Abstract
The hypothalamus monitors body energy status in part through specialized glucose sensing neurons that comprise both glucose-excited and glucose-inhibited cells. Here we discuss recent work on the elucidation of neurochemical identities and physiological significance of these hypothalamic cells, including caveats resulting from the currently imprecise functional and molecular definitions of glucose sensing and differences in glucose-sensing responses obtained with different experimental techniques. We discuss the recently observed adaptive glucose-sensing responses of orexin/hypocretin-containing neurons, which allow these cells to sense changes in glucose levels rather than its absolute concentration, as well as the glucose-sensing abilities of melanin-concentrating hormone, neuropeptide Y, and proopiomelanocortin-containing neurons and the recent data on the role of ventromedial hypothalamic steroidogenic factor-1 (SF-1)/glutamate-containing cells in glucose homeostasis. We propose a model where orexin/hypocretin and SF-1/glutamate neurons cooperate in stimulating the sympathetic outflow to the liver and pancreas to increase blood glucose, which in turn provides negative feedback inhibition to these cells. Orexin/hypocretin neurons also stimulate feeding and reward seeking and are activated by hunger and stress, thereby providing a potential link between glucose sensing and goal-oriented behavior. The cell-type-specific neuromodulatory actions of glucose in several neurochemically distinct hypothalamic circuits are thus likely to be involved in coordinating higher brain function and behavior with autonomic adjustments in blood glucose levels.
Keywords: hypocretin, hypothalamus, neuron, orexin
about half a century ago, subgroups of hypothalamic neurons were found to show specialized excitatory or inhibitory firing responses to extracellular glucose, revealing a strategy for how the brain can directly monitor body energy status (3, 69, 70). Glucose sensing in these glucose-excited and glucose-inhibited neurons was not a general energy-related response, because during examination of a large number of neurons in several brain areas, glucose-responding cells were observed only in the hypothalamus and brain stem, but not in other areas, such as the thalamus or cortex (1, 60, 69, 70, 80, 83, 111). More recent work suggests that glucose-sensing neurons may also be found in substantia nigra (113). It is important to emphasize that the effects of glucose on at least some of the glucose-sensing neurons are fundamentally different form the general effects of glucose on neuronal firing due to energy availability. While it may be argued that glucose-excited neurons are simply a more sensitive version of non-glucose-sensing neurons, which would also be stimulated by glucose, especially if they are energy depleted, glucose-inhibited neurons respond in the opposite way to that expected from the general stimulatory fuel injection effects of glucose, and their operation is thus clearly different from a general energy-related effect. Glucose-sensing cells are also found outside the brain, in tissues such as the endocrine pancreas [glucose-excited β-cells and glucose-inhibited α-cells (7, 81)] and the gut [glucose-excited L-cells (79)], but in this review we will predominantly focus on a selection of recent studies of glucose sensing in the hypothalamus. Our aim is not to provide a comprehensive overview of mechanisms of glucose sensing in the brain and periphery, but to highlight key findings and caveats in the recent work linking glucose sensing to specific neurochemically defined hypothalamic neurons and the implications of these findings for whole body glucose homeostasis. For detailed discussions of the electrophysiological and molecular mechanisms of glucose sensing in the brain and in peripheral glucose-sensing cells of the pancreas and the intestine, readers are referred to other recent reviews (e.g., 6, 21, 40, 58, 54, 63, 81, 102). To put the subject into a more general physiological perspective, we will begin with a brief overview of the nature and sources of glucose changes in the brain.
Physiological Fluctuations in Brain Glucose Levels
Simultaneous measurements of extracellular glucose levels in blood and brain show that brain [glucose] is generally lower than plasma [glucose], yet changes in blood [glucose] cause rapid parallel changes in brain [glucose] (83, 92). A thorough review of data on brain glucose levels (30) suggests that during euglycemia, brain glucose levels are ∼0.7–2.5 mM, and a maximum of ∼5 mM may be reached under severe plasma hyperglycemia. In turn, plasma hypoglycemia can cause the brain glucose to fall to 0.2–0.5 mM. This triggers counterregulatory responses where pancreatic glucagon and adrenal catecholamine secretion, as well as hepatic glucose production, are stimulated through activation of sympathetic nerves. Apart from the counterregulatory responses, which are orchestrated by glucosensors in both the brain and periphery (58, 85), hypoglycemia also induces feeding in mammals [glucoprivic feeding (93)]. Glucoprivic feeding has been recently suggested to involve glucose-sensing neurons in the ventromedial hypothalamus (VMH), since it was reduced by blockade of VMH glucokinase, a critical molecular component of some glucose-sensing neurons (31).
Although brain glucose levels are generally lower than those in the blood, it is commonly assumed that glucose concentrations can approach those in the blood at circumventricular organs, areas where the blood-brain barrier is highly permeable, such as the median eminence in the hypothalamus (35). However, it has recently been shown that this does not necessarily apply to brain structures in close vicinity, such as the arcuate nucleus (ARC) (31), perhaps because of tanycyte barriers separating the ARC from the median eminence (64, 74).
Generally speaking, a meal will increase blood glucose and thus also brain glucose, but the extent to which this happens depends on the food. The potency of foods to increase blood glucose is measured as the glycemic index (48), and a major factor affecting this is the macronutrient composition of the food. In particular, meals high in protein or fat generally have a low glycemic index, i.e., they elevate blood glucose less than carbohydrate-rich meals. Another source of blood glucose is the endogenous production of glucose by the liver, which is also under hypothalamic control as reviewed below. Hepatic glucose production is controlled by the pancreatic hormones insulin and glucagon as well as, but to a lesser extent, directly by autonomic innervation (77). Insulin and parasympathetic innervation increase hepatic glucose uptake and glycogen synthesis, whereas glucagon and sympathetic innervation promote glycogenolysis, gluconeogenesis, and glucose release. Blood glucose is also affected by glucose uptake into muscle and adipose tissue, both of which are increased by insulin and sympathetic innervation (67). Below, we will first discuss the neurochemical identities and functional features of glucose-sensing hypothalamic neurons, and then focus on recent studies suggesting that they are key regulators of sympathetic drive that controls uptake and release of glucose in peripheral tissues.
Glucose-Sensing Capabilities of Neurochemically Defined Hypothalamic Neurons
The lateral hypothalamus.
Most recent work focused on lateral hypothalamus (LH) cells that contain the peptide transmitters orexins/hypocretins, which are not expressed anywhere else in the brain (29, 86). Orexin/hypocretin-containing neurons project widely throughout the brain, with especially dense innervation of regions regulating arousal, metabolism, and reward (75). Lack of orexins/hypocretins produces the symptoms of narcolepsy/cataplexy, hypophagia, hypoactivity, and late onset obesity (23, 42). Orexin/hypocretin neurons are most active during wakefulness and almost silent during slow-wave sleep (32, 52). Several lines of evidence indicate that the activity of orexins/hypocretin neurons promotes wakefulness, sympathetic outflow, exploratory locomotor activity, reward seeking, and food consumption (13, 14, 44, 53, 91, 97, 99, 100, 109). Interestingly, recent studies also suggest that underactivity and overactivity of the orexin/hypocretin system could be linked to depression and anxiety, respectively (16, 17, 47, 98).
Whole animal studies looking at genetic markers of neuronal activation and orexin/hypocretin mRNA expression following in vivo manipulation of glucose levels concluded that orexin/hypocretin neurons are activated by systemic hypoglycemia (22, 61, 86) and could thus be glucose inhibited, especially considering that they are not directly modulated by insulin (110). During initial cellular level investigations of the effects of glucose on rat LH neurons, it was found that orexin-A/hypocretin-1 was not present in glucose-inhibited neurons (55); and a more recent electrophysiological study also failed to elicit responses to glucose in rat orexin/hypocretin neurons (71). In contrast, at least three different groups independently reported acute inhibition of orexin/hypocretin neurons by glucose, using calcium imaging in rat orexin/hypocretin neurons (65), or whole cell patch-clamp recordings from isolated mouse orexin/hypocretin cells (110), or mouse orexin/hypocretin cells in brain slices (41, 108).
The published discrepancies in the ability of glucose to inhibit orexin/hypocretin neurons could, in theory, be related to species differences (more responsive in the mouse, less responsive in the rat), which remain to be investigated in detail. If the rat orexin/hypocretin neurons are not electrically responsive to glucose, as suggested by the data in Ref. 71, then the calcium imaging data, which do show glucose-induced drops in calcium concentration in ∼ 50% of rat orexin/hypocretin neurons (65), would suggest a possible dissociation between biochemical and electrical effects of glucose in these cells in the rat. As an alternative to the species differences explanation, the reported absence of acute glucose responses in orexin/hypocretin neurons in cytosol-sparing (cell-attached or perforated patch) recordings (71), but their presence in whole cell recordings (19, 110), could in theory be explained by a currently unidentified cytosolic factor, which suppresses the glucose-sensing ability of these cells in in vitro preparations, but whose influence is removed in the whole cell configuration due to the exchange of solution between the cytosol and the pipette in this recording mode.
The mechanism of glucose-induced inhibition of mouse orexin/hypocretin cells is not well understood but involves activation of background K+ channels (reviewed in Ref. 20). Interestingly, the glucose responses of orexin/hypocretin cells display a unique sugar selectivity, which suggests that the sensing pathway in orexin/hypocretin cells may be distinct from pathways involving glucose-binding proteins such as GLUT2, hSGLT3, and SGLT1 (39). The glucose responses of orexin/hypocretin neurons are also insensitive to glucokinase inhibitors and cannot be mimicked by the intracellular ATP or extracellular lactate, suggesting that they do not require conventional glucose-metabolizing machinery (39, 40).
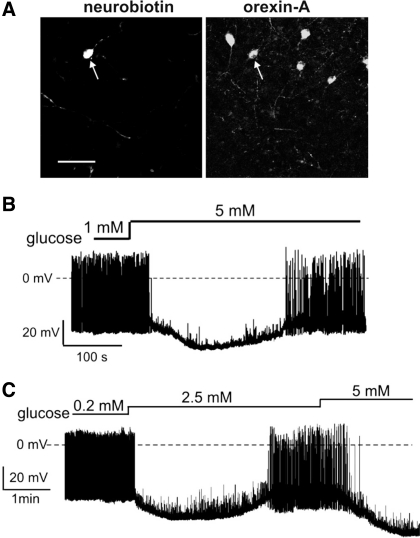
Interestingly, at physiological temperatures, ∼70% of orexin/hypocretin cells exhibit only transient, or adaptive, responses to sustained physiological rises in glucose levels (Fig. 1). Importantly, this allows orexin/hypocretin neurons to adjust their baseline potential to background glucose levels, and thus to continue to respond to changes in glucose levels independently of the glucose baseline (Fig. 1). We propose that, by analogy with classical sensory organs such as the eye, this adaptation allows orexin/hypocretin neurons to adjust their glucose sensitivity to background glucose levels (108). In other words, the glucose dose-response curve of orexin/hypocretin cells is not fixed, but can slide along the glucose concentration axis depending on the glucose baseline. Analysis of membrane currents and membrane resistance during the glucose adaptation response of orexin/hypocretin cells suggests that the cellular mechanism of this adaptation involves a time-dependent closure of the hyperpolarizing ion channels originally opened by glucose, rather than opening of an additional population of depolarizing channels (108). How these channels become less active with time after they are opened by glucose is currently unknown, but this process is highly temperature sensitive [very slow or undetectable at room temperature but prominent at 35°C (108)]. This steep temperature sensitivity is consistent with a process involving internalization/endocytosis of the glucose-activated channels and/or putative glucose receptors; this possibility, as well as alternative explanations (e.g., phosphorylation-induced desensitization), remain to be examined.
Fig. 1.
Adaptive glucose-sensing in orexin/hypocretin neurons. A: identification of an orexin/hypocretin neuron in a mouse brain slice by postrecording immunocytochemistry (left, orexin cell labelled with Neurobiotin is arrowed; right, the same arrowed cell is labelled with an orexin-A antibody). Scale bar = 50 μm; both images are shown at the same magnification. B: a mouse orexin/hypocretin cell is transiently inhibited by glucose but then adapts its membrane potential back to baseline despite the continuing presence of elevated glucose. C: this adaptation allows an orexin/hypocretin cell to respond to a second change in glucose levels. (Composited from Figs. 1, 4, and 5 of Ref. 108 with permission from Proc Natl Acad Sci USA).
Because orexin/hypocretin neurons are thought to stimulate wakefulness and signal reward deficiency, their inhibition by glucose may, in theory, be involved in anxiolytic, rewarding, and soporific effects of sugar ingestion (reviewed in Ref. 18), as well as in the regulation of blood glucose levels (see Hypothalmic Glucose-Sensing Neurons as Regulators of Peripheral Glucose Handling). In terms of arousal and reward, there is a theory that proposes a functional separation of the orexin/hypocretin system into a lateral population that regulates reward and a medial population that regulates arousal (43). At least in the mouse, inhibition of orexin/hypocretin cells by glucose does not appear to follow such a clear topographic separation; the glucose responses are observed in most if not all orexin/hypocretin cells across both lateral and medial parts of the lateral hypothalamic area, suggesting that glucose may affect both arousal and reward-related parts of the orexin/hypocretin system (108). However, analysis of the time course of glucose responses in mouse hypothalamus suggests that the medial group of orexin/hypocretin cells contains a greater proportion of adaptive orexin/hypocretin neurons than the lateral group (108). It is thus tempting to speculate that adaptive and nonadaptive glucose-sensing responses may be differentially involved in arousal or reward.
Another population of widely projecting lateral hypothalamic cells use the peptide transmitter melanin-concentrating hormone (MCH) (10). Although, like orexins/hypocretins, MCH is often considered an appetite-promoting transmitter, in many other respects the physiological roles of MCH neurons appear to be the opposite of those of orexin/hypocretin cells. In mice, knockout of MCH increases energy expenditure and reduces body weight (88), and these characteristics are also seen in animals lacking the MCH receptor -1 (MCH1R) (57). Central injection of MCH in rats increases the quantities of rapid eye movement and especially slow-wave sleep (106), while deletion of MCH or MCH1R in mice leads to increased wheel-running activity (115). These data suggest that endogenous MCH promotes sleep and suppresses locomotor activity and energy expenditure, i.e., the opposite of actions of orexins/hypocretins. It should be noted that, while MCH neurons are often referred to as appetite promoting, their role in the control of food intake is not entirely clear cut. For example, in mice, knockout of MCH increases food intake during the day but decreases it at night with the net daily result being a reduction in food intake (88). Although most (57, 78, 82), but not all (76), studies show that brain injections of MCH increase food intake, mice lacking the MCH receptor actually exhibited increased food intake (24, 57). Feeding-related effects of MCH thus appear to be complex, and may be influenced by its possible roles in anxiety and depression (15, 37). A closely related issue, which remains to be resolved, is whether MCH neurons are a functionally homogenous population or comprise subsets of cells with different profiles of ion channels and receptor expression and differential projection patterns, giving rise to several different behavioral roles, as recently proposed for orexin/hypocretin neurons (43).
Examination of the effects of changes in glucose on the electrical excitability of MCH neurones using whole cell recordings in mouse brain slices suggests that most MCH neurones are directly and dose-dependently depolarized and excited by glucose within the physiological concentration window (19). Based on the above-mentioned effects of MCH on locomotor activity and body energy balance, these data imply that glucose-induced excitation of MCH neurones may promote sleep and suppress energy expenditure. To the best of our knowledge, the glucose-sensing abilities of MCH neurons have not yet been examined in species other than mouse or with different recording techniques.
ARC of the hypothalamus.
This hypothalamic region is currently probably the best understood in terms of the control of appetite and metabolism. The generally accepted model is that the ARC of the hypothalamus, neuropeptide Y (NPY) neurons promote weight gain by stimulating appetite and suppressing energy expenditure, whereas ARC proopiomelanocortin (POMC) neurones cause weight loss by inhibiting feeding and stimulating energy expenditure (26, 87). A key feature of this model is that NPY and POMC neurons are oppositely regulated by signals of body energy status, such as leptin (26–28, 87, 105). Whether the NPY and POMC neatly correspond to glucose-inhibited and glucose-excited neurons, respectively, which would fit in nicely into the above model, is still debated. For example, Muroya et al. (66) concluded that 94% of ARC cells that decreased their calcium levels in response to glucose were immunoreactive for NPY. Whole cell patch-clamp recordings also indicated that a significant proportion (40%) of NPY neurons are glucose inhibited (34). But, in contrast, perforated patch recordings of Claret et al. (25) failed to show inhibitory effects of glucose on NPY cells. These discrepancies appear to show a similar methodology correlation to discrepancies in the studies of orexin/hypocretin neurons noted above: in both NPY and orexin/hypocretin cells, glucose-induced inhibition appears to be readily observed in whole cell recordings but, paradoxically, not in the less invasive perforated patch recordings. Interestingly, for arcuate glucose-excited POMC neurons, the differences in the literature appear to follow the opposite methodology correlation. Specifically, Fioramonti et al. (34) did not observe any glucose responses in most POMC neurons when using the cytosol-disrupting whole cell recordings. In contrast, using the cytosol-preserving loose patch or perforated patch recordings shows that the majority of POMC neurons are excited by glucose in the physiological concentration range (25, 46, 72). We would like to propose that the operation of glucose-excited neurons requires a highly diffusible cytosolic messenger [presumably ATP (59), but see Ref. 2] and can thus be particularly easily disrupted especially in small cells by experimental techniques that wash out the cytosol (such as the whole cell recording with large-tipped pipettes). In contrast, glucose-inhibited neurons use a completely different (but as yet undetermined) intracellular signaling pathway (see Refs. 39 and 40), and we would like to speculate that this pathway is boosted in whole cell recordings, possibly due to diffusion of a suppressor substance(s) away from cytosol into the pipette.
Ventromedial nucleus of the hypothalamus.
This hypothalamic area is probably the most studied in terms of brain glucose sensing and has long been known to contain both glucose-excited and glucose-inhibited neurons. However, in terms of neurochemistry of glucose sensing, the ventromedial nucleus of the hypothalamus (VMH) is currently understood much less than the ARC and LH. Single cell gene expression analysis suggests that some VMH neurons, including glucose-excited cells, are GABAergic; however, the GABAergic marker GAD is not expressed in a clear relationship to glucose-sensing capacity (49, 59). Recent data show that most VMH neurons express a protein called steroidogenic factor-1 (SF-1) and that SF-1-expressing neurons have key roles in glucose homeostasis (103, 114). However, how SF-1 expression relates to glucose-excited and glucose-inhibited neurons of the VMH is currently unclear, although there is some interesting recent data that indirectly suggest that some of the glucose-inhibited VMH neurons may express SF-1 and glutamate (see discussion at the end of Hypothalmic Glucose-sensing Neurons as Regulators of Peripheral Glucose Handling). Perhaps the most critical issue to resolve here is how gene expression and glucose-sensing identities of VMH neurons relate to their projection targets, since there is emerging evidence that different subregions of the VMH are differentially connected to other key feeding centers, such as the ARC (96).
Need for Better Functional and Molecular Markers of Glucose Sensing
After glucose sensing has been linked to specific populations of vital neurons described above, more and more researchers have moved into this field, creating an increasing demand for clear criteria for classifying neurons as glucose excited and glucose inhibited. In terms of functional experiments, a key source of uncertainty stems from the fact that glucose is used as an energy fuel by all neurons, either directly or indirectly by stimulating lactate production by astrocytes (71, 73). Thus, experimental alterations of glucose levels can often elicit general energy-related and/or neuroprotective responses that are unrelated to specific glucose sensing. An example of this is silencing of neurons by very low glucose, which is a widespread response found in both glucose-sensing and non-glucose-sensing neurons and often involving neuroprotective opening of ATP-inhibited K (KATP) channels, and consequent hyperpolarization, induced by the fall in glucose (and thus cytosolic ATP) levels (9, 60). Although in glucose-excited neurons the hyperpolarization induced by 0 mM glucose is likely to be much faster than in non-glucose-sensing neurons, and thus the speed of hyperpolarization has been used by some researchers to identify glucose-sensing cells, this criterion can be very sensitive to experimental variables such as location of cells in the recording chamber and in the tissue (for brain slice recording). For these reasons, a more robust, and more physiological, criterion for classifying a glucose-excited neuron as glucose sensing would perhaps be a test of whether its firing can be significantly affected by changes in extracellular glucose in the physiological glucose range in the brain, e.g., 1 to 2.5 mM (83), although there is currently no agreement on how large the effects on firing should be to pass this qualifying test. As mentioned in the introduction, the functional definition of glucose-inhibited neurons is much more clear, because their membrane potential responses to glucose occur in the opposite direction (hyperpolarization) from the general energy-related effects of glucose (depolarization).
In terms of molecular definitions of brain glucose-sensing cells, no molecules unique to glucose-sensing cells have yet been identified. Several markers of glucose-sensing ability have been proposed, including KATP channels, glucokinase, AMP kinase, and the GLUT2 transporter (25, 101, 111), but the correlation between the expression of these proteins and the brain locations of glucose-sensing neurons is imperfect (5, 49, 50). For glucose-inhibited neurons, the need for molecular markers is particularly critical since even the final effector channels remain to be defined in exact molecular detail (20). It is probably accurate to say that it is currently unknown exactly what makes glucose-sensing neurons distinct from other neurons at the molecular level.
Hypothalamic Glucose-Sensing Neurons as Regulators of Peripheral Glucose Handling
Although ARC neurons send signals to key central and peripheral regulators of energy balance (95, 62), the roles of glucose sensing in the POMC and NPY cells in glucose homeostasis remain somewhat unclear, despite recent attempts to inactivate NPY/POMC glucosensing through targeted genetic manipulations [(25, 72), but see discussion in Refs. 54 and 40]. In orexin/hypocretin and MCH neurons, an equivalent analysis has not been performed due to the lack of knowledge of molecular components of glucose sensing in these cells (19, 20, 38). However, the original study by Yamanaka et al. (110) that described the intrinsic inhibitory responses of orexin/hypocretin cells to glucose also observed a lack of fasting-induced stimulation of arousal in mice lacking orexins/hypocretins, suggesting that disinhibition of orexin/hypocretin cells by falling glucose may have a role in the initiation of foraging. In this section, we will not discuss the involvement of glucose-sensing neurons in behavior and higher brain function further but instead discuss recent findings on their interactions with peripheral tissues relevant to glucose homeostasis, focusing in particular on recent work on control of glucose homeostasis by LH orexin/hypocretin neurons and VMH SF-1 neurons.
As reviewed in Refs. 33 and 104, orexin/hypocretin neurons can control basal metabolic rate in addition to alertness and reward seeking. Intracerebroventricular administration of orexin-A/hypocretin-1 increases energy expenditure even in anaesthetized rats (107). A number of experiments (4, 89) showed that intracerebroventricular or intrathecal administration of orexin/hypocretin stimulates sympathetic outflow and increases plasma epinephrine and norepinephrine levels. Anatomical data employing pseudorabies virus transsynaptic tract tracing (36, 51, 95) or electron microscopy and cholera toxin B subunit tracing (56), show that orexin/hypocretin cells project polysynaptically to various sympathetic outflow systems. Two recent papers have demonstrated the potential physiological significance of these findings in relation to glucose homeostasis.
The data of Yi et al. (112) suggested that orexin/hypocretin neurons, especially those in the perifornical area, can stimulate endogenous glucose production and increase blood glucose through sympathetic nervous control. They retrodialyzed bicuculline into the LH and found that orexin/hypocretin neurons were specifically activated in the perifornical area. This led to stimulation of hepatic glucose production, which was inhibited by intracerebroventricular pretreatment with an orexin/hypocretin receptor antagonist. An increase in endogenous glucose production was also induced by intracerebroventricular injection of orexin-A/hypocretin-1, and this increase was inhibited by hepatic sympathetic denervation.
On the other hand, Shiuchi et al. (90) found no change in blood glucose, but increase in glucose turnover rate, upon direct infusion of orexin-A/hypocretin-1 into the medial hypothalamus. This was interpreted as simultaneous increase in glucose utilization and production, since it was also observed that glucose uptake by muscle was increased. Orexins/hypocretins promoted glucose uptake and insulin-dependent glycogen synthesis in skeletal muscle by a mechanism involving β2-adrenoreceptors on non-myocyte cells of skeletal muscle, suggesting that orexin/hypocretin cells could activate this mechanism through sympathetic nerves.
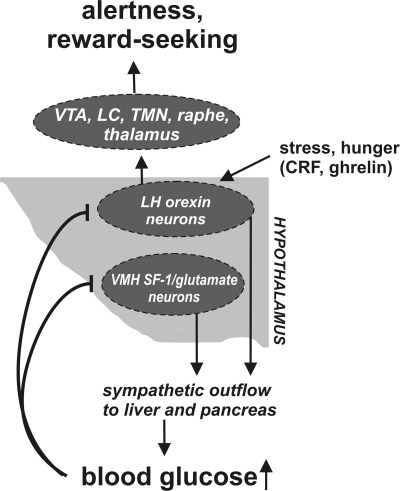
Based on these studies, it can be concluded that at least some of the orexin/hypocretin neurons control key peripheral mediators of glucose homeostasis via the sympathetic nerves. It remains to be examined whether some subsets of orexin/hypocretin neurons [for example, medial vs. lateral (43)] are more important for this. We propose that these findings (90, 112) could mean that the activity of orexin/hypocretin neurons promotes shuttling of glucose from liver to muscle, as would be useful in foraging that is thought to be stimulated by the orexin/hypocretin system (110). Thus, it is possible that the glucose inhibition of orexin/hypocretin cells provides negative feedback in a circuit that consists of orexin/hypocretin cells, sympathetic nerves, the pancreas, and the liver (Fig. 2). Since MCH cells decrease heart rate and thermogenesis via the sympathetic nervous system (8) and glucose increases their activity (19), they might also be involved in this putative feedback loop. It is noteworthy that MCH neurons also project polysynaptically via the sympathetic ganglia to the adrenal medulla, white and brown adipose tissue, and the liver (51, 68, 95). However, to the best of our knowledge, it is not yet known whether MCH neuron activity increases or decreases sympathetic outflow to these organs.
Fig. 2.
Hypothetical model integrating the physiological roles of glucose-inhibited lateral hypothalamus (LH) and ventromedial hypothalamus (VMH) neurons (see text for details). Arrows indicate stimulation (or increased levels), t-bars show inhibition. VTA, ventral tegmental area; LC, locus coeruleus; TMN, hypothalamic tuberomammillary nucleus; CRF, corticotropin-releasing factor; SF-1 steroidogenic factor-1.
The VMH is especially important for the counterregulatory response (84). Local glucoprivation in the VMH results in pancreatic glucagon secretion (12) and glucose infusion into the VMH suppresses glucagon secretion in response to falling blood glucose (11). In turn, the blunting of the counterregulatory response by repetitive hypoglycemia is associated with an impairment of glucosensing in VMH glucose-inhibited neurons (94). Although the precise cellular mechanisms of the counterregulatory response are not fully understood, and other factors, such as glucosensors in the portal vein, play a critical role (45), these data suggest that, like the orexin/hypocretin neurons, the VMH glucose-sensing neurons may control sympathetic outflow. As the glucose-sensing VMH cells are not currently neurochemically identified, it is not yet straightforward to demonstrate a connection to sympathetic innervation targets by tracing techniques. However, some hypotheses can be formulated from data looking at the expression of GAD-67 (glutamic acid decarboxylase, a GABAergic marker) in VMH neurons that are likely to be glucose excited (59) and experiments looking at systemic effects of inactivation of glutamate release from VMH SF-1 neurons (103). The former study suggests that VMH glucose-excited neurons are GABAergic, whereas the latter shows that the counterregulatory release of glucagon upon fasting, which is stimulated by the sympathetic system, requires glutamate release from VMH SF-1 neurons. Therefore, we hypothesize that glucose-inhibited VMH neurons that increase sympathetic outflow and control glucagon secretion are glutamatergic (Fig. 2), whereas at least some of VMH glucose-excited neurons are GABAergic [in line with the recent demonstration that glucose stimulates GABA release in the VMH, (116)].
Perspectives and Significance
Many glucose-sensing neurons of the hypothalamus have now been assigned neurochemical identities and are beginning to be linked to specific higher and lower functions of the nervous system (Fig. 2). Most, if not all, of the glucose-sensing neurons of the hypothalamus are well placed to affect peripheral glucose utilization in liver, muscle, and adipose tissue through the autonomic nervous system (Fig. 2). This might give a general rationale for their ability to sense changes in glucose levels as a feedback regulation of their control of these organs. Our hypothesis would predict that glucose-excited neurons inhibit sympathetic input to key peripheral regulators of glucose homeostasis, whereas glucose-inhibited neurons would stimulate it. It remains a challenge to find molecular markers and mechanisms that are unique to glucose-sensing cells. In our view, this is one of the key current obstacles in assessing the relative importance of the multiple circuits involved in hypothalamic glucose sensing and in investigating how specific features of brain glucose-sensing cells, such as its adaptive time course in some neurons (Fig. 1), relate to the regulation of glucose homeostasis and behavior.
GRANTS
Work in the authors' laboratory has been funded by the European Research Council (FP7). M. Karnani was also supported by the Osk. Huttunen Foundation.
DISCLOSURES
No conflicts of interest, financial or otherwise, are declared by the author(s).
REFERENCES
- 1. Adachi A, Kobashi M, Funahashi M. Glucose-responsive neurons in the brainstem. Obes Res 3, Suppl 5: 735S–740S, 1995 [DOI] [PubMed] [Google Scholar]
- 2. Ainscow EK, Mirshamsi S, Tang T, Ashford ML, Rutter GA. Dynamic imaging of free cytosolic ATP concentration during fuel sensing by rat hypothalamic neurones: evidence for ATP-independent control of ATP-sensitive K+ channels. J Physiol 544: 429–445, 2002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Anand BK, Chhina GS, Sharma KN, Dua S, Singh B. Activity of single neurons in the hypothalamic feeding centers: effect of glucose. Am J Physiol 207: 1146–1154, 1964 [DOI] [PubMed] [Google Scholar]
- 4. Antunes VR, Brailoiu GC, Kwok EH, Scruggs P, Dun NJ. Orexins/hypocretins excite rat sympathetic preganglionic neurons in vivo and in vitro. Am J Physiol Regul Integr Comp Physiol 281: R1801–R1807, 2001 [DOI] [PubMed] [Google Scholar]
- 5. Arluison M, Quignon M, Nguyen P, Thorens B, Leloup C, Penicaud L. Distribution and anatomical localization of the glucose transporter 2 (GLUT2) in the adult rat brain–an immunohistochemical study. J Chem Neuroanat 28: 117–136, 2004 [DOI] [PubMed] [Google Scholar]
- 6. Ashcroft FM. KATP channels and insulin secretion: a key role in health and disease. Biochem Soc Trans 34: 243–246, 2006 [DOI] [PubMed] [Google Scholar]
- 7. Ashcroft FM, Rorsman P. Electrophysiology of the pancreatic β-cell. Prog Biophys Mol Biol 54: 87–143, 1989 [DOI] [PubMed] [Google Scholar]
- 8. Astrand A, Bohlooly YM, Larsdotter S, Mahlapuu M, Andersen H, Tornell J, Ohlsson C, Snaith M, Morgan DG. Mice lacking melanin-concentrating hormone receptor 1 demonstrate increased heart rate associated with altered autonomic activity. Am J Physiol Regul Integr Comp Physiol 287: R749–R758, 2004 [DOI] [PubMed] [Google Scholar]
- 9. Ballanyi K. Protective role of neuronal KATP channels in brain hypoxia. J Exp Biol 207: 3201–3212, 2004 [DOI] [PubMed] [Google Scholar]
- 10. Bittencourt JC, Presse F, Arias C, Peto C, Vaughan J, Nahon JL, Vale W, Sawchenko PE. The melanin-concentrating hormone system of the rat brain: an immuno- and hybridization histochemical characterization. J Comp Neurol 319: 218–245, 1992 [DOI] [PubMed] [Google Scholar]
- 11. Borg MA, Sherwin RS, Borg WP, Tamborlane WV, Shulman GI. Local ventromedial hypothalamus glucose perfusion blocks counterregulation during systemic hypoglycemia in awake rats. J Clin Invest 99: 361–365, 1997 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Borg WP, Sherwin RS, During MJ, Borg MA, Shulman GI. Local ventromedial hypothalamus glucopenia triggers counterregulatory hormone release. Diabetes 44: 180–184, 1995 [DOI] [PubMed] [Google Scholar]
- 13. Borgland SL, Chang SJ, Bowers MS, Thompson JL, Vittoz N, Floresco SB, Chou J, Chen BT, Bonci A. Orexin A/hypocretin-1 selectively promotes motivation for positive reinforcers. J Neurosci 29: 11215–11225, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Borgland SL, Taha SA, Sarti F, Fields HL, Bonci A. Orexin A in the VTA is critical for the induction of synaptic plasticity and behavioral sensitization to cocaine. Neuron 49: 589–601, 2006 [DOI] [PubMed] [Google Scholar]
- 15. Borowsky B, Durkin MM, Ogozalek K, Marzabadi MR, DeLeon J, Lagu B, Heurich R, Lichtblau H, Shaposhnik Z, Daniewska I, Blackburn TP, Branchek TA, Gerald C, Vaysse PJ, Forray C. Antidepressant, anxiolytic and anorectic effects of a melanin-concentrating hormone-1 receptor antagonist. Nat Med 8: 825–830, 2002 [DOI] [PubMed] [Google Scholar]
- 16. Boutrel B, Kenny PJ, Specio SE, Martin-Fardon R, Markou A, Koob GF, de Lecea L. Role for hypocretin in mediating stress-induced reinstatement of cocaine-seeking behavior. Proc Natl Acad Sci USA 102: 19168–19173, 2005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Brundin L, Bjorkqvist M, Petersen A, Traskman-Bendz L. Reduced orexin levels in the cerebrospinal fluid of suicidal patients with major depressive disorder. Eur Neuropsychopharmacol 17: 573–579, 2007 [DOI] [PubMed] [Google Scholar]
- 18. Burdakov D. K+ channels stimulated by glucose: a new energy-sensing pathway. Pflügers Arch 454: 19–27, 2007 [DOI] [PubMed] [Google Scholar]
- 19. Burdakov D, Gerasimenko O, Verkhratsky A. Physiological changes in glucose differentially modulate the excitability of hypothalamic melanin-concentrating hormone and orexin neurons in situ. J Neurosci 25: 2429–2433, 2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Burdakov D, Lesage F. Glucose-induced inhibition: how many ionic mechanisms? Acta Physiol (Oxf), 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Burdakov D, Luckman SM, Verkhratsky A. Glucose-sensing neurons of the hypothalamus. Philos Trans R Soc Lond B Biol Sci 360: 2227–2235, 2005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Cai XJ, Evans ML, Lister CA, Leslie RA, Arch JR, Wilson S, Williams G. Hypoglycemia activates orexin neurons and selectively increases hypothalamic orexin-B levels: responses inhibited by feeding and possibly mediated by the nucleus of the solitary tract. Diabetes 50: 105–112, 2001 [DOI] [PubMed] [Google Scholar]
- 23. Chemelli RM, Willie JT, Sinton CM, Elmquist JK, Scammell T, Lee C, Richardson JA, Williams SC, Xiong Y, Kisanuki Y, Fitch TE, Nakazato M, Hammer RE, Saper CB, Yanagisawa M. Narcolepsy in orexin knockout mice: molecular genetics of sleep regulation. Cell 98: 437–451, 1999 [DOI] [PubMed] [Google Scholar]
- 24. Chen Y, Hu C, Hsu CK, Zhang Q, Bi C, Asnicar M, Hsiung HM, Fox N, Slieker LJ, Yang DD, Heiman ML, Shi Y. Targeted disruption of the melanin-concentrating hormone receptor-1 results in hyperphagia and resistance to diet-induced obesity. Endocrinology 143: 2469–2477, 2002 [DOI] [PubMed] [Google Scholar]
- 25. Claret M, Smith MA, Batterham RL, Selman C, Choudhury AI, Fryer LG, Clements M, Al-Qassab H, Heffron H, Xu AW, Speakman JR, Barsh GS, Viollet B, Vaulont S, Ashford ML, Carling D, Withers DJ. AMPK is essential for energy homeostasis regulation and glucose sensing by POMC and AgRP neurons. J Clin Invest 117: 2325–2336, 2007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Cone RD, Cowley MA, Butler AA, Fan W, Marks DL, Low MJ. The arcuate nucleus as a conduit for diverse signals relevant to energy homeostasis. Int J Obes Relat Metab Disord 25, Suppl 5: S63–S67, 2001 [DOI] [PubMed] [Google Scholar]
- 27. Cowley MA, Smart JL, Rubinstein M, Cerdan MG, Diano S, Horvath TL, Cone RD, Low MJ. Leptin activates anorexigenic POMC neurons through a neural network in the arcuate nucleus. Nature 411: 480–484, 2001 [DOI] [PubMed] [Google Scholar]
- 28. Cowley MA, Smith RG, Diano S, Tschop M, Pronchuk N, Grove KL, Strasburger CJ, Bidlingmaier M, Esterman M, Heiman ML, Garcia-Segura LM, Nillni EA, Mendez P, Low MJ, Sotonyi P, Friedman JM, Liu H, Pinto S, Colmers WF, Cone RD, Horvath TL. The distribution and mechanism of action of ghrelin in the CNS demonstrates a novel hypothalamic circuit regulating energy homeostasis. Neuron 37: 649–661, 2003 [DOI] [PubMed] [Google Scholar]
- 29. de Lecea L, Kilduff TS, Peyron C, Gao X, Foye PE, Danielson PE, Fukuhara C, Battenberg EL, Gautvik VT, Bartlett FS, Frankel WN, II, van den Pol AN, Bloom FE, Gautvik KM, Sutcliffe JG. The hypocretins: hypothalamus-specific peptides with neuroexcitatory activity. Proc Natl Acad Sci USA 95: 322–327, 1998 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Dunn-Meynell AA, Routh VH, Kang L, Gaspers L, Levin BE. Glucokinase is the likely mediator of glucosensing in both glucose-excited and glucose-inhibited central neurons. Diabetes 51: 2056–2065, 2002 [DOI] [PubMed] [Google Scholar]
- 31. Dunn-Meynell AA, Sanders NM, Compton D, Becker TC, Eiki J, Zhang BB, Levin BE. Relationship among brain and blood glucose levels and spontaneous and glucoprivic feeding. J Neurosci 29: 7015–7022, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Estabrooke IV, McCarthy MT, Ko E, Chou TC, Chemelli RM, Yanagisawa M, Saper CB, Scammell TE. Fos expression in orexin neurons varies with behavioral state. J Neurosci 21: 1656–1662, 2001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Ferguson AV, Samson WK. The orexin/hypocretin system: a critical regulator of neuroendocrine and autonomic function. Front Neuroendocrinol 24: 141–150, 2003 [DOI] [PubMed] [Google Scholar]
- 34. Fioramonti X, Contie S, Song Z, Routh VH, Lorsignol A, Penicaud L. Characterization of glucosensing neuron subpopulations in the arcuate nucleus: integration in neuropeptide Y and pro-opio melanocortin networks? Diabetes 56: 1219–1227, 2007 [DOI] [PubMed] [Google Scholar]
- 35. Ganong WF. Circumventricular organs: definition and role in the regulation of endocrine and autonomic function. Clin Exp Pharmacol Physiol 27: 422–427, 2000 [DOI] [PubMed] [Google Scholar]
- 36. Geerling JC, Mettenleiter TC, Loewy AD. Orexin neurons project to diverse sympathetic outflow systems. Neuroscience 122: 541–550, 2003 [DOI] [PubMed] [Google Scholar]
- 37. Georgescu D, Sears RM, Hommel JD, Barrot M, Bolanos CA, Marsh DJ, Bednarek MA, Bibb JA, Maratos-Flier E, Nestler EJ, DiLeone RJ. The hypothalamic neuropeptide melanin-concentrating hormone acts in the nucleus accumbens to modulate feeding behavior and forced-swim performance. J Neurosci 25: 2933–2940, 2005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Gonzalez JA, Jensen LT, Doyle SE, Miranda-Anaya M, Menaker M, Fugger L, Bayliss DA, Burdakov D. Deletion of TASK1 and TASK3 channels disrupts intrinsic excitability but does not abolish glucose or pH responses of orexin/hypocretin neurons. Eur J Neurosci 30: 57–64, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Gonzalez JA, Jensen LT, Fugger L, Burdakov D. Metabolism-independent sugar sensing in central orexin neurons. Diabetes 57: 2569–2576, 2008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Gonzalez JA, Reimann F, Burdakov D. Dissociation between sensing and metabolism of glucose in sugar sensing neurones. J Physiol 587: 41–48, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Guyon A, Tardy MP, Rovere C, Nahon JL, Barhanin J, Lesage F. Glucose inhibition persists in hypothalamic neurons lacking tandem-pore K+ channels. J Neurosci 29: 2528–2533, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Hara J, Beuckmann CT, Nambu T, Willie JT, Chemelli RM, Sinton CM, Sugiyama F, Yagami K, Goto K, Yanagisawa M, Sakurai T. Genetic ablation of orexin neurons in mice results in narcolepsy, hypophagia, and obesity. Neuron 30: 345–354, 2001 [DOI] [PubMed] [Google Scholar]
- 43. Harris GC, Aston-Jones G. Arousal and reward: a dichotomy in orexin function. Trends Neurosci 29: 571–577, 2006 [DOI] [PubMed] [Google Scholar]
- 44. Harris GC, Wimmer M, Aston-Jones G. A role for lateral hypothalamic orexin neurons in reward seeking. Nature 437: 556–559, 2005 [DOI] [PubMed] [Google Scholar]
- 45. Hevener AL, Bergman RN, Donovan CM. Portal vein afferents are critical for the sympathoadrenal response to hypoglycemia. Diabetes 49: 8–12, 2000 [DOI] [PubMed] [Google Scholar]
- 46. Ibrahim N, Bosch MA, Smart JL, Qiu J, Rubinstein M, Ronnekleiv OK, Low MJ, Kelly MJ. Hypothalamic proopiomelanocortin neurons are glucose responsive and express KATP channels. Endocrinology 144: 1331–1340, 2003 [DOI] [PubMed] [Google Scholar]
- 47. Ito N, Yabe T, Gamo Y, Nagai T, Oikawa T, Yamada H, Hanawa T. Icv administration of orexin-A induces an antidepressive-like effect through hippocampal cell proliferation. Neuroscience 157: 720–732, 2008 [DOI] [PubMed] [Google Scholar]
- 48. Jenkins DJ, Wolever TM, Taylor RH, Barker H, Fielden H, Baldwin JM, Bowling AC, Newman HC, Jenkins AL, Goff DV. Glycemic index of foods: a physiological basis for carbohydrate exchange. Am J Clin Nutr 34: 362–366, 1981 [DOI] [PubMed] [Google Scholar]
- 49. Kang L, Routh VH, Kuzhikandathil EV, Gaspers LD, Levin BE. Physiological and molecular characteristics of rat hypothalamic ventromedial nucleus glucosensing neurons. Diabetes 53: 549–559, 2004 [DOI] [PubMed] [Google Scholar]
- 50. Karschin C, Ecke C, Ashcroft FM, Karschin A. Overlapping distribution of KATP channel-forming Kir6.2 subunit and the sulfonylurea receptor SUR1 in rodent brain. FEBS Lett 401: 59–64, 1997 [DOI] [PubMed] [Google Scholar]
- 51. Kerman IA, Bernard R, Rosenthal D, Beals J, Akil H, Watson SJ. Distinct populations of presympathetic-premotor neurons express orexin or melanin-concentrating hormone in the rat lateral hypothalamus. J Comp Neurol 505: 586–601, 2007 [DOI] [PubMed] [Google Scholar]
- 52. Kiyashchenko LI, Mileykovskiy BY, Maidment N, Lam HA, Wu MF, John J, Peever J, Siegel JM. Release of hypocretin (orexin) during waking and sleep states. J Neurosci 22: 5282–5286, 2002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Lawrence AJ, Cowen MS, Yang HJ, Chen F, Oldfield B. The orexin system regulates alcohol-seeking in rats. Br J Pharmacol 148: 752–759, 2006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Levin BE. Neuronal glucose sensing: still a physiological orphan? Cell Metab 6: 252–254, 2007 [DOI] [PubMed] [Google Scholar]
- 55. Liu XH, Morris R, Spiller D, White M, Williams G. Orexin a preferentially excites glucose-sensitive neurons in the lateral hypothalamus of the rat in vitro. Diabetes 50: 2431–2437, 2001 [DOI] [PubMed] [Google Scholar]
- 56. Llewellyn-Smith IJ, Martin CL, Marcus JN, Yanagisawa M, Minson JB, Scammell TE. Orexin-immunoreactive inputs to rat sympathetic preganglionic neurons. Neurosci Lett 351: 115–119, 2003 [DOI] [PubMed] [Google Scholar]
- 57. Marsh DJ, Weingarth DT, Novi DE, Chen HY, Trumbauer ME, Chen AS, Guan XM, Jiang MM, Feng Y, Camacho RE, Shen Z, Frazier EG, Yu H, Metzger JM, Kuca SJ, Shearman LP, Gopal-Truter S, MacNeil DJ, Strack AM, MacIntyre DE, Van der Ploeg LH, Qian S. Melanin-concentrating hormone 1 receptor-deficient mice are lean, hyperactive, and hyperphagic and have altered metabolism. Proc Natl Acad Sci USA 99: 3240–3245, 2002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Marty N, Dallaporta M, Thorens B. Brain glucose sensing, counterregulation, and energy homeostasis. Physiology (Bethesda) 22: 241–251, 2007 [DOI] [PubMed] [Google Scholar]
- 59. Miki T, Liss B, Minami K, Shiuchi T, Saraya A, Kashima Y, Horiuchi M, Ashcroft F, Minokoshi Y, Roeper J, Seino S. ATP-sensitive K+ channels in the hypothalamus are essential for the maintenance of glucose homeostasis. Nat Neurosci 4: 507–512, 2001 [DOI] [PubMed] [Google Scholar]
- 60. Mobbs CV, Kow LM, Yang XJ. Brain glucose-sensing mechanisms: ubiquitous silencing by aglycemia vs. hypothalamic neuroendocrine responses. Am J Physiol Endocrinol Metab 281: E649–E654, 2001 [DOI] [PubMed] [Google Scholar]
- 61. Moriguchi T, Sakurai T, Nambu T, Yanagisawa M, Goto K. Neurons containing orexin in the lateral hypothalamic area of the adult rat brain are activated by insulin-induced acute hypoglycemia. Neurosci Lett 264: 101–104, 1999 [DOI] [PubMed] [Google Scholar]
- 62. Morton GJ, Cummings DE, Baskin DG, Barsh GS, Schwartz MW. Central nervous system control of food intake and body weight. Nature 443: 289–295, 2006 [DOI] [PubMed] [Google Scholar]
- 63. Mountjoy PD, Rutter GA. Glucose sensing by hypothalamic neurones and pancreatic islet cells: AMPle evidence for common mechanisms? Exp Physiol 92: 311–319, 2007 [DOI] [PubMed] [Google Scholar]
- 64. Mullier A, Bouret SG, Prevot V, Dehouck B. Differential distribution of tight junction proteins suggests a role for tanycytes in blood-hypothalamus barrier regulation in the adult mouse brain. J Comp Neurol 518: 943–962, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. Muroya S, Uramura K, Sakurai T, Takigawa M, Yada T. Lowering glucose concentrations increases cytosolic Ca2+ in orexin neurons of the rat lateral hypothalamus. Neurosci Lett 309: 165–168, 2001 [DOI] [PubMed] [Google Scholar]
- 66. Muroya S, Yada T, Shioda S, Takigawa M. Glucose-sensitive neurons in the rat arcuate nucleus contain neuropeptide Y. Neurosci Lett 264: 113–116, 1999 [DOI] [PubMed] [Google Scholar]
- 67. Nonogaki K. New insights into sympathetic regulation of glucose and fat metabolism. Diabetologia 43: 533–549, 2000 [DOI] [PubMed] [Google Scholar]
- 68. Oldfield BJ, Giles ME, Watson A, Anderson C, Colvill LM, McKinley MJ. The neurochemical characterisation of hypothalamic pathways projecting polysynaptically to brown adipose tissue in the rat. Neuroscience 110: 515–526, 2002 [DOI] [PubMed] [Google Scholar]
- 69. Oomura Y, Ono T, Ooyama H, Wayner MJ. Glucose and osmosensitive neurones of the rat hypothalamus. Nature 222: 282–284, 1969 [DOI] [PubMed] [Google Scholar]
- 70. Oomura Y, Ooyama H, Sugimori M, Nakamura T, Yamada Y. Glucose inhibition of the glucose-sensitive neurone in the rat lateral hypothalamus. Nature 247: 284–286, 1974 [DOI] [PubMed] [Google Scholar]
- 71. Parsons MP, Hirasawa M. ATP-sensitive potassium channel-mediated lactate effect on orexin neurons: implications for brain energetics during arousal. J Neurosci 30: 8061–8070, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72. Parton LE, Ye CP, Coppari R, Enriori PJ, Choi B, Zhang CY, Xu C, Vianna CR, Balthasar N, Lee CE, Elmquist JK, Cowley MA, Lowell BB. Glucose sensing by POMC neurons regulates glucose homeostasis and is impaired in obesity. Nature 449: 228–232, 2007 [DOI] [PubMed] [Google Scholar]
- 73. Pellerin L. How astrocytes feed hungry neurons. Mol Neurobiol 32: 59–72, 2005 [DOI] [PubMed] [Google Scholar]
- 74. Peruzzo B, Pastor FE, Blazquez JL, Schobitz K, Pelaez B, Amat P, Rodriguez EM. A second look at the barriers of the medial basal hypothalamus. Exp Brain Res 132: 10–26, 2000 [DOI] [PubMed] [Google Scholar]
- 75. Peyron C, Tighe DK, van den Pol AN, de Lecea L, Heller HC, Sutcliffe JG, Kilduff TS. Neurons containing hypocretin (orexin) project to multiple neuronal systems. J Neurosci 18: 9996–10015, 1998 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76. Presse F, Sorokovsky I, Max JP, Nicolaidis S, Nahon JL. Melanin-concentrating hormone is a potent anorectic peptide regulated by food-deprivation and glucopenia in the rat. Neuroscience 71: 735–745, 1996 [DOI] [PubMed] [Google Scholar]
- 77. Puschel GP. Control of hepatocyte metabolism by sympathetic and parasympathetic hepatic nerves. Anat Rec A Discov Mol Cell Evol Biol 280: 854–867, 2004 [DOI] [PubMed] [Google Scholar]
- 78. Qu D, Ludwig DS, Gammeltoft S, Piper M, Pelleymounter MA, Cullen MJ, Mathes WF, Przypek R, Kanarek R, Maratos-Flier E. A role for melanin-concentrating hormone in the central regulation of feeding behaviour. Nature 380: 243–247, 1996 [DOI] [PubMed] [Google Scholar]
- 79. Reimann F, Habib AM, Tolhurst G, Parker HE, Rogers GJ, Gribble FM. Glucose sensing in L cells: a primary cell study. Cell Metab 8: 532–539, 2008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80. Ritter RC, Slusser PG, Stone S. Glucoreceptors controlling feeding and blood glucose: location in the hindbrain. Science 213: 451–452, 1981 [DOI] [PubMed] [Google Scholar]
- 81. Rorsman P, Salehi SA, Abdulkader F, Braun M, MacDonald PE. KATP-channels and glucose-regulated glucagon secretion. Trends Endocrinol Metab 19: 277–284, 2008 [DOI] [PubMed] [Google Scholar]
- 82. Rossi M, Choi SJ, O'Shea D, Miyoshi T, Ghatei MA, Bloom SR. Melanin-concentrating hormone acutely stimulates feeding, but chronic administration has no effect on body weight. Endocrinology 138: 351–355, 1997 [DOI] [PubMed] [Google Scholar]
- 83. Routh VH. Glucose-sensing neurons: are they physiologically relevant? Physiol Behav 76: 403–413, 2002 [DOI] [PubMed] [Google Scholar]
- 84. Routh VH. Glucosensing neurons in the ventromedial hypothalamic nucleus (VMN) and hypoglycemia-associated autonomic failure (HAAF). Diabetes Metab Res Rev 19: 348–356, 2003 [DOI] [PubMed] [Google Scholar]
- 85. Routh VH, Song Z, Liu X. The role of glucosensing neurons in the detection of hypoglycemia. Diabetes Technol Ther 6: 413–421, 2004 [DOI] [PubMed] [Google Scholar]
- 86. Sakurai T, Amemiya A, Ishii M, Matsuzaki I, Chemelli RM, Tanaka H, Williams SC, Richardson JA, Kozlowski GP, Wilson S, Arch JR, Buckingham RE, Haynes AC, Carr SA, Annan RS, McNulty DE, Liu WS, Terrett JA, Elshourbagy NA, Bergsma DJ, Yanagisawa M. Orexins and orexin receptors: a family of hypothalamic neuropeptides and G protein-coupled receptors that regulate feeding behavior. Cell 92: 573–585, 1998 [DOI] [PubMed] [Google Scholar]
- 87. Schwartz MW, Woods SC, Porte D, Jr, Seeley RJ, Baskin DG. Central nervous system control of food intake. Nature 404: 661–671, 2000 [DOI] [PubMed] [Google Scholar]
- 88. Shimada M, Tritos NA, Lowell BB, Flier JS, Maratos-Flier E. Mice lacking melanin-concentrating hormone are hypophagic and lean. Nature 396: 670–674, 1998 [DOI] [PubMed] [Google Scholar]
- 89. Shirasaka T, Nakazato M, Matsukura S, Takasaki M, Kannan H. Sympathetic and cardiovascular actions of orexins in conscious rats. Am J Physiol Regul Integr Comp Physiol 277: R1780–R1785, 1999 [DOI] [PubMed] [Google Scholar]
- 90. Shiuchi T, Haque MS, Okamoto S, Inoue T, Kageyama H, Lee S, Toda C, Suzuki A, Bachman ES, Kim YB, Sakurai T, Yanagisawa M, Shioda S, Imoto K, Minokoshi Y. Hypothalamic orexin stimulates feeding-associated glucose utilization in skeletal muscle via sympathetic nervous system. Cell Metab 10: 466–480, 2009 [DOI] [PubMed] [Google Scholar]
- 91. Siegel JM. Hypocretin (orexin): role in normal behavior and neuropathology. Annu Rev Psychol 55: 125–148, 2004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92. Silver IA, Erecinska M. Extracellular glucose concentration in mammalian brain: continuous monitoring of changes during increased neuronal activity and upon limitation in oxygen supply in normo-, hypo-, and hyperglycemic animals. J Neurosci 14: 5068–5076, 1994 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93. Smith GP, Epstein AN. Increased feeding in response to decreased glucose utilization in the rat and monkey. Am J Physiol 217: 1083–1087, 1969 [DOI] [PubMed] [Google Scholar]
- 94. Song Z, Routh VH. Recurrent hypoglycemia reduces the glucose sensitivity of glucose-inhibited neurons in the ventromedial hypothalamus nucleus. Am J Physiol Regul Integr Comp Physiol 291: R1283–R1287, 2006. [DOI] [PubMed] [Google Scholar]
- 95. Stanley S, Pinto S, Segal J, Perez CA, Viale A, DeFalco J, Cai X, Heisler LK, Friedman JM. Identification of neuronal subpopulations that project from hypothalamus to both liver and adipose tissue polysynaptically. Proc Natl Acad Sci USA 107: 7024–7029 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96. Sternson SM, Shepherd GM, Friedman JM. Topographic mapping of VMH –> arcuate nucleus microcircuits and their reorganization by fasting. Nat Neurosci 8: 1356–1363, 2005 [DOI] [PubMed] [Google Scholar]
- 97. Sutcliffe JG, de Lecea L. The hypocretins: setting the arousal threshold. Nat Rev Neurosci 3: 339–349, 2002 [DOI] [PubMed] [Google Scholar]
- 98. Suzuki M, Beuckmann CT, Shikata K, Ogura H, Sawai T. Orexin-A (hypocretin-1) is possibly involved in generation of anxiety-like behavior. Brain Res 1044: 116–121, 2005 [DOI] [PubMed] [Google Scholar]
- 99. Taheri S, Zeitzer JM, Mignot E. The role of hypocretins (orexins) in sleep regulation and narcolepsy. Annu Rev Neurosci 25: 283–313, 2002 [DOI] [PubMed] [Google Scholar]
- 100. Taylor MM, Samson WK. The other side of the orexins: endocrine and metabolic actions. Am J Physiol Endocrinol Metab 284: E13–E17, 2003 [DOI] [PubMed] [Google Scholar]
- 101. Thorens B. GLUT2 in pancreatic and extra-pancreatic gluco-detection. Mol Membr Biol 18: 265–273, 2001 [DOI] [PubMed] [Google Scholar]
- 102. Tolhurst G, Reimann F, Gribble FM. Nutritional regulation of glucagon-like peptide-1 secretion. J Physiol 587: 27–32, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103. Tong Q, Ye C, McCrimmon RJ, Dhillon H, Choi B, Kramer MD, Yu J, Yang Z, Christiansen LM, Lee CE, Choi CS, Zigman JM, Shulman GI, Sherwin RS, Elmquist JK, Lowell BB. Synaptic glutamate release by ventromedial hypothalamic neurons is part of the neurocircuitry that prevents hypoglycemia. Cell Metab 5: 383–393, 2007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104. Tsuneki H, Wada T, Sasaoka T. Role of orexin in the regulation of glucose homeostasis. Acta Physiol (Oxf) 198: 335–348, 2010 [DOI] [PubMed] [Google Scholar]
- 105. van den Top M, Lee K, Whyment AD, Blanks AM, Spanswick D. Orexigen-sensitive NPY/AgRP pacemaker neurons in the hypothalamic arcuate nucleus. Nat Neurosci 7: 493–494, 2004 [DOI] [PubMed] [Google Scholar]
- 106. Verret L, Goutagny R, Fort P, Cagnon L, Salvert D, Leger L, Boissard R, Salin P, Peyron C, Luppi PH. A role of melanin-concentrating hormone producing neurons in the central regulation of paradoxical sleep. BMC Neurosci 4: 19, 2003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107. Wang J, Osaka T, Inoue S. Energy expenditure by intracerebroventricular administration of orexin to anesthetized rats. Neurosci Lett 315: 49–52, 2001 [DOI] [PubMed] [Google Scholar]
- 108. Williams RH, Alexopoulos H, Jensen LT, Fugger L, Burdakov D. Adaptive sugar sensors in hypothalamic feeding circuits. Proc Natl Acad Sci USA 105: 11975–11980, 2008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109. Willie JT, Chemelli RM, Sinton CM, Yanagisawa M. To eat or to sleep? Orexin in the regulation of feeding and wakefulness. Annu Rev Neurosci 24: 429–458, 2001 [DOI] [PubMed] [Google Scholar]
- 110. Yamanaka A, Beuckmann CT, Willie JT, Hara J, Tsujino N, Mieda M, Tominaga M, Yagami K, Sugiyama F, Goto K, Yanagisawa M, Sakurai T. Hypothalamic orexin neurons regulate arousal according to energy balance in mice. Neuron 38: 701–713, 2003 [DOI] [PubMed] [Google Scholar]
- 111. Yang XJ, Kow LM, Funabashi T, Mobbs CV. Hypothalamic glucose sensor: similarities to and differences from pancreatic β-cell mechanisms. Diabetes 48: 1763–1772, 1999 [DOI] [PubMed] [Google Scholar]
- 112. Yi CX, Serlie MJ, Ackermans MT, Foppen E, Buijs RM, Sauerwein HP, Fliers E, Kalsbeek A. A major role for perifornical orexin neurons in the control of glucose metabolism in rats. Diabetes 58: 1998–2005, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113. Yuan H, Yamada K, Inagaki N. Glucose sensitivity in mouse substantia nigra pars reticulata neurons in vitro. Neurosci Lett 355: 173–176, 2004 [DOI] [PubMed] [Google Scholar]
- 114. Zhang R, Dhillon H, Yin H, Yoshimura A, Lowell BB, Maratos-Flier E, Flier JS. Selective inactivation of Socs3 in SF1 neurons improves glucose homeostasis without affecting body weight. Endocrinology 149: 5654–5661, 2008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115. Zhou D, Shen Z, Strack AM, Marsh DJ, Shearman LP. Enhanced running wheel activity of both Mch1r- and Pmch-deficient mice. Regul Pept 124: 53–63, 2005 [DOI] [PubMed] [Google Scholar]
- 116. Zhu W, Czyzyk D, Paranjape SA, Zhou L, Horblitt A, Szabo G, Seashore MR, Sherwin RS, Chan O. Glucose prevents the fall in ventromedial hypothalamic GABA that is required for full activation of glucose counterregulatory responses during hypoglycemia. Am J Physiol Endocrinol Metab 298: E971–E977, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]