Abstract
BACKGROUND
Many have called for ambulatory training redesign in internal medicine (IM) residencies to increase primary care career outcomes. Many believe dysfunctional, clinic environments are a key barrier to meaningful ambulatory education, but little is actually known about the educational milieu of continuity clinics nationwide.
OBJECTIVE
We wished to describe the infrastructure and educational milieu at resident continuity clinics and assess clinic readiness to meet new IM-RRC requirements.
DESIGN
National survey of ACGME accredited IM training programs.
PARTICIPANTS
Directors of academic and community-based continuity clinics.
RESULTS
Two hundred and twenty-one out of 365 (62%) of clinic directors representing 49% of training programs responded. Wide variation amongst continuity clinics in size, structure and educational organization exist. Clinics below the 25th percentile of total clinic sessions would not meet RRC-IM requirements for total number of clinic sessions. Only two thirds of clinics provided a longitudinal mentor. Forty-three percent of directors reported their trainees felt stressed in the clinic environment and 25% of clinic directors felt overwhelmed.
LIMITATIONS
The survey used self reported data and was not anonymous. A slight predominance of larger clinics and university based clinics responded. Data may not reflect changes to programs made since 2008.
CONCLUSIONS
This national survey demonstrates that the continuity clinic experience varies widely across IM programs, with many sites not yet meeting new ACGME requirements. The combination of disadvantaged and ill patients with inadequately resourced clinics, stressed residents, and clinic directors suggests that many sites need substantial reorganization and institutional commitment.New paradigms, encouraged by ACGME requirement changes such as increased separation of inpatient and outpatient duties are needed to improve the continuity clinic experience.
KEY WORDS: clinic, resident education, ACGME, primary care
BACKGROUND
Multiple organizations and educational leaders have called for the redesign of ambulatory training in internal medicine (IM) residencies.1–6 Changes in ambulatory training are vital as the current graduate medical education system fails to produce a sufficient quantity and quality of primary care physicians.7 In addition to the steep decline in the number of residents choosing ambulatory primary care careers, the additional decline in medical student applications to primary care fields and residencies8–10) and accelerated loss of many current practitioners has created a crisis in primary care.1,8,10–14
Many believe dysfunctional clinic environments are a key barrier to meaningful ambulatory education.6,15 Continuity of patient care and education have been described as a key principle in professional development of trainees.16 While residents have reported that continuity clinic patient and preceptor interactions can be a favorable experience, interruptions from inpatient service and witnessed frustration of attendings in the clinic detract from their overall positive impression.17–19 Too many clinics lack sufficient infrastructure to adequately support the longitudinal care of complex patients. Modeling practices in the residency training environment which are efficient, effective and with fewer stressors may lead to more trainees choosing careers in ambulatory medicine.20
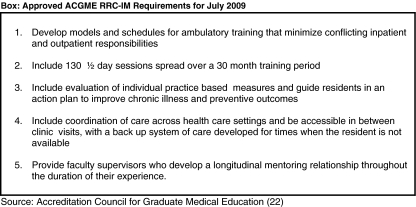
New requirements approved by the Accreditation Council for Graduate Medical Education’s (ACGME) Internal Medicine Residency Review Committee (RRC-IM) for implementation July 2009 called for significant changes regarding resident continuity clinic training (Fig. 1).21
Figure 1.
Approved ACGME RRC-IM Requirements for July 2009 Source: Accreditation Council for Graduate Medical Education.22
Reform of ambulatory training in internal medicine will require substantial attention in two broad domains; the system infrastructure of the clinic and the educational experience of the residents within the clinic. To date, little comprehensive data have been published regarding the educational milieu in which residents are trained in continuity clinic. Understanding the current training environment is an important precursor for informing program leadership and national policymakers who wish to improve ambulatory training. Investigators from the American Board of Internal Medicine (ABIM), Society of General Internal Medicine (SGIM), Association of Chiefs of General Internal Medicine (ACGIM) and the Alliance for Academic Internal Medicine (AAIM) sought to assess the current status of educational systems and operations of continuity clinic training sites at ACGME-accredited programs. We report this descriptive study of important educational support processes and structure in resident continuity clinics.
METHODS
In March 2007, we invited all 378 ACGME-accredited IM residency training programs to participate. Program directors identified medical directors of residency continuity clinics to complete the survey. Clinic directors were then invited to complete the survey and up to 9 email reminders and three telephone calls were placed until the survey was closed in January 2008. Survey completers received a $50 incentive.
The 132 item survey consisted of two sections. The first section, based on an annual survey developed by the SGIM Medical Resident Clinic Directors interest group, included 67 items which focused on clinic demographics and operations, including trainee characteristics, resources and support; patient and payer characteristics; student roles; faculty roles, supervision and assessment; access and scheduling; and organizational culture.22 Results of these items are presented here. The second section was developed by the ABIM with questions focused on elements of the patient-centered medical home model of care.23,24 Clinic system characteristics are reported elsewhere ( acad med in press). The survey was delivered online using Grapevine Surveys (survey copy available at https://data.grapevinesurveys.com/survey.asp?sid=20093275054906 Data analysis and descriptive statistics were performed using SPSS (SPPS, Inc., Chicago,IL USA). Continuous variables were examined for evidence of skewness, outliers, and non-normality, and described using distributions, means, medians, standard deviations, and ranges. Missing data and “impossible” (e.g. 1000 half-day sessions per week) responses were excluded from the survey analysis
RESULTS
Program directors from 264 programs (70%) identified 365 clinic directors. Nine clinic directors declined, leaving 356 eligible respondents. Two hundred twenty one (62%) completed the entire survey, representing 185 programs (49% of all U.S. programs;). All geographic regions and program sizes (<31, 31-50, >50 residents) were well represented, but there was a statistically greater proportion (p < 0.001) of large programs (>=50 residents, 58%) than smaller programs (<50 residents, 40%) completing the survey Additionally, we saw a statistically greater proportion (p = 0.025) of university-based programs (63%) represented versus university-affiliated community hospital programs (49%). Nonresponders were slightly more likely to be community based residencies (15.5% vs. 8.6%) and more likely to be fully university based (21% versus 36%) but equally likely to be from “university affiliated community hospitals (43%).”
CLINIC CHARACTERISTICS
The majority of clinics (N = 139, 63%) were hospital-based, while an additional 41 (19%) were hospital-supported but located offsite. A much smaller proportion was either VA-supported (N = 12, 5%) or a federally-qualified health center (N = 10, 5%). Seventy percent (151 clinics) were situated in urban areas, 25% (54 clinics) in suburban and 5% (11 clinics) in rural settings.
PATIENT CHARACTERISTICS
Overall, the clinics provided care to lower socioeconomic status patients reporting panels with high percentages overall of Medicaid (mean 38%), Medicare (mean 32%) and self-pay (mean 25%) patients. Resident clinics cared for few adolescents but patient panels were composed of a high numbers of minority (African American, Hispanic, other noncaucausian) patients (mean 59%) and 17% required a language translator. Diabetes (97%) and hypertension (91%) cardiovascular disease (58%) and depression (27%) were the most frequent conditions reported in the clinic populations.
INFRASTRUCTURE AND EDUCATIONAL LOGISTICS
Approximately two-thirds of clinics (N = 136, 63%) reported either a partial or complete “firm system” in which discrete teams support provision of continuity care. The majority adjusted clinic schedules based on inpatient call schedules. When the primary resident was unavailable approximately one-third (N = 75) had a resident “buddy” designated to see the patient, but the majority of clinics (N = 160, 73%) stated that the patients are seen by any available resident or faculty member. Overall, most of the clinics had clerical and nursing support with variable support from pharmacy, anticoagulation and other ancillary staff (Table 1).
Table 1.
Support Staff and Resident Evaluation Characteristics
| Clinic support staff (220 Clinics responding) | ||
|---|---|---|
| Available for residents (where faculty do not see their own patients) N = 80 clinics (36%) | Shared (where faculty see their own patients) N = 141 clinics (64%) | |
| Frequency (%) | Frequency (%) | |
| Clerical | 75 (97%) | 130 (94%) |
| RN | 73 (96%) | 125 (93%) |
| Social worker | 68 (93%) | 105 (79%) |
| Nursing assistant | 61 (90%) | 120 (90%) |
| Office manager | 61 (86%) | 121 (92%) |
| Nutritionist | 48 (83%) | 78 (63%) |
| LPN | 48 (77%) | 97 (76%) |
| Pharmacist | 43 (77%) | 70 (57%) |
| Psychologist | 20 (43%) | 34 (31%) |
| Case manager | 19 (43%) | 45 (39%) |
| Nurse practitioner | 18 (40%) | 54 (46%) |
| Physician assistant | 7 (18%) | 16 (15%) |
| Faculty tools for resident evaluation (219 clinics responding) | ||
| Frequency (%) | ||
| Mini-CEX | 179 (82%) | |
| Standardized written evaluation by supervising faculty | 157 (78%) | |
| Formal written evaluations | 127 (58%) | |
| Evaluation by allied or other clinic personnel | 100 (46%) | |
| Patient evaluation | 82 (37%) | |
| Performance-based chart review of patients in panel | 79 (36%) | |
| CEX (traditional or full clinical evaluation exercise) | 41 (19%) | |
| Individual quality improvement report | 39 (18%) | |
| Videotaped reviews of a patient encounters | 28 (13%) | |
| Standardized patient encounters | 18 (8%) | |
| Other | 15 (7%) | |
The total number of clinic sessions and number of patients seen per session increased by year of training (Table 2). Clinics below the 25th percentile of total clinic sessions, however, would not have met the new 2009 RRC –IM 130 session requirement. Mean patient panel size per resident increased modestly from 54 (PGY-1) to 102 (PGY-3) over the 3-year training period. Knowledge resources available onsite included internet resources, most frequently UpToDate (93%), Medline (85%), MD Consult (69%), the Cochrane Library (60%) and textbooks (85%). Two thirds reported providing an educational clinic conference onsite with pre-clinic conference or ambulatory case discussions being most frequent.
Table 2.
Resident Clinic Experiences
| # clinics responding | Mean clinics/resident/year | SD | |
|---|---|---|---|
| Clinic Weeks/Year | |||
| PGY1 | 178 | 39 | 814 |
| PGY2 | 179 | 39 | 714 |
| PGY3 | 176 | 40 | 14 |
| Total Clinics/Year | |||
| PGY1 | 180 | 48 | 25 |
| PGY2 | 181 | 57 | 32 |
| PGY3 | 180 | 60 | 37 |
| Total for 3 years | 180 | 165 | 90 |
| Number of clinics meeting 130 session requirement | 105 (58%) | ||
| Patients scheduled mean | |||
| PGY1 | 204 | 4.6 | 8 |
| PGY2 | 209 | 6.1 | 3.5 |
| PGY3 | 207 | 7.0 | 4.2 |
| Actual Visits | |||
| PGY1 | 204 | 3.1 | 1.1 |
| PGY2 | 205 | 4.3 | 1.5 |
| PGY3 | 203 | 5.0 | 1.8 |
| Panel size | |||
| PGY1 | 90 | 54.4 | 35 |
| PGY2 | 91 | 81.2 | 46 |
| PGY3 | 97 | 102.2 | 58 |
FACULTY SUPPORT AND ASSESSMENT
Faculty supervised a mean of 3.7 residents per session and 7% saw their own patients while precepting. Table 1 reveals that evaluations most commonly involve the mini-CEX, and standardized written faculty evaluations. One third of clinics performed chart reviews of resident panels and only 18% provided an individual quality report to the residents. Furthermore, only 36% surveyed patients about their experience with the resident in the clinic.
CLINIC ENVIRONMENT
Clinic directors reported both they and residents experience significant stress (Table 3). The perceived ability for residents to handle the stress improved with each higher level of training. Forty-three percent of directors (N = 93) reported they believed their interns experienced significant stress in caring for patients in the clinic with many feeling overwhelmed by and unable to make significant changes in their clinics.
Table 3.
Perceived Stress Levels and Ability to Make Changes at Clinic (self report by clinic director)
| PGY1 | PGY2 | PGY3 | |
|---|---|---|---|
| Residents experience significant stress caring for patients at this clinic. | 43% | 31% | 25% |
| Residents have the ability to handle environmental stress at this clinic. | 74% | 78% | 81% |
| Clinic director | |||
| I often feel overwhelmed by my role as the clinic director | 25% | ||
| In my role, I feel like I have too many things to take care of in a given day or week | 59% | ||
| I can easily make changes at the clinic, including those that concern operations, system, and staff. | 27% | ||
| Staff | Faculty | Residents | |
| Receptive to changes that I (clinic director) institute at the clinic | 67% | 69% | 70% |
Legend: Percentages represent Agree or Strongly agree responses based on a five-point Likert-type scale. N varied from 209 to 217 for each question and PGY level.
DISCUSSION
The results of this large national survey provide empiric evidence that the educational experiences of residents in longitudinal ambulatory clinics are highly variable. The “good news” from this study is the finding that half of clinics already meet the new RRC-IM requirements of 130 clinic sessions per year, and that the faculty-to-resident precepting ratio is below 1:4. In addition, most clinics have access to core web-based educational resources for point-of-care learning and use.
However, this study also highlights a number of areas for concern. The majority of clinics care for significantly disadvantaged patient populations with substantial health care needs and challenges, consistent with the findings of a small study of 15 residency programs involved in a quality improvement initiative.25 Many clinics were not yet meeting new ACGME requirements. For example, more than a third of clinics provide neither longitudinal resident mentorship nor a team based system of care. Additionally, fewer than one in five respondent programs indicated current use of data-based resident quality improvement plans as the ACGME now requires. Support structures at resident clinics also varied widely, and may not allow for adequate management of patients between clinic visits. Additionally, most programs had variable schedules based on inpatient duties, which may interfere with patient continuity, and could be exacerbated by further work hour changes.
Perhaps most concerning is the high level of perceived stress among trainees and directors. Future studies should explore resident opinion on the stress in clinic in comparison to other training environments. Competing demands faced by residents in continuity clinic during ward rotations might be solved with greater separation between inpatient and clinic work; inadequate knowledge in managing ambulatory problems would require increased clinic time and curriculum. Such changes may be difficult as a substantial minority of clinic directors feel overwhelmed and a majority do not feel empowered to bring about change.
The climate, may be changing. New RRC guidelines urge that programs minimize conflict between inpatient and outpatient rotations.1,3 The ACGME’s Educational Innovation Project (EIP) first allowed selected training programs flexibility in restructuring continuity clinic scheduling. Some redesigns ( “long blocks”, increased ambulatory blocks) have proven successful in improving resident satisfaction and patient outcomes.26,27 New RRC rules allow similar flexibility to all programs focusing on numbers of continuity sessions rather than on weeks of continuity clinics. Results of Thomas et al.’s national survey of residents and program directors28 indicate that while over 80% of residents feel overlap of inpatient and clinic duties are problematic, the majority still prefer schedules with a weekly clinic. While we await reports from more of these programs on patient outcomes and continuity of care we recommend more pilots of schedules which separate inpatient and outpatient duties as well as focusing more on team based care.
We must also look to new metrics to assess the breadth and depth of primary care patient experience. In our study a PGY-3 resident, on average, cares for a panel of 100 patients. Generously assuming an average of five patients per session, a resident would see only 650 encounters in the entirety of 130 continuity sessions in 3 years. It should come as no surprise that several previous surveys found graduating residents felt substantially underprepared for jobs in primary care upon graduation.29–32
LIMITATIONS
This study has several limitations. First, we were unable to contact every program director, Thus, while we know which programs were represented, we do not know the true number of actual continuity clinics that are involved in training IM residents. Furthermore, we received slightly greater representation from larger programs and university-based programs, which may have resulted in mild selection bias. Second, despite an excellent overall response rate, some respondents did not answer each question, usually based on lack of data available at the home site. Third, while the responses were confidential, our survey was not completely anonymous. This may have resulted in some withholding of negative data or skewed the results toward compliance with ACGME requirements. Fifth, the data were collected in late 2007 thus may not reflect changes made by programs to date to meet the ACGME guidelines. Finally, responses could not be linked to specific patient or resident outcomes.
CONCLUSION
This large-scale national survey demonstrates that the continuity clinic experience varies widely across IM programs, with many sites not yet meeting criteria recently required by the ACGME. Significant opportunities for change provide a challenge to many clinic directors and the obstacles to true transformation are many. These data indicate that more comprehensive and robust changes must occur to achieve the purposes of the RRC-IM. Enhanced emphasis on ambulatory training by training programs likely with separation in time from inpatient duties and the requisite structural and economic changes this entails are vital to achieve such transformation. These ACGME requirement changes provide a guide, encourage innovation and offer leverage for program leaders to achieve important program enhancements that will produce quality internists who find outpatient continuity care rewarding and fulfilling.
Acknowledgment
Funding for the survey and analysis provided by the American Board of Internal Medicine. Portions of this data were presented at the annual meeting of the Society of General Internal Medicine April 2008.
Conflict of Interest None disclosed.
References
- 1.Weinberger SE, Smith LG, Collier VU. Education Committee of the American College of Physicians. Redesigning training for internal medicine. Ann Intern Med. 2006;144:927–32. doi: 10.7326/0003-4819-144-12-200606200-00124. [DOI] [PubMed] [Google Scholar]
- 2.Meyers FJ, Weinberger SE, Fitzgibbons JP, Glassroth J, Duffy FD. Clayton CP; Alliance for Academic Internal Medicine Education Redesign Task Force. Redesigning residency training in internal medicine: the consensus report of the Alliance for Academic Internal Medicine Education Redesign Task Force. Acad Med. 2007;82:1211–19. doi: 10.1097/ACM.0b013e318159d010. [DOI] [PubMed] [Google Scholar]
- 3.Fitzgibbons JP, Bordley DR, Berkowitz LR, Miller BW, Henderson MC. Redesigning residency education in internal medicine: A position paper from the Association of Program Directors in Internal Medicine. Ann Intern Med. 2006;144:920–26. doi: 10.7326/0003-4819-144-12-200606200-00010. [DOI] [PubMed] [Google Scholar]
- 4.Stevens DP, Sixta CS, Wagner E, Bowen JL. The evidence is at hand for improving care in settings where residents train. J Gen Intern Med. 2008;23(7):1116-17. [DOI] [PMC free article] [PubMed]
- 5.Bowen JL, Salerno SM, Chamberlain JK, Eckstrom E, Chen HL, Brandenburg S. Changing habits of practice: Transforming internal medicine residency education in ambulatory settings. J Gen Intern Med. 2005;20:1181–87. doi: 10.1111/j.1525-1497.2005.0248.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Huddle TS, Heudebert GR. Internal medicine training in the 21st century. Acad Med. 2008;83:910. doi: 10.1097/ACM.0b013e3181850a92. [DOI] [PubMed] [Google Scholar]
- 7.Association of American Medical Colleges. Residency Applicants of U.S. Medical School Graduates by Specialty, 2003-2009. Accessed at http://www.aamc.org/data/facts/erasmdphd/table40-erasschltype0309bb.pdf; 2010.
- 8.American College of Physicians. The impending collapse of primary care medicine and its implications for the state of the nation’s health care: a report from the American College of Physicians. January, 30 2006. Accessed at http://www.acponline.org/advocacy/events/state_of_healthcare/statehc06_1.pdf; 2010.
- 9.Garibaldi RA, Popkave C, Bylsma W. Career plans for trainees in internal medicine. Acad Med. 2005;80:507–12. doi: 10.1097/00001888-200505000-00021. [DOI] [PubMed] [Google Scholar]
- 10.Steinbrook R. Easing the shortage in adult primary care – is it all about money? NEJM. 2009;360:2696–99. doi: 10.1056/NEJMp0903460. [DOI] [PubMed] [Google Scholar]
- 11.Hauer KE, Durning SJ, Kernan WN, Fagan MJ, Mintz M, O'Sullivan PS, et al. Factors associated with medical students' career choices regarding internal medicine. JAMA. 2008;300:1154–64. doi: 10.1001/jama.300.10.1154. [DOI] [PubMed] [Google Scholar]
- 12.Compton MT, Frank E, Elon L, Carrera J. Changes in U.S. medical students’ specialty interests over the course of medical school. J Gen Intern Med. 2008;23:1095–1100. doi: 10.1007/s11606-008-0579-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lee TH, Bodenheimer T, Goroll AH, Starfield B, Treadway KN. Redesigning Primary Care. N Engl J Med. 2008;359:e24. doi: 10.1056/NEJMp0809050. [DOI] [PubMed] [Google Scholar]
- 14.National Resident Matching Program. Accessed at http://www.nrmp.org/data/index.html; 2010.
- 15.Keirns CC, Bosk CL. Perspective: the unintended consequences of training residents in dysfunctional outpatient settings. Acad Med. 2008;83:498–50. doi: 10.1097/ACM.0b013e31816be3ab. [DOI] [PubMed] [Google Scholar]
- 16.Hirsh DA, Ogur B, Thibault GE, Cox M. Continuity as an organizational principle for clinical education reform. NEJM. 2007;356:858–66. doi: 10.1056/NEJMsb061660. [DOI] [PubMed] [Google Scholar]
- 17.Bodenheimer T. Coordinating Care – A Perilous Journey through the Health Care System. N Engl J Med. 2008;358:1064–71. doi: 10.1056/NEJMhpr0706165. [DOI] [PubMed] [Google Scholar]
- 18.Sisson S, Boonyasai R, Baker-Genaw K, Silverstein J. Continuity Clinic Satisfaction and Valuation in Residency Training. J Gen Intern Med. 2007;22:1704–10. doi: 10.1007/s11606-007-0412-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Salerno SM, Faestel PM, Mulligan T, Rosenblum MJ. Disruptions and satisfaction in internal medicine resident continuity clinic differ between inpatient and outpatient rotations. Teach Learn Med. 2007;19:30–34. doi: 10.1207/s15328015tlm1901_6. [DOI] [PubMed] [Google Scholar]
- 20.Holmboe ES, Bowen JL, Green M, et al. Reforming internal medicine residency training. A report from the Society of General Internal Medicine’s Task Force for Residency Reform. J Gen Intern Med. 2005;20:1165–72. doi: 10.1111/j.1525-1497.2005.0249.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Accreditation Council for Graduate Medical Education. Internal Medicine Program Requirements. Accessed at http://www.acgme.org/acWebsite/RRC_140/140_prIndex.asp; 2010.
- 22.Society of General Internal Medicine. Medical Resident Clinic Director Interest Group Survey Results 2008. Accessed at http://www.sgim.org/userfiles/file/Blank%20MRCDIG%20Survey.pdf (June 14, 2010).
- 23.Turner BJ, Centor RM, Rosenthal GE. Council of the Society of General Internal Medicine. Principles to consider in defining new directions in internal medicine training and certification. J Gen Intern Med. 2006;3:276–8. doi: 10.1111/j.1525-1497.2006.00393.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Barr M, Ginsburg J. The advanced medical home: A patient-centered, physician guided model of health care. Philadelphia PA: American College of Physicians Policy Monograph; 2006. [Google Scholar]
- 25.Mladenovic J, Shea JA, Duffy FD, Lynn LA, Holmboe ES, Lipner RS. Variation in internal medicine residency clinic practices: Assessing practice environments and quality of care. J Gen Intern Med. 2008;23:914–20. doi: 10.1007/s11606-008-0511-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Warm EJ, Schauer DP, Diers T, et al. The ambulatory long-block: An Accreditation Council for Graduate Medical Education (ACGME) Educational Innovations Project (EIP) J Gen Intern Med. 2008;23:921–926. doi: 10.1007/s11606-008-0588-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Tess AV, Yang JJ, Smith CC, Fawcett CM, Bates CK, Reynolds EE. Combining clinical microsystems and experiential quality improvement curriculum to improve residency education in internal medicine. Acad Med. 2009;84:326–34. doi: 10.1097/ACM.0b013e31819731bf. [DOI] [PubMed] [Google Scholar]
- 28.Thomas KG, West CP, Popkave C, Bellini LM, Weinberger SE, Kolars JC, et al. Alternative approaches to ambulatory training: Internal medicine residents’ and program directors’ perspectives. J Gen Intern Med. 2009;24:904–10. doi: 10.1007/s11606-009-1015-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Cantor JC, Baker LC, Hughes RG. Preparedness for practice: Young physicians' views of their professional education. JAMA. 1993;270:1035–40. doi: 10.1001/jama.270.9.1035. [DOI] [PubMed] [Google Scholar]
- 30.Wiest FC, Ferris TG, Gokhale M, Campbell EG, Weissman JS, Blumenthal D. Preparedness of internal medicine and family practice residents for treating common conditions. JAMA. 2002;288:2609–14. doi: 10.1001/jama.288.20.2609. [DOI] [PubMed] [Google Scholar]
- 31.Blumenthal D, Gokhale M, Campbell EG, Weissman JS. Preparedness for clinical practice: reports of graduating residents at academic health centers. JAMA. 2001;286:1127–34. doi: 10.1001/jama.286.9.1027. [DOI] [PubMed] [Google Scholar]
- 32.Linzer M, Manwell LB, Williams ES, et al. Working Conditions in Primary Care: Physician Reactions and Care Quality. Ann Intern Med. 2009;151:28–36. doi: 10.7326/0003-4819-151-1-200907070-00006. [DOI] [PubMed] [Google Scholar]