ABSTRACT
Endoscopic endonasal skull base surgery is a growing field in which the nasal corridors are used to address skull base lesions. Whether the middle turbinates must be removed for adequate exposure is controversial and not well addressed in the literature. This is a prospective, observational study of 163 consecutive cases of purely endoscopic endonasal transsphenoidal surgeries performed at a single tertiary care institution. The primary study outcome measurement is the feasibility of middle turbinate preservation in endoscopic transsphenoidal skull base surgery. The pathologies included 99 pituitary tumors, 15 craniopharyngiomas, 11 meningiomas, 11 Rathke's cleft cysts, 7 encephaloceles, 5 cerebrospinal fluid leak repairs, 9 clival chordomas, and 6 other pathologies of the sella. In patients undergoing surgery for a neoplasm, the average tumor size was 2.3 cm. The middle turbinate was preserved in 160/163 cases (98%). One hundred and twenty magnetic resonance imaging (MRI) studies were reviewed at a median of 16 months postoperatively and no patients (0%) developed frontal sinusitis. The middle turbinate can be preserved in nearly every endonasal, endoscopic transsphenoidal skull base case while still providing good exposure for successful tumor resection and skull base reconstruction. Postoperative sinonasal function may be better preserved with this technique.
Keywords: Middle turbinate, endsocopic skull base surgery, transsphenoidal, sinonasal, pituitary adenoma, rhinology, skull base
The endoscopic transsphenoidal approach to the midline skull base structures has been increasing in popularity as it provides a minimally invasive yet maximally aggressive therapeutic treatment option. Short-term outcomes compare favorably to more traditional open or microscopic approaches.1,2,3 One quality of life outcome measure that has not been carefully considered in these approaches is postoperative sinonasal function.
The turbinates are important nasal structures that help humidify, filter, and regulate temperature of nasal airflow before entering the lower airways. They also provide nasal resistance and contain sensory fibers essential for the perception of nasal airflow. In addition, the middle and superior turbinate contain olfactory fibers in the superior region.4 Finally, the middle turbinate serves as an important surgical landmark for the skull base, frontal sinus, and orbit.
The indications for partial or total middle turbinectomy in the setting of sinusitis are controversial. Most surgeons agree that a compromised middle turbinate secondary to polypoid degeneration, concha bullosa, or a paradoxical middle turbinate contributing to nasal obstruction or sinus disease is an acceptable reason to remove a portion of the turbinate.5,6 However, routine turbinectomy for surgical access to the paranasal sinuses has become less favorable amongst surgeons in recent years.
Many surgeons describe the routine sacrifice of one or both middle turbinates in endoscopic transsphenoidal skull base surgery,7,8,9,10 whereas other authors report adequate visualization and surgical access with preservation of this structure. The main purpose of this study is to determine the feasibility of performing endoscopic transsphenoidal skull base surgery with preservation of the middle turbinates. We report our experience with middle turbinate preservation in endoscopic transsphenoidal skull base surgery.
MATERIALS AND METHODS
We performed a review of prospectively collected data of all patients undergoing endoscopic endonasal skull base surgery from January 2005 through June 2008. This study was approved by the Institutional Review Board at the Weill Cornell Medical College. Out of a total of 225 patients, 156 were included in the study. Patients were considered eligible for inclusion if they underwent a purely endoscopic endonasal approach for treatment of pathology of the midline or paramedian skull base. Patients were excluded if this approach was used in combination with a transcribriform approach to the anterior cranial fossa as these procedures usually mandate middle turbinate resection either for complete tumor resection or access to the cribriform plate.
All patients were treated at a single tertiary care institution by a single surgical team (V.K.A., T.H.S.). A minimum follow-up of 3 months postoperatively was required for inclusion into the study. Computed tomography (CT) and magnetic resonance imaging (MRI) scans were reviewed for all patients in the pre- and postoperative period. MRI scans were reviewed in the immediate postoperative period and 3 months thereafter by a neuroradiologist and neurosurgeon (T.H.S.) to determine the presence of tumor recurrence. Gross tumor resection was determined by surgeon assessment intra-operatively and MRI at 3 months.
Additionally, an otolaryngologist (G.G.N.) analyzed all available postoperative CT or MRI scans performed at a minimum of 2 months after surgery to detect the presence of frontal sinusitis. The frontal sinuses were graded as having no opacification, partial opacification, or complete opacification. If only reports were available, then only those that directly commented on the paranasal sinuses were included. Patients with undeveloped frontal sinuses were excluded along with patients who had no imaging available.
SURGICAL PROCEDURE
A surgical team approach that included an otolaryngologist and neurosurgeon was employed for all cases. The surgical technique for endoscopic endonasal surgery has been previously described and the portions related to management of the sinonasal corridor are briefly discussed.3,11,12,13,14 The nasal mucosa is topically decongested with cottonoids soaked in 4 mL of 4% cocaine. The nasal septum and middle turbinates are injected with lidocaine 1% with a 1:100,000 dilution of epinephrine. A nasal septoplasty is performed if significant deviation of the nasal septum is noted and a piece of vomer is harvested as an autologous graft for skull base reconstruction. The inferior turbinates are lateralized. The middle and superior turbinates are also gently lateralized to expose the natural ostium of the sphenoid sinus. The spehenoid sinus ostia are enlarged bilaterally and the interposed portion of the sphenoid rostrum is resected along with the posterior 1 cm of the nasal septum. The sphenoid rostrum is opened widely allowing for a panoramic view of the sphenoid sinus cavity (Fig. 1).
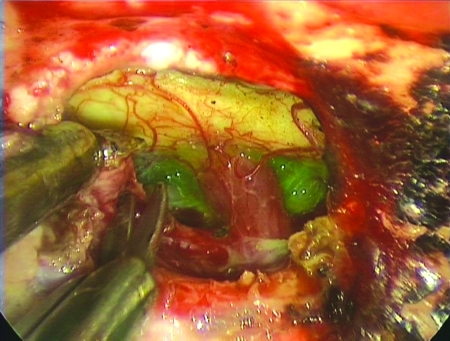
Figure 1.
Intraoperative photograph of an extended transsphenoidal approach to a suprasellar tumor that demonstrates good exposure with middle turbinate preservation. The optic chiasm is in the center of the picture.
In select cases, the transethmiod and transpterygoid corridors were used to gain access to the lateral sphenoid sinus.3 Partial resection of the middle and superior turbinates is performed if additional exposure is required for tumor extirpation or skull base reconstruction. Next, depending on the surgical target, the appropriate area of the anterior skull base is opened using a high-speed drill, curette, and a Kerrison rongeur. The pathology is addressed and the skull base is reconstructed in a multilayer fashion as discussed in several previous articles.3,12,13 Telfa nasal splints are placed along the septum and removed on postoperative day number one. Telfa splints are placed under the middle meatus in cases where a transethmoid corridor was used and removed 1 week postoperatively. Patients return for endoscopic debridements until the nasal cavity is healed and then for routine surveillance (Fig. 2).
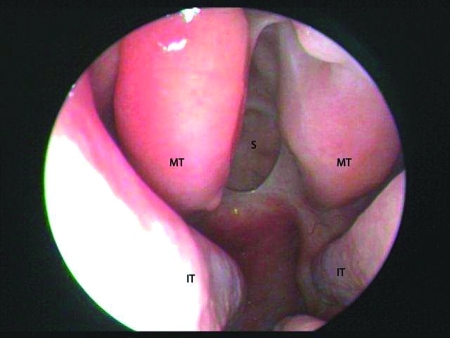
Figure 2.
Postoperative photograph of the nasal cavity after endoscopic transsphenoidal resection of a pituitary tumor. The middle turbinates (MT), inferior turbinates (IT), and sella (S) are illustrated.
RESULTS
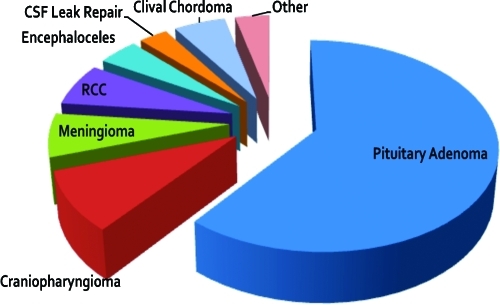
One hundred and sixty-three consecutive endoscopic transsphenoidal surgeries satisfied the aforementioned criteria and were performed on 156 patients. Ages ranged from 9 to 81 years (mean 46 years old) and 56% were female. The indications for surgery included 99 pituitary tumors, 15 craniopharyngiomas, 11 meningiomas, 11 Rathke's cleft cysts, 7 encephaloceles, 5 cerebrospinal fluid (CSF) leak repairs, 9 clival chordomas, and 6 other sellar pathologies (Fig. 3). Mean tumor size was 2.3 cm (range: 0.2 to 8 cm). Gross tumor resection was achieved in 74% of cases. Subtotal tumor resections were limited by cavernous sinus involvement, massive suprasellar extension, adherence to the optic nerve or critical brain structure, or surgery was performed for palliative or diagnostic purposes only. Twenty-four percent of the cases were revision cases, the majority of them from outside institutions. No revision cases from our institution were performed secondary to inadequate access.
Figure 3.
Indications for endoscopic transsphenoidal skull base surgery.
Twelve approaches to the lateral sphenoid sinus were performed for treatment of an encephalocele or CSF leak. All cases were completed with the assistance of a posterior ethmoidectomy and some with a transpterygoid approach. The middle turbinate was preserved in 11 of these cases. An elective, unilateral partial middle turbinectomy was performed in two other cases for surgical access (Table 1). One middle turbinate was resected in a patient with a giant clival chordoma who had previously undergone multiple surgical resections and radiotherapy at an outside institution. The third patient was transferred to our facility with a large suprasellar pituitary tumor and developed necrosis of the middle turbinate and septum after a nonendoscopic attempt at resection. The necrotic middle turbinate was believed to be secondary to over-aggressive intranasal retraction with a Hardy retractor. Overall middle turbinate preservation rate was 98% (160/163).
Table 1.
Indications for Middle Turbinate Resection
| Disease Process | Surgical Approach | Indications | |
|---|---|---|---|
| MT, middle turbinate; TC, transclival; TE, transethmoidal; TPl, transplanum; TS, transsphenoidal; TSe, transsellar; TP, transpterygoidal; TT, transtuberculum. | |||
| Patient 1 | Encephalocele | TS, TE, TP | Access |
| Patient 2 | Clival chordoma | TS, TSe, TC | Access |
| Patient 3 | Pituitary macroadenoma | TS, TT, TPl | Necrosis of MT |
MRI scans were available for 120 patients and were evaluated postoperatively for frontal sinusitis at a mean time interval of 16 months (2 to 46 months). No patients had frontal sinusitis at the time of this radiographic evaluation.
DISCUSSION
Restoration of normal sinonasal physiology is an implicit axiom of functional endoscopic sinus surgery for inflammatory sinusitis. Preservation of the middle turbinates at the time of surgery is commonly felt to contribute to this overall goal.5,6 Concerns about partial or total middle turbinectomy include alteration of nasal function, synechia formation with obstruction of sinonasal outflow tracts, promotion of frontal sinusitis, development of hyposmia, formation of excessive scar tissue, intra- and postoperative epistaxis, increased crusting postoperatively, loss of anatomic landmarks for revision surgery, and development of atrophic rhinitis or empty nose syndrome.5,6,14,15,16,17,18,19
An expert panel at the American Rhinologic Society in May 2001 addressed the issue and concluded, “the middle turbinate should not be sacrificed without a satisfactory reason.”6 Indications for total or subtotal resection might include polypoid degeneration, concha bullosa, or a paradoxically bent middle turbinate that contributes to nasal obstruction or sinus disease. In addition, resection in patients with severe allergic fungal sinusitis, eosinophilic mucincous rhinosinusitis, or tumor involvement is often indicated.
The most dubious indication is routine middle turbinate resection in endoscopic sinus surgery for surgical access. This reasoning would translate into tens of thousands of healthy middle turbinates resected annually. Some authors advocate this technique not only for access but also to improve postoperative management, increase antrostomy patency rates and reduce scarring.15,17,20,21,22,23,23 However, in transsphenoidal skull base surgery, the maxillary and ethmoid sinuses are rarely instrumented; thus, postoperative surgical debridement of the middle meatus is unnecessary.
The role of middle turbinate resection in endoscopic skull base surgery is debated and this article represents the first study to address the issue directly. Potential benefits may include increased exposure at the time of surgery, increased postoperative sinonasal patency, and the use of a free mucosal graft from the resected middle turbinate.7,8,9,10,17,20,21,22,23 However, given the potential negative impact on sinonasal function, a critical examination of this issue is necessary. The results of this study demonstrate that the middle turbinate can be preserved in nearly every case (98.2%) with good visualization and access to the surgical target. This included extended transplanum and transclival approaches. Thus, the feasibility of middle turbinate preservation in endoscopic transsphenoidal skull base surgery as the primary outcome measure of this study was possible in nearly every case. We did not use one free mucosal graft from the middle turbinate in this large series as we prefer an axial flap like the well-vascularized nasoseptal flap for skull base reconstruction. We do not advocate routine middle turbinectomy for the sole purpose of obtaining a mucosal graft as mucosa from the posterior septum or sphenoid sinus can be easily harvested. Additional concerns with middle turbinectomy in the setting of endoscopic skull base surgery include increased crusting and atrophic rhinitis that may occur long term secondary to the creation of wide sphenoidotomies, a posterior septectomy, and resection of the middle turbinate. Moreover, there may be an increased possibility of frontal sinusitis and decreased olfaction.
To our knowledge, there are no previously published studies investigating iatrogenic frontal sinusitis after middle turbinectomy in endonasal, endoscopic transsphenoidal surgery. Other series, however, have examined this issue following middle turbinate resection in endoscopic sinus surgery for inflammatory disease. Swanson et al. reported a 75% incidence of mild or moderate frontal sinusitis with middle turbinate resection, compared with a 45% incidence among those with middle turbinate preservation during endoscopic sinus surgery for sinusitis.16 Other studies report an incidence between 0 and 27% of iatrogenic frontal sinusitis secondary to a lateralized, partially resected middle turbinate.15,16,20,21,22 Moreover, the management of iatrogenic frontal sinusitis is a technically challenging problem as it is often refractory to medical management and may require an extended frontal sinus procedure.23 In our review of the postoperative MRI scans of 120 patients undergoing transsphenoidal surgery with turbinate preservation, we did not find a single case of frontal sinusitis at a median radiographic evaluation of 16 months.
Based on our experience, several technical points may allow for the simultaneous combination of adequate surgical exposure and preservation of the middle turbinates. Topical vasoconstriction at the beginning of the procedure will decrease mucosal bleeding and swelling throughout the procedure. Correction of any significant septal deviation and out-fracturing of the inferior turbinates will enlarge the dimensions of the nasal passageways. Attention to performing an adequate posterior septectomy and resection of the sphenoid rostrum is critical to the transsphenoidal corridor. This portion of the procedure allows for a two-nostril technique and wide working passageways. The use of an endoscope holder with an irrigation port to clean the lens allows for a stable view, decreased need to navigate around the middle turbinate, and decreased soilage by blood. The endoscope can be then used freehand in the portions of the procedure where a dynamic view is indicated.
Several limitations associated with this study are identified. This nonrandomized study represents a single case series by a single surgical team. It does not provide data on outcomes following endoscopic endonasal transsphenoidal surgery with middle turbinate resection. Clinical sinonasal outcome measures like endoscopy scores would be useful additional measures to determine the importance of the middle turbinate in this patient population.
CONCLUSION
In conclusion, we were able to preserve the middle turbinate in nearly all endonsal endoscopic transsphenoidal skull base cases. We maintained good visualization and surgical access to the target without jeopardizing nasal function. We suggest that the endoscopic skull base surgeon consider middle turbinate preservation in transsphenoidal approaches to the skull base. However, we would caution this recommendation by reminding the surgeon that the middle turbinate should not compromise safe and total completion of the surgical objectives. Further studies exploring postoperative sinonasal function following endoscopic skull base surgery are required to further advance the field.
NOTES
This paper was presented at the North American Skull Base Society Meeting, Vancouver, British Columbia, Canada, September 2008.
Institutional Review Board approval was obtained through the Weill Cornell Medical College.
ACKNOWLEDGMENTS
Nicholas A. Ross, BS, Research Assistant.
REFERENCES
- Frank G, Pasquini E, Farneti G, et al. The endoscopic versus the traditional approach in pituitary surgery. Neuroendocrinology. 2006;83(3–4):240–248. doi: 10.1159/000095534. [DOI] [PubMed] [Google Scholar]
- Tabaee A, Anand V K, Barrón Y, et al. Endoscopic pituitary surgery: a systematic review and meta-analysis. J Neurosurg. 2009;111(3):545–554. doi: 10.3171/2007.12.17635. [DOI] [PubMed] [Google Scholar]
- Schwartz T H, Fraser J F, Brown S, Tabaee A, Kacker A, Anand V K. Endoscopic cranial base surgery: classification of operative approaches. Neurosurgery. 2008;62(5):991–1002. discussion 1002–1005. doi: 10.1227/01.neu.0000325861.06832.06. [DOI] [PubMed] [Google Scholar]
- Leopold D A, Hummel T, Schwob J E, Hong S C, Knecht M, Kobal G. Anterior distribution of human olfactory epithelium. Laryngoscope. 2000;110(3 Pt 1):417–421. doi: 10.1097/00005537-200003000-00016. [DOI] [PubMed] [Google Scholar]
- Kennedy D W. Middle turbinate resection: evaluating the issues—should we resect normal middle turbinates? Arch Otolaryngol Head Neck Surg. 1998;124(1):107. doi: 10.1001/archotol.124.1.107. [DOI] [PubMed] [Google Scholar]
- Rice D H, Kern E B, Marple B F, Mabry R L, Friedman W H. The turbinates in nasal and sinus surgery: a consensus statement. Ear Nose Throat J. 2003;82(2):82–84. [PubMed] [Google Scholar]
- Cappabianca P, Cavallo L M, de Divitiis O, Solari D, Esposito F, Colao A. Endoscopic pituitary surgery. Pituitary. 2008;11(4):385–390. doi: 10.1007/s11102-008-0087-5. [DOI] [PubMed] [Google Scholar]
- Kassam A, Snyderman C H, Mintz A, et al. Expanded endonasal approach: the rostrocaudal axis. Part I. Crista galli to sella turcica. Neurosurg Focus. 2005;19(1):1–12. [PubMed] [Google Scholar]
- de Divitiis E, Cavallo L M, Cappabianca P, Esposito F. Extended endoscopic endonasal transsphenoidal approach for the removal of suprasellar tumors: part 2. Neurosurgery. 2007;60(1):46–58. discussion 58–59. doi: 10.1227/01.NEU.0000249211.89096.25. [DOI] [PubMed] [Google Scholar]
- Frank G, Pasquini E, Doglietto F, et al. The endoscopic extended transsphenoidal approach for craniopharyngiomas. Operative Neurosurgery. 2006;59(1 Suppl):S75–S83. doi: 10.1227/01.NEU.0000219897.98238.A3. [DOI] [PubMed] [Google Scholar]
- Cappabianca P, Cavallo L M, Colao A, et al. Endoscopic endonasal transsphenoidal approach: outcome analysis of 100 consecutive procedures. Minim Invasive Neurosurg. 2002;45(4):193–200. doi: 10.1055/s-2002-36197. [DOI] [PubMed] [Google Scholar]
- Leng L Z, Brown S, Anand V K, Schwartz T H. “Gasket-seal” watertight closure in minimal-access endoscopic cranial base surgery. Neurosurgery. 2008;62(5, Suppl 2):E342–E343. discussion E343. doi: 10.1227/01.neu.0000326017.84315.1f. [DOI] [PubMed] [Google Scholar]
- Tabaee A, Anand V K, Brown S M, Lin J W, Schwartz T H. Algorithm for reconstruction after endoscopic pituitary and skull base surgery. Laryngoscope. 2007;117(7):1133–1137. doi: 10.1097/MLG.0b013e31805c08c5. [DOI] [PubMed] [Google Scholar]
- Lawson W. The intranasal ethmoidectomy: an experience with 1,077 procedures. Laryngoscope. 1991;101(4 Pt 1):367–371. doi: 10.1002/lary.1991.101.4.367. [DOI] [PubMed] [Google Scholar]
- Morgenstein K M, Krieger M K. Experiences in middle turbinectomy. Laryngoscope. 1980;90(10 Pt 1):1596–1603. [PubMed] [Google Scholar]
- Swanson P B, Lanza D C, Vining E M, et al. The effect of middle turbinate resection upon the frontal sinus. Am J Rhinol. 1995;9:191–195. [Google Scholar]
- Biedlingmaier J F, Whelan P, Zoarski G, Rothman M. Histopathology and CT analysis of partially resected middle turbinates. Laryngoscope. 1996;106(1 Pt 1):102–104. doi: 10.1097/00005537-199601000-00020. [DOI] [PubMed] [Google Scholar]
- Gaskins R E., Jr Scarring in endoscopic ethmoidectomy. Am J Rhinol. 1994;8:271–274. [Google Scholar]
- Houser S M. Surgical treatment for empty nose syndrome. Arch Otolaryngol Head Neck Surg. 2007;133(9):858–863. doi: 10.1001/archotol.133.9.858. [DOI] [PubMed] [Google Scholar]
- Fortune D S, Duncavage J A. Incidence of frontal sinusitis following partial middle turbinectomy. Ann Otol Rhinol Laryngol. 1998;107(6):447–453. doi: 10.1177/000348949810700601. [DOI] [PubMed] [Google Scholar]
- Havas T E, Lowinger D S. Comparison of functional endonasal sinus surgery with and without partial middle turbinate resection. Ann Otol Rhinol Laryngol. 2000;109(7):634–640. doi: 10.1177/000348940010900704. [DOI] [PubMed] [Google Scholar]
- Saidi I S, Biedlingmaier J F, Rothman M I. Pre- and postoperative imaging analysis for frontal sinus disease following conservative partial middle turbinate resection. Ear Nose Throat J. 1998;77(4):326–328, 330, 332 passim. [PubMed] [Google Scholar]
- Kuhn F A, Javer A R, Nagpal K, Citardi M J. The frontal sinus rescue procedure: early experience and three-year follow-up. Am J Rhinol. 2000;14(4):211–216. doi: 10.2500/105065800779954437. [DOI] [PubMed] [Google Scholar]