Abstract
Objective
A comprehensive case-control study was conducted to determine potential risk factors for medulloblastoma/primitive neuroectodermal tumor (PNET), a common brain tumor in children. This analysis evaluated possible associations between previous head injury and ionizing radiation exposure through diagnostic x-rays and medulloblastoma/PNET.
Methods
Mothers of 318 cases < 6 years of age at diagnosis between 1991 and 1997 and registered with the Children’s Oncology Group were interviewed. Mothers of 318 matching controls were selected through random digit dialing and interviewed.
Results
An association was not detected between previous head injury (OR: 0.78, 95% CI: 0.40–1.5) or head x-ray for any reason including head injury with medulloblastoma/PNET. A statistically non-significant excess of cases reported having an x-ray for reason other than head injury (OR 2.3, 95%CI 0.91–5.7). When cases that received an x-ray for a common symptom of medulloblastoma/PNET were considered unexposed this association weakened (OR: 1.3, 95% CI: 0.49–3.7). No dose-response relationship was observed.
Conclusions
Head injury and exposure to diagnostic head x-rays were not associated with medulloblastoma/PNET in this study. Future studies should investigate all imaging procedures with ionizing radiation exposure including computed tomography (CT) scans and utilize radiation dose estimations.
Keywords: Brain neoplasms, Radiography, Craniocerebral trauma
Introduction
Tumors of the brain and central nervous system are the second most common type of cancer among children [1]. Medulloblastoma and primitive neuroectodermal tumor (PNET) are histologically similar but genetically distinct brain tumors that occur primarily in children [2, 3] and together account for about 20% of brain tumors in children [4]. Medulloblastoma accounts for about 80% of the tumors in the combined medulloblastoma/PNET grouping [3].
The only known risk factors for brain tumors in children are some genetic conditions and exposure to therapeutic doses of ionizing radiation [3, 5, 6]. Although diagnostic x-rays confer much lower doses of ionizing radiation, children may be more susceptible to the effects than adults. The harmful effects of fetal x-ray exposure have been established since the 1950s [7, 8]. However, the evidence regarding x-rays and brain tumors in young children after birth is not consistent [9–13].
Studies examining the effect of head injury on brain tumor occurrence are conflicting [12, 14–17]. Generally, studies in children show that head injuries that occur during birth or those that are severe enough to result in hospitalization or the loss of consciousness are associated with higher brain tumor risk [11, 13, 18].
We report here our results on head injury and diagnostic x-ray exposure from a case-control study of medulloblastoma/PNET in young children.
Materials and Methods
Institutional review boards (IRBs) of all participating institutions approved the study and all participants gave informed consent. The study design and methods for subject selection have been described in detail elsewhere [19]. Briefly, to be eligible as a case, an individual had to be diagnosed with medulloblastoma/PNET before the age of six years between July 1991 and November 1997 [9]. Member institutions of the Children’s Oncology Group (COG) that were previously affiliated with the Children’s Cancer Group (CCG) identified 558 potentially eligible cases that met these criteria. From these 558, cases were excluded for the following reasons: physician did not give consent to contact family (n=35), not PNET on pathology review (n=28), biologic mother not available (n=17), language barrier (n=16), no phone in household (n=13), residence outside North America (n=6), prior or concurrent cancer (n=3), and no response from institution (n=2). In addition, the IRBs of many participating institutions required that parents give their consent to participate before they were invited by the principal investigator. The participating institutions could not locate seven families to obtain their consent, and an additional 39 families either did not respond to the consent letter or actively refused to participate. When the investigators attempted to contact the case mothers, 41 could not be located and 27 refused. Controls could not be found for 6 cases. A total of 318 case mothers comprise the study population (68% of all cases; 73% of eligible cases).
Controls were selected by random digit dialing (RDD). They were matched to the cases on area code, race, and date of birth (± 6 months for cases diagnosed prior to one year of age, ± 1 year for all other cases) The response rate was 67% for the RDD screening and 73% for the study interview. In total, 318 controls participated [9].
Every child was assigned a reference age after which exposures were deemed not to have contributed to tumor formation. As the critical period of exposure for development of these tumors is not known, reference ages were assigned based on researchers’ assumptions about the critical period and were, by necessity, arbitrary. Reference ages were assigned by age at diagnosis as follows: birth if diagnosis at 0 to 5 months, 3 months if diagnosis at 6 to 11 months, 6 months if diagnosis at 12 to 17 months, 9 months if diagnosis at 18 to 23 months, age at diagnosis minus 12 months if diagnosis at 24 months or older. Each matched control was assigned the same reference age as the case. Nineteen case-control pairs with reference age at birth were excluded from the current analysis of postnatal factors. As a result the final sample utilized in this study consisted of 299 cases and 299 controls.
Data Collection Methods and Procedures
Trained interviewers conducted structured telephone interviews with the mothers of cases and controls. All data for this study came from maternal interviews; no medical records were reviewed. Interviews of case mothers took place a median of 1.6 years after the child’s diagnosis (range 0.1 to 6.2 years).
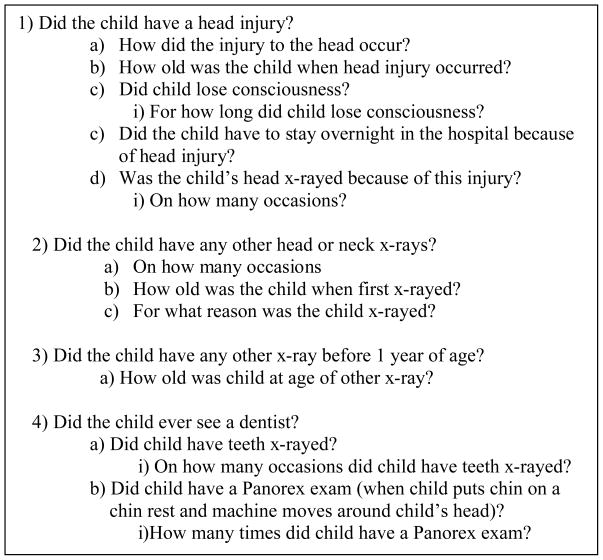
The interview included questions about head injury including how it happened, age, loss of consciousness, hospitalization, and related x-rays (Figure 1). Questions about loss of consciousness and hospitalization were included in order to judge severity. Mothers were asked about dental visits and associated x-rays, other head and neck x-rays, and any x-rays before one year of age. X-rays that occurred before one year of age were considered to have exposed the head because of the small size of the child.
Figure 1.
Interview Questions from Maternal Survey
The interview also included questions on demographic factors that might be confounders or indicators of possible selection bias. For example, more residential moves for cases compared to controls could result in a reduced ability to locate the cases and thus a sample potentially biased by the exclusion of residentially mobile cases.
Statistical Analysis
Odds ratios (ORs) and 95% confidence intervals were determined for associations between the exposures of interest and medulloblastoma/PNET. The exposures analyzed for the time period from birth until the reference age were 1) head injury, 2) head x-ray related to a head injury, 3) head x-ray not related to a head injury, 4) head x-ray regardless of reason, 5) number of head x-rays, 7) dental x-ray (standard or Panorex), 8) x-ray of any part of the body other than the head before age one, and 9) any x-ray in categories 1 – 8. Although we intended to consider head injuries resulting in loss of consciousness and those requiring hospitalization, the small number of such injuries (3 and 4, respectively) precluded analysis.
Subjects who had a head x-ray not related to a head injury were asked the reason for the x-ray in order to ascertain whether the x-ray was for a common symptom of medulloblastoma/PNET. We performed alternate analyses where subjects who had x-rays for common symptoms of medulloblastoma/PNET were not considered exposed. The symptoms included head tilt, balance disorder, large head size, and hydrocephalus.
The associations between variables and medulloblastoma/PNET were estimated by conditional logistic regression. We adjusted for annual household income (< $50,000 vs. ≥ $50,000), education (less than high school, high school, some post high school, college/grad/professional), and age of child at interview. Subjects with missing data for income were included in the less than $50,000 category as these subjects were similar demographically to those in this income category. Using the income category midpoint as a continuous variable or considering missing values as a distinct income category did not change the results appreciably. Inclusion of mother’s marital status, number of moves, and date of interview did not appreciably change the OR estimates and these factors were therefore not included in the final models.
All analysis was done using SPSS version 15.0.
Results
Case and control mothers were similar on most demographic categories including race, education, marital status, number of moves, and geographic location (Table 1). Income was not statistically different between cases and controls, but cases were somewhat more likely to have an annual household income over $50,000. Age of child at interview and date of interview in months since start of study were statistically significantly higher in controls as control identification did not begin until the case was interviewed. The mean reference age for both cases and controls was 1.7 years.
Table 1.
Demographic and other characteristics of cases and controls
| Characteristic | Case Number (N = 299) | Percent | Control Number (N=299) | Percent |
|---|---|---|---|---|
| Mother’s Race | ||||
| White, Non-Hispanic | 245 | 82 | 252 | 84 |
| Other | 54 | 18 | 47 | 16 |
| Mother’s Education | ||||
| Less than high school | 26 | 9 | 36 | 12 |
| High School | 86 | 29 | 78 | 26 |
| Some post high school | 94 | 31 | 103 | 34 |
| College/Grad/Professional | 93 | 31 | 82 | 27 |
| Mother’s Marital Status | ||||
| Married | 249 | 83 | 242 | 81 |
| Other | 50 | 17 | 57 | 19 |
| Mother’s IncomeA | ||||
| Less than $15,000 | 41 | 15 | 47 | 17 |
| $15,00 –$24,999 | 47 | 17 | 53 | 20 |
| $25,000–$34,999 | 52 | 18 | 52 | 19 |
| $35,000–$49,999 | 63 | 22 | 59 | 22 |
| $50,000–$74,999 | 51 | 18 | 36 | 13 |
| ≥$75,000 | 28 | 10 | 24 | 9 |
| Times family moved between start of pregnancy and reference date | ||||
| 0 | 141 | 47 | 131 | 44 |
| 1 | 78 | 26 | 78 | 26 |
| 2 | 40 | 13 | 39 | 13 |
| 3 | 26 | 9 | 27 | 9 |
| 4 + | 14 | 5 | 24 | 8 |
| Mean (SD) | Mean (SD) | |||
| Age (Years) of Child at Interview | 5.1 (2.0) | 5.7 (2.2) | ||
| Date interviewed in months since start of study | 15.8 (10.7) | 23.3 (9.1) | ||
N=288 for cases and N=271 for control
Head injury and head x-rays due to head injury were not statistically associated with medulloblastoma/PNET (Table 2).
Table 2.
Odds ratios for head injury and x-rays with exposure to the head from a case-control study of medulloblastoma/PNET with 299 case-control pairs A
| Risk Factor | Number Cases Exposed/Controls Exposed | ORB | 95% CI | p-value |
|---|---|---|---|---|
| Head Injury | 33/36 | 0.78 | 0.40–1.5 | 0.47 |
| Head X-ray due to head injury | 8/10 | 0.62 | 0.21–1.9 | 0.40 |
| Head X-ray not due to head injury | 24/12 | 2.3 | 0.91–5.7 | 0.08 |
| 1 x- ray | 17/9 | 2.5 | 0.83–7.5 | 0.11 |
| 2 or more x- rays | 6/3 | 1.7 | 0.31–9.2 | 0.55 |
| Head X-ray not due to head injuryC | 15/12 | 1.3 | 0.49–3.7 | 0.57 |
| 1 x- ray | 13/9 | 1.9 | 0.56–6.1 | 0.31 |
| 2 or more x- rays | 2/3 | 0.50 | 0.06–3.9 | 0.51 |
| Head X-ray any Reason | 32/20 | 1.7 | 0.82–3.4 | 0.16 |
| Head X-ray any ReasonC | 23/20 | 1.2 | 0.54–2.5 | 0.69 |
| Any X-ray before age 1 | 35/23 | 1.3 | 0.68–2.61 | 0.40 |
| Dental X-ray | 16/18 | 0.85 | 0.37–1.9 | 0.70 |
| Any type of X- ray D | 75/55 | 1.4 | 0.83–2.3 | 0.22 |
| Any type of X- ray C D | 69/55 | 1.2 | 0.71–2.0 | 0.51 |
The number of matched case control sets ranged from 294-299 due to missing data
Adjusted for annual household income > $50,000, mother’s education (less than high school, high school, some post high school, and college/grad/professional), and age of child at interview
Subjects were considered “unexposed” if the reason for x-ray was possibly tumor related
Includes head x-ray for any reason, other x-ray before 1, and dental x-ray
More cases than controls reported having had a head x-ray not related to head injury with results approaching statistical significance (OR 2.3, 95%CI 0.91–5.7). Nine cases had head x-rays for head tilt, balance disorder, large head size, or hydrocephalus, all of which are presenting symptoms of medulloblastoma/PNET. When these 9 cases were not considered as exposed or were excluded from the analysis, the association between medulloblastoma and PNET was reduced substantially (OR:1.3, 95% CI: 0.49–3.7). Few subjects had had more than one head x-ray and there was no evidence of a dose-response relationship.
The OR for any head x-ray was increased but not statistically significant (OR: 1.7, 95% CI: 0.68–2.61) Once again, no association was present when subjects with x-rays for possible presenting symptoms were not considered exposed.
The OR for other (not of the head) x-ray before age one was slightly increased but not statistically significant (OR 1.3, 95%CI: 0.68–2.6). No association was observed between medulloblastoma/PNET and dental x-ray.
The OR for any x-ray was not statistically significant (OR: 1.4, 95%CI: 0.83–2.3). There was no suggestion of a statistically significant association when the cases whose only head x-ray was for a possible tumor symptom were considered unexposed. For this analysis, 3 of the 9 cases that had symptom-related x-rays remained exposed because they had had other x-rays.
Discussion
We did not detect a relationship between medulloblastoma/PNET and head injury, replicating the finding of a previous CCG study [17]. By contrast, many other studies that investigated brain tumors in children have reported an association with head injury [4, 13, 18]. However, these studies only observed an association when the head injury required hospitalization, resulted in a loss of consciousness, or occurred during birth. We might have failed to detect an association with severe head injuries because of low power as only 4 subjects required hospitalization or lost consciousness. Another possibility is that head injury is a risk factor only for brain tumor types other than medulloblastoma/PNET.
There was a statistically non-significant excess of cases reporting a head x-ray not related to head injury. Once again this replicates the finding of the previous CCG study that also found a statistically non-significant excess of cases reporting an x-ray [17]. Other studies have reported a statistically non-significant relationship between childhood central nervous system tumors and diagnostic x-ray [10], including a cohort study based on medical records in which increasing doses were not associated with increased cancer incidence [19].
Interestingly, Howe et al., who reported an association between childhood brain tumor and skull x-ray, indicated that these x-rays might have been the result of early case symptoms [18]. A strength of our study was the ability to investigate this concern. Nine of the 32 exposed cases had x-rays for reasons that are common symptoms of medulloblastoma and PNET. For most of the nine cases, the head x-ray occurred slightly more than a year before the medulloblastoma/PNET diagnosis, with a range of 3 to 29 months. The average duration of symptoms prior to medulloblastoma diagnosis is 8 weeks for males and 5 weeks for females [20]. Clearly the average symptom duration is much shorter than the time between x-ray and diagnosis of these 9 cases. However the time interval between diagnosis and symptom occurrence can be up to 100 weeks [20]. As a result, it is difficult to definitively determine whether the symptoms were the result of the brain tumor in these 9 cases.
We also did not detect an association between dental x-rays and medulloblastoma/PNET. Research regarding previous dental x-rays is limited. However, five or more full mouth series x-rays have been associated with increased brain tumor risk in adolescents and young adults [12,13]. In our study, the exposure to ionizing radiation was much lower, as a single dental x-ray was considered exposure. The difference in exposure level could explain the difference in the results observed as could low power in our study due to small numbers of exposed children in this age group. In this study we did not ask about full mouth series x-rays, and only 7 individuals had a Panorex exam.
A potential limitation of this study is a limited ability detect an association. Although we did not observe an association between the exposures studied and medulloblastoma/PNET, the confidence intervals for effect estimates were very wide. Despite a fairly large overall sample size, the exposures studied are fairly rare and it is possible that the sample size was not large enough to detect statistically significant associations.
A key feature of this study is its reliance on maternal recall of head injury and x-rays. Case mothers may have devoted more thought to past exposures as a result of their child’s illness and might remember more x-rays than control mothers, suggesting the possibility of a bias away from the null. However, as few ORs in this study were substantially increased, this possible recall bias is not a major concern. However, there is certainly some degree of inaccuracy in the recall of exposures that occurred several years ago.
There is also the potential for selection bias. The use of RDD may result in a population that is not representative of the general population because households choosing to respond to the RDD screening and study interview may have differed from those who refused. For example, those who refused may have been of higher or lower SES, and SES may be related to access to health care and likelihood of x-ray exposure. In this scenario, the OR for x-ray exposure would be biased either toward or away from the null. However, we cannot assess the likelihood or direction of this bias since no information is available on RDD non-responders. Reliance on a non-population-based case group ascertained through COG could have also resulted in selection bias as the cases may not have been representative of the larger population of cases in terms of x-ray history.
Medical records could provide more accurate information than parental report on head injury and x-rays. However, accessing medical records for a study population spread across the US and Canada in numerous health systems would not be feasible. An improved approach would be a cohort study of exposed children such as the one the National Cancer Institute is currently implementing in the United Kingdom. A large cohort of individuals who received computed tomography (CT) scans as children or adolescents will be followed for cancer incidence and mortality using national medical records [21].
Although cohort studies conducted through medical records are close to ideal, these studies will rarely be feasible because of the very large numbers required for a rare disease such as childhood brain tumors. Therefore, there may still be a role for case-control interview studies with carefully designed questionnaires. Our findings suggest several ways to enhance the recall and accuracy of responses in future studies. In the current format, there was likely some misclassification of head injuries. When mothers were asked the reason for the head x-ray not due to head injury, the reasons given included, “bumped his head”, “accident”, “walked into door”, and “tripped and hit head”. We would have expected these to be reported as related to a head injury. A possible explanation could be that the child was x-rayed for a suspected head injury and found not to have one. To accommodate this possibility, we recommend asking whether the child ever had a head injury or was ever suspected of having a head injury and whether the child had x-rays for this purpose.
Questions regarding x-rays could also be improved in several key ways. We recommend that questionnaires ask about CT scans specifically. In the questionnaire used here, mothers may or may not have reported CT scans when asked about x-rays. In the U.S. CT scans are standard protocol for head injuries and the number of pediatric CT examinations has increased 200% in the recent years [22]. The effective dose of radiation from a head CT (2 mSV) is almost 150 times greater than that received from a skull x-ray (0.015 mSV) [23]. Other imaging procedures that expose the child’s brain should also be included in the questionnaire. Lack of information on CT scans and other procedures could obscure an association between ionizing radiation exposure of the brain and medulloblastoma/PNET.
To further enhance responses, researchers could apply an approach used to improve recall of medication use [24]. Research regarding recall of pharmacological treatments has shown that it is more effective to ask indication-oriented questions than open-ended questions alone [25]. To apply that principle to imaging procedures, one could ask about common indications such as suspected head injury, abnormal head or neck development, or possible brain infection in addition to asking about the imaging procedures themselves. When a mother reports an x-ray for an indication that can be a presenting symptom of a brain tumor, we recommend directly asking the mother if this was a symptom of the brain tumor. This would allow a more accurate assessment of whether the x-ray was related to the diagnosis of the tumor.
The analysis of detailed data collected on x-rays and CT scans could be improved by accounting, at least crudely, for radiation dose. A radiation physicist or other expert could estimate the typical dose for a given procedure based on the typical views, typical number of films taken, size of child, and other factors. Although these would be crude estimates, they would provide a basis for separating procedures with high levels of exposure from those with low-level exposure.
In conclusion, we detected no relationship between head injury and medulloblastoma/PNET and no conclusive evidence of an association between x-ray and medulloblastoma/PNET. More research is needed regarding the critical exposure period for tumor formation. We recommend that future studies utilize an enhanced questionnaire and dose estimation. Possible associations between CT scans as well as other sources of ionizing radiation exposure and medulloblastoma/PNET need to be investigated.
Acknowledgments
Financial Support: This work was supported in part by grants CA60951 and CA98543 (COG Chair’s Grant) from the National Cancer Institute at the National Institutes of Health (United States) and CureSearch NCCF.
We thank the project managers and interviewers (Kathy Walsh, Anne Goldblatt, the late Jean Rodwell, Mary Rewinski, Christine Plourde, and Sallie McLaughlin) for their hard work and dedication during the data collection phase of the study.
Footnotes
Conflicts of Interest: The authors of this paper have no conflicts of interest to disclose.
Contributor Information
Saira Khan, Department of Epidemiology and Biostatistics, Drexel University School of Public Health, Philadelphia, PA, USA, General Pediatrics, Children’s Hospital of Philadelphia, Philadelphia, PA, USA.
Alison A. Evans, Department of Epidemiology and Biostatistics, Drexel University School of Public Health, Philadelphia, PA, USA.
Lucy Rorke-Adams, Departments of Pathology, Neurology, and Pediatrics, University of Pennsylvania School of Medicine, Philadelphia, PA, USA, Departments of Pathology and Neurology, Children’s Hospital of Philadelphia, Philadelphia, PA, USA.
Manuela A Orjuela, Departments of Pediatrics and Environmental Health Sciences, Columbia University, New York, NY, USA.
Tania Shiminski-Maher, Pediatric Nurse Practitioner, Neurosurgery, The Children’s Hospital at Montefiore, New York, NY, USA.
Greta R. Bunin, Division of Oncology, Center for Childhood Cancer Research, Children’s Hospital of Philadelphia, Philadelphia, PA, USA, Department of Pediatrics, University of Pennsylvania School of Medicine, Philadelphia, PA, USA
References
- 1.U.S. Cancer Statistics Working Group. United States Cancer Statistics: 2002 Incidence and Mortality. Atlanta, GA: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Cancer Institute; 2005. [Google Scholar]
- 2.Pomeroy SL, Tamayo P, Gaasenbeek M, et al. Prediction of central nervous system embryonal tumour outcome based on gene expression. Nature. 2002;415:436–462. doi: 10.1038/415436a. [DOI] [PubMed] [Google Scholar]
- 3.Surveillance, Epidemiology, and End Results (SEER) Program. Public-use data (1973– 2001) Bethesda, MD: Cancer Statistics Branch, Surveillance Research Program, Division of Cancer Control and Population Sciences, National Cancer Institute; 2004. [Google Scholar]
- 4.Gurney JG, Smith MA, Bunin GR. CNS and miscellaneous intracranial and intraspinal neoplasms. In: Ries LAG, Smith MA, Gurney JG, Linet M, Tamra T, Young JL, Bunin GR, editors. Cancer Incidence and Survival among Children and Adolescents: United States SEER Program 1975–1995. Bethesda, MD: National Cancer Institute, SEER Program; 1999. pp. 51–63. [Google Scholar]
- 5.Ron E, Modan B, Boice JD, et al. Tumors of the brain and Central Nervous System after radiotherapy in childhood. N Engl J Med. 1988;319:1033–1039. doi: 10.1056/NEJM198810203191601. [DOI] [PubMed] [Google Scholar]
- 6.National Institute of Environmental Health Sciences. Report on Carcinogens. 11. U.S. Department of Health and Human Services, Public Health Service, National Toxicology Program; 2004. [Google Scholar]
- 7.Stewart A, Webb J, Hewitt D. A survey of childhood malignancies. Br Med J. 1958;1:1495– 1508. doi: 10.1136/bmj.1.5086.1495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Harvey EB, Boice JD, Honeyman M, Flannery JT. Prenatal x-ray exposure and childhood cancer in twins. N Engl J Med. 1985;312:541–545. doi: 10.1056/NEJM198502283120903. [DOI] [PubMed] [Google Scholar]
- 9.Bunin GR, Robison LL, Biegel JA, Pollack IF, Rorke-Adams LB. Parental heat exposure and risk of childhood brain tumor: a Children’s Oncology Group Study. Am J Epidemiol. 2006;164:222–231. doi: 10.1093/aje/kwj174. [DOI] [PubMed] [Google Scholar]
- 10.Schuz J, Kaletsch U, Kaatsch P, Meinert R, Michaelis J. Risk factors for pediatric tumors of the central nervous system: Results from a German population-bases case-control study. Med Pediatr Oncol. 2000;36:274–282. doi: 10.1002/1096-911X(20010201)36:2<274::AID-MPO1065>3.0.CO;2-D. [DOI] [PubMed] [Google Scholar]
- 11.Gurney JG, Preston-Martin S, McDaniel AM, Mueller BA, Holly EA. Head injury as a risk factor for brain tumors in children: results from a multicenter case-control study. Epidemiology. 1996;7:485–489. [PubMed] [Google Scholar]
- 12.Preston-Martin S, Mack W, Henderson BE. Risk factors for gliomas and meningiomas in males in Los Angeles County. Cancer Res. 1989;49:6137–6143. [PubMed] [Google Scholar]
- 13.Preston-Martin S, Yu MC, Benton B, Henderson BE. N-nitroso compounds and childhood brain tumors: a case-control study. Cancer Res. 1982;42:5240–5245. [PubMed] [Google Scholar]
- 14.Inskip PD, Mellemkjaer L, Gridley G, Olsen JH. Incidence of intracranial tumors following hospitalization for head injuries (Denmark) Cancer Causes Control. 2004;9:109–116. doi: 10.1023/a:1008861722901. [DOI] [PubMed] [Google Scholar]
- 15.Preston-Martin S, Pogoda JM, Schlehofer B, et al. An international case-control study of adult glioma and meningioma: the role of head trauma. Int J epidemiol. 1998;27:579–586. doi: 10.1093/ije/27.4.579. [DOI] [PubMed] [Google Scholar]
- 16.Nyrgen C, Adami J, Weimin Y, et al. Primary brain tumors following traumatic brain injury: a population-based cohort study in Sweden. Cancer Causes Control. 2001;12:733–737. doi: 10.1023/a:1011227617256. [DOI] [PubMed] [Google Scholar]
- 17.Bunin GR, Buckley JD, Boesel CP, Rorke LB, Meadows AT. Risk factors for Astrocytic Glima and Primitive Neuroectodermal Tumor of the brain in young children: a report from the Children’s Cancer Group. Caner Epidemiol Biomarkers Prev. 1994;3:197–204. [PubMed] [Google Scholar]
- 18.Howe GR, Burch JD, Chiarelli AM, Risch A, Choi BCK. An exploratory case- control study of brain tumors in children. Cancer Res. 1989;49:4349–4352. [PubMed] [Google Scholar]
- 19.Hammer GP, Seidenbusch MC, Schneider K, et al. A cohort study of childhood incidence after postnatal diagnostic x-ray exposure. Radiat Res. 2009;171:504–512. doi: 10.1667/RR1575.1. [DOI] [PubMed] [Google Scholar]
- 20.Halperin EC, Watson DM, George SL. Duration of symptoms prior to diagnosis is related to inversely presenting disease stage in children with medulloblastoma. Cancer. 2001;91:1444–1450. doi: 10.1002/1097-0142(20010415)91:8<1444::aid-cncr1151>3.0.co;2-u. [DOI] [PubMed] [Google Scholar]
- 21.National Cancer Institute. [Accessed on 13 October 2009];Pediatric CT Scans. 2009 Available at: http://dceg.cancer.gov/reb/research/ionizing/medical/4.
- 22.Linton OW, Mettler FA. National Conference on Dose Reduction in CT, with an Emphasis on Pediatric Patients. Am J Roentgenol. 2003;181:321–329. doi: 10.2214/ajr.181.2.1810321. [DOI] [PubMed] [Google Scholar]
- 23.Linet MS, Kim KP, Rajaraman P. Children’s exposure to diagnostic medical radiation and cancer risk: epidemiologic and dosimetric considerations. Pediatric Radiol. 2009;39:S4–S26. doi: 10.1007/s00247-008-1026-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.West SL, Strom BL, Poole C. Validity of pharmacoepidemiologic drug and diagnosis data. In: Strom BL, editor. Pharmacoepidemiology. 4. Chichester: John Wiley & Sons, Ltd; 2005. pp. 709–65. [Google Scholar]
- 25.Gama H, Correia S, Lunet N. Questionnaire design and the recall of pharmacological treatments: a systematic review. Pharmacoepidemiol Drug Saf. 2009;18:175–187. doi: 10.1002/pds.1703. [DOI] [PubMed] [Google Scholar]