ABSTRACT
BACKGROUND
There has been considerable focus on the burden of mental illness (including post-traumatic stress disorder, PTSD) in returning Operation Enduring Freedom/Operation Iraqi Freedom (OEF/OIF) veterans, but little attention to the burden of medical illness in those with PTSD.
OBJECTIVES
(1) Determine whether the burden of medical illness is higher in women and men OEF/OIF veterans with PTSD than in those with No Mental Health Conditions (MHC). (2) Identify conditions common in those with PTSD.
DESIGN
Cross-sectional study using existing databases (Fiscal Year 2006–2007).
SETTING
Veterans Health Administration (VHA) patients nationally.
PATIENTS
All 90,558 OEF/OIF veterans using VHA outpatient care nationally, categorized into strata: PTSD, Stress-Related Disorders, Other MHCs, and No MHC.
MEASUREMENTS
(1) Count of medical conditions; (2) specific medical conditions (from ICD9 codes, using Agency for Health Research and Quality’s Clinical Classifications software framework).
MAIN RESULTS
The median number of medical conditions for women was 7.0 versus 4.5 for those with PTSD versus No MHC (p < 0.001), and for men was 5.0 versus 4.0 (p < 0.001). For PTSD patients, the most frequent conditions among women were lumbosacral spine disorders, headache, and lower extremity joint disorders, and among men were lumbosacral spine disorders, lower extremity joint disorders, and hearing problems. These high frequency conditions were more common in those with PTSD than in those with No MHC.
CONCLUSIONS
Burden of medical illness is greater in women and men OEF/OIF veteran VHA users with PTSD than in those with No MHC. Health delivery systems serving them should align clinical program development with their medical care needs.
Electronic supplementary material
The online version of this article (doi:10.1007/s11606-010-1497-4) contains supplementary material, which is available to authorized users.
KEY WORDS: stress disorders, post-traumatic, veterans, Afghan campaign 2001-, Iraq War 2003-, women
INTRODUCTION
In response to recent attention to high rates of post-traumatic stress disorder (PTSD) in soldiers returning from Operation Enduring Freedom/Operation Iraqi Freedom (OEF/OIF), there have been considerable efforts to characterize their burden of mental illness.1–3 However, general medical care needs of OEF/OIF veterans with PTSD have not been characterized.
Excess burden of medical illness in returning veterans with PTSD is likely. Serious medical comorbidity (cardiovascular disease, chronic pain, etc.) has been documented among veterans of other eras with PTSD.4 Potential mechanisms include neuroendocrine dysregulation, tissue injury, health risk behaviors, and quality of care.4–6
Lack of information about the relationship between PTSD and medical illness in the newest generation of veterans represents a serious gap. First, their deployment experience (e.g., exposure to improvised explosive devices, heavy body armor, etc.) differs from that of veterans of earlier eras. Second, prior studies examining the relationship between PTSD and medical conditions have typically focused on patients with remote trauma exposure. Shifting the focus to recently returned veterans spotlights opportunities for intervention in younger veterans for whom late effects of chronic illness might still be averted.
Women could manifest stress-related consequences of deployment in distinct ways.7 For example, hormone differences could modulate neuroendocrine stress responses. Occupational duties or sexual trauma exposure during service8 and family roles after return from war differ by gender, potentially impacting both PTSD severity and health. An understanding of the health needs of this rapidly expanding sector of the armed services is critical.9
Therefore, we examined whether burden of medical illness is heavier in women and men Veterans Health Administration (VHA) OEF/OIF veteran patients with PTSD than in those without mental illness. Secondary analyses described medical conditions contributing to the burden of illness in women and men with PTSD.
METHODS
Overview of Study Design and Data Sources
In this cross-sectional, national study of all OEF/OIF veteran users of VHA outpatient care in Fiscal Year 2006–2007 (FY06–FY07), we examined the burden of medical illness as a function of PTSD status. Data came from VHA’s National Patient Care Database (NPCD) (centralized clinical/administrative data for all VHA patients), linked to OEF/OIF Roster data.10 The Institutional Review Board, Stanford University, approved this study.
Subjects
From the 281,170 individuals in the OEF/OIF Roster as of December 2006, we selected the 100,402 who received face-to-face VHA outpatient care at least once in both FY06 and FY07, reasoning that patients who received VHA care twice within a 2-year interval were VHA patients (i.e., they had not only presented for a one-time VHA enrollment exam). Among them, we selected confirmed veterans of OEF/OIF, with a valid service end date in the range September 11, 2001–September 30, 2006, and with confirmed gender, leaving an analytic cohort of N = 90,558.
Variables
General Approach to Identification of Diagnoses
The independent variable (PTSD status) and dependent variables (specific medical conditions) represent clinician-diagnosed conditions/symptoms, identified from International Classification of Diseases, 9th Edition (ICD9) diagnosis codes. We used the Agency for Health Research and Quality’s (AHRQ) Clinical Classifications Software (CCS) framework to map ICD9 codes to conditions; specific conditions group into broad categories.11
We selected a 2-year diagnosis ascertainment window (FY06-FY07) for two reasons. First, we expected this to have better sensitivity for detecting conditions than a 1-year window. Second, since some patients could have joined VHA in late FY06, we wanted to include patients for whom an additional year of data (FY07) was available, i.e., for whom there likely was sufficient opportunity to have identified a diagnosis, if present.
Independent Variable: PTSD Status
The independent variable was “PTSD status,” representing four mutually exclusive groups: PTSD, Stress-Related Disorders (SRD), Other Mental Health Conditions (MHC), or No MHC. Patients were considered to have PTSD if they had at least one instance of diagnosed PTSD (ICD9 309.81). Concerns have been raised about under-diagnosis of PTSD in primary care settings12 and about sub-clinical PTSD13 in patients who have experienced severe stressors. This could be a particularly important issue for recently returned veterans still undergoing diagnostic assessment. Therefore, patients not meeting the “PTSD” criterion were considered to have SRD if they had at least one instance of Acute Stress Disorder (ICD9 308.xx) or Adjustment Disorder (ICD9 309.xx except 309.21, 309.81). Patients without PTSD or SRD were considered to have Other MHC if they had at least one ICD9 code in any of the following categories (derived from CCS, with minor modifications) (Online Appendix 1): other anxiety, depressive, psychotic, bipolar, alcohol/drug use, personality, conduct/impulse control, eating, dissociative, psychogenic, and other miscellaneous mental disorders. Patients not meeting criteria for PTSD, SRD, or Other MHC were considered to have No MHC, the reference group for all analyses.
Dependent Variables: Medical Conditions
The 15 CCS medical condition categories examined were: infectious diseases; neoplasms; endocrine/metabolic; hematologic; neurologic/sense organs; circulatory; respiratory; digestive; genitourinary; pregnancy-related; dermatologic; musculoskeletal; injury; symptoms, signs and ill-defined conditions; and other. Within these categories, we made minor modifications to the CCS approach to identify 222 specific conditions.
A patient was considered to have 1 of the 15 categories of medical conditions if he/she had at least one instance of an ICD9 code falling into that condition category at a face-to-face outpatient visit in FY06 or FY07. E codes (external causes of injury) and V codes (treatments/factors influencing health) were not included as diagnoses.
A patient was considered to have one of the 222 medical conditions if he/she had at least one ICD9 code mapping to that condition associated with a face-to-face outpatient visit in FY06 or FY07. A summary “counter” variable indicated total number of medical conditions, from 0–222 (truncated at 25+).
Other Variables
Sex, age, race/ethnicity, and service-connected disability status came from NPCD (supplemented with OEF/OIF Roster data), year of military separation came from the Roster, and utilization came from clinic type “stop codes” in NPCD. Specifications for stop codes representing face-to-face outpatient visits (i.e., not Telephone Care, Laboratory, or Radiology encounters) and stop codes representing Primary Care are listed in Online Appendices 4 and 5.
Analysis
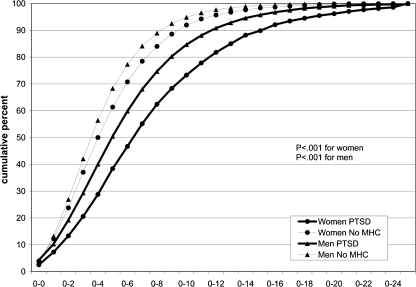
Since prevalence of medical conditions and PTSD differ by gender, all analyses were gender-stratified. Data are shown for all four “PTSD status” subgroups, but the primary focus was on comparing the PTSD subgroup with the No MHC subgroup within each gender.
Main Analyses: Burden of Medical Illness
We compared median count of medical conditions for women (and, separately, for men) with PTSD versus No MHC using the Wilcoxon Mann-Whitney test. We then created Empirical Distribution Function (EDF) curves representing proportion of patients with 0, 0–1, 0–2, …, 0–25+ medical conditions, comparing curves for women with PTSD vs. women with No MHC and for men with PTSD vs. men with No MHC using the Komolgorov-Smirnov test.14
Secondary Analyses: Types of Medical Illness
We calculated proportion within each of the 15 categories/222 conditions by PTSD status by gender. We also calculated the age-adjusted odds ratios (AOR) (and 95% confidence interval) for having the category/ condition as a function of PTSD status (PTSD versus No MHC), by gender.
Sensitivity Analyses
We conducted a series of sensitivity analyses to test stability of core findings to varying assumptions. We repeated analyses examining condition counts in patients with PTSD versus No MHC, varying specific assumptions as follows, while leaving other assumptions unchanged. Sensitivity Analysis 1: To address the possibility that some patients without PTSD (e.g., subthreshold PTSD or non-persistent PTSD) are included in the PTSD group, we required at least one instance of a PTSD diagnosis in FY06 and again in FY07 for a patient to be considered to have PTSD. Sensitivity Analysis 2: To address possible under-detection of PTSD and under-detection of medical conditions among patients who made few visits to VHA (e.g., new users or those receiving most care outside VHA), we limited our cohort to patients who were regular VHA users throughout the study period, i.e., who had ≥2 primary care visits in FY06 and ≥2 primary care visits in FY07. Sensitivity Analysis 3: To address the possibility that some ICD9 codes may be entered erroneously, we required at least two instances of an ICD9 code in FY06-FY07 to qualify for a condition. Sensitivity Analysis 4: To address the possibility that some diagnoses may be coded with E or V codes, we allowed these codes to qualify towards condition counts.
RESULTS
Among the 12,831 OEF/OIF women veterans, 27.3% had PTSD, 7.6% SRD, 17.1% Other MHC, and 48.0% No MHC. Among the 77,727 men, 34.8% had PTSD, 6.1% SRD, 11.9% Other MHC, and 47.1% No MHC. Thus, the majority of these VHA users had an MHC.
Table 1 shows characteristics for women and men by PTSD status. Nearly all had used VHA primary care services. The mean number of primary care visits across the 2-year period (FY06-FY07) for women with PTSD vs. No MHC was 6.7 vs. 4.6 (P < 0.001), and for men was 4.7 vs. 3.4 (P < 0.001).
Table 1.
Characteristics of OEF/OIF Veteran VHA Patients, by PTSD Status and Gender (N = 90,558)*
| Women | Men | |||||||
|---|---|---|---|---|---|---|---|---|
| PTSD | SRD | Other MHC | No MHC | PTSD | SRD | Other MHC | No MHC | |
| N | 3,501 | 981 | 2,189 | 6,160 | 27,083 | 4,748 | 9,259 | 36,637 |
| Sociodemographics | ||||||||
| Age groups, % | ||||||||
| <25 years | 22.2 | 26.7 | 21.9 | 25.9 | 22.1 | 20.2 | 18.8 | 18.8 |
| 25–29 years | 29.6 | 32.1 | 36.1 | 35.0 | 28.0 | 26.2 | 30.2 | 26.6 |
| 30–34 years | 14.4 | 12.3 | 14.3 | 12.0 | 13.5 | 12.7 | 12.5 | 11.2 |
| 35–39 years | 12.1 | 9.5 | 9.4 | 7.9 | 12.1 | 11.9 | 9.8 | 10.3 |
| 40+ years | 21.7 | 19.4 | 18.3 | 19.2 | 24.3 | 29.0 | 28.9 | 33.0 |
| Race/ethnicity, % | ||||||||
| White | 50.5 | 53.5 | 57.0 | 48.0 | 66.9 | 64.6 | 67.5 | 64.0 |
| Black | 34.3 | 30.1 | 27.3 | 34.0 | 17.0 | 16.5 | 14.4 | 17.8 |
| Hispanic | 9.9 | 10.4 | 10.8 | 11.3 | 11.3 | 13.8 | 13.4 | 12.5 |
| Other | 3.1 | 2.7 | 2.8 | 3.1 | 2.1 | 2.5 | 2.2 | 2.4 |
| Unknown | 2.2 | 3.0 | 2.1 | 3.5 | 2.6 | 2.5 | 2.4 | 3.2 |
| Service-connected disability status, % † | ||||||||
| Not service-connected | 28.3 | 47.5 | 37.7 | 49.2 | 26.8 | 47.6 | 42.1 | 47.8 |
| SC 0–40% | 34.1 | 37.9 | 39.0 | 39.7 | 34.6 | 37.1 | 37.6 | 39.8 |
| SC 50%+ | 37.6 | 14.6 | 23.3 | 11.1 | 38.5 | 15.2 | 20.3 | 12.3 |
| Military characteristics | ||||||||
| Separated from military prior to FY06,% | 74.4 | 65.1 | 74.3 | 69.9 | 68.2 | 59.1 | 71.7 | 65.3 |
| Use of VHA care | ||||||||
| Used VHA prior to FY06, % ‡ | 66.2 | 60.8 | 63.0 | 57.4 | 56.6 | 50.7 | 59.0 | 52.6 |
| Count of VHA primary care visits in FY06–07, % | ||||||||
| 0 | 2.0 | 2.2 | 2.1 | 3.4 | 4.1 | 4.4 | 4.4 | 5.0 |
| 1 | 4.6 | 4.0 | 5.0 | 7.3 | 9.5 | 10.2 | 10.0 | 11.6 |
| 2 | 9.7 | 11.6 | 11.7 | 16.8 | 14.8 | 17.2 | 17.5 | 24.8 |
| 3 | 10.3 | 11.3 | 14.1 | 16.8 | 16.0 | 16.9 | 17.3 | 20.5 |
| 4 | 12.1 | 12.5 | 13.5 | 15.1 | 13.9 | 14.9 | 14.0 | 14.0 |
| 5 | 10.5 | 11.6 | 11.9 | 11.5 | 10.8 | 11.0 | 10.9 | 9.2 |
| 6+ | 50.8 | 46.7 | 41.8 | 29.2 | 31.0 | 25.4 | 25.9 | 14.8 |
Abbreviations: OEF/OIF, Operation Enduring Freedom/Operation Iraqi Freedom; PTSD, post-traumatic stress disorder; SRD, stress-related disorder; MHC, mental health condition; VHA, Veterans Health Administration; FY, fiscal year; SC, service-connected disability
*This table is descriptive; p-values are not shown
†The means test variable in VHA administrative records classified patients as service-connected (<50% or 50%+ rating) or non-service-connected (i.e., without any service-related disability rating).
‡Use of VHA prior to FY06: any use of VHA outpatient services in FY02–FY05
Burden of Illness
The median number of medical conditions for those with PTSD, SRD, Other MHC, and No MHC was 7.0, 6.0, 6.0, and 4.5, respectively, for women and 5.0, 5.0, 5.0, and 4.0, respectively, for men (for both genders, p < 0.001 for PTSD versus No MHC, for SRD versus No MHC, and for Other MHC versus No MHC). (Note, among those with PTSD, women had a higher median number of medical conditions than did men, p < 0.001.) The EDF curve (Fig. 1) likewise confirmed a higher number of medical conditions in those with PTSD than in those with No MHC. Specifically, for both women and men, at every level of cumulative percent of population (y-axis), patients with PTSD had accumulated more conditions than had patients with No MHC.
Figure 1.
Cumulative medical condition count, by PTSD status by gender. Abbreviations: PTSD, post-traumatic stress disorder; MHC, mental health condition.
Conditions Common in Patients with PTSD
Table 2 characterizes rates of each condition in women and men with PTSD, benchmarked against rates in those with SRD, Other MHC, or No MHC. (Only conditions with prevalence ≥10% in women or men with PTSD or SRD are included in Table 2; the full list is in Online Appendix 2.) Traumatic brain injury (TBI) did not fall in the top 10%, but was common: aggregating the category “organic brain syndromes, coma, brain damage” with the category “intracranial injury,” prevalence of diagnosed TBI for patients with PTSD, SRD, Other MHC, and No MHC was 4.5%, 1.2%, 1.3%, and 0.7% for women, and 8.5%, 4.1%, 2.9%, and 1.2% for men, respectively. After age adjustment, all of the 20 most frequent conditions in women/men with PTSD were significantly more common in those with PTSD.
Table 2.
Medical Condition Categories and Specific Conditions: Gender-Stratified Frequency by PTSD Status, and Age-Adjusted OR (PTSD vs No MHC)
| Frequency of medical conditions, %† | Age-adjusted odds ratio (CI)‡ | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Women | Men | Women | Men | |||||||
| Category/ condition* | PTSD | SRD | Other MHC | No MHC | PTSD | SRD | Other MHC | No MHC | PTSD vs No MHC | PTSD vs No MHC |
| N | 3,501 | 981 | 2,189 | 6,160 | 27,083 | 4,748 | 9,259 | 36,637 | ||
| Infectious diseases | 22.3 | 22.8 | 19.2 | 17.8 | 16.6 | 17.2 | 16.8 | 15.4 | 1.36 (1.23, 1.51) | 1.08 (1.03, 1.12) |
| Neoplasms | 11.5 | 12.6 | 10.9 | 10.4 | 6.2 | 7.2 | 6.4 | 6.3 | 1.05 (0.92, 1.21) | 1.08 (1.01, 1.16) |
| Endocrine-metabolic | 36.7 | 33.9 | 33.7 | 27.0 | 35.8 | 37.0 | 38.0 | 35.3 | 1.49 (1.36, 1.64) | 1.18 (1.14, 1.22) |
| Overweight/ obesity | 18.6 | 15.2 | 16.8 | 12.3 | 13.5 | 14.4 | 13.7 | 11.9 | 1.58 (1.41, 1.77) | 1.22 (1.16, 1.28) |
| Hyperlipidemia | 14.5 | 14.4 | 12.2 | 10.3 | 24.1 | 24.1 | 26.0 | 24.8 | 1.37 (1.20, 1.56) | 1.15 (1.10, 1.19) |
| Hematologic | 8.0 | 8.1 | 6.4 | 6.7 | 2.2 | 2.3 | 2.6 | 2.2 | 1.16 (0.99, 1.36) | 1.05 (0.94, 1.17) |
| Neurologic/ sense organs | 60.0 | 54.8 | 50.9 | 42.0 | 55.6 | 51.1 | 46.8 | 41.1 | 2.03 (1.86, 2.21) | 1.91 (1.85, 1.97) |
| Headache, including migraine | 32.7 | 26.0 | 25.3 | 17.6 | 17.4 | 12.5 | 11.6 | 7.4 | 2.27 (2.06, 2.50) | 2.63 (2.50, 2.76) |
| Hearing problems | 13.4 | 10.3 | 7.5 | 7.3 | 26.6 | 22.4 | 16.4 | 16.6 | 1.92 (1.68, 2.21) | 1.91 (1.84, 1.98) |
| Vision defects | 19.5 | 19.1 | 14.5 | 12.4 | 16.1 | 16.1 | 14.6 | 11.8 | 1.64 (1.46, 1.84) | 1.60 (1.52, 1.67) |
| Circulatory | 26.8 | 22.4 | 22.6 | 18.7 | 30.1 | 30.1 | 32.6 | 27.9 | 1.51 (1.36, 1.67) | 1.29 (1.25, 1.34) |
| Hypertension | 12.9 | 9.4 | 9.7 | 8.6 | 20.2 | 19.3 | 22.2 | 19.5 | 1.48 (1.28, 1.70) | 1.24 (1.19, 1.30) |
| Respiratory | 43.8 | 43.2 | 40.8 | 33.8 | 31.7 | 32.3 | 33.1 | 27.1 | 1.52 (1.40, 1.66) | 1.26 (1.21, 1.30) |
| Acute upper respiratory tract infections | 18.9 | 19.9 | 18.6 | 13.2 | 10.3 | 10.9 | 11.3 | 8.6 | 1.57 (1.40, 1.76) | 1.17 (1.11, 1.23) |
| Allergic and other chronic sinusitis/ rhinitis | 20.9 | 21.8 | 18.6 | 16.9 | 14.1 | 14.5 | 14.8 | 13.1 | 1.27 (1.14, 1.41) | 1.12 (1.07, 1.17) |
| Digestive | 49.4 | 45.8 | 44.1 | 38.8 | 47.6 | 49.3 | 45.6 | 41.4 | 1.51 (1.38, 1.64) | 1.33 (1.29, 1.38) |
| Dental disorders | 26.7 | 24.7 | 21.3 | 22.4 | 22.8 | 26.8 | 19.4 | 21.2 | 1.24 (1.13, 1.37) | 1.11 (1.07, 1.16) |
| Esophageal disorders | 16.3 | 12.8 | 14.3 | 8.5 | 17.5 | 16.2 | 17.2 | 12.2 | 2.02 (1.78, 2.29) | 1.65 (1.58, 1.73) |
| Diarrhea, constipation and functional bowel disorders | 13.1 | 11.3 | 10.6 | 6.2 | 8.1 | 6.0 | 6.1 | 3.8 | 2.26 (1.96, 2.61) | 2.23 (2.08, 2.39) |
| Genitourinary | 55.6 | 55.1 | 53.2 | 48.9 | 12.9 | 13.1 | 13.7 | 11.1 | 1.32 (1.21, 1.43) | 1.27 (1.21, 1.33) |
| Urinary tract infection | 10.4 | 8.7 | 11.2 | 7.8 | 1.6 | 1.9 | 1.9 | 1.6 | 1.44 (1.25, 1.67) | 0.92 (0.81, 1.05) |
| Vaginitis, cervicitis, other pelvic inflammatory conditions | 16.2 | 16.6 | 15.6 | 14.4 | N/A | N/A | N/A | N/A | 1.19 (1.06, 1.33) | N/A |
| Menstrual disorders | 18.6 | 18.9 | 17.5 | 14.8 | N/A | N/A | N/A | N/A | 1.34 (1.20, 1.50) | N/A |
| Cervical dysplasia and ASCUS | 12.9 | 16.3 | 14.3 | 14.8 | N/A | N/A | N/A | N/A | 0.93 (0.82, 1.05) | N/A |
| Other female genital disorders | 10.9 | 10.0 | 9.0 | 7.8 | N/A | N/A | N/A | N/A | 1.44 (1.25, 1.65) | N/A |
| Pregnancy-related conditions | 2.4 | 2.1 | 1.9 | 1.5 | N/A | N/A | N/A | N/A | 1.70 (1.26, 2.29) | N/A |
| Dermatologic | 28.2 | 27.7 | 27.7 | 23.1 | 22.1 | 23.0 | 20.8 | 19.3 | 1.31 (1.19, 1.44) | 1.18 (1.14, 1.23) |
| Musculoskeletal | 71.6 | 67.5 | 63.1 | 55.6 | 71.6 | 67.9 | 63.2 | 60.6 | 1.95 (1.78, 2.13) | 1.71 (1.65, 1.77) |
| Joint disorders, upper extremity | 14.4 | 12.1 | 10.7 | 8.1 | 16.7 | 15.7 | 13.7 | 12.6 | 1.82 (1.60, 2.08) | 1.44 (1.38, 1.51) |
| Joint disorders, lower extremity | 32.3 | 28.0 | 24.4 | 22.6 | 28.3 | 25.8 | 22.1 | 21.7 | 1.60 (1.45, 1.75) | 1.44 (1.39, 1.50) |
| Joint disorders, unspecified or multiple joints | 18.2 | 14.0 | 13.9 | 10.3 | 17.5 | 15.2 | 14.6 | 12.9 | 1.84 (1.63, 2.08) | 1.60 (1.53, 1.67) |
| Tendonitis, bursitis, myalgia, and other soft tissue conditions | 30.4 | 27.8 | 22.4 | 18.0 | 23.2 | 21.6 | 19.1 | 17.1 | 1.93 (1.75, 2.13) | 1.54 (1.48, 1.60) |
| Cervical spine disorders | 13.6 | 11.1 | 8.6 | 7.3 | 10.4 | 9.1 | 8.5 | 6.1 | 1.93 (1.69, 2.22) | 1.91 (1.81, 2.03) |
| Lumbosacral spine disorders | 38.2 | 36.0 | 30.5 | 24.9 | 40.6 | 37.0 | 33.5 | 27.7 | 1.83 (1.67, 2.00) | 1.82 (1.76, 1.88) |
| Injury | 33.6 | 27.4 | 23.0 | 19.0 | 34.1 | 29.5 | 25.4 | 23.9 | 2.13 (1.94, 2.34) | 1.60 (1.54, 1.65) |
| Joint injuries, lower extremity | 10.2 | 8.9 | 6.8 | 6.8 | 9.8 | 9.1 | 7.1 | 7.6 | 1.54 (1.33, 1.79) | 1.30 (1.23, 1.37) |
| Symptoms, ill-defined conditions | 30.8 | 29.6 | 28.0 | 21.8 | 17.3 | 16.0 | 16.9 | 13.5 | 1.61 (1.46, 1.77) | 1.34 (1.28, 1.40) |
| Abdominal pain | 12.3 | 10.5 | 11.0 | 7.5 | 5.2 | 4.2 | 5.3 | 3.3 | 1.76 (1.53, 2.03) | 1.61 (1.48, 1.74) |
| Residual codes/other | 22.7 | 18.0 | 19.3 | 8.7 | 26.5 | 24.0 | 20.8 | 12.4 | 3.00 (2.66, 3.38) | 2.76 (2.65, 2.88) |
| Sleep disturbance | 14.7 | 11.4 | 12.4 | 3.9 | 19.8 | 18.1 | 14.7 | 7.8 | 4.09 (3.49, 4.80) | 3.15 (3.00, 3.31) |
*Medical condition categories are shown in bold. Specific medical conditions are in regular type face only specific conditions with frequency ≥10% are displayed
†The 15 most frequent conditions in women and men with PTSD are shown in italics. Data on frequency of categories and conditions by PTSD status are descriptive; p-values are not shown
‡Statistically significant AORs are shown in bold. AOR > 1 indicates that those with PTSD are more likely than those with no mental health conditions to have been diagnosed with the specified medical condition; an AOR is statistically significant at p < 0.05 if the CI does not cross 1.0
Abbreviations: PTSD, Post Traumatic Stress Disorder; SRD, Stress-Related Disorder; MHC, Mental Health Condition; ASCUS, Atypical Squamous Cells of Undetermined Significance
Sensitivity Analyses
In each sensitivity analysis, burden of illness was higher in women and men with PTSD than in those with No MHC (Online Appendix 3).
COMMENT
We found that, among both women and men OEF/OIF veterans who use VHA, burden of medical illness (measured as a count of diagnosed conditions) is greater for those with PTSD than for those with no mental health conditions. A number of specific medical conditions are more prevalent among women and men with PTSD than among those without MHC, even after adjusting for age. The most frequent conditions among women with PTSD are lumbosacral spine disorders, headache, lower extremity joint disorders, skin disorders, tendonitis/myalgia, dental disorders, allergies, vision defects, acute upper respiratory tract infections, and overweight/obesity. The most frequent conditions among men with PTSD are lumbosacral spine disorders, lower extremity joint disorders, hearing problems, hyperlipidemia, tendonitis/myalgia, skin disorders, dental disorders, hypertension, sleep disturbance, and other joint disorders.
These findings are aligned with earlier studies, but notable given the younger age and unique war experiences of these veterans. Excess burden of medical illness has been documented in patients with PTSD,4 whether measured by physician-diagnosed conditions15 as in our study or by self-report.15–17 However, most studies have focused on older veterans whose PTSD has presumably been present for decades. A few have examined aspects of this question in recent returnees from the first Gulf War,18–21 and self-reported health status, TBI, self-reported physical symptoms, and primary care use have been examined in OEF/OIF veterans,17,22–24 but we are aware of no prior studies characterizing the relationship between PTSD and the spectrum of clinician-diagnosed medical illness in OEF/OIF veterans. Furthermore, while some have included women, only few have focused on women,16,18,25–27 or described the relationship between PTSD and medical conditions by gender. Particular strengths of our study include its focus upon newly returned veterans, evaluation of not only PTSD but also SRD, assessment of gender differences, comprehensive approach to medical condition assessment, reliance upon physician-diagnosed medical conditions, and national scope.
Women with PTSD had an even greater burden of medical illness than did men with PTSD, perhaps a factor in women’s heavier use of primary care. Leading medical conditions were generally similar in women and men with PTSD, although headache and overweight/obesity ranked higher in women than in men; management of such conditions in women with comorbid PTSD may require novel biopsychosocial approaches to care.
MHCs other than PTSD were also associated with excess burden of medical illness. Concerns about the high rates of PTSD in returning veterans should not detract from attention to the substantial medical care needs of those with other MHCs.
Looking to the future, the need for early intervention is evident. For many of the medical conditions prevalent in veterans with PTSD (e.g., hyperlipidemia, hypertension, obesity), chronic disease management and health behavior interventions reduce risk of adverse long-term outcomes, but are more effective if initiated early in the course of disease. Older veterans in VHA have a heavier burden of medical illness than do their civilian counterparts.28 By recognizing the excess burden of medical illness in recently returned OEF/OIF veterans and addressing their health care needs, the elderly veterans of tomorrow may enjoy better health and functional status.
Study findings need to be interpreted in the context of several caveats. First, PTSD status was determined from ICD9 diagnosis codes. Some without PTSD could have been categorized as having PTSD. However, this is unlikely to occur repeatedly in the medical record, so it is reassuring that the main findings persisted in sensitivity analyses requiring at least two instances of a PTSD diagnosis to qualify as PTSD. A more likely scenario is under-diagnosis of PTSD. We attempted to offset this problem by categorizing PTSD status (PTSD, SRD, Other MHC, No MHC) rather than creating a dichotomous PTSD variable. This allowed us to create a comparison group (No MHC) less likely to be contaminated with true PTSD cases. To the extent that we observed a tendency toward increasing burden of medical illness from PTSD to SRD/Other MHC to No MHC, it appears this strategy may have been successful.
Second, medical conditions were ascertained from ICD9 codes as well. While the use of clinician-diagnosed (rather than self-reported) medical conditions is a strength of the study, under-ascertainment of disease likely occurred for some conditions, especially for under-recognized conditions (e.g., sexual dysfunction). Under-ascertainment of disease could potentially be more common among those with No MHC. For example, if they received more care outside VHA, then providers may have had fewer opportunities to diagnose a medical condition. It is reassuring that the direction of findings did not change in sensitivity analyses when we limited the cohort to regular, frequent users of VHA primary care. Conversely, under-ascertainment of disease could be more common among those with PTSD (e.g., if the presence of PTSD adversely affects a clinician’s ability to attend to other problems during a time-pressured visit).29 This would tend to bias our results toward the null.
Over-ascertainment of medical conditions is also possible. While many of the conditions examined in this study (such as hypertension, hyperlipidemia, obesity) are easily confirmed with objective measurements, others represent subjective symptoms. PTSD can be associated with high rates of somatic symptoms.30 However, regardless of whether they are physiologically or psychologically mediated, somatic symptoms can have a profound adverse effect upon physical health status and quality of life,31 and thus merit serious attention in primary care settings. For this reason, we chose to include symptoms (formally recorded by clinicians with ICD9 codes) in our assessment of overall burden of medical illness. Since diseases and symptoms that are repeatedly a reason for a patient’s visit are likely to be more clinically important, in sensitivity analyses we defined medical conditions more stringently (i.e., requiring that the clinician assigned the patient the same diagnosis at two or more separate visits). Study conclusions did not change, but rates of medical conditions did decrease. This could mean that there was some over-ascertainment of disease using the 1+ diagnosis criterion, that some of the conditions studied were self-limited or intermittent, or that the presence of chronic conditions was not recorded at every visit and thus not detected with the more stringent method.
Third, we studied OEF/OIF veteran VHA patients. Findings may not be generalizable to OEF/OIF veterans who do not use VHA, veterans of other eras, or non-veterans.
CONCLUSIONS
Based on these findings, VHA’s response to the newest generation of returning veterans with PTSD should account for not only their increased mental health services needs, but also their increased medical services needs. Capacity may need to be augmented for the care of certain conditions, including painful musculoskeletal conditions (e.g., physical therapy, pain clinics), conditions potentially related to health behaviors like obesity (e.g., behavioral medicine, nutrition), hearing problems (e.g., audiology), and gender-specific conditions (e.g., women’s health services). Despite the added case complexity associated with presence of co-morbid PTSD, primary care providers will need to fit screening for cardiovascular risk factors (hyperlipidemia, hypertension, smoking) into the visit. Prevalent conditions like sexual dysfunction and sleep problems may require a coordinated effort between medical and mental health providers. Recent re-organization of VHA’s health care delivery system (e.g., patient-centered medical home, mental health providers embedded in primary care settings, tele-mental health initiatives, case management) may prove particularly beneficial for veterans with comorbid PTSD and medical illness. More work is needed to clarify whether the intensity and types of medical services currently received by OEF/OIF veterans with PTSD are well matched to the specific conditions common in this cohort, and whether medical treatments need closer integration with mental health services for this special population newly returned from military service.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Mental Health Condition Specifications (PDF 54.4 KB)
Gender-stratified Frequency of all 222 Medical Conditions, by PTSD Status, in OEF/OIF Veterans Health Administration Patients; Frequency Rank for Women and Men with PTSD (with 1 indicating most frequent); and Age-Adjusted Odds Ratio (PTSD vs No MHC)* (PDF 484 KB)
Cumulative Medical Condition Count by PTSD Status by Gender, Sensitivity Analysis 1-4, truncated at 25 conditions. (PDF 295 KB)
Definition of VA Outpatient Face-to-Face Visits (Technical specifications: clinic “stop” codes used to define face-to-face visits.) (PDF 118 KB)
Definition of Primary Care Clinic Stops. (Technical specifications: Clinic stop codes used to define primary care encounters.) (PDF 13.2 KB)
Acknowledgements
The authors are very grateful to Kristian Gima, BA (National Center for PTSD, VA Palo Alto Health Care System), for his technical contributions, to Ann Thrailkill, RNP, MSN, CNS (Women’s Health Center of Excellence, VA Palo Alto Health Care System), Mark W. Smith PhD (Health Economics Resource Center, VA Palo Alto Health Care System), Jenny Hyun MPH, PhD (National Center for PTSD, VA Palo Alto Health Care System), and Amy Street, PhD (National Center for PTSD, VA Boston Healthcare System) for their contributions to study development, and to Rudolf Moos, PhD (Center for Health Care Evaluation, VA Palo Alto Health Care System, and Department of Psychiatry, Stanford University) for his helpful comments on an earlier version of the manuscript. None of the individuals listed in the Acknowledgements section received compensation from this study.
Conflicts of Interest None disclosed.
Disclaimer The views expressed in this article are those of the authors and do not necessarily represent the views of the Department of Veterans Affairs.
Prior Presentation One aspect of the data (information regarding the relationship between PTSD and obesity) was presented in poster format at a national meeting: Phibbs CS, Frayne S, Kimerling R, Pavao J, Berg E, Laungani K, Gima K. "Obesity and PTSD in OIF-OEF Veterans." Poster presentation at AcademyHealth National Meeting, Washington DC, June 2008.
Financial Support This material is based upon work supported by Department of Veterans Affairs Health Services Research and Development grants SDR 07-331, SHP 08-161, and IAE 05-291. The views expressed in this article are those of the authors and do not necessarily represent the views of the Department of Veterans Affairs.
Role of the Funding Sources The funding sources had no role in any of the following: design and conduct of the study; collection, management, analysis, and interpretation of the data; and preparation, review, or approval of the manuscript.
Access to Data Dr. Frayne and Mr. Berg had full access to all the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis.
REFERENCES
- 1.Seal KH, Bertenthal D, Miner CR, Sen S, Marmar C. Bringing the war back home: mental health disorders among 103,788 US veterans returning from Iraq and Afghanistan seen at Department of Veterans Affairs facilities. Arch Intern Med. 2007;167(5):476–482. doi: 10.1001/archinte.167.5.476. [DOI] [PubMed] [Google Scholar]
- 2.Hoge CW, Auchterlonie JL, Milliken CS. Mental health problems, use of mental health services, and attrition from military service after returning from deployment to Iraq or Afghanistan. JAMA. 2006;295(9):1023–1032. doi: 10.1001/jama.295.9.1023. [DOI] [PubMed] [Google Scholar]
- 3.Kang HK, Hyams KC. Mental health care needs among recent war veterans. N Engl J Med. 2005;352(13):1289. doi: 10.1056/NEJMp058024. [DOI] [PubMed] [Google Scholar]
- 4.Schnurr PP, Green BL. Trauma and Health, Physical Health Consequences of Exposure to Extreme Stress. Washington, DC: American Psychological Association; 2004. [Google Scholar]
- 5.Lang AJ, Rodgers CS, Laffaye C, Satz LE, Dresselhaus TR, Stein MB. Sexual trauma, posttraumatic stress disorder, and health behavior. Behav Med. Winter. 2003;28(4):150–158. doi: 10.1080/08964280309596053. [DOI] [PubMed] [Google Scholar]
- 6.Geuze E, Westenberg HG, Jochims A, et al. Altered pain processing in veterans with posttraumatic stress disorder. Arch Gen Psychiatry. 2007;64(1):76–85. doi: 10.1001/archpsyc.64.1.76. [DOI] [PubMed] [Google Scholar]
- 7.Kimerling R, Ouimette P, Wolfe J, eds. Gender and PTSD. New York: The Guilford Press; 2002.
- 8.Friedman MJ, Schnurr PP, McDonagh-Coyle A. Post-traumatic stress disorder in the military veteran. Psychiatr Clin North Am. 1994;17(2):265–277. [PubMed] [Google Scholar]
- 9.Yano EM, Bastian LA, Frayne SM, et al. Toward a VA Women’s health research agenda: setting evidence-based priorities to improve the health and health care of women veterans. J Gen Intern Med. 2006;21(s3):S93–S101. doi: 10.1111/j.1525-1497.2006.00381.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.VIREC, VIREC Research User Guide: FY2006 VHA Medical SAS Outpatient Datasets. Hines, IL: Edward J. Hines, Jr. VA Hospital (151 V); September 2007 2007.
- 11.Elixhauser A, Steiner C, Palmer L. Clinical Classifications Software (CCS), 2008. (accessed August 13, 2010); http://www.hcup-us.ahrq.gov/toolssoftware/ccs/ccs.jsp.
- 12.Kimerling R, Ouimette P, Prins A, et al. Brief report: Utility of a short screening scale for DSM-IV PTSD in primary care. J Gen Intern Med. 2005;21(1):65–67. doi: 10.1111/j.1525-1497.2005.00292.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Schnurr PP, Ford JD, Friedman MJ, Green BL, Dain BJ, Sengupta A. Predictors and outcomes of posttraumatic stress disorder in World War II veterans exposed to mustard gas. J Consult Clin Psychol. 2000;68(2):258–268. doi: 10.1037/0022-006X.68.2.258. [DOI] [PubMed] [Google Scholar]
- 14.Stephens M. EDF statistics for goodness of fit and some comparisons. Journal of the American Statistical Association. 1974;69:730–737. doi: 10.2307/2286009. [DOI] [Google Scholar]
- 15.Beckham JC, Moore SD, Feldman ME, Hertzberg MA, Kirby AC, Fairbank JA. Health status, somatization, and severity of posttraumatic stress disorder in Vietnam combat veterans with posttraumatic stress disorder. Am J Psychiatry. 1998;155(11):1565–1569. doi: 10.1176/ajp.155.11.1565. [DOI] [PubMed] [Google Scholar]
- 16.Frayne SM, Seaver MR, Loveland S, et al. Burden of medical illness in women with depression and posttraumatic stress disorder. Arch Intern Med. 2004;164(12):1306–1312. doi: 10.1001/archinte.164.12.1306. [DOI] [PubMed] [Google Scholar]
- 17.Hoge CW, Terhakopian A, Castro CA, Messer SC, Engel CC. Association of posttraumatic stress disorder with somatic symptoms, health care visits, and absenteeism among Iraq war veterans. Am J Psychiatry. 2007;164(1):150–153. doi: 10.1176/appi.ajp.164.1.150. [DOI] [PubMed] [Google Scholar]
- 18.Wagner AW, Wolfe J, Rotnitsky A, Proctor SP, Erickson DJ. An investigation of the impact of posttraumatic stress disorder on physical health. J Trauma Stress. 2000;13(1):41–55. doi: 10.1023/A:1007716813407. [DOI] [PubMed] [Google Scholar]
- 19.Wolfe J, Proctor SP, Erickson DJ, et al. Relationship of psychiatric status to Gulf War veterans’ health problems. Psychosom Med. 1999;61(4):532–540. doi: 10.1097/00006842-199907000-00018. [DOI] [PubMed] [Google Scholar]
- 20.Engel CC, Jr, Liu X, McCarthy BD, Miller RF, Ursano R. Relationship of physical symptoms to posttraumatic stress disorder among veterans seeking care for Gulf War-related health concerns. Psychosom Med. 2000;62(6):739–745. doi: 10.1097/00006842-200011000-00001. [DOI] [PubMed] [Google Scholar]
- 21.Barrett DH, Doebbeling CC, Schwartz DA, et al. Posttraumatic stress disorder and self-reported physical health status among US Military personnel serving during the Gulf War period: a population-based study. Psychosomatics. May-Jun. 2002;43(3):195–205. doi: 10.1176/appi.psy.43.3.195. [DOI] [PubMed] [Google Scholar]
- 22.Hoge CW, McGurk D, Thomas JL, Cox AL, Engel CC, Castro CA. Mild traumatic brain injury in US Soldiers returning from Iraq. N Engl J Med. 2008;358(5):453–463. doi: 10.1056/NEJMoa072972. [DOI] [PubMed] [Google Scholar]
- 23.Cohen BE, Gima K, Bertenthal D, Kim S, Marmar CR, Seal KH. Mental health diagnoses and utilization of VA non-mental health medical services among returning Iraq and Afghanistan veterans. J Gen Intern Med. 2010;25(1):18–24. doi: 10.1007/s11606-009-1117-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Helmer DA, Chandler HK, Quigley KS, Blatt M, Teichman R, Lange G. Chronic widespread pain, mental health, and physical role function in OEF/OIF veterans. Pain Med. 2009;10(7):1174–1182. doi: 10.1111/j.1526-4637.2009.00723.x. [DOI] [PubMed] [Google Scholar]
- 25.Wolfe J, Schnurr PP, Brown PJ, Furey J. Posttraumatic stress disorder and war-zone exposure as correlates of perceived health in female Vietnam War veterans. J Consult Clin Psychol. 1994;62(6):1235–1240. doi: 10.1037/0022-006X.62.6.1235. [DOI] [PubMed] [Google Scholar]
- 26.Taft CT, Stern AS, King LA, King DW. Modeling physical health and functional health status: the role of combat exposure, posttraumatic stress disorder, and personal resource attributes. J Trauma Stress. 1999;12(1):3–23. doi: 10.1023/A:1024786030358. [DOI] [PubMed] [Google Scholar]
- 27.Dobie DJ, Kivlahan DR, Maynard C, Bush KR, Davis TM, Bradley KA. Posttraumatic stress disorder in female veterans: association with self-reported health problems and functional impairment. Arch Intern Med. 2004;164(4):394–400. doi: 10.1001/archinte.164.4.394. [DOI] [PubMed] [Google Scholar]
- 28.Kazis LE, Miller DR, Clark J, et al. Health-related quality of life in patients served by the Department of Veterans Affairs: results from the Veterans Health Study. Arch Intern Med. 1998;158(6):626–632. doi: 10.1001/archinte.158.6.626. [DOI] [PubMed] [Google Scholar]
- 29.Redelmeier DA, Tan SH, Booth GL. The treatment of unrelated disorders in patients with chronic medical diseases. N Engl J Med. 1998;338(21):1516–1520. doi: 10.1056/NEJM199805213382106. [DOI] [PubMed] [Google Scholar]
- 30.Schnurr PP, Friedman MJ, Sengupta A, Jankowski MK, Holmes T. PTSD and utilization of medical treatment services among male Vietnam veterans. J Nerv Ment Dis. 2000;188(8):496–504. doi: 10.1097/00005053-200008000-00004. [DOI] [PubMed] [Google Scholar]
- 31.Sheehan B, Lall R, Bass C. Does somatization influence quality of life among older primary care patients? Int J Geriatr Psychiatry. 2005;20(10):967–972. doi: 10.1002/gps.1387. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Below is the link to the electronic supplementary material.
Mental Health Condition Specifications (PDF 54.4 KB)
Gender-stratified Frequency of all 222 Medical Conditions, by PTSD Status, in OEF/OIF Veterans Health Administration Patients; Frequency Rank for Women and Men with PTSD (with 1 indicating most frequent); and Age-Adjusted Odds Ratio (PTSD vs No MHC)* (PDF 484 KB)
Cumulative Medical Condition Count by PTSD Status by Gender, Sensitivity Analysis 1-4, truncated at 25 conditions. (PDF 295 KB)
Definition of VA Outpatient Face-to-Face Visits (Technical specifications: clinic “stop” codes used to define face-to-face visits.) (PDF 118 KB)
Definition of Primary Care Clinic Stops. (Technical specifications: Clinic stop codes used to define primary care encounters.) (PDF 13.2 KB)