Abstract
Oseltamivir resistance in pandemic 2009 influenza A/H1N1 is caused by the neuraminidase mutation H275Y. This mutation has also been associated with in vitro resistance to peramivir, but few clinical cases have been described to date. Using allele-specific real-time reverse-transcriptase polymerase chain reaction assay for the H275Y mutation, we were able to identify resistant H1N1 in a hematopoietic cell transplant recipient receiving intravenous peramivir therapy, and through serial testing we determined the molecular evolution of resistance. This case demonstrates that an H275Y mutant population can emerge early and replicate in vivo under peramivir antiviral pressure to become the major viral population.
Keywords: peramivir, zanamivir, influenza, H275Y, resistance
In immunocompromised patients with pandemic 2009 influenza A/H1N1 virus (pH1N1), symptoms can vary from mild to life threatening (1–2). Treatment of these patients, particularly those who develop severe multiorgan failure, has been limited by influenza-specific antiviral agents that are US Food and Drug Administration (FDA) approved only for oral or inhaled administration. Peramivir, an investigational intravenous (IV) neuraminidase inhibitor, was released under an FDA emergency use authorization in 2009 to respond to that urgent need (3). Unfortunately, emerging oseltamivir resistance in H1N1 related to the H275Y neuraminidase mutation is also associated with in vitro resistance to peramivir (4). We report a case of an immunocompromised host with severe pH1N1 who had emergence of an H275Y mutation during active IV peramivir therapy.
Case report
A man in his early 50’s with a history of an unrelated donor allogeneic stem cell transplant for acute myelogenous leukemia in September 2007 presented in October 2009 with history of subjective fever, nausea, vomiting and new upper respiratory tract symptoms. The patient’s post-transplant course had been complicated by chronic graft-versus-host-disease involving the skin, liver, and gut that required ongoing treatment with immunosuppressive drugs (mycophenolate mofetil, prednisone, and tacrolimus). At presentation, vital signs were significant for a blood pressure of 180/98, and a temperature of 36.6°C. Initial laboratory investigation disclosed a leukocyte count of 5.3 × 103/µL, with significant lymphopenia (0.11 × 103/µL) and thrombocytopenia (127 × 103/µL); his creatinine was also elevated at 1.9 mg/dL (baseline 1.3 mg/dL). Blood cultures and a nasopharyngeal (NP) wash for influenza were performed, and admission chest radiograph showed left lower lobe consolidation and patchy opacities in the right middle lobe. He was started on empiric IV levofloxacin. Before admission, the patient was not receiving oseltamivir prophylaxis.
The following morning, he developed a fever to 38.4°C, increased shortness of breath, tachypnea, and progressive oxygen requirements. Repeat chest radiographs demonstrated new bibasilar opacities but, because of his elevated creatinine, a chest computed tomography was deferred. The patient was found to have a peroneal vein thrombosis, but a ventilation perfusion scan indicated low probability for an acute pulmonary embolus. IV vancomycin and imipenem were added.
Owing to a high clinical suspicion for influenza, empiric high-dose oseltamivir (150 mg orally twice daily) was added the morning of day 3. Later that evening, his admission NP wash was reported to be positive by polymerase chain reaction (PCR) for pH1N1 with a viral load of 7.3 log copies/reaction (c/rxn). His respiratory status continued to decline, and despite maximal oxygen therapy he required intubation. He underwent diagnostic bronchoscopy the following day, which showed clinical evidence of alveolar hemorrhage, and bronchoalveolar lavage (BAL) fluid was positive for pH1N1 by PCR with a viral load of 7.3 log c/rxn.
On day 7, the patient was switched to IV peramivir (600 mg loading dose and then dose adjusted for renal function 150–100 mg daily) because of the concern for poor oral absorption of oseltamivir and severity of disease; he was also given a dose of IV immunoglobulin on day 8. He tolerated peramivir well, although on day 14 developed hallucinations and, out of concerns that peramivir could be contributing, 1 dose was held. Repeat NP swab from day 14 detected pH1N1 with a viral load of 6.8 log c/rxn. Peramivir was restarted on day 16 and the patient required re-intubation secondary to respiratory distress. Because of viral persistence and continued clinical decline, there were concerns the virus had developed resistance. Peramivir was discontinued on day 17 and testing for the H275Y resistance mutation was ordered. Although it was presumed that the virus was resistant to oseltamivir and adamantanes, combination therapy with oseltamivir (150 mg twice daily), oral ribavirin (600 mg once, then 200 mg daily) and rimantidine (100 mg daily) were started pending emergency approval of IV zanamivir.
The patient underwent repeat bronchoscopy on day 18 and, although the PCR did not detect influenza on the BAL specimen, an NP swab from the same day had a viral load of 3.4 log c/rxn. On day 19, combination therapy was discontinued and IV zanamivir was started per an emergency new drug application from the FDA. The patient developed oliguric renal failure requiring daily dialysis by day 20. On day 22, a repeat PCR done on NP swab remained positive for pH1N1 with a viral load of 3.4 log c/rxn.
His respiratory status continued to worsen, and he eventually required inhaled nitrous oxide for ongoing hypoxemia despite maximum ventilator support. By day 24, his pH1N1 viral load on NP swab had declined to 2.5 log c/rxn. He eventually developed an ileus, began to experience cardiac dysrythmias, and was eventually transitioned to comfort measures. He died on day 28 of his hospital stay.
Prior to diagnosis and throughout his hospitalization the patient’s lymphocyte count remained persistently <250 cells/µL. An autopsy demonstrated bilateral pulmonary consolidation, hemorrhage with diffuse alveolar damage and patchy fibrosis, diffuse necrotizing pancreatitis, and marantic endocarditis with vegetation of aortic valve.
Methods
All samples were collected with patient and family consent and tested retrospectively for the H275Y mutation. All samples that were positive by in-house developed pH1N1 real-time reverse-transcriptase (RT)-PCR assays targeting the matrix, and hemagglutinin genes were also tested by an allele-specific real-time RT-PCR (ASPCR) for the neuraminidase H275Y mutation. Genotyping by ASPCR has been shown to be sensitive, specific, and reliable for quantitative analysis of minor mutant populations (5). ASPCR targeting H275Y in pH1N1 was designed and validated in our laboratory and showed very good correlation with pyrosequencing (6). Our assay can detect at least 10% of a mutant genotype in 90% background of wild-type genotype virus, equivalent to the limit of detection for pyrosequencing, which is considered the gold standard for resistance testing (7). No samples were sent for culture.
Results
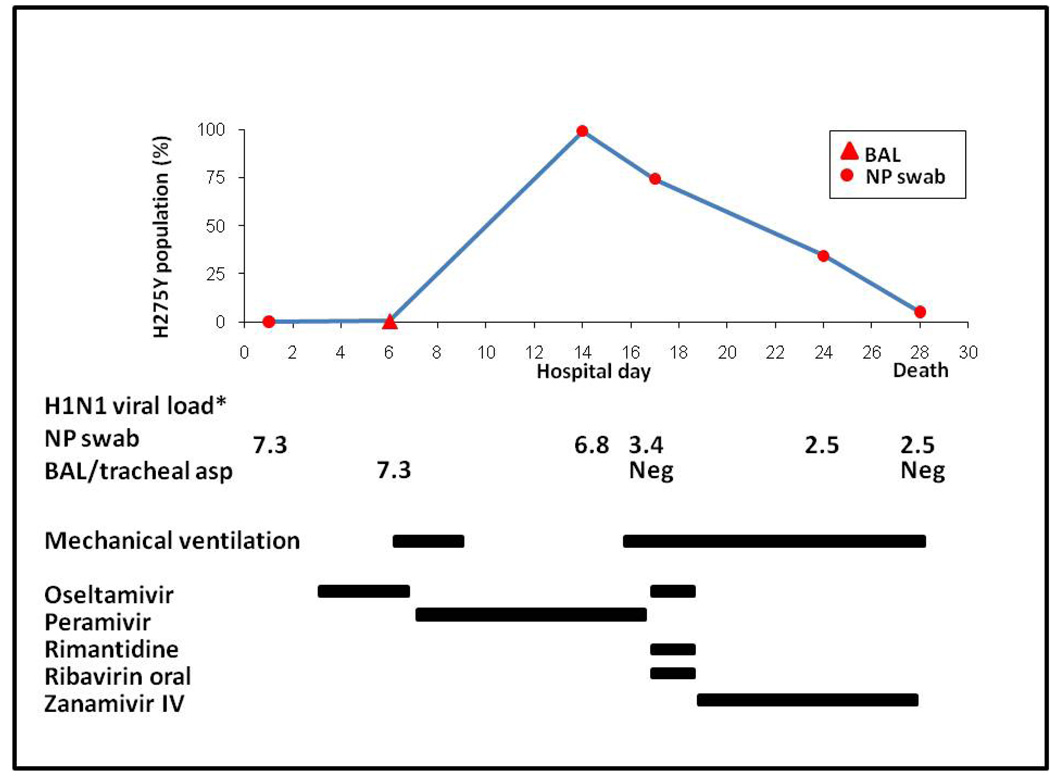
An NP swab collected on day 1 and BAL fluid collected on day 6 were >90% wild-type at position 275 of the neuraminidase protein, before the start of peramivir. However, repeat NP swab collected on day 13 of hospitalization after 6 days of IV peramivir, contained >90% H275Y mutant population as determined by ASPCR. On day 17 of hospitalization, the pH1N1 viral load in a NP swab diminished and the H275Y mutant population decreased to 75% of total viral population. IV zanamivir was started on day 19 of hospitalization, followed by a viral load decline and a continued decrease in the H275Y mutant population in a NP swab obtained on day 24 (Fig. 1). The last specimens obtained at autopsy were positive for pH1N1by PCR in a NP swab (viral load of 2.5 log c/rxn) but negative in tracheal aspirate, lung, heart, liver, pancreas, and bowel tissue. This positive NP swab showed only the presence of >90% wild-type virus.
Fig 1. Clinical course and percentage of pandemic H1N1 population with H275Y mutation.
*log10 copies/reaction. BAL, bronchoalveolar lavage; NP, nasopharyngeal; asp, aspirate; IV, intravenous; Neg, negative.
Discussion
IV peramivir and IV zanamivir are 2 new antiviral agents that treat severe influenza infection. Clinical experience with the emergence of resistance with these 2 drugs is limited. To date, >200 cases of oseltamivir-resistant pH1N1 have been documented around the world and all sequenced isolates had the same neuraminidase H275Y mutation (8). The H275Y mutation increases the 50% minimal inhibitory concentration (IC50) of oseltamivir from 230- to 2207-fold and the IC50 of peramivir 66- to 831-fold, depending on the functional neuraminidase inhibitor assay used (9). Clinical failures have been described with both drugs even when plasma concentrations are higher than the IC50 of the resistant virus (10).
Most mutant isolates have been selected by oseltamivir in immunocompromised hosts (11). There are some data available on H275Y mutant virus evolution under oseltamivir treatment but few under peramivir treatment (10, 12). In our patient, oseltamivir use was not associated with significant development of resistance but the H275Y mutation appeared to be selected during IV peramivir therapy. We could not prove that the virus was still wild-type in the nasal wash before starting peramivir, as the only specimen available for testing was from BAL. However, to date, discrepancy between upper and lower respiratory tract specimens in regards to resistance has not been described. It is possible that the patient developed early resistance while being treated with oseltamivir; if so, any mutant populations would have been below the level of detection of currently available resistance assays (<10% mutant). This case highlights the fact that an H275Y mutant population can emerge early and replicate in vivo under peramivir antiviral pressure to potentially become the major viral population.
Under-dosing may be another important cause for emerging resistance. Blood levels were not assessed in our case report, as oseltamivir and peramivir levels are not currently available in most clinical laboratories. However, pharmacokinetic analyses performed in critically ill patients have shown that oral oseltamivir administered 75 mg twice a day was enough to achieve plasma concentrations 2000- to 4000-fold higher than the IC50 of the pH1N1 virus (13). These data suggest that oseltamivir levels at the beginning of therapy were unlikely to be the driving force in the development of H275Y mutation. The patient in this study was given a loading dose of peramivir, and then dosing was adjusted for renal function, suggesting that plasma area under the curve should have been >80 µg*h/mL (14).
Serial testing for influenza resistance is recommended in all immunocompromised patients who continue to be symptomatic, and ideally should be started as soon as 5 days after beginning anti-influenza therapy. Cycle thresholds or viral loads may be useful, as in this case, to follow those receiving antiviral therapy and to screen for developing resistance. Figure 1 shows the evolution of viral loads and the development of mutant population percentages over time. During IV zanamivir treatment, the percentage of the mutant population continued to diminish in favor of wild-type population. While this could not be assessed in the laboratory, impaired fitness in the mutant virus is suggested by the decline of mutant population once antiviral pressure was switched from oseltamivir/peramivir to zanamivir, which should be equally effective against mutant and wild-type viruses. In vitro studies have shown decreased fitness in seasonal H1N1 with acquired H275Y mutation as well as in oseltamivir-resistant pH1N1 (15–16). Fitness recovery could be associated with improved transmissibility of resistant virus and lead to major clinical and public health concerns. Limited data are available on the impact of oseltamivir resistance on clinical symptoms and treatment in the community (17–20), and even less is known about the role of antiviral prophylaxis and containment in the context of oseltamivir-resistant viral strains (21).
Pyrosequencing, the molecular gold standard method for resistance testing, is time consuming, expensive, and is not clinically available at most centers. While pyrosequencing has the ability to determine multiple mutations at the same time, minor mutant populations of <10% can be missed (7). ASPCR is a PCR genotyping method that gives sensitive results, can be performed rapidly within a few hours, and may be an important diagnostic tool for determining resistance during influenza therapy (5). Unfortunately, this genotyping method identifies only pre-specified mutations and therefore misses other rare or novel mutations. Complete neuraminidase sequencing may have identified other mutations associated with oseltamivir or peramivir resistance that were missed by ASPCR in our case report. However, the H275Y mutation has been shown to play a major role in the development of oseltamivir resistance and has been shown to be equally important for peramivir resistance in in vitro studies (4). In the future, additional quantitative assessments are necessary to better understand H275Y mutant viral kinetics in vivo. Because viral culture tends to select viral subspecies, direct specimen testing with molecular assays may provide better quantitative analysis of viral populations in infected patients (22).
In conclusion, molecular methods for quantitative resistance testing highlighted the early development of an H275Y mutation during IV peramivir therapy and the subsequent decline of the mutant population under IV zanamivir therapy. This case also suggests that caution is needed when using peramivir in the presence of H275Y mutation. The absence of clinical response or virologic improvement after the institution of peramivir should prompt resistance testing, and if found, a change to zanamivir should be considered. This case also suggests that caution is needed when using peramivir in the presence of H275Y mutation. More data are needed on the use of combination antiviral regimens and their potential effect on the emergence of the H275Y mutation (23).
Acknowledgments
The authors would like to thank Anne Cent and the University of Washington Clinical Virology Laboratory for assistance with sample collection.
Funding Sources: National Institute of Health (NIH) grants CA-18029 and CA-15704. M.B. is funded through NIH grant K24HL093294, and S.P. is funded through NIH grant K23HL096831 and an ASBMT/Viropharma New Investigator Award.
Footnotes
Conflicts of interest: J.E. received research support from Adamas, Novartis, MedImmune, and Sanofi Pasteur. M.B. received grant support from Adamas and Roche, is a consultant for Roche and Novartis, and has received speaking fees from Roche. All other authors have no conflicts.
References
- 1.Redelman-Sidi G, Sepkowitz KA, Huang CK, et al. 2009 H1N1 influenza infection in cancer patients and hematopoietic stem cell transplant recipients. J Infect. 2010;60(4):257–263. doi: 10.1016/j.jinf.2010.01.009. [DOI] [PubMed] [Google Scholar]
- 2.Kharfan-Dabaja MA, Velez A, Richards K, Greene JN, Field T, Sandin R. Influenza A/pandemic 2009/H1N1 in the setting of allogeneic hematopoietic cell transplantation: a potentially catastrophic problem in a vulnerable population. Int J Hematol. 2010;91(1):124–127. doi: 10.1007/s12185-009-0464-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Birnkrant D, Cox E. The Emergency Use Authorization of peramivir for treatment of 2009 H1N1 influenza. N Engl J Med. 2009;361(23):2204–2207. doi: 10.1056/NEJMp0910479. [DOI] [PubMed] [Google Scholar]
- 4.Baz M, Abed Y, Boivin G. Characterization of drug-resistant recombinant influenza A/H1N1 viruses selected in vitro with peramivir and zanamivir. Antiviral Res. 2007;74(2):159–162. doi: 10.1016/j.antiviral.2006.10.012. [DOI] [PubMed] [Google Scholar]
- 5.Liu CM, Driebe EM, Schupp J, et al. Rapid quantification of single-nucleotide mutations in mixed influenza A viral populations using allele-specific mixture analysis. J Virol Methods. 2010;163(1):109–115. doi: 10.1016/j.jviromet.2009.09.007. [DOI] [PubMed] [Google Scholar]
- 6.Renaud C, Kuypers J, Corey L. Diagnostic accuracy of an allele-specific reverse transcriptase-PCR assay targeting the H275Y oseltamivir resistant mutation in 2009 pandemic influenza A/H1N1 virus. J Clin Virol. 2010;49(1):21–25. doi: 10.1016/j.jcv.2010.06.019. [DOI] [PubMed] [Google Scholar]
- 7.Deyde VM, Gubareva LV. Influenza genome analysis using pyrosequencing method: current applications for a moving target. Expert Rev Mol Diagn. 2009;9(5):493–509. doi: 10.1586/erm.09.21. [DOI] [PubMed] [Google Scholar]
- 8.World Health Organizaiton (WHO) Update on oseltamivir-resistant pandemic A (H1N1) 2009 influenza virus: January 2010. Weekly Epidemiological Record on pandemic (H1N1) 2009. 2010;85(6):3.
- 9.Nguyen HT, Sheu TG, Mishin VP, Klimov AI, Gubareva LV. Assessment of pandemic and seasonal influenza A (H1N1) virus susceptibility to neuraminidase inhibitors in three enzyme activity inhibition assays. Antimicrob Agents Chemother. 2010;54(9):3671–3677. doi: 10.1128/AAC.00581-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Memoli MJ, Hrabal RJ, Hassantoufighi A, Eichelberger MC, Taubenberger JK. Rapid selection of oseltamivir- and peramivir-resistant pandemic H1N1 virus during therapy in 2 immunocompromised hosts. Clin Infect Dis. 2010;50(9):1252–1255. doi: 10.1086/651605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Oseltamivir-resistant novel influenza A (H1N1) virus infection in two immunosuppressed patients - Seattle, Washington, 2009. MMWR Morb Mortal Wkly Rep. 2009;58(32):893–896. [PubMed] [Google Scholar]
- 12.Gaur AH, Bagga B, Barman S, et al. Intravenous zanamivir for oseltamivir-resistant 2009 H1N1 influenza. N Engl J Med. 362(1):88–89. doi: 10.1056/NEJMc0910893. [DOI] [PubMed] [Google Scholar]
- 13.Ariano RE, Sitar DS, Zelenitsky SA, et al. Enteric absorption and pharmacokinetics of oseltamivir in critically ill patients with pandemic (H1N1) influenza. CMAJ. 2010;182(4):357–363. doi: 10.1503/cmaj.092127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Mancuso CE, Gabay MP, Steinke LM, Vanosdol SJ. Peramivir: an intravenous neuraminidase inhibitor for the treatment of 2009 H1N1 influenza. Ann Pharmacother. 2010;44(7–8):1240–1249. doi: 10.1345/aph.1P031. [DOI] [PubMed] [Google Scholar]
- 15.Baz M, Abed Y, Simon P, Hamelin ME, Boivin G. Effect of the neuraminidase mutation H274Y conferring resistance to oseltamivir on the replicative capacity and virulence of old and recent human influenza A (H1N1) viruses. J Infect Dis. 2010;201(5):740–745. doi: 10.1086/650464. [DOI] [PubMed] [Google Scholar]
- 16.Duan S, Boltz DA, Seiler P, et al. Oseltamivir-Resistant Pandemic H1N1/2009 Influenza Virus Possesses Lower Transmissibility and Fitness in Ferrets. PLoS Pathog. 2010;6(7) doi: 10.1371/journal.ppat.1001022. e1001022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Matsuzaki Y, Mizuta K, Aoki Y, et al. A two-year survey of the oseltamivir-resistant influenza A (H1N1) virus in Yamagata, Japan and the clinical effectiveness of oseltamivir and zanamivir. Virol J. 2010;7:53. doi: 10.1186/1743-422X-7-53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Tamura D, Mitamura K, Yamazaki M, et al. Oseltamivir-resistant influenza a viruses circulating in Japan. J Clin Microbiol. 2009;47(5):1424–1427. doi: 10.1128/JCM.02396-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ujike M, Shimabukuro K, Mochizuki K, et al. Oseltamivir-resistant influenza viruses A (H1N1) during 2007–2009 influenza seasons Japan. Emerg Infect Dis. 2010;16(6):926–935. doi: 10.3201/eid1606.091623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Saito R, Sato I, Suzuki Y, et al. Reduced Effectiveness of Oseltamivir in Children Infected With Oseltamivir-Resistant Influenza A (H1N1) Viruses With His275Tyr Mutation. Pediatr Infect Dis J. 2010;29(10):898–904. doi: 10.1097/INF.0b013e3181de9d24. [DOI] [PubMed] [Google Scholar]
- 21.Lackenby A, Thompson CI, Democratis J. The potential impact of neuraminidase inhibitor resistant influenza. Curr Opin Infect Dis. 2008;21(6):626–638. doi: 10.1097/QCO.0b013e3283199797. [DOI] [PubMed] [Google Scholar]
- 22.Okomo-Adhiambo M, Nguyen HT, Sleeman K, et al. Host cell selection of influenza neuraminidase variants: implications for drug resistance monitoring in A (H1N1) viruses. Antiviral Res. 2010;85(2):381–388. doi: 10.1016/j.antiviral.2009.11.005. [DOI] [PubMed] [Google Scholar]
- 23.Nguyen JT, Hoopes JD, Le MH, et al. Triple combination of amantadine, ribavirin, and oseltamivir is highly active and synergistic against drug resistant influenza virus strains in vitro. PLoS One. 2010;5(2):e9332. doi: 10.1371/journal.pone.0009332. [DOI] [PMC free article] [PubMed] [Google Scholar]