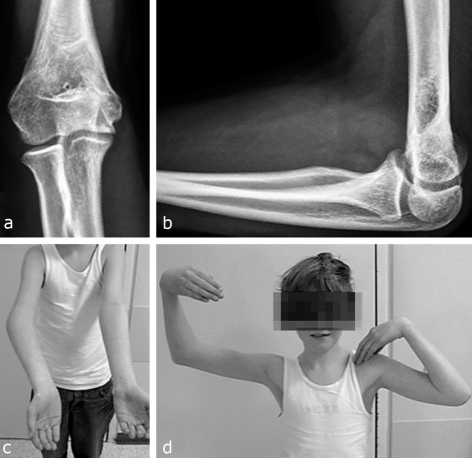
Assessment of the radiograph of a reduced supracondylar humerus fracture may be difficult (7, 12, 17, e15). Rotational deformities can be interpreted incorrectly. Unrecognized, they lead to instability and tilting and result in cosmetically bothersome varus deformities (e78– e80) (figure 2). Intraoperative clinical inspection of the arm axes with control of elbow joint motion is therefore indispensable (20, e81, e82). A number of operations have been reported for correction of the posttraumatic cubitus varus (e83– e89).
Figure 2.
Radiographs and clinical photographs of an 11-year-old boy 2 years after malunion of a supracondylar fracture of the humerus: cubitus varus (a, c), antecurvation (b), and severe impairment of flexion (d). A varus deformity of this kind is not compensated by growth at any age, the antecurvation only until the 7th year of life at the latest
Radial condyle fracture is the most common intra-articular fracture during the period of skeletal development (e90, e91). When displaced, such a fracture requires open reduction and stable (tension screw) fixation to avoid pseudarthrosis (e33, e35, e36), which can lead to valgus deformity and secondary instability (e92– e96). Correct primary management is essential, because secondary operative correction yields clinically inferior results (21, e97– e100). Additional diagnostic measures are necessary in primarily non-displaced fractures to exclude secondary dislocation (e92, e94, e96). Since the peak age for lateral humeral condyle fracture is 4 to 5 years, magnetic resonance imaging necessitates anesthesia and thus represents a major intervention.
Sonography (22, e16) may be painful and high-quality devices are not universally available. The diagnostic standard for exclusion of secondary dislocation is therefore plaster-free radiography 4 to 5 days after treatment—this follow-up examination is indispensable (2, 4, 12, e81, e94).
Epicondylar avulsion fractures cause no growth disorders (4). The ossific nucleus of the lateral epicondyle must not be misinterpreted as a fracture fragment (e15). If avulsion of the medial epicondyle occurs in the context of dislocation of the elbow, one must exclude the presence of a fragment in the joint space (e101). In cases with a tendency to redislocation, e.g., when there is gross displacement, the fragment has to be refixed with the aid of a cannulated screw (e102– e104).
Proximal forearm
Fractures of the proximal forearm are rare, but occur in all age groups. Intra- and extra-articular fractures of the olecranon are found (cave: Monteggia fracture). Intra-articular step-offs are reduced precisely and fixed in place (e105). Almost all fractures of the proximal end of the radius are extra-articular radial neck fractures (4). Although the proximal radial growth plate contributes only a small proportion of the total longitudinal growth, up to the 10th year of life realignment of the growth plate can yield pronounced correction of axial deviations (up to 50°) (23, e106– e108). In older children, axial deviations of over 20° require closed reduction, e.g., by means of ESIN (e42, e43, e45, e109, e110). Elevation by means of the joystick technique (e111) may lead to rupture of the last connecting piece of periosteum that is maintaining the blood supply. Complete dislocation of the radial head necessitates open reduction (23, e43, e44, e107, e108, e111). Intra-articular head fractures occur only after growth is complete.
Common to all injuries in and around the elbow is the fact that physiotherapy is necessary only in exceptional cases; sometimes it may even be counterproductive (e112). Chronic physeal separations, periarticular calcifications, and persisting restrictions of movement have been described, but they have to be distinguished from sporadically occurring, non-influenceable aseptic bony necrosis (2– 4, e24).
Forearm shaft
Most greenstick fractures occur in the forearm. In up to 30% of cases the bone rebreaks within 12 months because of uneven fracture healing. If the concave side is therapeutically fractured (risk of instability) or the convex side compressed, the incidence of refracture decreases. Complete fractures of the forearm have a high rate of redisplacement (up to 50%) if they are reduced without operative stabilization (4, 24, e46, e113, e114). For this reason such fractures should be managed with ESIN in patients over 3 years of age (24, e115– e118). This surgical intervention is minimally invasive yet yields an optimal treatment outcome with a low rate of complications (e44– e46, e113, e118– e122). Both greenstick and complete fractures may impair pronation and supination of the forearm owing to changes in bony geometry (e123– e127). Post-traumatic axial malalignments should therefore not be left untreated (3, 4, 24, e115, e128, e129).
In the Monteggia fracture, a fracture of the ulna (complete displaced shaft fractures, bowing fracture, olecranon fracture) (e130– e132) is accompanied by dislocation of the head of the radius. Despite the repeated descriptions of this combined injury in the literature, the radial head dislocation is often overlooked (2– 4, 12, e4, e130). Therefore, in every patient with a fracture of the ulna, whether diaphyseal or metaphyseal, dislocation of the head of the radius must be actively excluded. On every radiological projection the axis of the neck of the radius is aligned with the center of the capitellum. Fresh radial head dislocations simply require axial correction, sometimes accompanied by ulnar osteosynthesis, but the treatment of old dislocations is elaborate, involving angulation osteotomy of the ulna, and prone to complications (21, e133– e136).
Distal forearm
Compression fractures heal with no problems. They require immobilization in plaster for 2–4 weeks (e9). Radiographic follow-up is unnecessary, as the bony healing can be monitored by clinical examination (e22– e24, e137, e138).
Both greenstick and complete fractures, particularly beyond the metaphysis, tend to angulate and must be checked radiologically at 7 to 10 days after injury (e139). Studies on the management of these very common fractures show a high rate of redisplacement after conservative treatment and a high complication rate for K-wire fixation (e140– e143). Some authors advocate encasing the whole arm in plaster, but this seems to have no advantage over a forearm cast (e8, e99, e144). A Cochrane Review showed a tendency towards swifter healing after K-wire fixation (5). Up to the 10th or even 12th year of life the distal radius has a particularly marked potential for spontaneous correction of post-traumatic deformities (e20, e145). Corrections of up to 50° have been observed (4). However, it may not be reasonable to expect the patient and his/her family to put up with a bayonet deformity for a period of several months, so this decision should be discussed with all involved (e10, e22).
Conclusion
This review of the treatment principles for fractures of the long bones, particularly those in the upper limb, during the period of bony growth can do no more than give an impression of the depth of knowledge of the physiology of skeletal development that is needed for the proper practice of pediatric traumatology. To do justice to our young patients, we always have to estimate future growth, assessing on one hand the potential for spontaneous correction and on the other the likelihood of growth disorders, taking into account the patient’s age, the fracture site, and the direction and extent of displacement. Also important is the ability to work together with the patient and parents in each individual case to achieve an optimal treatment outcome. This requires good communication skills. Possession of the requisite aptitude for correct selection and application of conservative and surgical treatment options is a self-evident requirement. A number of textbooks and compendia on pediatric traumatology—each emphasizing different aspects of the topic—have recently been published in German, giving the interested reader a solid foundation for appropriate and successful treatment of fractures in children and adolescents.
Key Messages.
Treatment of every fracture starts with appropriate pain therapy.
A growth prognosis represents an essential basis for treatment planning.
The pediatric traumatologist must be proficient in the whole spectrum of conservative and surgical treatments —which are complementary rather than competing.
Most cases of faulty treatment of injuries to the elbow joint are due to incorrect assessment of growth potential, misinterpretation of radiographs, and errors of tehnique.
If left untreated, axial malalignments following forearm fractures lead to persisting impairments of pronation and supination; angulated fractures of the distal forearm, on the other hand, are characterized by a considerable potential for correction.
Acknowledgments
Translated from the original German by David Roseveare.
Footnotes
Conflict of interest statement
The authors declare that no conflict of interest exists according to the guidelines of the International Committee of Medical Journal Editors.
References
- 1.Jones IE, Williams SM, Dow N, Goelding A. How many children remain fracture free during growth? A longitundinal study of children and adolescents participating in the Dunedin Multidisciplinary Health and Development Study. Osteoporos Int. 2002;13:990–995. doi: 10.1007/s001980200137. [DOI] [PubMed] [Google Scholar]
- 2.Marzi I, editor. Kindertraumatologie. Darmstadt: Steinkopff; 2006. [Google Scholar]
- 3.Weinberg AM, Tscherne H, editors. Berlin: Springer; 2006. Unfallchirurgie im Kindesalter. [Google Scholar]
- 4.v. Laer L, Kraus R, Linhart W. 5th edition. Stuttgart, New York: Thieme; 2007. Frakturen und Luxationen im Wachs-tumsalter. [Google Scholar]
- 5.Abraham A, Handoll HHG, Khan T. Interventions for treating wrist fractures in children. Cochrane Database of Systematic Reviews. 2008;(2) doi: 10.1002/14651858.CD004576.pub2. Art. No.: CD004576. DOI:10.1002/14651858.CD004576.pub2. [DOI] [PubMed] [Google Scholar]
- 6.Furyk JS, Grabowski WJ, Black LH. Nebulized fentanyl versus intravenous morphine in children with suspected limb fractures in the emergency department: a randomized controlled trial. Emerg Med Australas. 2009;21:203–209. doi: 10.1111/j.1742-6723.2009.01183.x. [DOI] [PubMed] [Google Scholar]
- 7.Tripuraneni KR, Bosch PP, Schwend RM, Yaste JJ. Prospective, surgeon-randomized evaluation of crossed pins versus lateral pins for unstable supracondylar humerus fractures in children. J Pediatr -Orthop B. 2009;18:93–98. doi: 10.1097/BPB.0b013e32832989ff. [DOI] [PubMed] [Google Scholar]
- 8.Kraus R, Schneidmüller D, Röder C. Aktuelle Daten zur Häufigkeit von Frakturen langer Röhrenknochen im Wachstumsalter. Dtsch Arztebl. 2005;102(12):A 838–A 842. [Google Scholar]
- 9.Slongo TF, Audige L. AO Pediatric Classification Group. Fracture and dislocation classification compendium for children: the AO padiatric comprehensive classification of long bone fractures (PCCF) J Orthop Trauma. 2007;21:135–160. doi: 10.1097/00005131-200711101-00020. [DOI] [PubMed] [Google Scholar]
- 10.Schneidmüller D, von Laer L, Li La. Klassifikation für Frakturen im Kindesalter. In: Marzi I, editor. Kindertraumatologie. Darmstadt: Steinkopff; 2006. pp. 23–27. [Google Scholar]
- 11.Durand C, Baudain P, Nugues F, Besaquet S. Osteoarticular manifestations of battered child syndrome. J Radiol. 1999;80:556–558. [PubMed] [Google Scholar]
- 12.Kraus R, Berthold LD, von Laer L. Effiziente Bildgebung von Ellenbogenverletzungen bei Kindern und Jugendlichen. Klein Paediat. 2007;219:282–289. doi: 10.1055/s-2007-970588. [DOI] [PubMed] [Google Scholar]
- 13.Aitken AP, Magill HK. Fractures involving the distal femoral epiphyseal cartilage. JBJS A. 1952;34:96–108. [PubMed] [Google Scholar]
- 14.Salter RB, Harris WR. Injuries involving the epiphyseal plate. J Bone Joint Surg. 1963;45:587–663. [Google Scholar]
- 15.Schmittenbecher PP, Blum J, David S, Knorr P, Marzi I, Schlickewei W, Schönecker G. Die Behandlung von Humerusschaftfrakturen und subkapitalen Humerusfrakturen im Kindesalter. Konsensusbericht der Sektion Kindertraumatologie der DGU. Unfallchirurg. 2004;107:8–14. doi: 10.1007/s00113-003-0717-3. [DOI] [PubMed] [Google Scholar]
- 16.Shrader MW. Pediatric supracondylar fractures and pediatric physeal elbow fractures. Orthop Clin North Am. 2008;39(2):163–171. doi: 10.1016/j.ocl.2007.12.005. [DOI] [PubMed] [Google Scholar]
- 17.Wessel LM, Günter SM, Jablonski M, Sinnig M, Weinberg A-M. Wie lässt sich die Wachstumsprognose nach kindlicher suprakondylärer Humerusfraktur erfassen? Orthopäde. 2003;32:824–832. doi: 10.1007/s00132-003-0469-3. [DOI] [PubMed] [Google Scholar]
- 18.Weinberg AM, Marzi I, Günter SM, Wessel L, Riedel J, von Laer L. Die suprakondyläre Oberarmfraktur im Kindesalter - eine Effizienzstudie. Ergebnisse der multizentrischen Studie der Sektion Kindertraumatologie der Deutschen Gesellschaft für Unfallchirurgie - Teil I: Epidemiologie, Effektivitätsprüfung und Klassifikation. Unfall-chirurg. 2002;105:208–216. doi: 10.1007/s001130100314. [DOI] [PubMed] [Google Scholar]
- 19.Weinberg AM, v. Bismarck S, Castellani C, Mayr J. Deszendierende intramedulläre Nagelung zur Behandlung dislozierter suprakondy-lärer Oberarmfrakturen im Kindesalter. Chirurg. 2003;74:432–436. doi: 10.1007/s00104-002-0595-1. [DOI] [PubMed] [Google Scholar]
- 20.Wessel L. Diagnostik der supracondylären Oberarmfraktur. Hefte zur Zeitschrift „Der Unfallchirurg“. 1998;272:598–607. [Google Scholar]
- 21.Günther P, Wessel LM. Korrektureingriffe nach ellenbogennahen Frakturen. Unfallchirurg. 2002;105:478–482. doi: 10.1007/s00113-001-0360-9. [DOI] [PubMed] [Google Scholar]
- 22.Vocke-Hell AK, Schmid A. Sonographic differentiation of stable and unstable lateral condyle fractures of the humerus in children. J Pediatr Orthop. 2001;B10:138–141. [PubMed] [Google Scholar]
- 23.Vocke-Hell AK, von Laer L. Die Prognose proximaler Radiusfrakturen im Wachstumsalter. Unfallchirurg. 1998;101:287–295. doi: 10.1007/s001130050270. [DOI] [PubMed] [Google Scholar]
- 24.Schmittenbecher PP. State-of-the-art treatment of forearm shaft fractures. Injury. 2005;36:A25–A34. doi: 10.1016/j.injury.2004.12.010. [DOI] [PubMed] [Google Scholar]
- e1.Landin LA. Epidemiology of children’s fractures. J Peadiatr -Orthop B. 1997;6:79–83. doi: 10.1097/01202412-199704000-00002. [DOI] [PubMed] [Google Scholar]
- e2.Brudvik C, Hove LM. Childhood fractures in Bergen. Norway: Identifying High risk groups and activities. J Pediatr Orthop. 2003;23:629–634. doi: 10.1097/00004694-200309000-00010. [DOI] [PubMed] [Google Scholar]
- e3.Khosla S, Melton LJ, Dekutoski MB, Achenbach SJ, Oberg AL, Riggs BL. Incidence of childhood distal forearm fractures over 30 years: a population-based study. JAMA. 2003;290:1479–1485. doi: 10.1001/jama.290.11.1479. [DOI] [PubMed] [Google Scholar]
- e4.Beaty JH, Kasser JR, Skaggs DL. 7th edition. Philadelphia: Lippincott Williams and Wilkins; 2009. Rockwood and Wilkins Fractures in Children. [Google Scholar]
- e5.Wilkins KE. Principles of fracture remodeling in children. Injury. 2005;36(Suppl 1):A 3–A 11. doi: 10.1016/j.injury.2004.12.007. [DOI] [PubMed] [Google Scholar]
- e6.Mahar PJ, Rana JA, Kennedy CS, Christopher NC. A randomized clinical trial of oral transmucosal fentanyl citrate vs. intravenous morphine sulfate for initial control of pain in children with extremity injuries. Pediatr Emerg Care. 2007;23:544–548. doi: 10.1097/PEC.0b013e318128f80b. [DOI] [PubMed] [Google Scholar]
- e7.Drendel AL, Gorelick MH, Weisman SJ, LLyon R, Brousseau DC, Kim MK. A randomized clinical trial of ibuprofen versus acet-aminophen with codeine for acute pediatric arm fracture pain. Ann Emerg Med. 2009;54:553–560. doi: 10.1016/j.annemergmed.2009.06.005. [DOI] [PubMed] [Google Scholar]
- e8.Bohm ER, Bubbar V, Yong Hing K, Dzus A. Above and below-the-elbow plaster casts for distal forearm fractures in children. A randomized controlled trial. JBJS A. 2006;88(1):1–8. doi: 10.2106/JBJS.E.00320. [DOI] [PubMed] [Google Scholar]
- e9.Oakley EA, Ooi KS, Barnett PL. A randomized controlled trial of 2 methods of immobilizing torus fractures of the distal forearm. Pediatr Emerg Care. 2008;24:65–70. doi: 10.1097/PEC.0b013e318163db13. [DOI] [PubMed] [Google Scholar]
- e10.Ploegmakers JJ, Verheyen CC. Acceptance of angulation in the non-operative treatment of paediatric forearm fractures. J Pediatr Orthop B. 2006;15:428–432. doi: 10.1097/01.bpb.0000210594.81393.fe. [DOI] [PubMed] [Google Scholar]
- e11.Shamsuddin SA, Penafort R, Sharaf I. Crossed-pin versus lateral-pin fixation in pediatric supracondylar fractures. Med J Malaysia. 2001;56(Suppl D):38–44. [PubMed] [Google Scholar]
- e12.Jayakumar P, Barry M, Ramachandran M. Orthopaedic aspects of paediatric non-accidental injuries. J Bone Joint Surg B. 2010;92:189–195. doi: 10.1302/0301-620X.92B2.22923. [DOI] [PubMed] [Google Scholar]
- e13.Jones JC, Feldman KW, Bruckner JD. Child abuse in infants with proximal physeal injuries of the femur. Pediatr Emerg Care. 2004;20:157–161. doi: 10.1097/01.pec.0000117923.65522.6f. [DOI] [PubMed] [Google Scholar]
- e14.Ravichandiran N, Schuh S, Bejuk M, et al. Delayed identification of pediatric abuse-related fractures. Pediatrics. 2010;125:60–66. doi: 10.1542/peds.2008-3794. [DOI] [PubMed] [Google Scholar]
- e15.Jacoby SM, Herman MJ, Morrison WB, Osterman AL. Pediatric Elbow Trauma. An Orthopaedic Perspective on the Importance of Radiographic Interpretation. Sem Musculoskel Radiol. 2007;11:48–56. doi: 10.1055/s-2007-984412. [DOI] [PubMed] [Google Scholar]
- e16.Hübner U, Schlicht W, Outzen S, Barthel M, Halsband H. Ultrasound in the diagnosis of fractures in children. J Bone Joint Surg B. 2000;82:1170–1173. doi: 10.1302/0301-620x.82b8.10087. [DOI] [PubMed] [Google Scholar]
- e17.Chapman VM, Grottkau BE, Albright M, Salamipour H, Jaramillo D. Multidetector computed tomography of pediatric lateral condylar fractures. J Comput Assist Tomogr. 2005;29:842–846. doi: 10.1097/01.rct.0000175504.64707.e3. [DOI] [PubMed] [Google Scholar]
- e18.Schneidmüller D, Maier D, Mack M, Straub R, Marzi I. Therapeutic relevance of magnetic resonance imaging in joint injuries in children. Unfallchirurg. 2005;108:537–543. doi: 10.1007/s00113-005-0936-x. [DOI] [PubMed] [Google Scholar]
- e19.Zimmermann R, Rudisch A, Fritz D, Gschwentner M, Arora R. MRT zur Beurteilung von Begleitverletzungen distaler Unterarmbrüche im Wachstumsalter. Handchir Mikrochir Plast Chir. 2007;39:60–67. doi: 10.1055/s-2007-964926. [DOI] [PubMed] [Google Scholar]
- e20.Cannata G, De Maio F, Mancini F. Ippolito. Physeal fractures of the distal radius and ulna: long-term prognosis. J Orthop Trauma. 2003;17:172–179. doi: 10.1097/00005131-200303000-00002. [DOI] [PubMed] [Google Scholar]
- e21.David S, Kuhn C, Ekkernkamp A. Proximale Humerusfraktur des Kindes und Adoleszenten. Eine häufig überbehandelte Fraktur. Chirurg. 2006;77:827–834. doi: 10.1007/s00104-006-1191-6. [DOI] [PubMed] [Google Scholar]
- e22.Do TT, Strub WM, Foad SL, Mehlman CT, Crawford AH. Reduction versus remodeling in pediatric distal forearm fractures: a preliminary cost analysis. J Pediatr Orthop B. 2003;12:109–115. doi: 10.1097/01.bpb.0000043725.21564.7b. [DOI] [PubMed] [Google Scholar]
- e23.May G, Grayson A. Towards evidence based emergency medicine: best BETs from the Manchester Royal Infirmary. Bet 3: do buckle fractures of the paediatric wrist require follow up? Emerg Med J. 2009;26:819–822. doi: 10.1136/emj.2009.082891. [DOI] [PubMed] [Google Scholar]
- e24.von Laer L, Kraus R. Die konservative Behandlung von Frakturen der langen Röhrenknochen im Wachstumsalter. Unfallchirurg. 2007;109:811–823. doi: 10.1007/s00113-007-1318-3. [DOI] [PubMed] [Google Scholar]
- e25.Shepherd M, Aickin R. Paracetamol versus ibuprofen: a ran-domized controlled trial of outpatient analgesia efficiacy for pediatric acute limb fractures. Emerg Med Australas. 2009;21:484–490. doi: 10.1111/j.1742-6723.2009.01232.x. [DOI] [PubMed] [Google Scholar]
- e26.Grottkau BE, Epps HR, Di Scala C. Compartment syndrome in children and adolescents. J Pediatr Surg. 2005;40:678–682. doi: 10.1016/j.jpedsurg.2004.12.007. [DOI] [PubMed] [Google Scholar]
- e27.Walmsley PJ, Kelly MB, Robb JE, Annan IH, Porter DE. Delay -increases the need for open reduction of type-III supracondylar fractures of the humerus. J Bone Joint Surg Br. 2006;88:528–530. doi: 10.1302/0301-620X.88B4.17491. [DOI] [PubMed] [Google Scholar]
- e28.Whitesides TE, Haney TC, Morimoto K, Harada H. Tissue pres-sure measurement as a determinant for the need of fasciotomiy. Clin Orthop. 1975;113:43–51. doi: 10.1097/00003086-197511000-00007. [DOI] [PubMed] [Google Scholar]
- e29.Mehlman CT, Strub WM, Roy DR, Wall EJ, Crawford AH. The -effect of surgical timing on the perioperative complications of treatment of supracondylar humeral fractures in children. J Bone Joint Surg Am. 2001;83:323–327. doi: 10.2106/00004623-200103000-00002. [DOI] [PubMed] [Google Scholar]
- e30.Slongo TF. The Choice of treatment according to the type and -location of the fracture and the age of the child. Injury. 2005;36(Suppl 1):A 12–A 9. doi: 10.1016/j.injury.2004.12.008. [DOI] [PubMed] [Google Scholar]
- e31.Berberich T, Reimann P, Steinacher M, Erb TO, Mayr J. Evaluation of cast wedging in a forearm fracture model. Clinical Biome-chanics. 2008;23:895–899. doi: 10.1016/j.clinbiomech.2008.04.003. [DOI] [PubMed] [Google Scholar]
- e32.Bhatia M, Housden PH. Re-displacement of paediatric forearm fractures: role of plaster moulding and padding. Injury. 2006;37:259–268. doi: 10.1016/j.injury.2005.10.002. [DOI] [PubMed] [Google Scholar]
- e33.Baharuddin M, Sharaf I. Screw osteosynthesis in the treatment of fracture lateral humeral condyle in children. Med J Malaysia. 2001;56(Suppl D):45–47. [PubMed] [Google Scholar]
- e34.Garcia-Mata S, Hidalgo-Ovejero A. Triplane fracture of the distal radius. J Ped Orthop B. 2006;15:298–301. doi: 10.1097/01202412-200607000-00013. [DOI] [PubMed] [Google Scholar]
- e35.Hasler C, v Laer L. Screw osteosynthesis in dislocated fractures of the radial condyle of the humerus in the growth period. A prospective long term study. Unfallchirurg. 1998;101:280–286. doi: 10.1007/s001130050269. [DOI] [PubMed] [Google Scholar]
- e36.Jenyo M, Mirdad T. Fractures of the lateral condyle of the -humerus in children. East Afr Med J. 2001;78:424–429. doi: 10.4314/eamj.v78i8.8995. [DOI] [PubMed] [Google Scholar]
- e37.Peterson HA. Triplane fracture of the distal radius: case report. J Pediatr Orthop. 1996;16:192–194. doi: 10.1097/00004694-199603000-00011. [DOI] [PubMed] [Google Scholar]
- e38.von Laer L, Günther SM, Knopf S, Weinberg AM. Die suprakondyläre Oberarmfraktur im Kindesalter - eine Effizienzstudie. Ergebnisse der multizentrischen Studie der Sektion Kindertraumatologie der Deutschen Gesellschaft für Unfallchirurgie - Teil II: Aufwand und Nutzen der Behandlung. Unfallchirurg. 2002;105:217–223. doi: 10.1007/s001130100315. [DOI] [PubMed] [Google Scholar]
- e39.Yu SW, Su JY, Kao FC, Ma CH, Yen CY, Tu YK. The use of the 3-mm K-Wire to supplement reduction of humeral supracondylar fractures in children. J Trauma. 2004;57:1038–1042. doi: 10.1097/01.ta.0000141877.53934.04. [DOI] [PubMed] [Google Scholar]
- e40.Zatti G, Bini A, De Pietri M, Cherubino P. The surgical treatment of supracondylar fractures of the humerus in children by percu-taneous fixation using Kirschner wires: analysis of residual -deformities. Chir Organi Mov. 2001;86:111–117. [PubMed] [Google Scholar]
- e41.Chee Y, Agorastides I, Garg N, Bass A, Bruce C. Treatment of -severely displaced proximal humeral fractures in children with elastic stable intramedullary nailing. J Pediatr Orthop B. 2006;15:45–50. doi: 10.1097/01202412-200601000-00010. [DOI] [PubMed] [Google Scholar]
- e42.Metaizeau JP. Reduction and osteosynthesis of radial neck fractures in children by centromedullary pinning. Injury. 2005;36(Suppl 1):A 75–A 77. doi: 10.1016/j.injury.2004.12.016. [DOI] [PubMed] [Google Scholar]
- e43.Ursei M, Sales de Gauzy J, Knorr J, Abid A, Darodes P, Cahuzac JP. Surgical treatment of radial neck fractures in children by intramedullary pinning. Acta Orthop Belg. 2006;72:131–137. [PubMed] [Google Scholar]
- e44.Berger P, De Graaf JS, Leemans R. The use of elastic intramedullary nailing in the stabilisation of paediatric fractures. Injury. 2005;36:1217–1220. doi: 10.1016/j.injury.2005.05.012. [DOI] [PubMed] [Google Scholar]
- e45.Dietz HG, Schmittenbecher PP, Slongo T, Wilkins KE. Stuttgart, New York: AO Publishing, Thieme; 2006. Elastic Stable Intramedullary Nailing (ESIN) in Children. [Google Scholar]
- e46.Jubel A, Andermahr J, Isenberg J, Schiffer G, Prokop A, Rehm KE. Erfahrungen mit der elastisch stabilen intramedullaren Nagelung (ESIN) diaphysarer Frakturen im Kindesalter. Orthopäde. 2004;33:928–935. doi: 10.1007/s00132-004-0662-z. [DOI] [PubMed] [Google Scholar]
- e47.Jubel A, Andermahr J, Prokop A, Bergmann H, Isenberg J, Rehm KE. Pitfalls und Komplikationen der elastisch stabilen intramedullaren Nagelung (ESIN) von Femurfrakturen im Kindesalter. Unfallchirurg. 2004;107:744–749. doi: 10.1007/s00113-004-0799-6. [DOI] [PubMed] [Google Scholar]
- e48.Lascombes P, Haumont T, Journeau P. Use and abuse of flexible intramedullary nailing in children and adolescents. J Pediatr -Orthop. 2006;26:827–834. doi: 10.1097/01.bpo.0000235397.64783.d6. [DOI] [PubMed] [Google Scholar]
- e49.Mann D, Schnabel M, Baacke M, Gotzen L. Ergebnisse der elastisch stabilen intramedullaren Nagelung (ESIN) bei Unterarm-schaftfrakturen im Kindesalter. Unfallchirurg. 2003;106:102–109. doi: 10.1007/s00113-002-0474-8. [DOI] [PubMed] [Google Scholar]
- e50.Slongo TF. Complications and failures of the ESIN technique. Injury. 2005;36(Suppl 1):A 78–A 85. doi: 10.1016/j.injury.2004.12.017. [DOI] [PubMed] [Google Scholar]
- e51.Caviglia H, Garrido CP, Palazzi FF, Meana NV. Pediatric fractures of the humerus. Clin Orthop Relat Res. 2005;432:49–56. doi: 10.1097/01.blo.0000156452.91271.fb. [DOI] [PubMed] [Google Scholar]
- e52.El Hayek T, Daher AA, Meouchy W, Ley P, Chammas N, Griffet J. External fixators in the treatment of fractures in children. J Pediatr Orthop B. 2004;13:103–109. doi: 10.1097/00009957-200403000-00008. [DOI] [PubMed] [Google Scholar]
- e53.Kraus R. Oberarmschaftfrakturen im Wachstumsalter. Unfallmedizinische Schriften der Landesverbände der gewerblichen Berufsgenossenschaften. 2005;106:131–142. [Google Scholar]
- e54.Linhart WE. Schultergürtel und Oberarm Das verletzte Kind - Komplikationen vermeiden, erkennen, behandeln. In: Laer L, editor. Stuttgart New York: Thieme; 2007. pp. 41–48. [Google Scholar]
- e55.Fernandez FF, Eberhardt O, Wirth T. Elastic Stable intramedullary Nailing as alternative therapy for the management of pediatric humeral shaft fractures. Z Orthop Unfall. 2010;148:49–53. doi: 10.1055/s-0029-1186113. [DOI] [PubMed] [Google Scholar]
- e56.Larsen LB, Barfred T. Radial nerve palsy after simple fracture of the humerus. Scand J Plast Reconstr Surg Hand Surg. 2000;34:363–366. doi: 10.1080/028443100750059156. [DOI] [PubMed] [Google Scholar]
- e57.Lim KE, Yap CK, Ong SC. Aminuddin. Plate osteosynthesis of the humerus shaft fracture and its association with radial nerve -injury - a retrospective study in Melaka General Hospital. Med J Malaysia. 2001;56(Suppl C):8–12. [PubMed] [Google Scholar]
- e58.Ogawa BK, Kay RM, Choi PD, Stevanic MV. Complete division of the radial nerve associated with a closed fracture of the humeral shaft in a child. J Bone Joint Surg Br. 2007;89:821–824. doi: 10.1302/0301-620X.89B6.18942. [DOI] [PubMed] [Google Scholar]
- e59.Thomsen NO, Dahlin LB. Injury to the radial nerve caused by fracture of the humeral shaft: timing and neurobiological aspects related to treatment and diagnosis. Scand J Plast Reconstr Surg Hand Surg. 2007;41:153–157. doi: 10.1080/02844310701445586. [DOI] [PubMed] [Google Scholar]
- e60.Chung MS, Baek GH. Three-dimensional corrective osteotomy for cubitus varus in adults. J Shoulder Elbow Surg. 2003;12:472–475. doi: 10.1016/s1058-2746(03)00090-9. [DOI] [PubMed] [Google Scholar]
- e61.Devnani AS. Late presentation of supracondylar fracture of the humerus in children. Clin Orthop Relat Res. 2005;431:36–41. doi: 10.1097/01.blo.0000152439.43810.11. [DOI] [PubMed] [Google Scholar]
- e62.Ay S, Akinci M, Kamiloglu S, Ercetin O. Open reduction of displaced pediatric supracondylar humeral fractures through the anterior cubital approach. J Pediatr Orthop. 2005;25:149–155. doi: 10.1097/01.bpo.0000153725.16113.ab. [DOI] [PubMed] [Google Scholar]
- e63.Louahem DM, Nebunescu A, Canavese F, Dimeglio A. Neurovascular complications and severe displacement in supracondylar humerus fractures in children: defensive or offensive strategy? J Pediatr Orthop B. 2006;15:51–57. doi: 10.1097/01202412-200601000-00011. [DOI] [PubMed] [Google Scholar]
- e64.Akakpo-Numado GK, Mal-Lawane M, Belouadah M, Kabore B, Lefort G, Daoud S. Management of Lagrange and Rigault stage IV extension type supracondylar fracture of the humerus in children. Rev Chir Orthop Reparatrice Appar Mot. 2005;91:664–671. doi: 10.1016/s0035-1040(05)84471-x. [DOI] [PubMed] [Google Scholar]
- e65.Kaiser MM, Kamphaus A, Massalme E, Wessel LM. Percu-taneous closed pin fixation of supracondylar fractures of the -distal humerus in children. Oper Orthop Traumatol. 2008;20:297–309. doi: 10.1007/s00064-008-1402-z. [DOI] [PubMed] [Google Scholar]
- e66.Abraham E, Gordon A, Abdul-Hadi O. Management of supracondylar fractures of humerus with condylar involvement in children. J Pediatr Orthop. 2005;25:709–716. doi: 10.1097/01.bpo.0000184645.96356.fe. [DOI] [PubMed] [Google Scholar]
- e67.Brauer CA, Lee BM, Bae DS, Waters PM, Kocher MS. A systematic review of medial and lateral entry pinning vs. lateral entry pinning for supracondylar fractures of the humerus. J Pediatr -Orthop. 2007;27:181–186. doi: 10.1097/bpo.0b013e3180316cf1. [DOI] [PubMed] [Google Scholar]
- e68.Karapinar L, Ozturk H, Altay T, Kose B. Closed reduction and -percutaneous pinning with three Kirschner wires in children with type III displaced supracondylar fractures of the humerus. Acta Orthop Traumatol Turc. 2005;39:23–29. [PubMed] [Google Scholar]
- e69.Kraus R, Joeris A, Castellani C, Weinberg A, Slongo T, Schnettler R. Intraoperative radiation exposure in displaced supracondylar humeral fractures - a comparison of surgical methods. J Pediatr Orthop B. 2007;16:44–47. doi: 10.1097/01.bpb.0000236238.87763.cf. [DOI] [PubMed] [Google Scholar]
- e70.Mangwani J, Nadarajah R, Paterson JM. Supracondylar humeral fractures in children: ten years’ experience in a teaching hospital. J Bone Joint Surg Br. 2006;88:362–365. doi: 10.1302/0301-620X.88B3.16425. [DOI] [PubMed] [Google Scholar]
- e71.Skaggs DL, Cluck MW, Mostofi A, Flynn JM, Kay RM. Lateral-entry pin fixation in the management of supracondylar fractures in children. J Bone Joint Surg Am. 2004;86:702–707. doi: 10.2106/00004623-200404000-00006. [DOI] [PubMed] [Google Scholar]
- e72.Slongo T, Schmid T, Wilkins K, Joeris A. Lateral external fixation - a new surgical technique for displaced unreducible supracondylar humeral fractures in children. J Bone Joint Surg Am. 2008;90:1690–1697. doi: 10.2106/JBJS.G.00528. [DOI] [PubMed] [Google Scholar]
- e73.Weinberg AM, Fischerauer E, Castellani C. Frakturen der oberen Extremität beim Kind. Teil I: Schulter, Humerus und Ellenbogengelenk. Orthopädie und Unfallchirurgie up2date. 2008;3:1–20. [Google Scholar]
- e74.Buys Roessingh AS, Reinberg O. Open or closed pinning for distal humerus fractures in children? Swiss Surg. 2003;9:76–81. doi: 10.1024/1023-9332.9.2.76. [DOI] [PubMed] [Google Scholar]
- e75.Ozcelik A, Tekcan A, Omeroglu H. Correlation between iatrogenic ulnar nerve injury and angular insertion of the medial pin in -supracondylar humerus fractures. J Pediatr Orthop B. 2006;15:58–61. doi: 10.1097/01202412-200601000-00012. [DOI] [PubMed] [Google Scholar]
- e76.Rose RE, Phillips W. Iatrogenic ulnar neuropathies post-pinning of displaced supracondylar humerus fractures in children. West Indian Med J. 2002;51:17–20. [PubMed] [Google Scholar]
- e77.Handelsman JE, Weinberg J, Hersch JC. Corrective supracondylar humeral osteotomies using the small AO external fixator. J Pediatr Orthop B. 2006;15:194–197. doi: 10.1097/01.bpb.0000194440.75378.97. [DOI] [PubMed] [Google Scholar]
- e78.Jimulia T, Sabnis SK. Supracondylar corrective osteotomy for cubitus varus—the internal rotation component and its impor-tance. An unique bone experiment. J Postgrad Med. 1994;40:194–196. [PubMed] [Google Scholar]
- e79.Mahaisavariya B, Laupattarakasem W. Supracondylar fracture of the humerus: malrotation versus cubitus varus deformity. Injury. 1993;24:416–418. doi: 10.1016/0020-1383(93)90109-j. [DOI] [PubMed] [Google Scholar]
- e80.Usui M, Ishii S, Miyano S, Narita H, Kura H. Three-dimensional corrective osteotomy for treatment of cubitus varus after supracondylar humeral fractures. Elbow Surg. 1995;4:17–22. doi: 10.1016/s1058-2746(10)80003-5. [DOI] [PubMed] [Google Scholar]
- e81.Hasler CC, von Laer L. Prevention of growth disturbances after fractures of the lateral humeral condyle in children. J Pediatr -Orthop B. 2001;10:123–130. [PubMed] [Google Scholar]
- e82.Jain AK, Dhammi IK, Arora A, MP Singh. JS Luthra Cubitus varus: Problem and Solution. Arch Orthop Trauma Surg. 2000;120:420–425. doi: 10.1007/s004029900102. [DOI] [PubMed] [Google Scholar]
- e83.Barrett IR, Bellemore MC, Kwon YM. Cosmetic results of supracondylar osteotomy for correction of cubitus varus. J Pediatr -Orthop. 1998;18:445–447. [PubMed] [Google Scholar]
- e84.Devnani AS. Lateral closing wedge supracondylar osteotomy of humerus for post-traumatic cubitus varus in children. Injury. 1997;28:643–647. doi: 10.1016/s0020-1383(97)00139-3. [DOI] [PubMed] [Google Scholar]
- e85.Gaddy BC, Manske PR, Pruitt DL, Schoenecker PL, Rouse AM. Distal humeral osteotomy for correction of posttraumatic cubitus varus. J Pediatr Orthop. 1994;14:214–219. doi: 10.1097/01241398-199403000-00016. [DOI] [PubMed] [Google Scholar]
- e86.Hasler CC. Correction of Malunion after Pediatric Supracondylar Elbow Fractures. Closing Wedge Osteotomy and External Fixation. Eur J Trauma. 2003;29:309–315. [Google Scholar]
- e87.Hernandez MA, Roach JW. Corrective osteotomy for cubitus varus deformity. J Pediatr Orthop. 1994;14:487–491. doi: 10.1097/01241398-199407000-00012. [DOI] [PubMed] [Google Scholar]
- e88.Karatosun V, Alekberov C, Alici E, Ardic CO, Aksu G. Treatment of cubitus varus using the Ilizarov technique of distraction osteogenesis. J Bone Joint Surg Br. 2000;82:1030–1033. doi: 10.1302/0301-620x.82b7.10669. [DOI] [PubMed] [Google Scholar]
- e89.Voss FR, Kasser JR, Trepman E, Simmons E, Hall JE. Uniplanar supracondylar humeral osteotomy with preset Kirschner wires for posttraumatic cubitus varus. J Pediatr Orthop. 1994;14:471–478. doi: 10.1097/01241398-199407000-00010. [DOI] [PubMed] [Google Scholar]
- e90.Boz U, Ulusal AE, Vuruskaner H, Aydinoglu Y. Functional results of displaced lateral condyle fractures of the humerus with four-week K-wire fixation in children. Acta Orthop Traumatol Turc. 2005;39:193–198. [PubMed] [Google Scholar]
- e91.Lemme K, Lubicky JP, Zeni a, Riley E. Pediatric lateral condyle humeral fractures with and without associated elbow dislocations: a retrospective study. Am J Orthop (Belle Mead NJ) 2009;38:453–456. [PubMed] [Google Scholar]
- e92.Horn BD, Herman MJ, Crisci K, Pizzutillo PD, MacEwen GD. Fractures of the lateral humeral condyle: role of the cartilage hinge in fracture stability. J Pediatr Orthop. 2002;22:8–11. [PubMed] [Google Scholar]
- e93.Kanellopoulos AD, Yiannakopoulos CK. Closed reduction and percutaneous stabilization of pediatric T-condylar fractures of the humerus. J Pediatr Orthop. 2004;24:13–16. doi: 10.1097/00004694-200401000-00003. [DOI] [PubMed] [Google Scholar]
- e94.Pirker ME, Weinberg A, Hollwarth ME, Haberlik A. Subsequent displacement of initially nondisplaced and minimally displaced fractures of the lateral humeral condyle in children. J Trauma. 2005;58:1202–1207. doi: 10.1097/01.ta.0000169869.08723.c8. [DOI] [PubMed] [Google Scholar]
- e95.Skak SV, Olsen SD, Smaabrekke A. Deformity after fracture of the lateral humeral condyle in children. J Pediatr Orthop B. 2001;10:142–152. [PubMed] [Google Scholar]
- e96.Thomas DP, Howard AW, Cole WG, Hedden DM. Three weeks of Kirschner wire fixation for displaced lateral condylar fractures of the humerus in children. J Pediatr Orthop. 2001;21:565–569. [PubMed] [Google Scholar]
- e97.Dohler JR. Suprakondyläre Korrekturosteotomie beim posttraumatischen Cubitus varus. 3 Fälle bei 2 Patienten. Unfallchirurg. 2002;105:397–400. doi: 10.1007/s00113-001-0368-1. [DOI] [PubMed] [Google Scholar]
- e98.Tien YC, Chen JC, Fu YC, Chih TT, Huang PJ, Wang GJ. Supracondylar dome osteotomy for cubitus valgus deformity associated with a lateral condylar nonunion in children. Surgical technique. J Bone Joint Surg Am. 2006;88(Suppl 1 Pt 2):191–201. doi: 10.2106/JBJS.F.00328. [DOI] [PubMed] [Google Scholar]
- e99.Toh S, Tsubo K, Nishikawa S, Inoue S, Nakamura R, Narita S. -Osteosynthesis for nonunion of the lateral humeral condyle. Clin Orthop Relat Res. 2002;405:230–241. doi: 10.1097/00003086-200212000-00030. [DOI] [PubMed] [Google Scholar]
- e100.von Laer L. Korrektureingriffe am kindlichen Ober- und Unterarm. Unfallchirurg. 2004;107:552–562. doi: 10.1007/s00113-004-0807-x. [DOI] [PubMed] [Google Scholar]
- e101.Mehta JA, Bain GI. Elbow dislocations in adults and children. Clin Sports Med. 2004;23:609–627. doi: 10.1016/j.csm.2004.04.014. [DOI] [PubMed] [Google Scholar]
- e102.El Andaloussi Y, Yousri B, Aboumaarouf M, El Andaloussi M. Medial epicondyle fractures in children. Chir Main. 2006;25:303–308. doi: 10.1016/j.main.2006.11.003. [DOI] [PubMed] [Google Scholar]
- e103.Farsetti P, Potenza V, Caterini R, Ippolito E. Long-term results of treatment of fractures of the medial humeral epicondyle in children. J Bone Joint Surg Am. 2001;83:1299–1305. doi: 10.2106/00004623-200109000-00001. [DOI] [PubMed] [Google Scholar]
- e104.Ngom G, Fall I, Sy MH, Dieme C, Ndoye M. Fractures of the medial humeral epicondyle in child: preliminary study about 18 cases. Dakar Med. 2003;48:199–201. [PubMed] [Google Scholar]
- e105.Gicquel PH, De Billy B, Karger CS, Clavert JM. Olecranon fractures in 26 children with mean follow-up of 59 months. J Pediatr Orthop. 2001;21:141–147. [PubMed] [Google Scholar]
- e106.Malmvik J, Herbertsson P, Josefsson PO, Hasserius R, Besjakov J, Karlsson MK. Fracture of the radial head and neck of Mason types II and III during growth: a 14-25 year follow-up. J Pediatr Orthop B. 2003;12:63–68. doi: 10.1097/01.bpb.0000043568.17315.40. [DOI] [PubMed] [Google Scholar]
- e107.Matuszewski L, Nogalski A, Lübek T. Isolated Fractures of the Head and Neck of the Radial Bone in Children and Adolescents - Types and Methods of Treatment. Osteo Trauma Care. 2006;14:130–134. [Google Scholar]
- e108.Vocke AK, von Laer L. Displaced fractures of the radial neck in children: long-term results and prognosis of conservative treatment. J Pediatr Orthop B. 1998;7:217–222. doi: 10.1097/01202412-199807000-00007. [DOI] [PubMed] [Google Scholar]
- e109.Garcia-Alvarez F, Gil-Albarova J, Bello ML, Bueno AL, Seral F. Results in displaced radial neck fractures in children. Metaizeau technique versus arthrotomy. Chir Organi Mov. 2001;86:211–217. [PubMed] [Google Scholar]
- e110.Waters PM, Stewart SL. Radial neck fracture nonunion in children. J Pediatr Orthop. 2001;21:570–574. [PubMed] [Google Scholar]
- e111.Yarar S, Sommerfeldt D, Gehrmann S, Rueger JM. Stark dislozierte Radiushalsfrakturen nach minimal-invasiver Joystick-Reposition und Prévot-Nagelung. Unfallchirurg. 2007;110:460–466. doi: 10.1007/s00113-006-1181-7. [DOI] [PubMed] [Google Scholar]
- e112.Marzi I, Meenen NM, Dallek M, et al. Suprakondyläre Humerusfraktur beim Kind. AWMF Leitlinie Nr. 012/014, Version 1/2009 [Google Scholar]
- e113.Altay M, Aktekin CN, Ozkurt B, Birinci B, Ozturk AM, Tabak AY. Intramedullary wire fixation for unstable forearm fractures in children. Injury. 2006;37:966–973. doi: 10.1016/j.injury.2006.06.017. [DOI] [PubMed] [Google Scholar]
- e114.Boyer BA, Overton B, Schrader W, Riley P, Fleissner P. Position of immobilization for pediatric forearm fractures. J Pediatr Orthop. 2002;22:185–187. [PubMed] [Google Scholar]
- e115.Fernandez FF, Egenolf M, Carsten C, Holz F, Schneider S, Wentzensen A. Unstable diaphyseal fractures of both bones of the forearm in children: plate fixation versus intramedullary nailing. Injury. 2005;36:1210–1216. doi: 10.1016/j.injury.2005.03.004. [DOI] [PubMed] [Google Scholar]
- e116.Kraus R, Pavlidis T, Szalay G, Meyer C, Schnettler R. Elastisch Stabile Intramedulläre Nagelung (ESIN) von Unterarmschaft-frakturen im Wachstumsalter: Intraoperative Bildwandlerzeiten. Z Orthop Unfallchir. 2007;145:195–198. doi: 10.1055/s-2007-965171. [DOI] [PubMed] [Google Scholar]
- e117.Ogonda L, Wong-Chung J, Wray R, Canavan B. Delayed union and non-union of the ulna following intramedullary nailing in children. J Pediatr Orthop B. 2004;13:330–333. doi: 10.1097/01202412-200409000-00009. [DOI] [PubMed] [Google Scholar]
- e118.Schmittenbecher PP, Fitze G, Gödeke J, Kraus R, Schneidmüller D. Delayed healing of forearm shaft fractures in children following intramedullary nailing. J Pediatr Orthop. 2008;28:303–306. doi: 10.1097/BPO.0b013e3181684cd6. [DOI] [PubMed] [Google Scholar]
- e119.Smith VA, Goodman HJ, Strongwater A, Smith B. Treatment of pediatric both-bone forearm fractures: a comparison of operative techniques. J Pediatr Orthop. 2005;25:309–313. doi: 10.1097/01.bpo.0000153943.45396.22. [DOI] [PubMed] [Google Scholar]
- e120.Calder PR, Achan P, Barry M. Diaphyseal forearm fractures in children treated with intramedullary fixation: outcome of K-wire versus elastic stable intramedullary nail. Injury. 2003;34:278–282. doi: 10.1016/s0020-1383(02)00310-8. [DOI] [PubMed] [Google Scholar]
- e121.Kapoor V, Theruvil B, Edwards SE, Taylor GR, Clarke NM, Uglow MG. Flexible intramedullary nailing of displaced diaphyseal forearm fractures in children. Injury. 2005;36:1221–1225. doi: 10.1016/j.injury.2005.06.033. [DOI] [PubMed] [Google Scholar]
- e122.Qidwai SA. Treatment of diaphyseal forearm fractures in children by intramedullary Kirschner wires. J Trauma. 2001;50:303–307. doi: 10.1097/00005373-200102000-00017. [DOI] [PubMed] [Google Scholar]
- e123.Muensterer OJ, Regauer MP. Closed reduction of forearm -refractures with flexible intramedullary nails in situ. J Bone Joint Surg Am. 2003;85:2152 55. doi: 10.2106/00004623-200311000-00014. [DOI] [PubMed] [Google Scholar]
- e124.Price CT, Knapp DR. Osteotomy for malunited forearm shaft fractures in childrenJ. Pediatr Orthop. 2006;26:193–196. doi: 10.1097/01.bpo.0000194699.29269.76. [DOI] [PubMed] [Google Scholar]
- e125.Schmittenbecher PP. Komplikationen und Fehler bei der Anwendung intramedullarer Stabilisierungsverfahren bei Schaftfrakturen im Kindesalter. Kongressbd Dtsch Ges Chir Kongr. 2001;118:435–437. [PubMed] [Google Scholar]
- e126.Weinberg AM, Pietsch IT, Helm MB, Hesselbach J, Tscherne H. A new kinematic model of pro- and supination of human forearm. J Biomech. 2000;33:487–491. doi: 10.1016/s0021-9290(99)00195-5. [DOI] [PubMed] [Google Scholar]
- e127.Weinberg AM, Kasten P, Castellani C, Jablonski M, Hofmann U, Reilmann H. Which axial Deviation Results in Limitation of Pro- and Supination following Diaphyseal Lower Arm Fracture in Childhood. Eur J Trauma. 2001;27:309–316. [Google Scholar]
- e128.Hankins SM, Bezwada HP, Kozin SH. Corrective osteotomies of the radius and ulna for supination contracture of the pediatric and adolescent forearm secondary to neurologic injury. J Hand Surg Am. 2006;31:118–124. doi: 10.1016/j.jhsa.2005.08.011. [DOI] [PubMed] [Google Scholar]
- e129.Vorlat P, De Boeck H. Bowing fractures of the forearm in children: a long-term follow up. Clin Orthop Relat Res. 2003;413:233–237. doi: 10.1097/01.blo.0000072901.36018.25. [DOI] [PubMed] [Google Scholar]
- e130.Kemnitz S, De Schrijver F, De Smet L. Radial head dislocation with plastic deformation of the ulna in children. A rare and frequently missed condition. Acta Orthop Belg. 2000;66:359–362. [PubMed] [Google Scholar]
- e131.Kuminack KF, Reising KJ, Schmal H, Südkamp NP, Strohm PC. Monteggia Lesions in Children - A clinical Trial. Z Orthop Unfall. 2010;148:54–59. doi: 10.1055/s-0029-1186190. [DOI] [PubMed] [Google Scholar]
- e132.Ruchelsman DE, Klugman JA, Madan SS, Chorney GS. Anterior dislocation of the radial head with fractures of the olecranon and radial neck in a young child: a Monteggia equivalent fracture-dislocation variant. J Orthop Trauma. 2005;19:425–428. doi: 10.1097/01.bot.0000177389.43178.e2. [DOI] [PubMed] [Google Scholar]
- e133.Exner GU. Missed chronic anterior Monteggia lesion. Closed -reduction by gradual lengthening and angulation of the ulna. J Bone Joint Surg Br. 2001;83:547–550. doi: 10.1302/0301-620x.83b4.11103. [DOI] [PubMed] [Google Scholar]
- e134.Hirayama T, Takemitsu Y, Yagihara K, A Mikita. Operation for chronic dislocation of the radial head in children. Reduction by osteotomy of the ulna. J Bone Joint Surg Br. 1987;69:639–642. doi: 10.1302/0301-620X.69B4.3611173. [DOI] [PubMed] [Google Scholar]
- e135.Vocke-Hell AK, von Laer L, Slongo T, Stankovic P. Secondary -radial head dislocation and dysplasia of the lateral condyle after elbow trauma in children. J Pediatr Orthop. 2001;21:319–323. [PubMed] [Google Scholar]
- e136.von Laer LR, Hasler C, Vocke-Hell AK. Late missed Monteggia -lesions - reconstruction of the humeroradial join. Operat Orthop Traumatol. 2003;1:3–19. [Google Scholar]
- e137.Kraus R, Szalay G, Meyer C, Kilian O, Schnettler R. Die Distale Radiusfraktur - eine Torwart-Verletzung bei Kindern und -Jugendlichen. Sportverletz Sportschaden. 2007;21:177–179. doi: 10.1055/s-2007-963706. [DOI] [PubMed] [Google Scholar]
- e138.Kropman RH, Bemelman M, Segers MJ, Hammacher ER. Treatment of impacted greenstick forearm fractures in children using bandage or cast therapy: a prospective randomized trial. J Trauma. 2010;68:425–428. doi: 10.1097/TA.0b013e3181a0e70e. [DOI] [PubMed] [Google Scholar]
- e139.Randsborg PH, Sivertsen EA. Distal radius fractures in children: substantial difference in stability between buckle and greenstick fractures. Acta Orthop. 2009;80:585–589. doi: 10.3109/17453670903316850. [DOI] [PMC free article] [PubMed] [Google Scholar]
- e140.Laurer H, Sander A, Wutzler S, Walcher F, Marzi I. Therapy -principles of distal fractures of the forearm in childhood. Chirurg. 2009;80:1042–1052. doi: 10.1007/s00104-009-1750-8. [DOI] [PubMed] [Google Scholar]
- e141.Miller BS, Taylor B, Widman RF, Bae DS, Snyder BD, Waters PM. Cast immobilization versus percutaneous pin fixation of -displaced distal radius fractures in children: a prospective, -randomized study. J Pediatr Orthop. 2005;25:490–494. doi: 10.1097/01.bpo.0000158780.52849.39. [DOI] [PubMed] [Google Scholar]
- e142.Muratli HH, Yagmurlu MF, Yuksel HY, Aktekin CN, Bicimoglu A, -Tabak AY. Treatment of childhood unstable radius distal metaphysis fractures with closed reduction and percutaneous Kirschner wires. Acta Orthop Traumatol Turc. 2002;36:52–57. [PubMed] [Google Scholar]
- e143.Zimmermann R, Gschwentner M, Kralinger F, Arora R, Gabl M, Pechlaner S. Long-term results following pediatric distal forearm fractures. Arch Orthop Trauma Surg. 2004;124:179–186. doi: 10.1007/s00402-003-0619-4. [DOI] [PubMed] [Google Scholar]
- e144.Webb GR, Galpin RD, Armstrong DG. Comparison of short and long plaster casts for displaced fractures in the distal third of the forearm in children. J Bone Joint Surg Am. 2006;88:9–17. doi: 10.2106/JBJS.E.00131. [DOI] [PubMed] [Google Scholar]
- e145.Meier R, Prommersberger KJ, Lanz U. Die operative Korrektur posttraumatischer Deformitaten am Unterarm nach Frakturen im Wachstumsalter. Z Orthop Ihre Grenzgeb. 2003;141:328–335. doi: 10.1055/s-2003-40086. [DOI] [PubMed] [Google Scholar]