Abstract
We have used a novel model of genetically imparted endurance exercise capacity and metabolic health to study the genetic and environmental contributions to skeletal muscle glucose and lipid metabolism. We hypothesized that metabolic abnormalities associated with low intrinsic running capacity would be ameliorated by exercise training. Selective breeding for 22 generations resulted in rat models with a fivefold difference in intrinsic aerobic capacity. Low (LCR)- and high (HCR)-capacity runners remained sedentary (SED) or underwent 6 wk of exercise training (EXT). Insulin-stimulated glucose transport, insulin signal transduction, and rates of palmitate oxidation were lower in LCR SED vs. HCR SED (P < 0.05). Decreases in glucose and lipid metabolism were associated with decreased β2-adrenergic receptor (β2-AR), and reduced expression of Nur77 target proteins that are critical regulators of muscle glucose and lipid metabolism [uncoupling protein-3 (UCP3), fatty acid transporter (FAT)/CD36; P < 0.01 and P < 0.05, respectively]. EXT reversed the impairments to glucose and lipid metabolism observed in the skeletal muscle of LCR, while increasing the expression of β2-AR, Nur77, GLUT4, UCP3, and FAT/CD36 (P < 0.05) in this tissue. However, no metabolic improvements were observed following exercise training in HCR. Our results demonstrate that metabolic impairments resulting from genetic factors (low intrinsic aerobic capacity) can be overcome by an environmental intervention (exercise training). Furthermore, we identify Nur77 as a potential mechanism for improved skeletal muscle metabolism in response to EXT.
Keywords: insulin sensitivity, lipid metabolism
low aerobic exercise capacity is a predictor of all-cause mortality (37), a relationship that is particularly strong in individuals with type 2 diabetes (28). The importance of this association is highlighted by the observation that individuals with type 2 diabetes and their first-degree relatives have lower aerobic exercise capacity than age- and weight-matched controls (38). Recent evidence suggests that adolescents with type 2 diabetes also exhibit impaired exercise capacity compared with age-matched peers, indicating that this impairment is present early in the onset of the disease (38). However, the complex interplay between environmental and genetic factors that contribute to both a reduced exercise capacity (5, 6) and an increased risk for developing type 2 diabetes (36) make it difficult to demonstrate a cause and effect relationship.
To study the contribution of aerobic exercise capacity to the etiology of complex disease states such as type 2 diabetes, we have developed unique animal models generated by artificial selection for low and high aerobic exercise capacity (26). In these models, 11 generations of selection resulted in a 347% difference in running capacity between low (LCR)- and high (HCR)-capacity runners (50). Importantly, selection for low aerobic capacity simultaneously resulted in metabolic dysfunction, including impaired cardiovascular function, increased adiposity, dyslipidemia, and whole body insulin resistance (50).
The molecular defect(s) that result in aberrant fuel metabolism in LCR are unclear. However, we have recently reported that LCR have impaired skeletal muscle glucose and lipid metabolism (30, 39). Furthermore, we have also demonstrated that impaired skeletal muscle metabolism is associated with reduced β2-adrenergic receptor (β2-AR) content, impaired adrenergic signal transduction, and reduced expression Nur77 in the skeletal muscle of LCR (30). Nur77 is a nuclear receptor that is downregulated in several models of insulin resistance and type 2 diabetes (12) and induces the transcription of important metabolic genes [i.e., glucose transporter-4 (GLUT4), CD36, uncoupling protein-3 (UCP3)] in response to β-adrenergic stimulation (10, 33). Indeed, altered β-adrenergic signal transduction has been proposed to contribute to metabolic disease (4), and variant alleles of the β2-AR have been identified as risk factors for obesity, dyslipidemia, and type 2 diabetes in humans (21, 34, 43, 51). Therefore, defects to whole body and skeletal muscle metabolism that occur following artificial selection for low aerobic capacity are similar to the impairments observed in individuals at risk for developing type 2 diabetes (36, 42). Accordingly, our model of divergent aerobic capacity offers a unique opportunity to investigate some of the intrinsic metabolic traits that link reduced exercise capacity to increased risk for the development of type 2 diabetes.
Although a genetic predisposition to the onset of obesity and type 2 diabetes is evident, lifestyle interventions, such as exercise training, may be used to overcome the increased risk for metabolic disease imparted via inheritance (14, 19). For example, the risk of diabetes in offspring of patients with type 2 diabetes is greatly reduced in physically fit individuals compared with their sedentary counterparts (1). Accordingly, the aim of the present investigation was to determine the genetic (inherent exercise capacity) and environmental (exercise training) contributions to skeletal muscle metabolism in animal models of low and high intrinsic aerobic capacity. We hypothesized that impaired skeletal muscle carbohydrate and lipid metabolism observed after artificial selection for low aerobic capacity would be reversed by exercise training.
METHODS
Experimental Animals
Rat models for HCR and LCR were derived from genetically heterogeneous N:NIH stock rats by artificial selection for low and high treadmill running capacity as described previously (25). Following 22 generations of artificial selection, animals were phenotyped for intrinsic running capacity at 11 wk of age using an incremental treadmill running test, and their average running capacity (in meters) was recorded (25). Rats were housed two per cage in a temperature-controlled animal room (21°C) maintained on a 12:12-h reverse light-dark cycle. Animals were provided with standard chow diets and water ad libitum. All animal experimentation procedures were carried out with the approval of animal ethics committees from California State University, Northridge, CA and the University of Michigan, Ann Arbor, MI.
Experimental Design
Following a 1-wk acclimatization period to laboratory conditions, age-matched pairs (∼20 wk) of LCR/HCR rats were randomly assigned to one of four groups (n = 10/group): LCR sedentary (LCR SED), LCR exercise-trained (LCR EXT), HCR sedentary (HCR SED), and HCR exercise-trained (HCR EXT). All EXT animals followed a 6-wk treadmill training protocol described previously (27). Briefly, exercise training consisted of an incremental protocol (4 days/wk) with the same absolute cumulative training distance (∼10 km) for all animals. Exercise-trained animals undertook their last training bout 48 h before all experimental procedures.
Blood Measures and Tissue Collection
Following the 6-wk intervention, the animals underwent a 5-h fast after which blood samples were taken for the determination of blood glucose concentration (Accu-Chek Go blood glucose meter; Roche Diagnostics, Sydney, Australia). Fasting serum nonesterified fatty acid measures were measured by using an enzymatic colorimetric method (NEFA C; Wako Pure Chemicals, Osaka, Japan). Animals were anesthetized (1 ml/kg Nembutal; Ovation Pharmaceutical, NJ), and muscle was then dissected and used in either the in vitro incubations experiments (soleus) or quickly frozen in liquid N2 [red gastrocnemius (RG)] with precooled clamps and stored at −80°C for later analysis.
In vitro muscle incubations.
The soleus muscle was excised, and under magnification was carefully dissected into longitudinal strips from tendon to tendon. Three to four strips were made from each muscle (15–20 mg/strip), with the soleus muscle of one leg used for the measure of basal and insulin-stimulated glucose transport and the contralateral muscle used for the measure of lipid oxidation. Muscle strips were allowed to recover at 30°C for 30 min in continuously gassed (95% O2-5% CO2) Krebs-Henseleit (KHB) solution containing either 0.1% fatty acid free BSA (Equitech-Bio), 8 mM glucose, and 32 mM mannitol (glucose transport experiments), or 4% fatty acid free BSA, 0.5 mM palmitate, and 5 mM glucose (lipid oxidation experiments). Throughout the experiments, vials were gently shaken in a water bath at 30°C.
Glucose transport.
Glucose transport was assessed using modified methods for determining 3-O-methylglucose transport in isolated rat soleus muscle (47). Following the 30-min preincubation period, the muscle was incubated with (insulin stimulated) or without (basal) 60 nM of insulin (Humulin, Eli Lilly, Indianapolis, IN) at 30°C for 30 min in continuously gassed KHB containing 0.1% BSA, 8 mM glucose, and 32 mM mannitol. Following incubation, the muscle was washed for 10 min in KHB with 2 mM pyruvate and 38 mM mannitol. The muscle strips were then transferred to vials containing oxygenated KHB with 8 mM 3-MG, 32 mM mannitol, 0.1% fatty acid free BSA, 1.0 μCi/ml 3-methyl-d-[1-3H] glucose (Perkin Elmer), and 0.1 μCi/ml d-[1-14C] mannitol (Perkin Elmer) as a extracellular space marker with or without 60 nM insulin for measure of glucose transport over 15 min. The reaction was stopped by rapidly washing three times in oxygenated KHB, blotting the muscle on filter paper, and freeze clamping with tongs precooled in liquid N2. Under these experimental conditions rates of 3-O-methylglucose transport remained linear for 15 min. The muscle strips were then weighed, digested in 10% TCA, transferred to glass vials containing 5 ml of scintillation fluid (Opti-fluor, Perkin Elmer, Waltham, MA), and counted in a scintillation counter (Beckman Instruments, Fullerton, CA) set for simultaneous 3H and 14C counting. Rates of basal and insulin-stimulated skeletal muscle 3-O-methylglucose transport were calculated as previously described for paired muscle strips (29).
Lipid oxidation.
Lipid oxidation was measured as previously described (9), with minor modifications. Following a 30-min preincubation, the muscle was transferred into vials containing pregassed KHB with 4% fatty acid free BSA, 0.5 mM palmitate, 5 mM glucose, and 0.2 μCi/ml [1-14C]-palmitate. The incubation medium was covered with a layer of mineral oil to trap 14CO2 released during incubation, capped, and incubated at 30°C for 30 min. The production of 14CO2 from the exogenous oxidation of [1-14C]-palmitate was measured by injecting duplicate 1.0 ml aliquots of anaerobically collected incubation medium into a sealed flask containing an equal volume of 1 M acetic acid. The released 14CO2 was trapped by a plastic insert containing filter paper saturated with 500 μl of benzothonium hydroxide and quantified using liquid scintillation counting. In addition to complete oxidative products (14CO2), incomplete oxidative products [acid-soluble metabolites (14C-ASM)] were also measured as previously described (46). Briefly, muscles were placed in borosilicate glass tubes containing 2.0 ml of ice-cold 2:1 chloroform-methanol (vol/vol), and were homogenized using a polytron (Kinematica, Lucerne, Switzerland). After homogenization, samples were centrifuged at 2,000 g (4°C) for 10 min. The supernatant was removed and transferred to a clean centrifuge tube. Distilled water (2.0 ml) was added; samples were shaken for 10 min and centrifuged to separate the aqueous and lipophilic phases. Then 200 μl of the aqueous phase was quantified by liquid scintillation counting to determine the amount of 14C-labeled oxidative intermediates resulting from isotopic fixation. The ratio of incomplete (ASM) to complete (14CO2) radiolabeled products was determined to provide an index of incomplete to complete fatty acid oxidation.
Analysis of intramuscular substrate storage.
Portions of RG were freeze dried, powdered and analyzed for the content of glycogen and intramuscular triacylglycerol as previously described (29). Briefly, freeze-dried muscle was powdered and cleaned of all visible connective tissue and blood under magnification. Portions (4–5 mg) of freeze-dried, powdered RG (9–10/group) were used to fluorometrically determine skeletal muscle triacylglycerol (total glycerol) content, following Folch lipid extraction and saponification. Portions (3–4 mg) of freeze-dried, powdered RG (8–10/group) were used to enzymatically analyze glycogen content by fluorometric detection after extraction with 2 M HCl and neutralization with 0.67 M NaOH.
Western blot analysis.
Portions of muscle cut from the RG were weighed, frozen, and homogenized in an ice-cold homogenization buffer (1:8 wt/vol) containing 50 mM Tris·HCl (pH 7.5), 5 mM Na-pyrophosphate, 50 mM NaF, 1 mM EDTA, 1 mM EGTA, 10% glycerol (vol/vol), 1% Triton-X, 1 mM DTT, 1 mM benzamidine, 1 mM PMSF, 10 μg/ml trypsin inhibitor, and 2 μg/ml aprotinin. Following centrifugation (21,000 g, 4°C) for 15 min, the supernatant was collected and assayed for protein content. RG (60 μg) was solubilized in Laemmli buffer, separated by SDS-PAGE, and transferred to polyvinylidene difluoride membranes. The membranes were then blocked (5% nonfat dry milk), and incubated overnight at 4°C with primary antibodies specific for either β2-AR (cat. no. H-73; Santa Cruz Biotechnology, Santa Cruz, CA), Nur77 (cat. no. 3562; Cell Signaling, Danvers, MA), UCP3 (cat. no. PA1–055; Pierce, Rockford, IL), fatty acid transporter (FAT)/CD36 (cat. no. FA6-152; Abcam, Cambridge, UK), or GLUT4 (cat. no. ab654; Abcam). Membranes were probed with α-tubulin (cat. no.T6074; Sigma, St. Louis, MO) antibody to monitor protein loading. The immunoreactive proteins were detected with enhanced chemiluminescence (Amersham Biosciences, Piscataway, NJ) and quantified by densitometry.
Muscle enzyme activity.
β-Hydroxyacyl-CoA dehydrogenase activity was measured according to the method of Bergmeyer (3) with minor modifications. Briefly, muscle homogenates were prepared in buffer containing 175 mM KCl and 2 mM EDTA, pH 7.4. Homogenates were added in duplicate to the appropriate wells of a 96-well microplate, along with a working solution containing 50 mM Tris·HCl, 2 mM EDTA, and 250 μM NADH. After reading the blank reaction to ensure no background activity, 100 μM acetoacetyl-CoA was added to each well, and the rate of disappearance of NADH was determined by monitoring its change in absorbance at 355 nm at 30°C over 3 min. Separate aliquots of muscle were homogenized in 100 mM potassium phosphate buffer (pH 7.3, 1:400 dilution), and citrate synthase activity was determined spectrophotometrically at 25°C by the reduction of DTNB as previously described (52).
Insulin Signaling
After the 30-min incubation, with (60 nM) or without insulin, portions of the soleus muscle strips were rapidly frozen by freeze clamping with tongs precooled in liquid N2 and stored at −80°C until later analyses. The determination of phospho-Akt Ser473 and phospho-Akt substrate (1:1,000; Cell Signaling) was determined by Western blot analysis as described above.
Statistical Analyses
Differences between treatment groups were determined using a one-way ANOVA with a Student-Newman-Keuls post hoc test using GraphPad Prism version 4.04 for Windows (GraphPad Software, La Jolla, CA). Results are expressed as means ± SE and statistical significance was accepted at P < 0.05.
RESULTS
Exercise Training Improves Whole Body Metabolic Measures in LCR
Intrinsic treadmill running capacity was 535% higher in HCR compared with LCR (P < 0.05; Table 1). HCR SED had lower body and epididymal fat pad weights and fasting serum glucose and NEFA levels than LCR SED (P < 0.05; Table 1). Exercise training lowered the body and epididymal fat pad weights and fasting serum NEFA levels in LCR (P < 0.05, LCR SED vs. LCR EXT; Table 1). There were no changes in whole body metabolic measures with exercise training in HCR (HCR SED vs. HCR EXT; Table 1).
Table 1.
Whole body metabolic health measures and skeletal muscle enzymatic activity in sedentary and exercise trained LCR/HCR rats and initial running capacity
| LCR SED | LCR EXT | HCR SED | HCR EXT | |
|---|---|---|---|---|
| Initial running capacity, m | 282 ± 12 | 276 ± 17 | 1927 ± 57*† | 1968 ± 64 |
| Body weight, g | 497 ± 19 | 432 ± 10* | 331 ± 8*† | 317 ± 14 |
| Fat pad weight, g | 6.4 ± 0.3 | 4.2 ± 0.5* | 2.1 ± 0.1 | |
| Fasting blood glucose | 6.2 ± 0.1 | 5.7 ± 0.2 | 5.3 ± 0.1* | |
| Serum nonesterified fatty acids, mM | 0.35 ± 0.04 | 0.18 ± 0.03* | 0.26 ± 0.03* | 0.20 ± 0.02 |
| Citrate synthase activity, μmol·min−1·g dry weight−1 | 46.0 ± 2.3 | 45.9 ± 1.8 | 61.5 ± 4.8*† | 66.8 ± 2.8*† |
| β-hydroxyacyl CoA dehydrogenase activity, μmol·min−1·g wet weight−1 | 4.9 ± 0.4 | 4.6 ± 0.2 | 6.2 ± 0.4*† | 6.3 ± 0.4*† |
Values are means ± SE. SCR, low aerobic capacity runners; HCR, high aerobic capacity runners; SED, sedentary; EXT, exercixed trained. Significant differences between groups:
P < 0.05 vs. LCR SED;
P < 0.05 vs. LCR EXT (n = 9–10 rats/group).
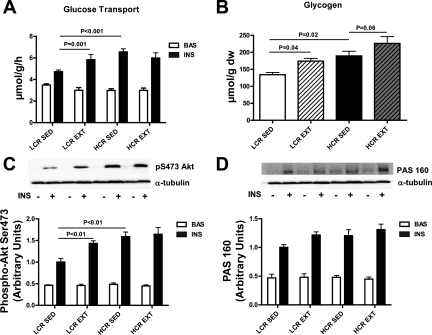
Exercise Training Enhances Glucose Metabolism in LCR but not HCR
To determine the effects of exercise training on skeletal muscle glucose metabolism, glycogen content and both basal- and insulin-stimulated glucose transport and insulin signaling were assessed in soleus muscle. Basal rates of glucose transport were similar between groups: LCR SED, 3.48 ± 0.12 μmol·−1·h−1; LCR EXT, 3.00 ± 0.26 μmol·−1·h−1; HCR SED, 2.98 ± 0.16 μmol·−1·h−1; and HCR EXT, 2.99 ± 0.21 μmol·−1·h−1 (P > 0.05). However, HCR SED had threefold higher rates of insulin-stimulated glucose transport than LCR SED (P < 0.001; Fig. 1A). Exercise training increased the rates of insulin-stimulated glucose transport in LCR by 2.3-fold (P = 0.001; LCR SED vs. LCR EXT; Fig. 1A). In contrast, exercise training did not alter insulin-stimulated glucose transport in HCR (Fig. 1A). Basal muscle glycogen content was higher in HCR SED than LCR SED (P = 0.02; Fig. 1B). Exercise training increased the muscle glycogen content in LCR (P = 0.04; LCR SED vs. LCR EXT; Fig. 1B), and there was a tendency for increased glycogen storage in HCR EXT (P = 0.06 vs. HCR SED; Fig. 1B). The phosphorylation of Akt on its Ser473 site mirrored the results of the insulin-stimulated glucose transport measures. HCR SED had a ∼60% increase in Ser473 Akt phosophorylation compared with LCR SED (P < 0.01; Fig. 1C). Insulin-stimulated Akt Ser273 phosphorylation was increased by ∼45% in LCR (P < 0.01, LCR SED vs. LCR EXT; Fig. 1C) but was unaltered by training in HCR (Fig. 1C). AS160 phosphorylation was similar in all groups (Fig. 1D).
Fig. 1.
Skeletal muscle glucose metabolism in sedentary (SED) and exercise-trained (EXT) low (LCR)- and high (HCR)-capacity runners. A: 3H-3-O-methylglucose transport was measured in the soleus muscle during in vitro incubations. Data are expressed as the rate (μmol·g−1·h−1) of glucose transport in paired muscle strips subjected to basal (BAS) or insulin-stimulated (INS) conditions (mean ± SE, n = 8–10). B: muscle glycogen content was determined in aliquots of freeze-dried/powdered red gastrocnemius muscle and expressed per gram dry weight (dw; mean ± SE, n = 9–10). BAS and INS Akt phosphorylation at Ser473 (C) and AS160 phosphorylation as detected by the phospho-Akt substrate (PAS) antibody (D) were determined by Western blot analysis using α-tubulin as a loading control (mean ± SE, n = 8–10). Significant differences between groups (P < 0.05; mean ± SE, n = 8–10) are shown.
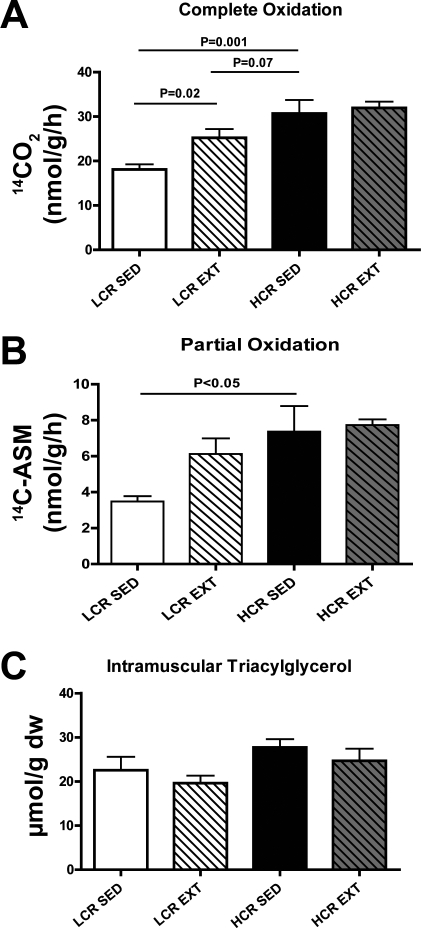
Exercise Training Improves Lipid Metabolism in LCR but not HCR
Complete (14CO2) and partial (14C-ASM) lipid oxidation were measured to determine the effect on exercise training in both phenotypes. HCR SED had significantly higher rates of complete and partial palmitate oxidation in soleus muscle compared with LCR SED (P = 0.001 and P < 0.05, respectively; Fig. 2, A and B). Exercise training increased the rates of complete palmitate oxidation by 40% in LCR (P = 0.02, LCR SED vs. LCR EXT; Fig. 2, A and B). There were no changes in the rates of postexercise training lipid oxidation in HCR (HCR SED vs. HCR EXT; Fig. 2, A and B). Intramuscular triacylglycerol content was unchanged in all groups (Fig. 2C).
Fig. 2.
Skeletal muscle lipid metabolism in LCR SED, LCR EXT, HCR SED, and HCR EXT. A: complete fatty acid oxidation (14CO2 production from labeled palmitate) was measured in soleus muscle during in vitro incubations (data expressed as rates of nmol·g−1·h−1; mean ± SE, n = 8–10). B: partial oxidation in soleus muscle as determined by the amount of label in the acid-soluble metabolite (ASM) phase of the muscle and expressed as rates of μmol·g−1·h−1 (mean ± SE, n = 8–10). C: intramuscular triacylglycerol content was determined in red gastrocnemius on aliquots of freeze-dried/powdered muscle and expressed per gram of dry weight (mean ± SE, n = 9–10). Significant differences between groups (P < 0.05; mean ± SE, n = 8–10) are shown.
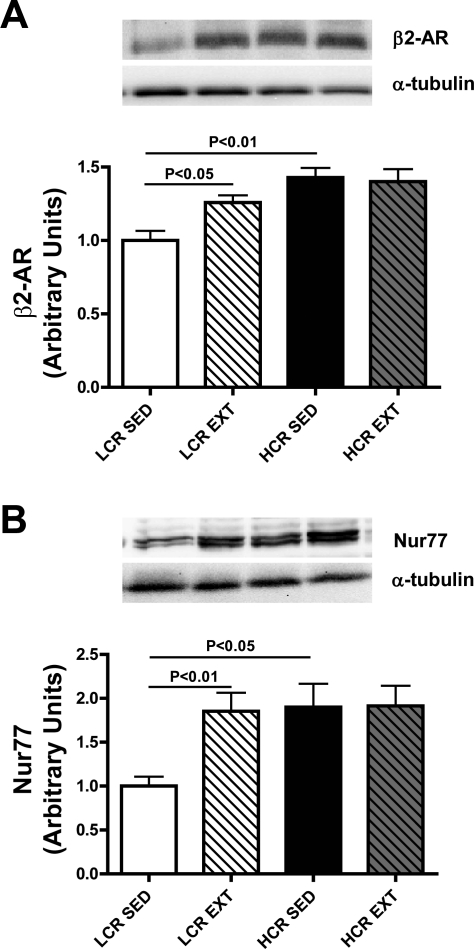
Exercise Training Increased the Expression of Components of the β-Adrenergic Pathway in LCR
HCR SED had a ∼45% higher expression of the β2-AR (P < 0.01 vs. LCR SED; Fig. 3A) and a ∼90% higher expression of the transcription factor Nur77 (P < 0.05 vs. LCR SED; Fig. 3B). Exercise training increased the expression of β2-AR by 26% (P < 0.05, LCR SED vs. LCR EXT; Fig. 3A) and Nur77 by 85% (P < 0.01, LCR SED vs. LCR EXT; Fig. 3B) in LCR to levels similar to HCR (LCR EXT vs. HCR SED; P > 0.05). Exercise training had no effect in the expression of β2-AR and Nur77 in HCR (HCR SED vs. HCR EXT, P > 0.05; Fig. 3 A and B).
Fig. 3.
Total protein content of β-adrenergic pathway components in the skeletal muscle of LCR SED, LCR EXT, HCR SED, and HCR EXT. Relative protein levels of β-adrenergic receptor (β-AR) (A) and the nuclear orphan receptor Nur77 (B) were quantified using Western blot analysis and densitometry in red gastrocnemius muscle using α-tubulin that was run as a loading control. Significant differences between groups (P < 0.05; n = 8–10/group) are shown.
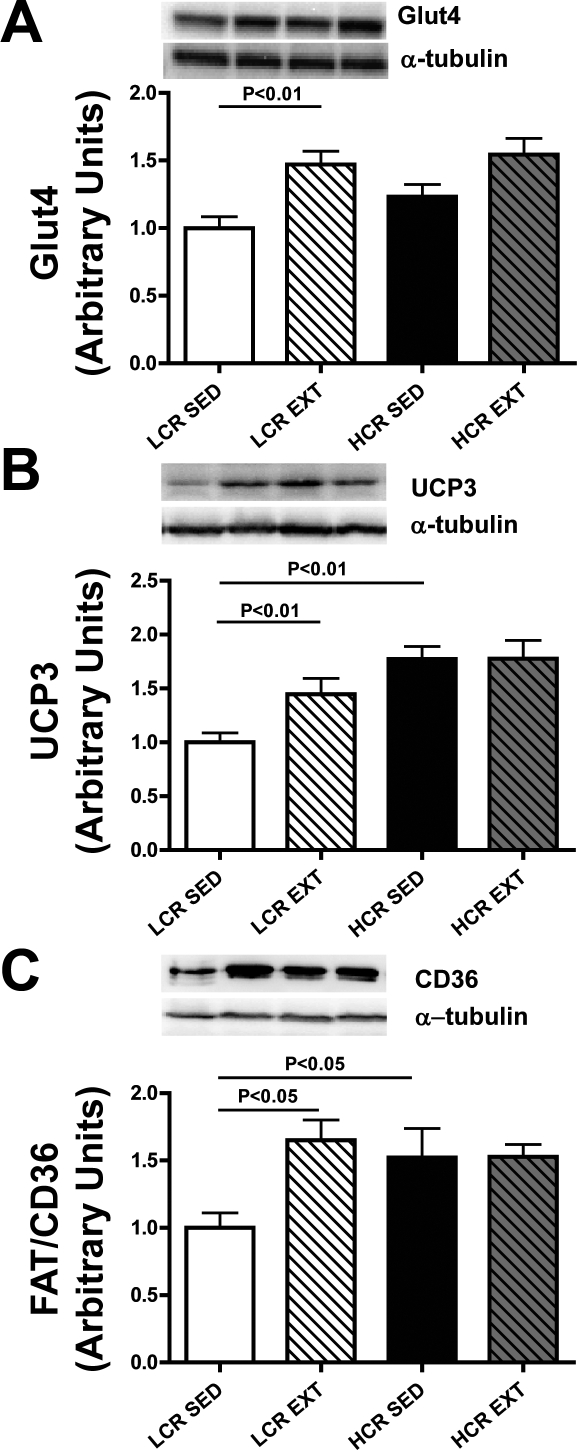
Exercise Training Enhanced the Expression of Nur77 Target Proteins in LCR
The nuclear orphan receptor Nur77 is a transcriptional regulator of target genes such as GLUT4, UCP3, and FAT/CD36. Muscle GLUT4 content was similar between HCR SED and LCR SED (Fig. 4A) and was increased by exercise training in LCR (LCR SED vs. LCR EXT, P < 0.01). UCP3 content was 70% higher (P < 0.01 vs. LCR SED; Fig. 4B) and FAT/CD36 content was 52% higher (P < 0.05 vs. LCR SED; Fig. 4C) in HCR SED. Exercise training increased the expression of Glut4 by ∼50% (P < 0.01, LCR SED vs. LCR EXT; Fig. 4A), UCP3 by ∼45% (P < 0.01, LCR SED vs. LCR EXT; Fig. 4B), and FAT/CD36 by ∼65% (P < 0.05, LCR SED vs. LCR EXT; Fig. 4C) in LCR. There were no changes in the expression of GLUT4, UCP3, or FAT/CD36 in response to exercise training in HCR (Fig. 4, A, B, and C, respectively).
Fig. 4.
Total protein content of Nur77 target genes in the skeletal muscle of LCR SED, LCR EXT, HCR SED, and HCR EXT. Relative protein levels of the glucose transporter-4 (Glut4; A), the uncoupling protein-3 (UCP3; B), and the fatty acid transporter (FAT)/CD36 (C) were quantified using Western blot analysis and densitometry in red gastrocnemius muscle using α-tubulin that was run as a loading control. Significant differences between groups (P < 0.05; n = 8–10/group) are shown.
DISCUSSION
Exercise training is a potent environmental stimulus for the improvement of insulin sensitivity in both humans (8, 24) and animals (29, 44) with insulin resistance and/or type 2 diabetes. However, there is also a strong genetic contribution to the onset of these disease states (5). Divergent selection for LCR and HCR has generated a powerful model system for dissection of aerobic endurance capacity and its contribution to metabolic disease. Importantly, simultaneous breeding of the LCR and HCR at each generation also allows for each line to serve as a control for unknown environmental changes. Hence, the results from the present investigation provide novel insight into the intrinsic and environmental contributors underlying increased risk for metabolic disease.
In the present investigation, we hypothesized that exercise training would overcome the genetic predisposition to impaired metabolic function imparted by artificial selection for low aerobic capacity. We present novel data demonstrating that exercise training improved both carbohydrate (Fig. 1) and lipid metabolism (Fig. 3) in the skeletal muscle of LCR, but not HCR. These changes were reflected by increases in the insulin-stimulated phosphorylation of Akt on Ser 473 (Fig. 1C) and improvements in whole body measures, such as circulating fatty acid levels and adiposity (Table 1). Exercise-induced improvements in skeletal muscle substrate metabolism coincided with enhancement to components of the β-adrenergic pathway (Fig. 3), and known target proteins (Fig. 4). Our results provide strong evidence to demonstrate that genetically induced impairments to muscle glucose and lipid metabolism can be ameliorated by exercise training.
Exercise training is a highly effective treatment for the reversal of skeletal muscle insulin resistance (15, 16). This occurs, in part, through an increase in oxidative enzymes that facilitate the turnover and oxidation of fatty acid both at rest and during exercise (13). Several independent research groups have reported that low-intensity exercise increases fat oxidation, decreases circulating lipids, and enhances insulin sensitivity in previously untrained, obese, and insulin-resistant individuals (14, 45, 48). Recently, Venables and Jeukendrup (48) reported that a 6-wk low-intensity exercise training regimen enhanced whole body fat oxidation and insulin sensitivity in obese individuals (48). In addition, it has been shown that low-to-moderate intensity exercise is as effective as moderate-to-high intensity exercise at improving whole body metabolic risk factors (i.e., HbA1c, body mass index, LDL) (14). The exercise training regimen employed in the present investigation was a low-intensity protocol designed for maximal compliance and was based upon physical activity guidelines in the clinical literature for the general population (i.e., three to five 30-min exercise sessions/wk). In agreement with the results of previous investigations (13,42, 45), we demonstrate that 6 wk of endurance exercise training reversed impaired skeletal muscle lipid oxidation in LCR (Fig. 2A).
Exercise-induced enhancements to lipid oxidation in LCR were associated with increased insulin-stimulated glucose uptake and Akt Ser473 phosphorylation in skeletal muscle. Yet, despite increased lipid oxidation (Fig. 2A) and improved insulin sensitivity (Fig. 1A) in the skeletal muscle of LCR EXT, there was no change in intramuscular triglyceride content compared with LCR SED (Fig. 2C). This observation is in agreement with Perdomo et al. (41) who observed enhanced insulin sensitivity in skeletal muscle cells with increased lipid oxidation despite increased intramyocellular lipid accumulation in culture (41). Enhanced lipid oxidation and insulin sensitivity following exercise training in LCR occurred in the absence of any increase in the maximal activity of the mitochondrial markers citrate synthase and β-HAD (Table 1). This suggests that under the conditions of the present investigation the observed changes in substrate handling occurred independently of any perturbations in mitochondrial biogenesis. However, exercise-training was associated with increases in the protein content of several important regulators of carbohydrate and lipid metabolism (GLUT4, CD36, Nur77, UCP3). The ability of low-intensity exercise to increase muscle GLUT4 expression in the absence of concomitant increases in the activity of mitochondrial enzymes (i.e., mitochondrial biogenesis) has been previously reported (17).
In the present investigation, both LCR and HCR underwent the same absolute exercise training protocol (i.e., the same frequency, intensity, and volume). However, exercise training-induced metabolic improvements were only observed in animals with intrinsic impairments to skeletal muscle glucose and lipid metabolism (i.e., LCR; Figs. 1 and 2). While it is possible that a higher absolute (i.e., similar relative) training stimulus may have induced metabolic changes in HCR, our results are consistent with those of Barwell et al. (2) who observed exercise training-induced improvements in the insulin sensitivity index in daughters of patients with type 2 diabetes but not in women with no family history of diabetes (2). Participants in that study (2) were matched for aerobic capacity (V̇o2max) and adiposity and undertook exercise sessions at the same relative intensity (65–80% maximum heart rate). Taken collectively, the results from the present investigation along with those of Barwell et al. (2) raise the intriguing possibility that individuals with a genetic predisposition to metabolic abnormalities may have enhanced responsiveness to the metabolic improvements induced by exercise training (2).
In the absence of exercise training, artificial selection for low intrinsic running capacity results in impaired skeletal muscle glucose and lipid metabolism (Figs. 1 and 2). However, it is unclear what specific molecular defect(s) are responsible for both reduced running capacity and impaired metabolism in LCR. A recent study by Novak et al. (40) demonstrated that daily cage activity is higher in HCR than LCR. This raises the possibility that metabolic impairments in LCR may, in part, result from lower habitual physical activity. However, it seems unlikely that a relatively small difference (∼18%) in daily cage activity (40) between LCR and HCR could result in such large (700%; Table 1) differences in intrinsic exercise capacity via a training effect. Furthermore, when cage activity of LCR/HCR was normalized by reducing cage size (40), expression of the important metabolic regulator PEPCK-C still remained lower in the skeletal muscle of LCR, compared with HCR. These results (40) suggest that intrinsic metabolic differences exist in the skeletal muscle of LCR/HCR that are independent of differences in daily cage activity.
We have previously conducted a comprehensive investigation of factors that may contribute to both exercise capacity and skeletal muscle insulin sensitivity in LCR/HCR and observed no differences in AMPK activation, or lipid (ceramide and diacylglycerol) storage in the muscle of these animals (30). We did, however, observe a reduction in β2-AR content and a concomitant impairment in β-adrenergic signal transduction and lipolysis in the skeletal muscle of LCR (30). Given that β-adrenergic pathways are critical for the regulation of glucose and lipid metabolism in skeletal muscle and other tissues (32, 49), it follows that reduced activation of these pathways could contribute to metabolic disease. In support of this contention, an impaired response of β2-adrenoreceptors has been identified as the source of reduced adrenergic-stimulated lipolysis in obese individuals (4). Furthermore, variant alleles of the β2-AR have been associated with obesity, dyslipidemia, and type 2 diabetes in humans (21, 34, 43, 51). However, the risk of obesity imparted by β2-AR alleles is reversed in physically active individuals (34). It has also been previously reported that continuous contractile activity of skeletal muscle results in elevated levels of cAMP and β2-AR within skeletal muscle, which occurred with a time course that is similar to that of activity-induced changes in mRNA and protein products of genes that encode proteins important for oxidative metabolism (41). In line with these observations, we now report that lower β2-AR content in LCR was normalized to the level of HCR by exercise training (Fig. 3A).
One mechanism by which improved β-adrenergic signal transduction may improve skeletal muscle metabolism is via activation of the nuclear receptor Nur77. Stimulation of the β-adrenergic pathway in skeletal muscle stimulates the expression of Nur77 and several of its target genes (i.e., GLUT4, CD36, UCP3) that are critical regulators of glucose and lipid metabolism in muscle (22, 30, 33). Skeletal muscle Nur77 expression is downregulated in several animal models of obesity and type 2 diabetes (i.e., ob/ob, db/db, ZDF) (12) and is increased in response to insulin-sensitizing treatments (i.e., thiazolidinediones) (12) or a single exercise bout (23, 31), indicating a possible role in the regulation of insulin sensitivity. Recent evidence suggests that Nur77 is also downregulated in response to high-fat diet-induced obesity (22) and that genetic deletion of Nur77 results in insulin resistance and altered systemic glucose metabolism in mice (10). We have previously proposed that reduced mRNA and protein expression of Nur77 and its target genes in the skeletal muscle of LCR provides a potential mechanism for impaired metabolism in this model (30). We now provide novel evidence to show that reduced Nur77, CD36, and UCP3 expression in LCR are normalized by exercise training and coincide with improved skeletal muscle insulin sensitivity and palmitate oxidation in this model. GLUT4 protein content was not different between LCR SED and HCR SED, but did increase following exercise training in LCR (Fig. 4). GLUT4 expression is known to be regulated by transcription factors other than Nur77 in skeletal muscle (19), which readily explains the disassociation between Nur77 and GLUT4 expression in untrained animals. Exercise-induced expression of Nur77 and its target genes (GLUT4, FAT/CD36, and UCP3; Fig. 4) provide a potential mechanism for improved skeletal muscle insulin sensitivity in LCR. In support of this contention, muscle-specific overexpression of FAT/CD36, UCP3, or GLUT4 improves insulin sensitivity in transgenic mice (7, 11, 18). Furthermore, independent investigations have observed an increase in the expression of FAT/CD36, UCP3, and GLUT4 following exercise training (20, 29, 35). Thus, when taken collectively, the results of the present and previous investigations identify Nur77-mediated transcription as a potential mechanism for the improvement of glucose and lipid metabolism in skeletal muscle following exercise training.
Perspectives and Significance
We have used a novel animal model of genetically imparted endurance exercise capacity and metabolic health to study selected genetic and environmental factors that contribute to skeletal muscle glucose and lipid metabolism. Our results demonstrate that rats bred for low intrinsic aerobic capacity display skeletal muscle insulin resistance and reduced lipid oxidation. Although the primary metabolic defect(s) resulting in impaired metabolism in LCR are unknown, β2-AR and Nur77 both play critical roles in the regulation of muscle glucose and lipid metabolism and were downregulated in LCR. Six weeks of low-intensity endurance training reversed impairments to glucose and lipid metabolism in the skeletal muscle of LCR and resulted in increased expression of β2-AR, Nur77, GLUT4, UCP3, and FAT/CD36. Our investigation demonstrates that metabolic impairments resulting from genetic factors (low intrinsic aerobic capacity) may be overcome by environmental factors (exercise training). We identify Nur77 as a potential mechanism for improved skeletal muscle metabolism in response to exercise training.
GRANTS
This study was supported by a Diabetes of Australia Research Trust Grant to J. A. Hawley. Rat models were supported by National Center for Research Resources Grant RR-17718, United States Department of Health and Human Services to L. G. Koch and S. L. Britton.
DISCLOSURES
No conflicts of interest, financial or otherwise, are declared by the author(s).
ACKNOWLEDGMENTS
We acknowledge the expert care of the LCR/HCR rat colony provided by Lori Gilligan and Molly Kalahar. We thank Neal Washburn and Jason Ue for their excellent technical assistance.
Present addresses: S. J. Lessard, Joslin Diabetes Center, Harvard Medical School, 1 Joslin Place, Boston, MA 02215; D. A. Rivas, Nutrition, Exercise Physiology and Sarcopenia Laboratory, J. Mayer USDA Human Nutrition Research Center on Aging, Tufts University, 711 Washington Street, Boston, MA 02111.
REFERENCES
- 1. Ahn CW, Song YD, Nam JH, Kim DM, Woo SO, Park SW, Cha BS, Lim SK, Kim KR, Lee JH, Lee HC, Huh KB. Insulin sensitivity in physically fit and unfit children of parents with Type 2 diabetes. Diabet Med 21: 59–63, 2004 [DOI] [PubMed] [Google Scholar]
- 2. Barwell ND, Malkova D, Moran CN, Cleland SJ, Packard CJ, Zammit VA, Gill JM. Exercise training has greater effects on insulin sensitivity in daughters of patients with type 2 diabetes than in women with no family history of diabetes. Diabetologia 51: 1912–1919, 2008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Bergmeyer HU. Methods of Enzymatic Analysis. New York: Academic, 1974 [Google Scholar]
- 4. Blaak EE, Schiffelers SL, Saris WH, Mensink M, Kooi ME. Impaired β-adrenergically mediated lipolysis in skeletal muscle of obese subjects. Diabetologia 47: 1462–1468, 2004 [DOI] [PubMed] [Google Scholar]
- 5. Bouchard C, Rankinen T. Individual differences in response to regular physical activity. Med Sci Sports Exerc 33: S446–S451, 2001 [DOI] [PubMed] [Google Scholar]
- 6. Bouchard C, Rankinen T, Chagnon YC, Rice T, Perusse L, Gagnon J, Borecki I, An P, Leon AS, Skinner JS, Wilmore JH, Province M, Rao DC. Genomic scan for maximal oxygen uptake and its response to training in the HERITAGE Family Study. J Appl Physiol 88: 551–559, 2000 [DOI] [PubMed] [Google Scholar]
- 7. Brozinick JT, II, Yaspelkis BB, III, Wilson CM, Grant KE, Gibbs EM, Cushman SW, Ivy JL. Glucose transport and GLUT4 protein distribution in skeletal muscle of GLUT4 transgenic mice. Biochem J 313: 133–140, 1996 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Bruce CR, Anderson MJ, Carey AL, Newman DG, Bonen A, Kriketos AD, Cooney GJ, Hawley JA. Muscle oxidative capacity is a better predictor of insulin sensitivity than lipid status. J Clin Endocrinol Metab 88: 5444–5451, 2003 [DOI] [PubMed] [Google Scholar]
- 9. Bruce CR, Mertz VA, Heigenhauser GJ, Dyck DJ. The stimulatory effect of globular adiponectin on insulin-stimulated glucose uptake and fatty acid oxidation is impaired in skeletal muscle from obese subjects. Diabetes 54: 3154–3160, 2005 [DOI] [PubMed] [Google Scholar]
- 10. Chao LC, Wroblewski K, Zhang Z, Pei L, Vergnes L, Ilkayeva OR, Ding S, Reue K, Watt MJ, Newgard CB, Pilch PF, Hevener AL, Tontonoz P. Insulin resistance and altered systemic glucose metabolism in mice lacking Nur77. Diabetes, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Choi CS, Fillmore JJ, Kim JK, Liu ZX, Kim S, Collier EF, Kulkarni A, Distefano A, Hwang YJ, Kahn M, Chen Y, Yu C, Moore IK, Reznick RM, Higashimori T, Shulman GI. Overexpression of uncoupling protein 3 in skeletal muscle protects against fat-induced insulin resistance. J Clin Invest 117: 1995–2003, 2007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Fu Y, Luo L, Luo N, Zhu X, Garvey WT. NR4A orphan nuclear receptors modulate insulin action and the glucose transport system: potential role in insulin resistance. J Biol Chem 282: 31525–31533, 2007 [DOI] [PubMed] [Google Scholar]
- 13. Goodpaster BH, Katsiaras A, Kelley DE. Enhanced fat oxidation through physical activity is associated with improvements in insulin sensitivity in obesity. Diabetes 52: 2191–2197, 2003 [DOI] [PubMed] [Google Scholar]
- 14. Hansen D, Dendale P, Jonkers RA, Beelen M, Manders RJ, Corluy L, Mullens A, Berger J, Meeusen R, van Loon LJ. Continuous low- to moderate-intensity exercise training is as effective as moderate- to high-intensity exercise training at lowering blood HbA1c in obese type 2 diabetes patients. Diabetologia 52: 1789–1797, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Hawley JA. Exercise as a therapeutic intervention for the prevention and treatment of insulin resistance. Diabetes Metab Res Rev 20: 383–393, 2004 [DOI] [PubMed] [Google Scholar]
- 16. Hawley JA, Lessard SJ. Exercise training-induced improvements in insulin action. Acta Physiol (Oxf) 192: 127–135, 2008 [DOI] [PubMed] [Google Scholar]
- 17. Helge JW, Overgaard K, Damsgaard R, Sorensen K, Andersen JL, Dyrskog SE, Hermansen K, Saltin B, Wojtaszewski JF. Repeated prolonged whole-body low-intensity exercise: effects on insulin sensitivity and limb muscle adaptations. Metabolism 55: 217–223, 2006 [DOI] [PubMed] [Google Scholar]
- 18. Heron-Milhavet L, Haluzik M, Yakar S, Gavrilova O, Pack S, Jou WC, Ibrahimi A, Kim H, Hunt D, Yau D, Asghar Z, Joseph J, Wheeler MB, Abumrad NA, LeRoith D. Muscle-specific overexpression of CD36 reverses the insulin resistance and diabetes of MKR mice. Endocrinology 145: 4667–4676, 2004 [DOI] [PubMed] [Google Scholar]
- 19. Holloszy JO. Regulation by exercise of skeletal muscle content of mitochondria and GLUT4. J Physiol Pharmacol 59 Suppl 7: 5–18, 2008 [PubMed] [Google Scholar]
- 20. Holloway GP, Bezaire V, Heigenhauser GJ, Tandon NN, Glatz JF, Luiken JJ, Bonen A, Spriet LL. Mitochondrial long chain fatty acid oxidation, fatty acid translocase/CD36 content and carnitine palmitoyltransferase I activity in human skeletal muscle during aerobic exercise. J Physiol 571: 201–210, 2006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Ishiyama-Shigemoto S, Yamada K, Yuan X, Ichikawa F, Nonaka K. Association of polymorphisms in the β2-adrenergic receptor gene with obesity, hypertriglyceridaemia, and diabetes mellitus. Diabetologia 42: 98–101, 1999 [DOI] [PubMed] [Google Scholar]
- 22. Kanzleiter T, Wilks D, Preston E, Ye J, Frangioudakis G, Cooney GJ. Regulation of the nuclear hormone receptor nur77 in muscle: influence of exercise-activated pathways in vitro and obesity in vivo. Biochim Biophys Acta 1792: 777–782, 2009 [DOI] [PubMed] [Google Scholar]
- 23. Kawasaki E, Hokari F, Sasaki M, Sakai A, Koshinaka K, Kawanaka K. Role of local muscle contractile activity in the exercise-induced increase in NR4A receptor mRNA expression. J Appl Physiol 106: 1826–1831, 2009 [DOI] [PubMed] [Google Scholar]
- 24. Kirwan JP, Solomon TP, Wojta DM, Staten MA, Holloszy JO. Effects of 7 days of exercise training on insulin sensitivity and responsiveness in type 2 diabetes mellitus. Am J Physiol Endocrinol Metab 297: E151–E156, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Koch LG, Britton SL. Artificial selection for intrinsic aerobic endurance running capacity in rats. Physiol Genomics 5: 45–52, 2001 [DOI] [PubMed] [Google Scholar]
- 26. Koch LG, Britton SL. Development of animal models to test the fundamental basis of gene-environment interactions. Obesity (Silver Spring) 16, Suppl 3: S28–S32, 2008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Koch LG, Green CL, Lee AD, Hornyak JE, Cicila GT, Britton SL. Test of the principle of initial value in rat genetic models of exercise capacity. Am J Physiol Regul Integr Comp Physiol 288: R466–R472, 2005 [DOI] [PubMed] [Google Scholar]
- 28. Kokkinos P, Myers J, Nylen E, Panagiotakos DB, Manolis A, Pittaras A, Blackman MR, Jacob-Issac R, Faselis C, Abella J, Singh S. Exercise capacity and all-cause mortality in African American and Caucasian men with type 2 diabetes. Diabetes Care 32: 623–628, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Lessard SJ, Rivas DA, Chen ZP, Bonen A, Febbraio MA, Reeder DW, Kemp BE, Yaspelkis BB, III, Hawley JA. Tissue-specific effects of rosiglitazone and exercise in the treatment of lipid-induced insulin resistance. Diabetes 56: 1856–1864, 2007 [DOI] [PubMed] [Google Scholar]
- 30. Lessard SJ, Rivas DA, Chen ZP, van Denderen BJ, Watt MJ, Koch LG, Britton SL, Kemp BE, Hawley JA. Impaired skeletal muscle β-adrenergic activation and lipolysis are associated with whole-body insulin resistance in rats bred for low intrinsic exercise capacity. Endocrinology 150: 4883–4891, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Mahoney DJ, Parise G, Melov S, Safdar A, Tarnopolsky MA. Analysis of global mRNA expression in human skeletal muscle during recovery from endurance exercise. FASEB J 19: 1498–1500, 2005 [DOI] [PubMed] [Google Scholar]
- 32. Martin WH, III, Spina RJ, Korte E, Ogawa T. Effects of chronic and acute exercise on cardiovascular β-adrenergic responses. J Appl Physiol 71: 1523–1528, 1991 [DOI] [PubMed] [Google Scholar]
- 33. Maxwell MA, Cleasby ME, Harding A, Stark A, Cooney GJ, Muscat GE. Nur77 regulates lipolysis in skeletal muscle cells. Evidence for cross-talk between the β-adrenergic and an orphan nuclear hormone receptor pathway. J Biol Chem 280: 12573–12584, 2005 [DOI] [PubMed] [Google Scholar]
- 34. Meirhaeghe A, Helbecque N, Cottel D, Amouyel P. β2-Adrenoceptor gene polymorphism, body weight, and physical activity (Comment). Lancet 353: 896, 1999 [DOI] [PubMed] [Google Scholar]
- 35. Mensink M, Hesselink MK, Borghouts LB, Keizer H, Moonen-Kornips E, Schaart G, Blaak EE, Schrauwen P. Skeletal muscle uncoupling protein-3 restores upon intervention in the prediabetic and diabetic state: implications for diabetes pathogenesis? Diabetes Obes Metab 9: 594–596, 2007 [DOI] [PubMed] [Google Scholar]
- 36. Mootha VK, Lindgren CM, Eriksson KF, Subramanian A, Sihag S, Lehar J, Puigserver P, Carlsson E, Ridderstrale M, Laurila E, Houstis N, Daly MJ, Patterson N, Mesirov JP, Golub TR, Tamayo P, Spiegelman B, Lander ES, Hirschhorn JN, Altshuler D, Groop LC. PGC-1α-responsive genes involved in oxidative phosphorylation are coordinately downregulated in human diabetes. Nat Genet 34: 267–273, 2003 [DOI] [PubMed] [Google Scholar]
- 37. Myers J, Prakash M, Froelicher V, Do D, Partington S, Atwood JE. Exercise capacity and mortality among men referred for exercise testing. N Engl J Med 346: 793–801, 2002 [DOI] [PubMed] [Google Scholar]
- 38. Nadeau KJ, Zeitler PS, Bauer TA, Brown MS, Dorosz JL, Draznin B, Reusch JE, Regensteiner JG. Insulin resistance in adolescents with type 2 diabetes is associated with impaired exercise capacity. J Clin Endocrinol Metab 94: 3687–3695, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Noland RC, Thyfault JP, Henes ST, Whitfield BR, Woodlief TL, Evans JR, Lust JA, Britton SL, Koch LG, Dudek RW, Dohm GL, Cortright RN, Lust RM. Artificial selection for high-capacity endurance running is protective against high-fat diet-induced insulin resistance. Am J Physiol Endocrinol Metab 293: E31–E41, 2007 [DOI] [PubMed] [Google Scholar]
- 40. Novak CM, Escande C, Burghardt PR, Zhang M, Barbosa MT, Chini EN, Britton SL, Koch LG, Akil H, Levine JA. Spontaneous activity, economy of activity, and resistance to diet-induced obesity in rats bred for high intrinsic aerobic capacity. Horm Behav 58: 355–367 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Perdomo G, Commerford SR, Richard AM, Adams SH, Corkey BE, O'Doherty RM, Brown NF. Increased β-oxidation in muscle cells enhances insulin-stimulated glucose metabolism and protects against fatty acid-induced insulin resistance despite intramyocellular lipid accumulation. J Biol Chem 279: 27177–27186, 2004 [DOI] [PubMed] [Google Scholar]
- 42. Perseghin G, Ghosh S, Gerow K, Shulman GI. Metabolic defects in lean nondiabetic offspring of NIDDM parents: a cross-sectional study. Diabetes 46: 1001–1009, 1997 [DOI] [PubMed] [Google Scholar]
- 43. Pinelli M, Giacchetti M, Acquaviva F, Cocozza S, Donnarumma G, Lapice E, Riccardi G, Romano G, Vaccaro O, Monticelli A. β2-Adrenergic receptor and UCP3 variants modulate the relationship between age and type 2 diabetes mellitus. BMC Med Genet 7: 85, 2006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Rivas DA, Yaspelkis BB, III, Hawley JA, Lessard SJ. Lipid-induced mTOR activation in rat skeletal muscle reversed by exercise and 5′-aminoimidazole-4-carboxamide-1-β-d-ribofuranoside. J Endocrinol 202: 441–451, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Schrauwen P, Mensink M, Schaart G, Moonen-Kornips E, Sels JP, Blaak EE, Russell AP, Hesselink MK. Reduced skeletal muscle uncoupling protein-3 content in prediabetic subjects and type 2 diabetic patients: restoration by rosiglitazone treatment. J Clin Endocrinol Metab 91: 1520–1525, 2006 [DOI] [PubMed] [Google Scholar]
- 46. Steinberg GR, Smith AC, Wormald S, Malenfant P, Collier C, Dyck DJ. Endurance training partially reverses dietary-induced leptin resistance in rodent skeletal muscle. Am J Physiol Endocrinol Metab 286: E57–E63, 2004 [DOI] [PubMed] [Google Scholar]
- 47. Thong FS, Lally JS, Dyck DJ, Greer F, Bonen A, Graham TE. Activation of the A1 adenosine receptor increases insulin-stimulated glucose transport in isolated rat soleus muscle. Appl Physiol Nutr Metab 32: 701–710, 2007 [DOI] [PubMed] [Google Scholar]
- 48. Venables MC, Jeukendrup AE. Endurance training and obesity: effect on substrate metabolism and insulin sensitivity. Med Sci Sports Exerc 40: 495–502, 2008 [DOI] [PubMed] [Google Scholar]
- 49. Wallberg-Henriksson H. Glucose transport into skeletal muscle. Influence of contractile activity, insulin, catecholamines and diabetes mellitus. Acta Physiol Scand Suppl 564: 1–80, 1987 [PubMed] [Google Scholar]
- 50. Wisloff U, Najjar SM, Ellingsen O, Haram PM, Swoap S, Al-Share Q, Fernstrom M, Rezaei K, Lee SJ, Koch LG, Britton SL. Cardiovascular risk factors emerge after artificial selection for low aerobic capacity. Science 307: 418–420, 2005 [DOI] [PubMed] [Google Scholar]
- 51. Yamada K, Ishiyama-Shigemoto S, Ichikawa F, Yuan X, Koyanagi A, Koyama W, Nonaka K. Polymorphism in the 5′-leader cistron of the β2-adrenergic receptor gene associated with obesity and type 2 diabetes. J Clin Endocrinol Metab 84: 1754–1757, 1999 [DOI] [PubMed] [Google Scholar]
- 52. Yeo WK, Lessard SJ, Chen ZP, Garnham AP, Burke LM, Rivas DA, Kemp BE, Hawley JA. Fat adaptation followed by carbohydrate restoration increases AMPK activity in skeletal muscle from trained humans. J Appl Physiol 105: 1519–1526, 2008 [DOI] [PubMed] [Google Scholar]