Abstract
Using high-resolution spectral-domain optical coherence tomography (SD-OCT) and adaptive optics (AO) imaging, photoreceptor damage in a patient with a central macular arteriovenous malformation (AVM) and otherwise unexplained progressive vision loss was demonstrated. This patient presented with a central scotoma, a macular AVM, and no evidence of macular edema, retinal hemorrhage, or subretinal fluid. Fluorescein angiography (FA) did not reveal leakage. Over 28 years, her vision progressively worsened from 20/25 to 20/400. Both time-domain OCT and FA did not reveal any significant retinal abnormality. However, high-resolution SD-OCT imaging revealed clear disorganization of the outer segments and focal photoreceptor disruption adjacent to the AVM. En face AO images further revealed loss of the photoreceptors in these regions. This case demonstrates the unique finding of progressive vision loss in a patient with a congenital retinal AVM, and how high-resolution imaging can detect structural changes of the retina in patients with otherwise unexplained vision loss.
INTRODUCTION
We report an unusual case of a woman who presented with progressive vision loss associated with a macular arteriovenous malformation (AVM), which could not be explained by exam or conventional imaging systems. Two high-resolution imaging systems developed in UC Davis, namely high-resolution spectral-domain optical coherence tomography (SD-OCT)1 and an adaptive optics (AO) flood-illuminated fundus camera2 were used to image the patient’s macula and revealed retinal abnormalities that correlated with the visual loss. Time-domain OCT has been rapidly popularized as an effective method to evaluate the retina; however, the lateral resolution of clinical OCT systems including SD-OCT is insufficient for the imaging of individual cellular structures. This can be achieved by implementing AO to measure and correct the wavefront error of the eye as shown in this case.2
CASE REPORT
A 19-year-old woman presented with a sudden loss of central vision in her right eye. Her visual acuity was 20/25 in the right eye (OD) and 20/20 in the left eye (OS). She was found to have a central scotoma in the affected eye. A Funduscopic examination revealed an anomalous retinal macular vessel; however, no macular thickening or scarring was noted. A Fluorescein angiogram (FA) conducted 6 months later showed no leakage or macular ischemia. Over the next 28 years, she noted increased visual deterioration in the affected eye.
At age 47, the patient’s scotoma increased in size and her vision decreased to 20/400 OD. A Funduscopic examination revealed the anomalous macular vessel unchanged. The left eye was normal, and brain MRI was normal with no intracranial AVMs. FA did not reveal any macular edema or pathology (Fig. 1A and B). Even Time-domain OCT could not explain this loss of vision (Fig. 1C). Multifocal electroretinogram (mfERG) and visual field tests confirmed her right central scotoma (Fig. 2).
Figure 1.
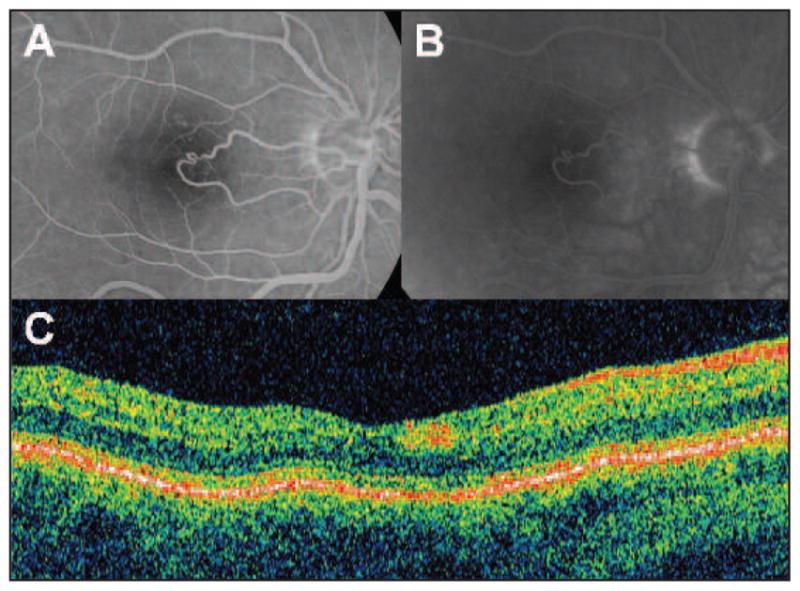
This figure shows the absence of macular fluorescein leakage or other retinal pathology by standard retinal imaging. Fluorescein angiography, early (A) and late (B) phase. No leakage detected suggesting no macular edema. (C) Stratus optical coherence tomography (OCT) revealing no retinal fluid accumulation in the retina.
Figure 2.
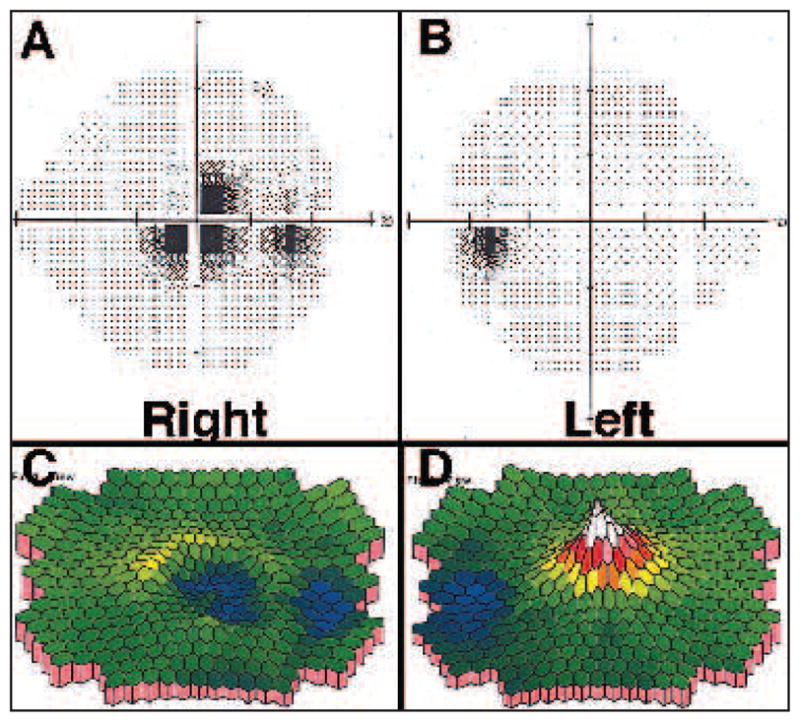
(A and B) HVF of both eyes (OU). Grayscale results of Humphrey static perimetry: 24–2 threshold test was performed with stimulus size III and SITA-Standard algorithm. Right (A) shows central scotoma, whereas the left visual field is unaffected. (C and D) Multifocal electroretinogram analysis using a 103-hexagon stimulus display shown as pseudocolor response density plots (first-order kernel response) of patient shows central macular depression in the right eye (OD) (C) whereas the left eye (OS) is within normal limits (D).
SD-OCT revealed a region of both photoreceptor outer segment loss and laminar disorganization as represented by the inconsistent areas of hyperreflectivity in the areas adjacent to the anomalous vessel (Fig. 3A). En face AO-flood images (Fig. 3B) and en face slices from SD-OCT2 at the level of the photoreceptor outer segments (Fig. 3C) confirmed the disruption of photoreceptors in the affected area. The areas of structural changes correspond to areas of reduced retinal response measured by mfERG and visual field testing.
Figure 3.
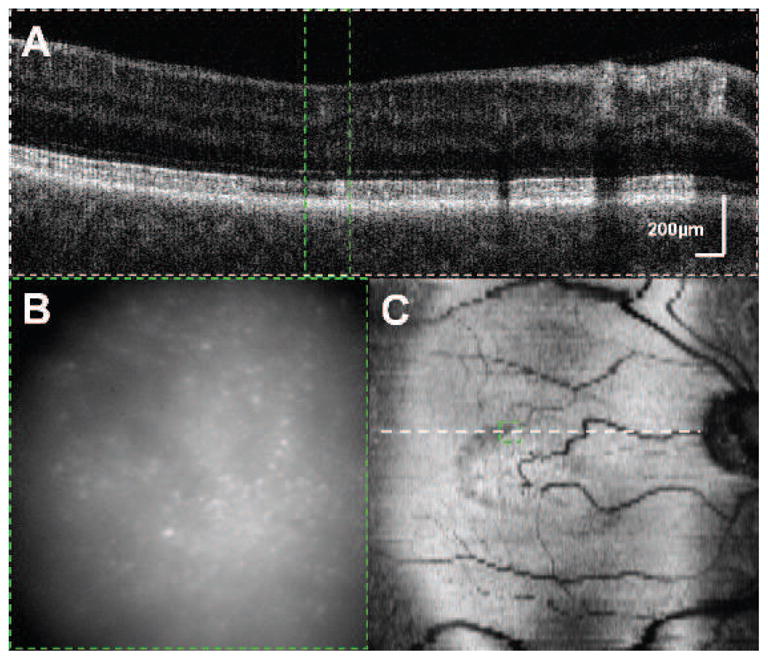
(A) High-Resolution Fd-OCT 6 × 1 mm section showing central fovea with photoreceptor damage superior to the fovea. Arrow indicates the area where there is loss of the outer segments. (B) Adaptive optics (AO) flood-illuminated fundus camera. The same region of the retina shown in A identified in green. Individual bright spots indicate individual cone photoreceptors, which are less numerous on the right side of the image. (C) En face reconstruction (6 × 6 mm) showing the level of the outer segments. Photoreceptor disorganization and loss noted temporally to the aberrant vessel. The green box in this image corresponds to image B and the green rectangle in A. The arrow points to an area of photoreceptor outer segment loss corresponding to the arrow in image A.
DISCUSSION
Retinal AVMs are rare congenital lesions that usually occur unilaterally and are often asymptomatic.3 Systemic work-up of these patients including brain MRI scan is essential in these patients for intracranial AVMs can be associated with retinal AVMs known as Wyburn-Mason syndrome.4
Retinal AVMs have been divided into three groups by Archer et al. 5 Our patient falls into group II of retinal AVMs, which have an arteriovenous connection without interposition of a capillary bed lacking exudation or subretinal fluid. These types of large-caliber communications result in hyperdynamic flow through low-resistance veins and can lead to complications ranging from edema to hemorrhage. This type is usually associated with good vision. When the macula is involved, visual acuity may be affected.
This case documents for the first time the loss and disruption of the photoreceptor layer associated with a retinal AVM and progressive vision loss. New imaging techniques revealed structural changes in the retina that were previously undetectable. The area of photoreceptor damage follows the course of the retinal vessel (Fig. 3C). These findings coupled with the history of progressive vision loss suggest that the central macular scotoma was caused by secondary photoreceptor injury.
The cause of this photoreceptor disruption is unclear. Retinal AVM’s are known to cause retinal and sub-retinal hemorrhaging; however, this was not found on any examination. Her loss of vision may be due to episodic edema causing photoreceptor damage; however, macular edema was not detected by examination, FA, or time-domain OCT. Hopen asserts that loss of vision in patients with retinal AVMs results from compression of nerve fibers.6 In contrast we found that our patient’s loss of vision correlated with photoreceptor damage rather than loss of the nerve fiber layer. Alternatively, high vascular flow in the foveal avascular zone may have indirectly caused photoreceptor injury as photoreceptor loss was only found in this region and not along the vessel closer to the disc.
In summary, this case demonstrates the new finding of photoreceptor damage associated with an anomalous macular vessel only detectable by new imaging techniques such as SD-OCT and AO imaging.
Acknowledgments
Supported in part by Research to Prevent Blindness and National Eye Institute grant EY 014743.
Footnotes
The authors have no financial or proprietary interest in the materials presented herein.
References
- 1.Alam S, Zawadzki RJ, Choi SS, et al. Clinical application of rapid serial Fourier-domain optical coherence tomography for macular imaging. Ophthalmology. 2006;113:1425–1431. doi: 10.1016/j.ophtha.2006.03.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Choi SS, Doble N, Hardy JL, et al. In vivo imaging of the photoreceptor mosaic in retinal dystrophies and correlations with visual function. Invest Ophthalmol Vis Sci. 2006;47:2080–2092. doi: 10.1167/iovs.05-0997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ebert EM, Albert DM. The Phakomatoses. In: Albert DM, Jakobiec FA, editors. Principles and Practice of Ophthalmology. Philadelphia: WB Saunders Co; 1994. pp. 3317–3320. [Google Scholar]
- 4.Reck SD, Zacks DN, Eibschitz-Tsimhoni M. Retinal and intracranial arteriovenous malformations: Wyburn-Mason syndrome. J Neuroophthalmol. 2005;25:205–208. doi: 10.1097/01.wno.0000177301.82963.9f. [DOI] [PubMed] [Google Scholar]
- 5.Archer DB, Deutman A, Ernest JT, Krill AE. Arteriovenous communications of the retina. Am J Ophthalmol. 1973;75:224–241. doi: 10.1016/0002-9394(73)91018-0. [DOI] [PubMed] [Google Scholar]
- 6.Hopen G, Smith JL, Hoff JT, Quencer R. The Wyburn-Mason syndrome. Concomitant chiasmal and fundus vascular malformations. J Clin Neuroophthalmol. 1983;3:53–62. [PubMed] [Google Scholar]


