Abstract
Objective
To evaluate the effectiveness of Tai Chi in the treatment of knee osteoarthritis (OA) symptoms.
Methods
We conducted a prospective, single-blind, randomized controlled trial of 40 individuals with symptomatic tibiofemoral OA. Patients were randomly assigned to 60 minutes of Tai Chi (10 modified forms from classical Yang style) or Attention Control (wellness education and stretching) twice-weekly for 12 weeks. The primary outcome was the Western Ontario and McMaster Universities OA (WOMAC) pain score at 12 weeks. Secondary outcomes included WOMAC function, patient and physician global assessments, timed chair stand, depression index, self-efficacy scale, and quality of life. We repeated these assessments at 24 and 48 weeks. Analyses were compared by intention-to-treat principles.
Results
The 40 patients had mean age 65 years and BMI 30.0 kg/m2. Compared to the controls, patients assigned to Tai Chi exhibited significantly greater improvement in WOMAC pain (mean difference at 12 weeks = −118.80 mm; 95% confidence interval [−183.66 to −53.94]; P= 0.0005), WOMAC physical function, −324.60 mm (CI, −513.98 to −135.22; P= 0.001), patients global VAS, −2.15 cm (CI, −3.82 to −0.49; P= 0.01), physician global VAS, −1.71 cm (CI, −2.75 to −0.66; P=0.002), chair stand time, −10.88 sec. (CI, −15.91 to −5.84; P= 0.00005), CES-Depression index, −6.70 (CI, −11.63 to −1.77; P= 0.009), self-efficacy score, 0.71 (CI, 0.03 to 1.39; P= 0.04) and SF-36 physical component summary, 7.43 (CI, 2.50 to 12.36; P=0.004). No severe adverse events were observed.
Conclusion
Tai Chi reduces pain and improves physical function, self-efficacy, depression and health-related quality of life for knee OA.
INTRODUCTION
Knee osteoarthritis (OA) is an increasing problem in the elderly population resulting in pain, functional limitation, disability, reduced quality of life and substantial health care costs (1–3). The pathophysiological basis of knee OA is multifaceted and includes degeneration of articular structures, impaired muscle function, and psychological traits of chronic pain (4–6). No feasible preventive intervention strategies or effective disease-modifying remedies currently exist for knee OA. Recommended core treatments include physical therapy such as aerobic and muscle strengthening exercise (2, 3, 7), but these have modest benefits for pain and physical function and may not affect psychological outcomes (8).
Tai Chi is a traditional Chinese mind-body exercise that enhances balance, strength, flexibility and self-efficacy, and reduces pain, depression and anxiety in diverse patient populations with chronic conditions (9). As a complementary mind-body approach, Tai Chi may be an especially applicable treatment for older adults with knee OA. The physical component provides exercise consistent with current recommendations for OA (range of motion, flexibility, muscle conditioning and aerobic cardiovascular exercise) (10); the mental component could address the chronic pain state through effects on psychological well-being, life satisfaction, and perceptions of health (11).
Although Tai Chi has spread worldwide over the past 2 decades, scientific evidence to support its efficacy for knee OA has been inconclusive (12). Some benefits were shown in one large-scale randomized, controlled trial (RCT), but interpretation of its results was limited by methodological issues including enrollment of individuals with hip as well as knee OA, absence of radiographic confirmation, short follow-up and poor adherence (13).
A well-designed study may overcome the previous limitations, and we therefore conducted a 12-week RCT with 1-year follow-up to test the effects of Tai Chi on pain (a marker of disease activity), functional independence (a marker of impairment), and health-related quality of life in elderly people with knee OA. We hypothesized that participants receiving Tai Chi would show greater improvement in knee pain, physical and psychological functioning, and health status than participants treated with an Attention Control intervention consisting of wellness education and stretching, and that the benefits would be mediated by effects on muscle function, musculoskeletal flexibility and mental health.
PATIENTS AND METHODS
Setting and Participants
The study was conducted at Tufts Medical Center, an urban tertiary care academic hospital in Boston, USA. It received ethics approval from the Tufts Medical Center/ Tufts University Human Institutional Review Board. A detailed version of the study protocol was reported in 2008 (14).
Patients with knee OA were recruited from the greater Boston area. To ensure adequate enrollment of underrepresented groups, we placed advertisements in local media. We also used the rheumatology clinic patient database at Tufts Medical Center to identify patients with knee OA. For interested respondents, we determined eligibility through a brief, scripted interview which posed questions whose predictive values for knee OA were known from population-based data. Applicants who screened positive on the telephone interview were scheduled for eligibility visits, when written informed consent was obtained.
The eligibility criteria were: age ≥ 55 years; Body Mass Index (BMI) ≤ 40 kg/m2; WOMAC pain subscale score (visual analog version) > 40 (range 0–500); fulfillment of the American College of Rheumatology criteria for knee OA (15) with radiographic Kellgren and Lawrence (K/L) knee OA grade ≥ 2 (16). We excluded individuals who had prior Tai Chi training or similar types of alternative medicine like Qi Gong or yoga; individuals with serious medical conditions, limiting their ability for full participation as determined by primary care physicians; individuals with intra-articular steroid injections in the previous three months, or reconstructive surgery on the affected knee and any intra-articular hyaluronate injections in the previous six months; individuals unable to pass the Mini-Mental examination (score < 24) (17).
To avoid bias in favor of the Tai Chi intervention, we informed participants that we were studying the effects of two different types of exercise training programs, one of which was combined with nutrition education. Participants were allowed to continue routine medications and maintain their usual visits with their primary care physicians or rheumatologists throughout the study.
Randomization
Participants were randomly assigned to Tai Chi (n=20) or an Attention Control group (n=20). Randomization assignments were designated by the statistician (CS), using computer-generated numbers to randomize permuted blocks of size 2 and 4 so that each block was complete. They were provided in sealed, opaque envelopes and opened upon the participant’s agreement to participate. The block size was randomly assigned to minimize correct prediction of assignments, while preserving approximate balance between groups. Outcomes that required analysis of knee strength were based on evaluation of the knee reported as most painful at baseline. If both knees were equally affected (which occurred in 2 participants), one knee was chosen at random as the affected knee.
The Tai Chi Intervention
Subjects participated in 60-minute Tai Chi sessions twice weekly for 12 weeks instructed by a Tai Chi master (R Rones) with more than 20 years of teaching experience. In the first session, we explained Tai Chi theory and procedures and provided the patients with printed teaching materials including a well-tested, validated IRB-approved Tai Chi program that described Tai Chi principles, practicing techniques, and safety precautions for knee OA (18). For the remaining sessions, each subject practiced Tai Chi under the instruction of the Tai Chi master. Every session included: (1) 10 minute self-massage and a review of Tai Chi principles; (2) 30 minutes of Tai Chi movement; (3) 10 minutes of breathing technique; (4) 10 minutes of relaxation. The program consisted of 10 forms from classical Yang Style Tai Chi (20) with minor modifications that were suitable for people with knee pain. This involved eliminating stances that require greater than 90° knee-flexion and can cause excess knee joint stress (21). We also provided a Tai Chi DVD published by R Rones. Patients were instructed to practice Tai Chi at least 20 minutes a day at home and encouraged to maintain their usual physical activities, but not to participate in additional new strength training or exercise programs other than Tai Chi. After completing the 24 treatment sessions, we instructed subjects to continue practicing Tai Chi at home following the DVD and handouts until the 48 week follow-up visit.
The Attention Control Intervention
The wellness education and stretching program provided an active control for the attention being paid to the Tai Chi group (19, 22). The control group attended two 60-minute class sessions per week for 12 weeks. In the first session, research staff explained the program and procedures. A variety of health professionals provided nutrition and medical information in the following sessions. Every session included 40 minutes of didactic lessons on: (1) OA as a disease; (2) diet and nutrition; (3) therapies to treat OA; or (4) physical and mental health education (e.g., recognizing and dealing with stress). The nutrition education was based on “Dietary Guidelines for Americans” (23) and focused on general knowledge of nutrition, cooking and shopping but not on specific nutrients and supplements. The final 20 minutes consisted of stretching exercises involving the upper body, trunk and lower body, each stretch being held for 10 to 15 seconds. Participants were instructed to practice at least 20 minutes of stretching exercises per day at home. They were encouraged to maintain their usual physical activities, but not to participate in additional strength and mind-body exercise programs other than their stretching exercise. The stretching and health information was compiled using materials from our previous program (18) and the website of the National Institute of Arthritis and Musculoskeletal and Skin Diseases at NIH (24).
Throughout the 12-week period, we tracked the reasons for missed sessions and the number of missed sessions and asked subjects to complete daily logs indicating the amount of time they practiced Tai Chi or stretching exercise.
Outcome Measures and Follow Up
Our knee OA outcome measurements were drawn from the core set recommended by the Osteoarthritis Research Society International (25), and focused on pain, physical function and patients’ overall assessment of their knee OA severity. The primary outcome measure was change in the WOMAC pain subscale between baseline and 12 weeks. The WOMAC is a validated, self-administered instrument specifically designed to evaluate knee and hip OA (26, 27). It has three subscales that we analyzed separately: pain (score range, 0–500), stiffness (0–200), and function (0–1700), with higher scores indicating more severe disease. Secondary outcomes included weekly WOMAC pain scores during the 0–12 week intervention and assessments of WOMAC function, WOMAC stiffness, and global knee pain status assessed separately by the participant and a study physician (RK) who was blinded to group assignment (VAS score range, 0–10; 0 equals no pain) (28). We evaluated physical performance using the timed chair stand (measured in seconds) (29), 6 minute walk test (measured in yards) (30) and standing balance (score range, 0–5; 0 equals worst balance) (31). Additional measures included the Center for Epidemiology Studies Depression (CES-D) index (score range, 0–60; 0 equals no dysphoria) (32); outcome expectations for exercise (score range, 1–5; 1 equals no outcome expectations) (33); self-efficacy (scores range 1–5; 1 equals no self-efficacy) (34); and the Physical Component Summary and Mental Component Summary of the SF-36 to assess quality of life (scores range 0–100; 0 equals worst health state) (35). Adherence and occurrence of adverse events were also assessed.
We instructed participants to maintain their regular medications, including nonsteroidal anti-inflammatory drugs (NSAIDs) and acetaminophen. We recorded any change of medication use at each assessment. To test durability of response, we repeated outcome measures at 24 and 48 week follow-ups.
Statistical Analysis
We determined the sample size of 40 patients using the results of a RCT conducted at our Tufts University that tested an exercise intervention among older adults with knee OA (19). That study enrolled 46 patients and randomized them to either a 4-month home-based progressive strength training or an attention control group. The strength training group experienced a 36% decrease in WOMAC pain (the primary outcome) [a mean change of 79 (SD: 91)] compared to an 11% decrease [a mean change of 20 (SD: 77)] in the Attention Control. Based on those numbers, a sample size of 20 per group at α=0.05, would have power 60% to detect an expected difference of 59 points. While we recognized that our study was underpowered for a definitive comparison, we were primarily directed toward gathering preliminary data in order to evaluate this research direction.
We analyzed the data on an intent-to-treat basis. We compared between group changes in outcomes across all times at 0, 12, 24 and 48 weeks with mixed models, using time and group as categorical fixed factors with random intercepts and first order autocorrelation of the errors. Similar mixed models were used to examine weekly WOMAC pain analyses from baseline to 12 weeks. Also, we evaluated for potential effects of confounding or interaction with treatment by covariates including age, gender, BMI, disease duration, disease severity (pain, function and radiograph score), comorbidities, health status, and use of pain medications. A 2-sided p-value < 0.05 was considered to indicate statistical significance. Results are presented as between group differences with 95% confidence intervals of the differences.
RESULTS
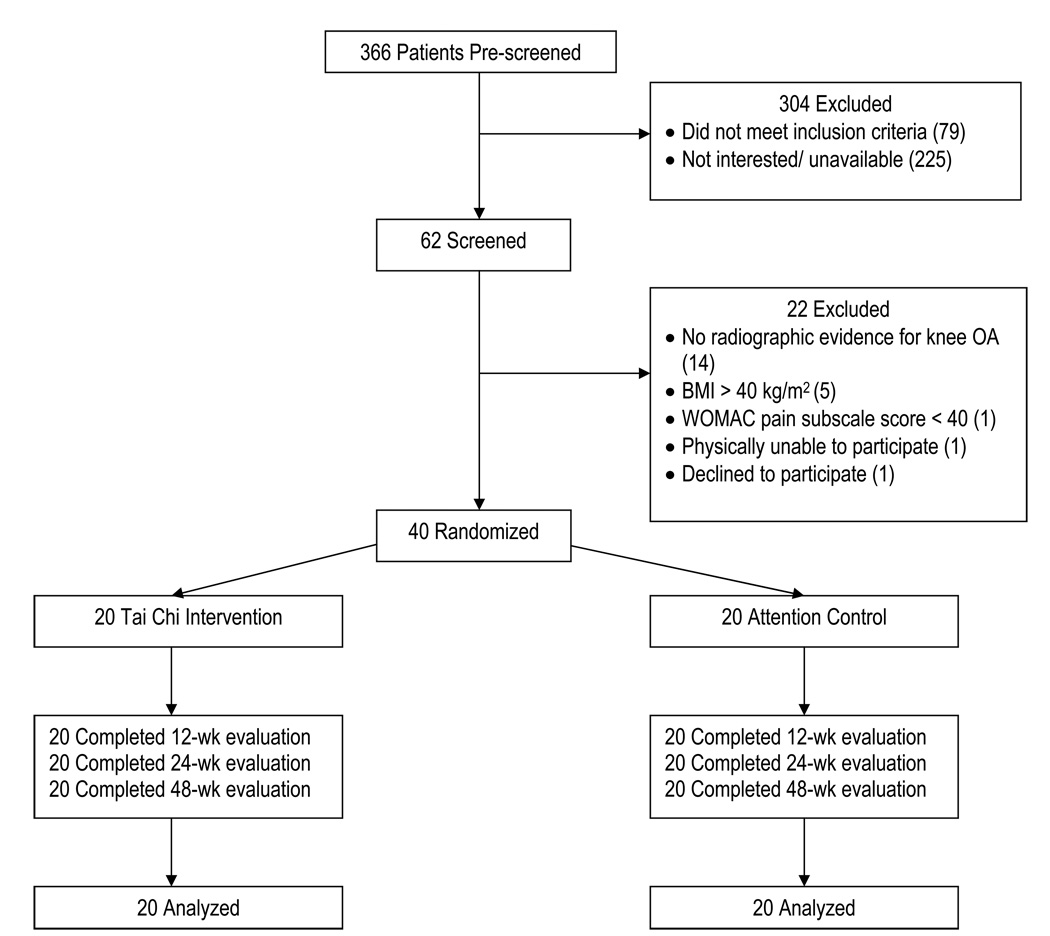
Between October 2005 and February 2006, 366 individuals were screened by telephone and 62 were identified for further evaluation. Forty participants (65%) were found eligible and randomized to the Tai Chi or Attention Control group. The remaining participants were excluded for a variety of reasons (Figure 1), the major one being absence of radiographic evidence of knee OA.
Figure 1.
Study Flow Chart
Baseline data
Table 1 shows baseline data of the 40 participants before randomization to the intervention groups. The participants had a mean age of 65 years, were mainly female (75%) and white (70%). On average, participants had 10 years of knee pain and BMI of 30.0 kg/m2. There were 2 patients, 1 in each group, who were enrolled with self-reported asymptomatic total knee replacement (one knee), but a symptomatic non-operated knee (study knee). Baseline characteristics were reasonably well-balanced between the groups, although there was somewhat greater knee OA severity and comorbidity in the control group.
Table 1.
Baseline Characteristics of Study Participants*
| Variable | Tai Chi (n=20) | Attention Control (n=20) | Total (n=40) | |
|---|---|---|---|---|
| Demographics | ||||
| Female, no. (%) | 16 (80) | 14 (70) | 30 (75) | |
| Age, yr. | 63 (8.1) | 68 (7.0) | 65 (7.8) | |
| White, n (%) | 14 (70) | 14 (70) | 28 (70) | |
| ≥ High school education, n (%) | 20 (100) | 19 (95) | 39 (98) | |
| Body Mass Index, kg/m2 | 30.0 (5.2) | 29.8 (4.3) | 29.9 (4.8) | |
| Disease condition | ||||
| Duration of knee pain, yrs. (on study knee) | 9.7 (7.0) | 9.7 (8.3) | 9.7 (7.6) | |
| Radiograph score, n (%) | ||||
| K and L 2 | 4 (20) | 3 (15) | 7 (18) | |
| K and L 3 | 7 (35) | 3 (15) | 10 (25) | |
| K and L 4 | 9 (45) | 14 (70) | 23 (58) | |
| Knee surgery, n (%) | 6 (30) | 8 (40) | 14 (35) | |
| (Knee Replacement) | 1 (5) | 1 (5) | 2 (5) | |
| Patient VAS, 0–10 cm† | 4.2 (2.1) | 4.8 (2.0) | 4.5 (2.0) | |
| Physician VAS (study knee), 0–10 cm† | 4.8 (1.7) | 5.8 (2.2) | 5.3 (2.0) | |
| WOMAC-Pain, 0–500 mm† | 209.3 (58.5) | 220.4 (101.0) | 214.8 (81.7) | |
| WOMAC-Physical Function, 0–1700 mm† | 707.6 (246.9) | 827 (258.8) | 767.3 (256.9) | |
| WOMAC-Stiffness, 0–200 mm† | 105.7 (37.3) | 120.7 (50.4) | 113.2 (44.4) | |
| Receiving NSAID prior to study, n (%) | 9 (45) | 13 (65) | 22.0 (55.0) | |
| Receiving analgesics prior to study, n (%) | 4 (20) | 6 (30) | 10.0 (25.0) | |
| Self-reported comorbidities, n (%) | ||||
| Congestive Heart Disease | 1 (5) | 4 (20) | 5 (13) | |
| Hypertension | 7 (35) | 12 (60) | 19 (48) | |
| Diabetes | 0 (0) | 4 (20) | 4 (10) | |
| Health-related quality of life and others | ||||
| SF-36 PCS, 0–100‡ | 37.5 (8.5) | 32.0 (8.8)§ | 34.8 (9.0) | |
| SF-36 MCS, 0–100‡ | 51.4 (12.2) | 50.8 (12.6) | 51.1 (12.3) | |
| CES-D, 0–60† | 13.6 (11.7) | 9.3 (9.2) | 11.5 (10.6) | |
| Self-Efficacy score, 1–5‡ | 3.1 (1.1) | 3.3 (1.0) | 3.2 (1.0) | |
| Outcome Expectation score, 1–5¶ | 4.1 (0.6) | 4.3 (0.4) | 4.2 (0.5) | |
| Physical Performance | ||||
| 6-Minute Walk Test (yards) | 500.1 (114.3) [19] | 488.9 (109.2) | 494.3 (110.4) [39] | |
| Balance score, 0–5 | 4.0 (0.7) | 3.8 (0.8) | 3.9 (0.7) | |
| Chair stand score (seconds) | 40.8 (13.4) | 35.6 (9.2) [19] | 38.3 (11.7) [39] | |
Values are mean (SD) unless otherwise noted. N=20 except where specified by data in square brackets. P values were calculated by the t-test for continuous variables and the chi-square test or Fisher exact tests for categorical variables. K and L= Kellgren and Lawrence scale; VAS= Visual Analogue Scale; WOMAC= Western Ontario and McMaster Universities; NSAID= Non-Steroidal Anti-inflammatory Drugs; SF-36= Short Form-36 questionnaire; CES-D= Center for Epidemiology Studies Depression index.
Lower scores indicate improved state.
Higher scores indicate improved state.
P< 0.05
Higher scores indicate high outcome expectations.
Adherence
Attendance for the interventions was 85% for Tai Chi and 89% for Attention Control over 12 weeks. No patient withdrew from the study (40/40 participants completed follow-ups at 12, 24 and 48 weeks). We followed our rigorous study protocol to achieve high levels of adherence and attendance (14). We built a highly experienced and dedicated research team, selected participants who were interested and reliable, accommodated patients preference when scheduling evaluation visits, randomized patients after the baseline evaluation to have a large enough pool for replacements, engaged in friendly personal contact with patients, organized interesting classes, conducted a rigorous quality control program, and prepared a detailed description of the training sessions which we pilot-tested prior to initiation of this study. We offered subjects a monetary incentive to maximize participation and rigorously adhered to the Manual of Operations to enhance compliance.
At the 24 week follow-up, 13 of 20 participants (65%) in the Tai Chi group continued to practice Tai Chi, and 12 of 20 (60%) in the control group continued to practice stretching exercises. At the 48 week follow-up, these rates were 9 of 20 (45%) for Tai Chi and 8 of 20 (40%) for the control.
Primary outcome
WOMAC pain at 12 weeks
At 12 weeks, the Tai Chi arm exhibited a statistically significant decrease in knee pain as measured by the WOMAC pain scale, compared to Attention Control. The between group mean difference was −118.80 (95% confidence interval, −183.66 to −53.94; P= 0.0005) (Table 2).
Table 2.
Changes in Primary and Secondary Outcomes.* Data presented as mean (95% CI).
| Improvement from Baseline | Between Group Differences | ||||
|---|---|---|---|---|---|
| Variable | Tai Chi (n=20) | Control (n=20) | Tai Chi vs. Control | P-value† | |
|
PRIMARY OUTCOME WOMAC-Pain, 0–500 mm‡ |
|||||
| Week 12 | −157.25 (−203.11 to −111.39) | −38.45 (−84.31 to 7.41) | −118.80 (−183.66 to −53.94) | 0.0005 | |
| Week 24 | −131.55 (−177.41 to −85.69) | −64.60 (−110.46 to −18.74) | −66.95 (−131.81 to −2.09) | 0.05 | |
| Week 48 | −115.35 (−161.21 to −69.49) | −69.20 (−115.06 to −23.34) | −46.15 (−111.01 to 18.71) | 0.2 | |
| SECONDARY OUTCOMES | |||||
|
WOMAC-Physical Function, 0–1700 mm‡ |
|||||
| Week 12 | −506.75 (−640.66 to −372.84) | −182.15 (−316.06 to −48.24) | −324.60 (−513.98 to −135.22) | 0.001 | |
| Week 24 | −440.50 (−574.41 to −306.59) | −257.30 (−391.21 to −123.39) | −183.20 (−372.58 to 6.18) | 0.06 | |
| Week 48 | −405.85 (−539.76 to −271.94) | −300.55 (−434.46 to −166.64) | −105.30 (−294.68 to 84.08) | 0.3 | |
| WOMAC-Stiffness, 0–200 mm‡ | |||||
| Week 12 | −73.05 (−94.36 to −51.74) | −50.15 (−71.46 to −28.84) | −22.90 (−53.04 to 7.24) | 0.1 | |
| Week 24 | −65.00 (−86.31 to −43.69) | −50.20 (−71.51 to −28.89) | −14.80 (−44.94 to 15.34) | 0.3 | |
| Week 48 | −64.15 (−85.46 to −42.84) | −60.50 (−81.81 to −39.19) | −3.65 (−33.79 to 26.49) | 0.8 | |
| Physician, 0– 10 cm VAS‡ | |||||
| Week 12 | −3.14 (−3.88 to −2.41) | −1.44 (−2.18 to −0.70) | −1.71 (−2.75 to −0.66) | 0.002 | |
| Week 24 | −2.59 (−3.33 to −1.86) | −2.06 (−2.80 to −1.32) | −0.53 (−1.58 to 0.51) | 0.3 | |
| Week 48 | −2.53 (−3.27 to −1.80) | −1.50 (−2.25 to −0.75) [19] | −1.03 (−2.09 to 0.02) | 0.06 | |
| Patient Global, 0– 10 cm VAS‡ | |||||
| Week 12 | −2.98 (−4.16 to −1.80) | −0.83 (−2.00 to 0.35) | −2.15 (−3.82 to −0.49) | 0.01 | |
| Week 24 | −2.36 (−3.53 to −1.18) | −1.71 (−2.89 to −0.53) | −0.65 (−2.31 to 1.02) | 0.4 | |
| Week 48 | −1.65 (−2.83 to −0.48) | −1.70 (−2.87 to −0.52) | 0.04 (−1.62 to 1.70) | 1.0 | |
| 6 Minute Walk Test (yards)§ | |||||
| Week 12 | 48.33 (11.15 to 85.50) [18] | −1.76 (−50.70 to 47.18) | 50.08 (−10.34 to 110.50) | 0.1 | |
| Week 24 | 53.12 (10.04 to 96.21) [19] | 9.41 (−33.48 to 52.30) | 43.71 (−15.07 to 102.50) | 0.1 | |
| Week 48 | 35.17 (−17.29 to 87.64) [19] | 20.56 (−20.73 to 61.85) [19] | 14.61 (−49.36 to 78.59) | 0.7 | |
| Balance Score, 0–5§ | |||||
| Week 12 | 0.15 (−0.16 to 0.46) | 0.25 (−0.06 to 0.56) | −0.10 (−0.54 to 0.34) | 0.7 | |
| Week 24 | 0.15 (−0.16 to 0.46) | 0.08 (−0.24 to 0.39) | 0.07 (−0.37 to 0.52) | 0.7 | |
| Week 48 | 0.35 (0.04 to 0.66) | 0.46 (0.14 to 0.77) [19] | −0.11 (−0.55 to 0.34) | 0.6 | |
| Chair Stand Time (seconds)‡ | |||||
| Week 12 | −12.03 (−15.60 to −8.46) [19] | −1.15 (−4.70 to 2.40) [19] | −10.88 (−15.91 to −5.84) | 0.00005 | |
| Week 24 | −9.87 (−13.44 to −6.30) [19] | −4.75 (−8.30 to −1.20) [19] | −5.12 (−10.15 to −0.08) | 0.05 | |
| Week 48 | −9.22 (−12.79 to −5.65) [19] | −3.24 (−6.85 to 0.37) [18] | −5.98 (−11.06 to −0.91) | 0.02 | |
| Body Mass Index, kg/m2 | |||||
| Week 12 | 0.04 (−0.27 to 0.36) | −0.17 (−0.51 to 0.17) | 0.21 (−0.23 to 0.66) | 0.34 | |
| Week 24 | 0.10 (−0.37 to 0.57) | −0.02 (−0.38 to 0.34) | 0.13 (−0.45 to 0.70) | 0.66 | |
| Week 48 | −0.07 (−0.54 to 0.40) | −0.29 (−0.72 to 0.15) | 0.22 (− 0.40 to 0.84) | 0.48 | |
| SF-36 Mental Component Summary, 0–100§ | |||||
| Week 12 | 2.14 (−2.35 to 6.64) | 1.93 (−2.56 to 6.43) | 0.21 (−6.15 to 6.57) | 0.9 | |
| Week 24 | 4.39 (−0.11 to 8.89) | 4.50 (0.00 to 9.00) | −0.11 (−6.47 to 6.25) | 1.0 | |
| Week 48 | 5.80 (1.31 to 10.30) | 1.04 (−3.46 to 5.53) | 4.77 (−1.59 to 11.13) | 0.1 | |
| SF-36 Physical Component Summary, 0–100§ | |||||
| Week 12 | 11.57 (8.08 to 15.06) | 4.14 (0.65 to 7.63) | 7.43 (2.50 to 12.36) | 0.004 | |
| Week 24 | 10.80 (7.31 to 14.29) | 6.29 (2.80 to 9.77) | 4.51 (−0.42 to 9.45) | 0.08 | |
| Week 48 | 10.41 (6.92 to 13.90) | 4.10 (0.61 to 7.58) | 6.32 (1.38 to 11.25) | 0.01 | |
| CES-D, 0–60‡ | |||||
| Week 12 | −7.40 (−10.88 to −3.92) | −0.70 (−4.18 to 2.78) | −6.70 (−11.63 to −1.77) | 0.009 | |
| Week 24 | −6.40 (−9.88 to −2.92) | −1.10 (−4.58 to 2.38) | −5.30 (−10.23 to −0.37) | 0.04 | |
| Week 48 | −7.25 (−10.73 to −3.77) | 1.65 (−1.83 to 5.13) | −8.90 (−13.83 to −3.97) | 0.0006 | |
| Self-Efficacy Score, 1–5§ | |||||
| Week 12 | 0.60 (0.12 to 1.08) | −0.11 (−0.59 to 0.37) | 0.71 (0.03 to 1.39) | 0.04 | |
| Week 24 | 0.68 (0.20 to 1.16) | −0.17 (−0.65 to 0.31) | 0.85 (0.17 to 1.53) | 0.02 | |
| Week 48 | 0.72 (0.24 to 1.20) | −0.24 (−0.72 to 0.24) | 0.96 (0.28 to 1.64) | 0.007 | |
N=20 except where specified by data in square brackets. WOMAC= Western Ontario and McMaster Universities; VAS= Visual Analogue Scale; SF-36= Short-Form health survey; CES-D= Center for Epidemiology Studies Depression index.
P values were calculated by the t-test for continuous variables.
Lower scores indicate improved state.
Higher scores indicate improved state.
Secondary outcomes
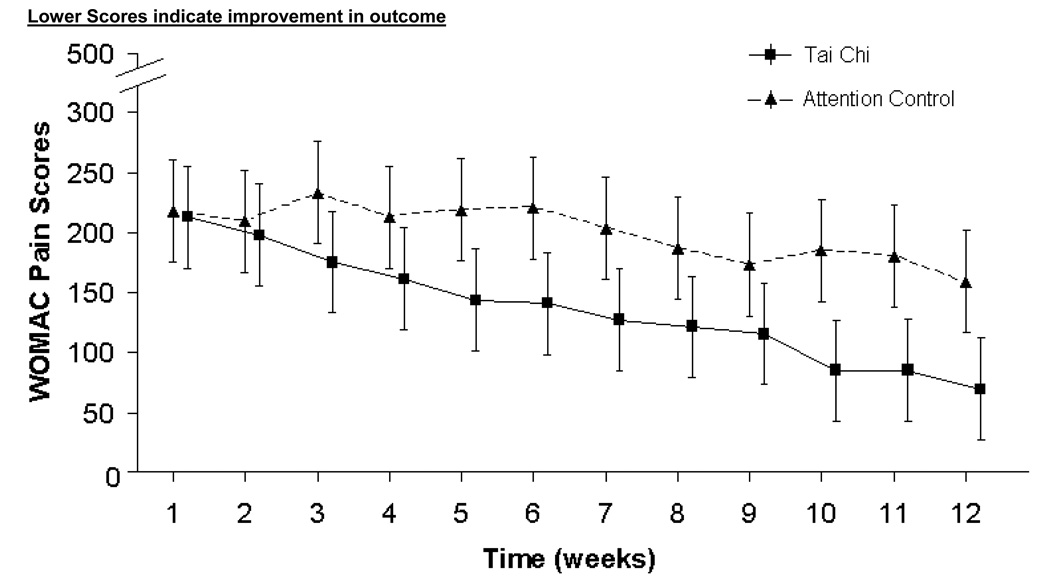
Figure 2 shows that the between group mean difference gradually increased during the 12-week intervention based on the nearly linear decline in pain with Tai Chi.
Figure 2.
WOMAC Pain Subscale over a 12 week Intervention Period by Treatment Group
Values shown are unadjusted means. Measurements were obtained weekly over a 12 week period, Error bars indicate the 95% Confidence Interval (CI) but the data are slightly offset in the figure for clarity. Means with 95% CI shown at each line for each group. Linear treads between weeks indicated by connected graph. WOMAC= Western Ontario and McMaster Universities Osteoarthritis index.
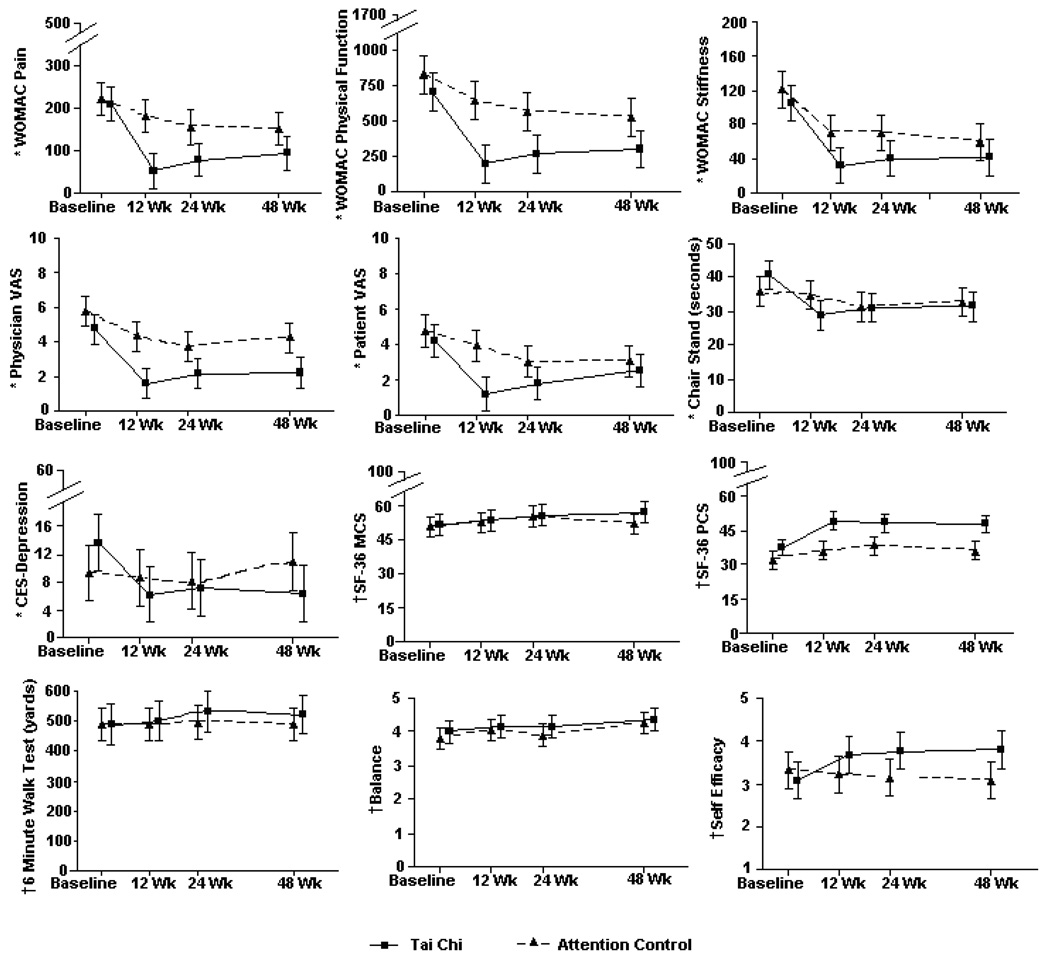
Table 2 compares changes in all of the secondary outcomes between groups from baseline to 12, 24 and 48 weeks. These changes are illustrated in Figure 3.
Figure 3.
Mean Change of Secondary Outcomes by Treatment Group at Baseline, 12, 24, and 48 Weeks
Values shown are unadjusted means (SD). Error bars indicate the 95% Confidence Interval. Measurements were obtained at Baseline, 12 weeks, 24 weeks and 48 weeks, but the data are slightly offset in the figure for clarity. WOMAC= Western Ontario and McMaster Universities; VAS= Visual Analogue Scale; CES-Depression= the Center for Epidemiology Studies Depression; SF-36= Short-Form health survey; MCS= Mental Component Summary; PCS= Physical Component Summary.
* Lower scores indicate improvement in outcome
† Higher scores indicate improvement in outcome.
WOMAC pain at 24 and 48 weeks
At 24 and 48 weeks, there remained a large WOMAC pain reduction from baseline, although not as large as at 12 weeks. The reduction was borderline statistically significant at 24 weeks (P= 0.05) but not statistically significant at 48 weeks (P= 0.2).
WOMAC physical function and stiffness at 12, 24 and 48 weeks
At 12 weeks, participants in the Tai Chi arm exhibited greater improvement in WOMAC physical function compared to the Attention Control (mean difference, −324.60 [CI, −513.98 to −135.22; P= 0.001]). There were non-statistically significant improvements at both 24 and 48 weeks. Tai Chi participants showed more improvement at all times for WOMAC stiffness though it was not statistically significant.
Patient and physician global assessment
At 12 weeks, compared to the Attention Control, participants in the Tai Chi group improved in the subjective self-report patients’ global assessment −2.15 (CI, −3.82 to −0.49; P= 0.01) and the objective physician global assessment, −1.71 (CI, −2.75 to −0.66; P=0.002). These changes did not remain statistically significant at 24 and 48 weeks.
Physical performance and Body Mass Index
The chair stand time was statistically significantly reduced, −10.88 seconds (CI, −15.91 to −5.84; P= 0.00005) at 12 weeks, 5 seconds at 24 weeks, and 6 seconds at 48 weeks. The Tai Chi group was also able to walk 50, 44 and 15 yards further in 6 minutes at 12, 24 and 48 weeks, respectively, although none were statistically significant. Notably, changes in BMI and balance test at each assessment were not statistically significant.
Quality of life and psychological variables
At 12 weeks, the Tai Chi group improved compared to the control group on mean Physical Component Summary score, 7.43 (CI, 2.50 to 12.36; P = 0.004), CES-Depression, −6.70 (CI, −11.63 to −1.77; P=0.009) and self-efficacy score, 0.71 (0.03 to 1.39, P = 0.04). Small non-statistically significant improvements were seen in both groups on the Mental Component Summary score. Notably, statistically significant improvements on self-efficacy and depression were maintained for Tai Chi at 24 and 48 weeks.
Evaluation for confounding by participant group characteristics
Regression adjustment for baseline characteristics, including radiographic severity and number of comorbidities, revealed no confounding variables or interactions with treatment assignment.
Adverse Events
One participant in the Tai Chi group reported an increase in knee pain at the 2 week assessment. This was resolved following modification of that participant’s Tai Chi technique. One participant in each assignment group reported newly diagnosed cancers (1 breast cancer, 1 colon cancer) during the 12-week intervention period (the patient in the Tai Chi group missed 4 intervention visits but completed her follow-up evaluations). No other adverse events were reported.
Analgesics and NSAIDs Use
At baseline, 11 of 20 (55%) participants in the Tai Chi group were receiving analgesics and NSAIDs, compared to 14 of 20 (70%) in the Attention Control. The numbers decreased to 6 of 20 (30 %) for Tai Chi and 10 of 20 (50%) for control at the 12-week assessment (Table 3). We found no statistically significant differences between groups who were using any of the 2 categories of medications.
Table 3.
Use of Analgesics and NSAIDs*
| Tai Chi, No. (%) (n=20) | Control, No. (%) (n=20) | |||
|---|---|---|---|---|
| Medication | Baseline | 12 week | Baseline | 12 week |
| Analgesics | 4 (20) | 3 (15) | 6 (30) | 4 (20) |
| NSAIDs | 9 (45) | 5 (25) | 13 (65) | 9 (45) |
NSAID= Nonsteroidal Anti-inflammatory Drugs.
DISCUSSION
Overall, Tai Chi appears to reduce pain and improve physical function for people with knee OA. The measures of benefit include patient-reported outcomes as well as physician assessments and several physical function tests. We also observed significant benefits in the measures of depression and self-efficacy that appeared durable for participants who continued to practice Tai Chi beyond the 12-week intervention period. Thus, in this first long term follow-up trial of Tai Chi for knee OA, the Tai Chi group seems to have developed a general sense of well being, suggesting that there may be synergy between the physical and mental components of this discipline. These findings are promising because there are few efficacious long-lasting treatments for knee OA (2, 3).
There have been several previous trials testing the effects of Tai Chi for OA (13, 36–39). However, interpretation of their results is limited by low levels of adherence (13, 37) short follow up (13, 36–39), deployment of varying Tai Chi styles (13, 37), and inclusion of heterogeneous types of OA (13). Nevertheless, our results are consistent with some of their positive findings for improvements in pain (36, 37) and function (13, 37, 39). Our findings are also consistent with prior studies showing benefits of Tai Chi on self-efficacy, depression and quality of life (9). However, our study did not show any improvement in balance tests as was shown in a number of other studies (9).
Recent efforts have suggested that there is the minimal clinically important difference for WOMAC scores from both pharmacological and rehabilitation trials (40–41). In our trial, the Tai Chi group had a 75% improvement of WOMAC pain over baseline (57% greater than control) and 72% improvement of WOMAC function over baseline (46% greater than control). Thus, our study shows that Tai Chi gives more than the minimally perceptible improvement for patients.
Most of our participants were significantly overweight with an average BMI of 30 kg/m2. It is well known that significant weight reduction can improve symptoms of knee OA (42). However, there was no significant weight reduction for either group during the trial. In addition, the two groups did not differ in medication usage, and it is unlikely that the difference in outcomes between the groups was attributable to changes in medication patterns occurring over the course of the trial.
Explanatory theories from eastern and western literature provide a supposed rationale for the effectiveness of Tai Chi to treat knee OA (43, 44). While the biological mechanisms by which Tai Chi may improve the clinical consequence of knee OA still remain unknown, synergy between its physical and mental components likely plays a major role. First, Tai Chi may enhance cardiovascular benefits, muscular strength, balance, coordination, and physical function (9). All of these are thought to be able to reduce joint pain. As the severity of pain is directly correlated with the degree of muscle weakness (43), stronger muscles and better coordination improve the stability of the joints and lessen pain. Increased peri-articular muscle strength may also protect joints from traumatic impacts. Second, evidence suggests that the mind-body component may influence immune, endocrine, neurochemical and autonomic functioning (44). Third, controlled breathing and movements promotes a restful state and mental tranquility. These influences may help break the arthritis “pain cycle” (45). Improving self-efficacy, social function and depression can also help people build confidence, get support and overcome fears of pain. Together, these can lead to improved physical, psychological and psychosocial well-being and overall quality of life (46).
Our study had some limitations: First, the attention group appears to have had more severe knee OA, as measured by WOMAC physical function, radiography scores and self-reported comorbidities at baseline. This difference likely occurred by chance as a result of the relatively small sample size, rather than as a problem with the randomization procedures. Regression adjustment for these baseline differences did not change any of the conclusions. The possibility exists that some unidentified confounding factors were not measured in our trial, such as socio-economic status and knee malalignment and these factors will be considered in our future work. Second, we could not mask the participants to treatment assignment. While an elaborate sham treatment might accomplish such blinding, no validated approach for this currently exists. As a result, participants’ a priori beliefs and expectations with respect to Tai Chi could have biased their subjective outcome assessments. Therefore, we attempted to minimize such expectations by maintaining a stance of equipoise regarding the likely benefits of the two interventions. By de-emphasizing our specific interest in Tai Chi, participant expectations would have been reduced. In addition, we tested to see if expectations might have produced any bias. We found that the baseline outcome expectations of benefit from an exercise intervention were similar in both groups (Tai Chi= 4.1 [SD 0.6], control = 4.3 [SD 0.4]). Furthermore, total session attendance was similar in both groups (89% control, 85% Tai Chi) indicating that our neutral presentation of the interventions may have succeeded. A third limitation, instruction by a single Tai Chi master, might limit generalizability. However, we only made minor modifications to the movements of the classical Yang Style to avoid knee injury. Thus, it should not be difficult for other instructors to implement and for participants to practice at home, so that the benefits of Tai Chi may be extended to the general population. Finally, even though the patients were instructed not to communicate to the blinded assessors about their treatment assignments, there is the possibility that leakage of information did occur even though the study physician reported no such leakage.
In conclusion, 12-week Tai Chi appears to reduce pain and improve physical function, self-efficacy, depression and health status for knee OA. These observations emphasize a need to further evaluate Tai Chi’s biological mechanisms and approaches to extend its benefits to a broader population. Further studies should replicate these results and deepen our understanding of this therapeutic modality.
ACKNOWLEDGMENTS
The authors gratefully acknowledge the Data Safety Monitoring Board members: Drs. Karen H. Costenbader, Kristin Baker, Wenjun Li and Ms. Resa Arovas for their insightful suggestions for the study protocol. We are grateful to Jun Wang, Marcie Griffith, Aghogho Okparavero, Xiaoyan Chen, Melynn Nuite, Erica McAdams, Xiaogang Gao, Steve Wong, Ian Schmid and Clinical Research Center nurses for their help with different aspects of the study and to Drs. Haewook Han and Harry Pino for their expertise in teaching the control group. The authors also thank Judith L Ramel for her assistance in preparing this manuscript. We gratefully acknowledge the participation of our study subjects; their cooperation, encouragement and enthusiasm were an inspiration to the investigators.
The contents of this manuscript are solely the responsibility of the authors and do not necessarily represent the official views of the National Center for Complementary and Alternative Medicine or the National Institutes of Health. The sponsors had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; and preparation, review or approval of the manuscript.
This study was supported by the National Center for Complementary and Alternative Medicine of the National Institutes of Health (R21AT002161).
Footnotes
Trial Registration: clinicaltrials.gov Identifier: NCT00362453
AUTHOR CONTRIBUTIONS
Dr. Wang had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Study design. Wang, Schmid, Hibberd, Kalish, Roubenoff, and McAlindon
Acquisition of data. Wang, Schmid, Hibberd and Kalish
Analysis and interpretation of data. Wang, Schmid, Hibberd, Kalish, Roubenoff, and McAlindon
Manuscript preparation. Wang, Schmid, Hibberd, Kalish, Roubenoff, and McAlindon
Statistical analysis. Schmid
Collection of funds. Wang
REFERENCES
- 1.Felson DT. Clinical practice. Osteoarthritis of the knee. N Engl J Med. 2006;354:841–848. doi: 10.1056/NEJMcp051726. [DOI] [PubMed] [Google Scholar]
- 2.Zhang W, Moskowitz RW, Nuki G, et al. OARSI recommendations for the management of hip and knee osteoarthritis, Part II: OARSI evidence-based, expert consensus guidelines. Osteoarthritis Cartilage. 2008;16:137–162. doi: 10.1016/j.joca.2007.12.013. [DOI] [PubMed] [Google Scholar]
- 3.Royal College of Physicians. URL: http://www.nice.org.uk/nicemedia/pdf/CG059FullGuideline.pdf.
- 4.van Baar ME, Dekker J, Lemmens JA, Oostendorp RA, Bijlsma JW. Pain and disability in patients with osteoarthritis of hip or knee: the relationship with articular, kinesiological, and psychological characteristics. J Rheumatol. 1998;25:125–133. [PubMed] [Google Scholar]
- 5.Slemenda C, Brandt KD, Heilman DK, et al. Quadriceps weakness and osteoarthritis of the knee. Ann Intern Med. 1997;127:97–104. doi: 10.7326/0003-4819-127-2-199707150-00001. [DOI] [PubMed] [Google Scholar]
- 6.Rejeski WJ, Miller ME, Foy C, Messier S, Rapp S. Self-efficacy and the progression of functional limitations and self-reported disability in older adults with knee pain. J Gerontol B Psychol Sci Soc Sci. 2001;56:S261–S265. doi: 10.1093/geronb/56.5.s261. [DOI] [PubMed] [Google Scholar]
- 7.Zhang W, Moskowitz RW, Nuki G, et al. OARSI recommendations for the management of hip and knee osteoarthritis, part I: critical appraisal of existing treatment guidelines and systematic review of current research evidence. Osteoarthritis Cartilage. 2007;15:981–1000. doi: 10.1016/j.joca.2007.06.014. [DOI] [PubMed] [Google Scholar]
- 8.Jamtvedt G, Dahm KT, Christie A, et al. Physical therapy interventions for patients with osteoarthritis of the knee: an overview of systematic reviews. Phys Ther. 2008;88:123–136. doi: 10.2522/ptj.20070043. [DOI] [PubMed] [Google Scholar]
- 9.Wang C, Collet JP, Lau J. The effect of Tai Chi on health outcomes in patients with chronic conditions: a systematic review. Arch Intern Med. 2004;164:493–501. doi: 10.1001/archinte.164.5.493. [DOI] [PubMed] [Google Scholar]
- 10.Jordan KM, Arden NK, Doherty M, et al. EULAR Recommendations 2003: an evidence based approach to the management of knee osteoarthritis: Report of a Task Force of the Standing Committee for International Clinical Studies Including Therapeutic Trials (ESCISIT) Ann Rheum Dis. 2003;62:1145–1155. doi: 10.1136/ard.2003.011742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Axford J, Heron C, Ross F, Victor CR. Management of knee osteoarthritis in primary care: pain and depression are the major obstacles. J Psychosom Res. 2008;64:461–467. doi: 10.1016/j.jpsychores.2007.11.009. [DOI] [PubMed] [Google Scholar]
- 12.Lee MS, Pittler MH, Ernst E. Tai chi for osteoarthritis: a systematic review. Clin Rheumatol. 2008;27:211–218. doi: 10.1007/s10067-007-0700-4. [DOI] [PubMed] [Google Scholar]
- 13.Fransen M, Nairn L, Winstanley J, Lam P, Edmonds J. Physical activity for osteoarthritis management: a randomized controlled clinical trial evaluating hydrotherapy or Tai Chi classes. Arthritis Rheum. 2007;57:407–414. doi: 10.1002/art.22621. [DOI] [PubMed] [Google Scholar]
- 14.Wang C, Schmid C, Hibberd P, et al. Tai Chi for treating knee osteoarthritis: designing a long-term follow up randomized controlled trial. BMC Musculoskelet Disord. 2008;9:108. doi: 10.1186/1471-2474-9-108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Altman R, Asch E, Bloch D, et al. Development of criteria for the classification and reporting of osteoarthritis. Classification of osteoarthritis of the knee. Diagnostic and Therapeutic Criteria Committee of the American Rheumatism Association. Arthritis Rheum. 1986;29:1039–1049. doi: 10.1002/art.1780290816. [DOI] [PubMed] [Google Scholar]
- 16.Kellgren JH, Lawrence JS. Radiological assessment of osteo-arthrosis. Ann Rheum Dis. 1957;16:494–502. doi: 10.1136/ard.16.4.494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Folstein MF, Folstein SE, McHugh PR. "Mini-mental state". A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res. 1975;12:189–198. doi: 10.1016/0022-3956(75)90026-6. [DOI] [PubMed] [Google Scholar]
- 18.Wang C, Lau J, Roubenoff R, Kalish R, Christopher S, Hibberd P. Tai Chi improves pain and functional status in adult with rheumatoid arthritis. Arthritis Rheum. 2003;48:3656–3658. [Google Scholar]
- 19.Baker KR, Nelson ME, Felson DT, Layne JE, Sarno R, Roubenoff R. The efficacy of home based progressive strength training in older adults with knee osteoarthritis: a randomized controlled trial. Journal of Rheumatology. 2001;28:1655–1665. [PubMed] [Google Scholar]
- 20.Simplified "Taijiquan". Beijing, China: China Publications Center; 1983. China Sports. [Google Scholar]
- 21.van Baar ME, Assendelft WJ, Dekker J, Oostendorp RA, Bijlsma JW. Effectiveness of exercise therapy in patients with osteoarthritis of the hip or knee: a systematic review of randomized clinical trials. Arthritis Rheum. 1999;42:1361–1369. doi: 10.1002/1529-0131(199907)42:7<1361::AID-ANR9>3.0.CO;2-9. [DOI] [PubMed] [Google Scholar]
- 22.Wang C, Schmid CH, Hibberd PL, et al. Tai Chi for treating knee osteoarthritis: designing a long-term follow up randomized controlled trial. BMC Musculoskelet Disord. 2008;9:108. doi: 10.1186/1471-2474-9-108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.U.S. Department of Health and Human Services and U.S. Department of Agriculture. URL: http://www.health.gov/DietaryGuidelines/dga2005/document/default.htm.
- 24.U.S. Department of Health and Human Services, National Institutes of Health, National Institute of Arthritis and Musculoskeletal and Skin Diseases. URL: http://www.niams.nih.gov/Health_Info/Osteoarthritis/default.asp.
- 25.Bellamy N, Kirwan J, Boers M, et al. Recommendations for a core set of outcome measures for future phase III clinical trials in knee, hip, and hand osteoarthritis. Consensus development at OMERACT III. J Rheumatol. 1997;24:799–802. [PubMed] [Google Scholar]
- 26.Bellamy N. WOMAC: osteoarthritis index: A user's guide. London, ON, Canada: University of Western Ontario; 1995. [Google Scholar]
- 27.Bellamy N, Buchanan WW, Goldsmith CH, Campbell J, Stitt LW. Validation study of WOMAC: a health status instrument for measuring clinically important patient relevant outcomes to antirheumatic drug therapy in patients with osteoarthritis of the hip or knee. J Rheumatol. 1988;15:1833–1840. [PubMed] [Google Scholar]
- 28.Altman R, Brandt K, Hochberg M, et al. Design and conduct of clinical trials in patients with osteoarthritis: recommendations from a task force of the Osteoarthritis Research Society. Results from a workshop. Osteoarthritis Cartilage. 1996;4:217–243. doi: 10.1016/s1063-4584(05)80101-3. [DOI] [PubMed] [Google Scholar]
- 29.Csuka M, McCarty DJ. Simple method for measurement of lower extremity muscle strength. Am J Med. 1985;78:77–81. doi: 10.1016/0002-9343(85)90465-6. [DOI] [PubMed] [Google Scholar]
- 30.Guyatt GH, Sullivan MJ, Thompson PJ, et al. The 6-minute walk: a new measure of exercise capacity in patients with chronic heart failure. Can Med Assoc J. 1985;132:919–923. [PMC free article] [PubMed] [Google Scholar]
- 31.Messier SP, Royer TD, Craven TE, O'Toole ML, Burns R, Ettinger WH., Jr Long-term exercise and its effect on balance in older, osteoarthritic adults: results from the Fitness, Arthritis, and Seniors Trial (FAST) J Am Geriatr Soc. 2000;48:131–138. doi: 10.1111/j.1532-5415.2000.tb03903.x. [DOI] [PubMed] [Google Scholar]
- 32.Radloff LS. The CES-D scale: a new self-report depression scale fore research in the general population. Applied Psychological Measure. 1977;1 385-340. [Google Scholar]
- 33.Resnick B, Zimmerman SI, Orwig D, Furstenberg AL, Magaziner J. Outcome expectations for exercise scale: utility and psychometrics. J Gerontol B Psychol Sci Soc Sci. 2000;55:S352–S356. doi: 10.1093/geronb/55.6.s352. [DOI] [PubMed] [Google Scholar]
- 34.Marcus BH, Selby VC, Niaura RS, Rossi JS. Self-efficacy and the stages of exercise behavior change. Res Q Exerc Sport. 1992;63:60–66. doi: 10.1080/02701367.1992.10607557. [DOI] [PubMed] [Google Scholar]
- 35.Ware JE, Jr, Sherbourne CD. The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Med Care. 1992;30:473–483. [PubMed] [Google Scholar]
- 36.Brismee JM, Paige RL, Chyu MC, et al. Group and home-based tai chi in elderly subjects with knee osteoarthritis: a randomized controlled trial. Clin Rehabil. 2007;21:99–111. doi: 10.1177/0269215506070505. [DOI] [PubMed] [Google Scholar]
- 37.Song R, Lee EO, Lam P, Bae SC. Effects of tai chi exercise on pain, balance, muscle strength, and perceived difficulties in physical functioning in older women with osteoarthritis: a randomized clinical trial. J Rheumatol. 2003;30:2039–2044. [PubMed] [Google Scholar]
- 38.Hartman CA, Manos TM, Winter C, Hartman DM, Li B, Smith JC. Effects of T'ai Chi training on function and quality of life indicators in older adults with osteoarthritis. J Am Geriatr Soc. 2000;48:1553–1559. doi: 10.1111/j.1532-5415.2000.tb03863.x. [DOI] [PubMed] [Google Scholar]
- 39.Lee HY, Lee KJ. Effects of Tai Chi exercise in elderly with knee osteoarthritis. Taehan Kanho Hakhoe Chi. 2008;38:11–18. doi: 10.4040/jkan.2008.38.1.11. [DOI] [PubMed] [Google Scholar]
- 40.Zhao SZ, McMillen JI, Markenson JA, et al. Evaluation of the functional status aspects of health-related quality of life of patients with osteoarthritis treated with celecoxib. Pharmacotherapy. 1999;19:1269–1278. doi: 10.1592/phco.19.16.1269.30879. [DOI] [PubMed] [Google Scholar]
- 41.Angst F, Aeschlimann A, Stucki G. Smallest detectable and minimal clinically important differences of rehabilitation intervention with their implications for required sample sizes using WOMAC and SF-36 quality of life measurement instruments in patients with osteoarthritis of the lower extremities. Arthritis Rheum. 2001;45:384–391. doi: 10.1002/1529-0131(200108)45:4<384::AID-ART352>3.0.CO;2-0. [DOI] [PubMed] [Google Scholar]
- 42.Rogers MW, Wilder FV. The association of BMI and knee pain among persons with radiographic knee osteoarthritis: A cross-sectional study. BMC Musculoskelet Disord. 2008;9:163. doi: 10.1186/1471-2474-9-163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.O'Reilly SC, Jones A, Muir KR, Doherty M. Quadriceps weakness in knee osteoarthritis: the effect on pain and disability. Ann Rheum Dis. 1998;57:588–594. doi: 10.1136/ard.57.10.588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.National Center for Complementary and Alternative Medicine, NIH. URL: http://nccam.nih.gov/health/taichi/
- 45.Yocum DE, Castro WL, Cornett M. Exercise, education, and behavioral modification as alternative therapy for pain and stress in rheumatic disease. Rheum Dis Clin North Am. 2000;26:145–159. x–xi. doi: 10.1016/s0889-857x(05)70128-9. [DOI] [PubMed] [Google Scholar]
- 46.Wilson IB, Cleary PD. Linking clinical variables with health-related quality of life. A conceptual model of patient outcomes. JAMA. 1995;273:59–65. [PubMed] [Google Scholar]