Abstract
BACKGROUND
Patient care provided by primary care physicians outside of office visits is important for care coordination and may serve as a substitute for office visits.
OBJECTIVES
To describe primary care physicians’ ambulatory patient care activities outside of office visits (“AOVs”) and their perceptions of the extent to which AOVs substitute for visits and may be performed by support staff.
DESIGN
Cross-sectional direct observational study.
PARTICIPANTS
Thirty-three general internists in 20 practices in two health care systems (one public, one private) in the New York metropolitan area.
MAIN MEASURES
Duration of AOVs by type of activity and whether they pertain to a patient visit on the study day (visit specific) or not (non-visit specific). Physician perceptions of the: (1) extent that non-visit-specific AOVs substitute for visits that would have otherwise occurred, (2) extent that visits that occurred could have been substituted for by AOVs, and (3) potential role of support staff in AOVs.
KEY RESULTS
Physicians spent 20% of their workday performing AOVs, 62% of which was for non-visit specific AOVs. They perceived that a median of 37% of non-visit-specific AOV time substituted for visits, representing a potential five visits saved per day. They also perceived that 15% of total AOV time (excluding charting) could be performed by support staff. Forty-two percent of physicians indicated that one or more visits during the study day could be substituted for by AOVs.
CONCLUSIONS
Though time spent on AOVs is generally not reimbursed, primary care general internists spent significant time performing AOVs, much of which they perceived to substitute for visits that would otherwise have occurred. Policies supporting physician and staff time spent on AOVs may reduce health care costs, save time for patients and physicians, and improve care coordination.
KEY WORDS: primary care, care management/care coordination, ambulatory care
INTRODUCTION
Primary care physicians spend much of their workdays in ambulatory patient care activities outside of office visits for patients who are not physically present (AOVs). The two direct observational studies performed to date indicate that family physicians spend an average of 23% of their workdays in AOVs1,2. Academic geriatricians self-report spending 22% of their practice sessions in AOVs3. Physicians in one general medicine practice performed 41 patient-related telephone calls and e-mails daily, as documented by the practice’s electronic medical record (EMR)4. Pediatricians caring for children with special needs perceive that 33% of self-reported non-reimbursable care coordination encounters substitute for more costly services, such as office visits5. Time spent in AOVs is generally not reimbursed by payers6,7. However, this time may be useful in coordinating patient care8,9 and substituting for office visits that would otherwise occur5,10, thus potentially reducing costs and saving time for patients and physicians11,12. Furthermore, innovative models substituting telephone and electronic communication for visits have found that patients are satisfied with and may prefer this time-saving approach12,13.
Aside from findings for pediatricians caring for children with special health care needs5,10, research to date has not addressed the following questions: To what extent do AOVs substitute for visits among primary care physicians? To what extent could AOVs currently performed by physicians be performed by non-physician support staff? To what extent could office visits that do occur be substituted for by AOVs? We addressed these questions by directly observing the practice of 33 general internists in 20 practices and eliciting their perceptions through questionnaires and interviews to test the hypotheses that a substantial portion of AOVs may substitute for visits and that many AOVs currently performed by physicians could be performed by support staff.
METHODS
Participants
We approached all general internists in two health care systems in the New York metropolitan area for participation if they were either: (1) employees of one public health care system or (2) affiliated physicians of one private health care system. The Institutional Review Boards of the two systems and Weill Cornell Medical College approved the study. Written informed consent was obtained.
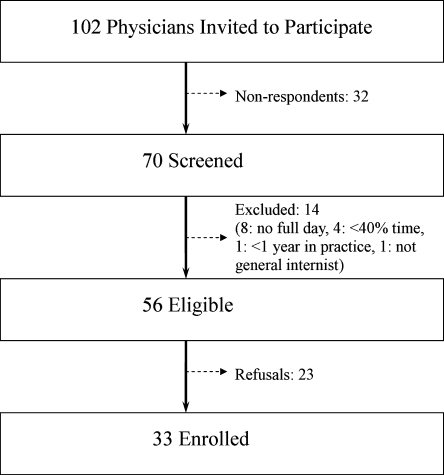
Physicians were eligible to participate if they were in primary care practice for at least 40% time for at least 1 year. Physicians were invited to participate through letters or meeting presentations with follow-up by telephone or e-mail. Physicians were considered non-respondents if they could not be contacted after three attempts. Out of the 102 physicians screened, 31% (32 out of 102) did not respond; 20% (14 out of 70) who responded were not eligible (Fig. 1). Fifty-nine percent (33 out of 56) of eligible physicians who responded were enrolled and completed the study. Participants were similar to non-participants in the percentage who were female (33% vs 31%) and years in clinical practice (18 vs 22). There was a non-statistically significant difference in board certification rate (91% vs. 76%).
Figure 1.
Recruitment and screening.
Pilot Testing
Pilot testing of the data collection process and questionnaires was completed during observation sessions with two study investigators during their general medicine practice sessions. Categories of AOVs derived through review of categorization methods from past studies1–3 were refined during pilot testing.
Data Collection
All data were collected by the study’s first author. For each physician, one full ambulatory patient care day was observed between April and October 2009. Physicians were observed from the time they indicated that their workday began to the time they indicated their workday was completed. The observer followed the physician during the workday, excluding time spent in face-to-face patient visits, to record the duration and activity category of each AOV performed (see Appendix for AOV activity categories list). We selected this direct observational approach because it has been found to measure clinician time more accurately than self-report methods14.
AOVs were subcategorized as visit specific (pertaining to a patient seen on the study day for an office visit) or non-visit specific (pertaining to a patient not seen on the study day for an office visit). An example of a visit-specific AOV is discussing with staff regarding care coordination for a patient seen on the study day. An example of a non-visit-specific AOV is calling a patient not seen for a visit on the study day regarding follow-up of laboratory tests. The start and stop times of AOVs and visits were recorded to the nearest second. Physicians were asked for estimates of additional time spent in AOVs on the study day outside of the observed workday (e.g., AOVs done from home); this time was reported separately and not included in our analyses of AOV time. We focused on outpatient care, so time spent caring for inpatient or nursing home patients during the observed workday (e.g., by phone from the physician’s office) or in rounds before or after the observed workday was not included in the definition of an AOV and is reported separately. We ascertained the time spent in inpatient or nursing home care by direct observation for time spent from the office during the observed workday and by physician self-report for time spent rounding outside of the observed workday. Non-patient-related activities and personal time during the observed workday were not recorded.
Each physician completed two questionnaires on the observation day. The first listed all observed AOVs, and the physician reviewed each AOV and suggested changes to categorization when appropriate. Physicians also indicated whether each AOV (excluding charting) could have been performed by non-physician staff. Charting was excluded from this analysis since it is generally regarded as an activity that physicians must perform themselves for medical-legal reasons. Physicians also indicated whether each non-visit-specific AOV could have substituted for an office or ER visit. Physicians completed a second questionnaire listing each office visit during the workday to indicate whether each visit could have been substituted for by an AOV.
The observer also interviewed physicians to ask open-ended questions regarding barriers to involving support staff in AOVs and reasons why visits occur for issues that could be handled without a face-to-face encounter. Physician job satisfaction was measured using a questionnaire from Grembowski15.
Statistical Analysis
The unit of analysis was each physician’s workday. Means, medians, standard deviations, and interquartile ranges of time spent in AOVs and visits during the workday were calculated. The data on the extent to which AOVs substituted for visits and could be performed by support staff were skewed, so their medians and interquartile ranges were reported. Baseline comparisons of physician and practice characteristics between groups were performed using Fisher’s exact test of independence, chi-square test of independence, t-test, and the Mann-Whitney U test, as appropriate. Analyses were performed using JMP 7 (SAS Institute, Cary, NC) and STATA SE, version 10 (Statacorp, College Station, TX).
RESULTS
Physician and Practice Characteristics
Of the 33 participating physicians, 16 worked at 1 of 14 private practices; 17 were employed at 1 of 6 publicly-run practices (Table 1). We represent our data for all physicians and also for private and public physicians separately to most accurately portray these different groups. The private practice physicians were more likely to be Caucasian. The publicly employed physicians were more likely to be salaried, practice in larger groups, use EMRs, and have a higher percentage of Medicaid and self-pay patients. Sixty-one percent of participants used EMRs. Thirty-six percent of participants reported having paid time to perform AOVs. Those with this paid time had a mean 3.4 h allotted weekly, although this time was often used instead to perform acute office visits. Physicians’ mean job satisfaction score was 3.66 out of 5 points (1 = very dissatisfied and 5 = very satisfied).
Table 1.
Physician and Practice Characteristics
| Characteristics | All physicians (N = 33) | Private physicians (N = 16) | Public physicians (N = 17) |
|---|---|---|---|
| Physician characteristics | |||
| Mean age–years (SD) | 52 (10) | 52 (8) | 52 (11) |
| Mean years in practice (SD) | 18 (10) | 17 (10) | 18 (10) |
| Female, N (%) | 11 (33) | 3 (19) | 8 (47) |
| Race, N (%) | |||
| Caucasian | 13 (40) | 13 (81) | 0 (0) |
| African American | 4 (12) | 0 (0) | 4 (24) |
| Latino | 9 (27) | 2 (13) | 7 (41) |
| Asian/Pacific Islander | 7 (21) | 1 (6) | 6 (35) |
| Board certified, N (%) | 30 (91) | 16 (100) | 14 (82) |
| Reimbursement, N (%) | |||
| Salaried | 14 (42) | 3 (19) | 11 (65) |
| Productivity component | 19 (58) | 13 (81) | 6 (35) |
| Paid time for AOVs, N (%) | 12 (36) | 4 (25) | 8 (47) |
| Mean job satisfaction (SD) | 3.66 (0.63) | 3.79 (0.53) | 3.54 (0.72) |
| Practice characteristics | |||
| Electronic medical record, N (%) | 20 (61) | 3 (19) | 17 (100) |
| Median no. physicians/practice (mean, range) | 5 (5.8, 1–13) | 2 (2.4, 1–5) | 8 (8.9, 3–13) |
| Mean no. staff/physician | |||
| Nurses | 0.5 | 0.1 | 1 |
| Medical assistants | 0.9 | 1.3 | 0.6 |
| Administrative assistants | 0.6 | 0.9 | 0.4 |
| Mean payer mix, % | |||
| Private insurance | 25 | 45 | 6 |
| Medicare | 25 | 38 | 13 |
| Medicaid | 31 | 10 | 51 |
| Self pay | 19 | 7 | 30 |
Time Distribution During Workday
Mean observed in-office workday duration was 7.7 h (Table 2). This excluded time for lunch and non-patient related meetings.
Table 2.
Description of Observed Physician Workday
| All physicians (N = 33) | Private physicians (N = 16) | Public physicians (N = 17) | |
|---|---|---|---|
| AOVs | |||
| Mean total time-h (SD) | 1.6 (0.7) | 1.6 (0.8) | 1.6 (0.6) |
| Visit-specific time | 0.6 (0.6) | 0.5 (0.4) | 0.8 (0.7) |
| Non-visit specific time | 1.0 (0.6) | 1.1 (0.6) | 0.8 (0.5) |
| Mean % of workday | 20 | 20 | 21 |
| Visits | |||
| Mean total time-h (SD) | 4.9 (1.5) | 4.8 (1.8) | 4.9 (1.2) |
| Mean % of workday | 62 | 59 | 65 |
| Median no. of visits/day (quartiles) | 18 (15–23) | 21 (18–24) | 15 (13–19) |
| Median visit duration-min (quartiles) | 15 (11–22) | 11 (10–17) | 18 (12–26) |
| Inpatient/nursing home care* | |||
| Mean total time-h (SD) | 0.1 (0.2) | 0.2 (0.3) | 0 (0) |
| Mean % of workday | 1 | 3 | 0 |
| Total observed workday | |||
| Mean total time-h (SD) | 7.7 (1.6) | 8.0 (1.9) | 7.5 (1.2) |
*This includes only inpatient and nursing home care provided during the observed workday from the physician’s ambulatory practice
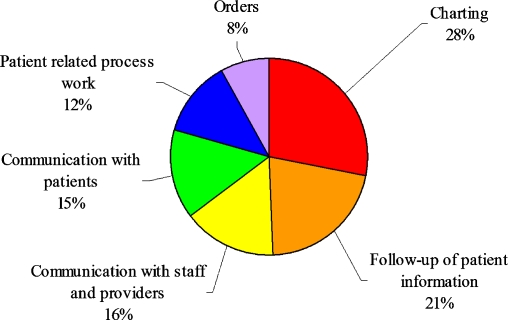
Physicians spent 20% of their observed workday performing AOVs (Table 2). Thirty-eight percent of AOV time was visit specific; 62% was non-visit specific. The highest percentages of AOV time during the observed workday were spent in charting and follow-up of patient information (Fig. 2). Of the 20 physicians who used EMRs, 60% (SD 21) of their AOVs were performed electronically, with the most common electronic AOVs being charting and review of diagnostic studies.
Figure 2.
Percentage of time spent in AOVs by category (Charting. Follow-up of patient information (diagnostic studies, consults, mail, chart review, health research). Communication with staff and providers. Communication with patients (phone calls, answering messages). Patient-related process work (forms, scheduling, insurance issues, getting supplies). Orders (medications, consults, studies).
Thirty-nine percent of physicians reported that they had spent or would spend additional AOV time before or after the observed workday. Including physicians’ estimates of this time would increase the mean total AOV time to 1.9 h, but we excluded this time from our analyses.
Sixty-two percent of the observed workday was spent in face-to-face office visits (Table 2). The median number of visits was 18. The median duration of each visit was 15 min.
One percent of the observed workday was spent in inpatient and nursing home care that the physician performed from their ambulatory practice. The remaining 17% of the observed workday was spent in personal and other activities unrelated to patient care.
Fifty percent of private physicians (and none of the public physicians) reported additional off-site inpatient or nursing home rounding responsibilities before or after the observed workday. These eight physicians reported that they had spent or were planning to spend a mean 2.8 h in off-site inpatient care or nursing home rounding.
At the end of the workday, physicians responded to a question adapted from Gottshalk2 about whether the observer’s presence changed their practice behavior, and their mean score was 1.1 (1 = no change and 4 = changed a lot).
Physicians’ Perceptions of AOVs
Physicians reviewed a questionnaire listing each AOV they performed and stated whether they believed that the AOV likely substituted for a visit that otherwise would have occurred. The individual AOVs that they stated substituted for visits amounted to a median 37% of non-visit-specific AOV time (Table 3). When the number of AOV encounters substituting for visits was calculated, this translated into a potential median savings of five visits (quartiles 2–8.5) per physician day. The mean duration of each AOV perceived to substitute for a visit was 3.5 min. The most frequent non-visit-specific AOVs substituting for visits were patient phone calls (26%), follow-up of diagnostic studies (22%), and prescriptions (12%).
Table 3.
Physicians’ Perceptions of AOVs Performed During the Observed Workday
| All physicians* (N = 33) | Private physicians* (N = 16) | Public physicians* (N = 17) | |
|---|---|---|---|
| Non-visit specific AOV time that could have substituted for a visit | |||
| Hours of non-visit-specific AOV time | 0.3 (0.1–0.5) | 0.4 (0.1–0.6) | 0.3 (0.1–0.4) |
| % of Non-visit specific AOV time | 37 (17–64) | 36 (14–65) | 40 (17–60) |
| AOV time that could have been performed by non-physician support staff† | |||
| Hours of AOV time | 0.2 (0–0.3) | 0.1 (0–0.2) | 0.2 (0.1–0.4) |
| % of AOV time | 15 (4–39) | 10 (1–29) | 21 (10–45) |
*Median (quartiles)
†Analysis performed excluding charting from total AOV time
Physicians perceived that a median 15% of total AOV time (excluding charting) could have been performed by support staff (Table 3). In responding to this question, physicians were asked to limit their answers to the types of staff currently existing in their practices and not to include mid-level providers, such as physician assistants or nurse practitioners. The most common AOVs that physicians believed could be performed by support staff were communication with staff and providers and communication with patients.
Perceived barriers to staff involvement in AOVs stated by physicians during the interviews were not having enough staff, lack of physician-staff trust, communication difficulties, patient preference, differing physician-staff expectations, and lack of staff training.
Physicians’ Perceptions of Visits
Fourteen physicians (42%) perceived that one or more visits during the study day could have been performed as an AOV, thus avoiding a visit (Table 4). The mean number of visits that these 14 physicians believed could have been substituted for by AOVs was 2.8 visits per physician day; the mean across all participating physicians was 1.2 visits per physician day. The mean duration of each office visit that could have been substituted for by an AOV was 11 min. During the interviews, physicians in the public system perceived that adherence to system policies as well as appointment triage errors were the most common reasons why visits occurred for issues that could be handled as AOVs. Private physicians perceived that physician and patient preferences for face-to-face visits were the main reason why visits occurred for issues that could be handled as AOVs. Other reasons given were miscommunication, liability, and lack of physician time to perform AOVs.
Table 4.
Physicians’ Perceptions of Number of Visits on the Study Day That Could Be Substituted for by AOVs
| Number of visits | All physicians* (N = 33) | Private physicians* (N = 16) | Public physicians* (N = 17) |
|---|---|---|---|
| 0 | 19 (58) | 9 (56) | 10 (59) |
| 1–2 | 6 (18) | 2 (13) | 4 (23) |
| 3–4 | 6 (18) | 4 (25) | 2 (12) |
| 5 | 2 (6) | 1 (6) | 1 (6) |
*N (%)
The most common reasons why physicians believed that most visits required face-to-face encounters were for physical examination or to deal with patients’ multiple medical problems.
DISCUSSION
Our findings suggest that general internists spend a substantial part of their workday performing AOVs and that much of this work substitutes for office or ER visits that would otherwise have occurred. Physicians perceived that care provided through AOVs saved a median of 5 patient visits per day, with each AOV performed in less than a quarter of the time that a visit required. They believed that most AOVs were best performed by themselves, although some could be performed by non-physician support staff.
Other studies1–4 have also found that primary care physicians perform a substantial amount of AOVs. Ours is the first direct observational study we are aware of to evaluate primary care physicians’ perceptions of the extent to which AOVs substituted for visits, the extent to which AOVs could have been performed by support staff, and the extent to which office visits that did occur could have been substituted for by AOVs. It is also the first direct observational study of which we know that examines AOVs performed by general internists.
Comparing our main outcome measures between subgroups of participating physicians was not an aim of this descriptive study. Given the wide variability within groups and presence of potential confounding variables, a substantially larger sample size would be necessary to carry out subgroup analyses. However, it is notable that the main outcomes of our study (total AOV time, AOV time substituting for visits, and visits that could be substituted for by AOVs) were similar between private and public physicians, although public physicians believed that more AOV time could have been performed by support staff than private physicians. Future studies employing larger scale methodologies should be conducted to further investigate this as well as to compare physicians’ use of AOVs by other factors such as EMR use, reimbursement mechanism, payment for AOV time, and practice and payer structures.
Our study has several limitations of note that should inform or be the subjects of future study. First, our study included 33 general internists from 20 different practices in one metropolitan area, and our results may not be generalizable to all physicians. However, our study includes the largest number of physicians of any direct observational study of primary care physician time spent in patient care outside of visits of which we are aware. Participants were similar in gender distribution although, slightly older than general internists from the American Medical Association Masterfile16. Participants were comparable to non-participants in gender and years in clinical practice. Participants’ mean job satisfaction score of 3.66 was similar to Grembowski’s score of 3.65 in a larger sample of 498 primary care physicians15, suggesting that it is unlikely that our study attracted physicians who were particularly satisfied or dissatisfied. Participants may have differed from non-participants in other ways, but it is unclear in which direction, if any, differences would bias our results. Physicians who do more AOVs might have been too busy to participate; alternatively, physicians not interested in AOVs might have declined to participate. Systematic bias is unlikely because we found a wide distribution among participants in time spent on AOVs and also because our finding that 20% of the workday was spent in AOVs is similar to both Gilchrist’s and Gottshalk’s findings of 23% in community-based family physicians1,2. Our finding of a median of 18 office visits per day is similar to Gilchrist’s findings of 21 visits per day1. Our median visit duration of 15 min is the same as both Gilchrist’s finding and data reported by internists from the 2006 National Ambulatory Medical Care Survey1,17.
A second limitation is that we did not address AOVs performed by non-physician staff or their perceptions of AOVs. Third, we did not directly observe AOVs that physicians may have performed off-site prior to or after the workday. Fourth, it is possible that the presence of an observer may have changed the physician’s practice behavior. However, participating physicians indicated that being observed did not change their behavior, consistent with findings from Gottshalk’s direct observational study2. Fifth, each physician was observed for one full day of practice, and this day may not have been representative of a typical workday. Sixth, we directly observed and documented AOVs but report only physicians’ perceptions of the extent to which these AOVs substituted for visits and could be performed by support staff. Seventh, because physicians gave their perceptions based on their practice situations as they currently exist, our results may underestimate the extent to which AOVs could substitute for visits and be performed by support staff as well as the extent to which visits could be substituted for by AOVs. Generally speaking, practices only receive reimbursement for face-to-face encounters between physicians and patients6,7. If payment methods of ambulatory care were changed so that AOVs were directly or indirectly reimbursed18–21 and if staff with training in AOVs were more common, physicians might perceive that a larger number of visits might be substituted for by AOVs performed by either physicians or staff.
Since physicians are generally not reimbursed for AOVs6,7, AOVs may be undersupplied compared to the optimum. Payment policies supporting use of AOVs by physicians and other staff (e.g., additional payments to practices that function as patient-centered medical homes or capitation with performance bonuses based on quality measures) may improve care coordination, reduce costs, and save patients’ time by reducing unnecessary office or ER visits.
Primary care physicians face significant time constraints22,23. Along with time spent in AOVs, physicians often spend additional non-patient care-related time dealing with health plans24 and other administrative issues that were not fully captured by our study. Adverse workflow has been strongly associated with low physician satisfaction, and nearly one third of primary care physicians intend to leave their practices within 2 years25. Crucial time may be saved by substituting more AOVs for visits and more staff time spent on AOVs for physician time. Appreciation of AOVs as valued, integral parts of the workday may enrich the primary care environment for physicians, staff, and patients.
Acknowledgments
The authors thank participating physicians for their time, Dr. Martin Wells for his statistical advice, and Dr. Robert Amoruso for his support and assistance. Dr. Melinda A. Chen was a Fellow in Clinical Epidemiology and Health Services Research supported by grant number 5 T32 HS000066 from the Agency for Healthcare Research and Quality during the period in which this work was conducted. This work was presented at the Annual National Research Service Award Trainees Research Conferences on June 27, 2009 and June 26, 2010.
Conflict Of Interest None disclosed.
APPENDIX
Categories of AOVs by Activity
Charting in patient’s medical record
- Follow-up of patient information:
- Diagnostic laboratory and imaging studies
- Consult letters
- Patient-related mail
- Review of patient’s chart
- Health information research pertaining to specific patient
Communication with staff and providers (care coordination discussions in person or via telephone)
Communication with patients (via telephone or written messages)
- Patient-related process work
- Forms
- Scheduling
- Insurance issues
- Getting supplies
- Orders
- Medications
- Consults
- Diagnostic laboratory and imaging studies
References
- 1.Gilchrist V, McCord G, Schrop SL, et al. Physician activities during time out of the examination room. Ann. Fam. Med. 2005;3:494–499. doi: 10.1370/afm.391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Gottschalk A, Flocke SA. Time spent in face-to-face patient care and work outside the examination room. Ann. Fam. Med. 2005;3:488–493. doi: 10.1370/afm.404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Farber J, Siu A, Bloom P. How much time do physicians spend providing care outside of office visits? Ann. Intern. Med. 2007;147:693–698. doi: 10.7326/0003-4819-147-10-200711200-00005. [DOI] [PubMed] [Google Scholar]
- 4.Baron RJ. What’s keeping us so busy in primary care? A snapshot from one practice. N Engl J. Med. 2010;362:1632–1636. doi: 10.1056/NEJMon0910793. [DOI] [PubMed] [Google Scholar]
- 5.Antonelli RC, Stille CJ, Antonelli DM. Care coordination for children and youth with special health care needs: A descriptive, multisite study of activities, personnel costs, and outcomes. Pediatrics. 2008;122:209–216. doi: 10.1542/peds.2007-2254. [DOI] [PubMed] [Google Scholar]
- 6.American College of Physicians. 2008 CPT codes clarify billing for phone and electronic E/M. Available at: http://www.acpinternist.org/archives/2008/01/billing.htm. Accessed August 10, 2010.
- 7.Bodenheimer T. Coordinating care: A major (unreimbursed) task of primary care. Ann. Intern. Med. 2007;147:730–731. doi: 10.7326/0003-4819-147-10-200711200-00010. [DOI] [PubMed] [Google Scholar]
- 8.Pham HH, O’Malley AS, Bach PB, Saiontz-Martinez C, Schrag D. Primary care physicians’ links to other physicians through Medicare patients: The scope of care coordination. Ann. Intern. Med. 2009;150:236–242. doi: 10.7326/0003-4819-150-4-200902170-00004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.American College of Physicians. Controlling health care costs while promoting the best possible health outcomes. Available at: http://www.acponline.org/advocacy/where_we_stand/policy/controlling_healthcare_costs.pdf. Accessed August 10, 2010.
- 10.Antonelli RC, Antonelli DM. Providing a medical home: The cost of care coordination in a community-based, general pediatric practice. Pediatrics. 2004;113:1522–1528. [PubMed] [Google Scholar]
- 11.Bodenheimer T, Grumbach K, Berenson RA. A lifeline for primary care. N Engl J. Med. 2009;360:2693–2696. doi: 10.1056/NEJMp0902909. [DOI] [PubMed] [Google Scholar]
- 12.Chen C, Garrido T, Chock D, Okawa G, Liang L. The Kaiser Permanente electronic health record: Transforming and streamlining modalities of care. Health Aff (Millwood, VA) 2009;28:323–333. doi: 10.1377/hlthaff.28.2.323. [DOI] [PubMed] [Google Scholar]
- 13.Meyer H. Group Health’s move to the medical home: For doctors, it’s often a hard journey. Health Aff. (Millwood, VA) 2010;29:844–851. doi: 10.1377/hlthaff.2010.0345. [DOI] [PubMed] [Google Scholar]
- 14.Bratt JH, Forfeit J, Chen P, West C, Janowitz B, Vargas T. A comparison of four approaches for measuring clinician time use. Health Policy Plan. 1999;14:374–381. doi: 10.1093/heapol/14.4.374. [DOI] [PubMed] [Google Scholar]
- 15.Grembowski D, Ulrich CM, Paschane D, et al. Managed care and primary physician satisfaction. J. Am. Board Fam. Pract. 2003;16:383–393. doi: 10.3122/jabfm.16.5.383. [DOI] [PubMed] [Google Scholar]
- 16.Smart DR. Physician Characteristics and Distribution in the US. Chicago: American Medical Association; 2009. pp. 282–283. [Google Scholar]
- 17.Cherry DK, Hing E, Woodwell DA, Rechtsteiner EA. National Ambulatory Medical Care Survey: 2006 summary. Natl. Health Stat. Report. 2008;3:1–39. [PubMed] [Google Scholar]
- 18.Arrow K, Auerbach A, Bertko J, et al. Toward a 21st-century health care system: Recommendations for health care reform. Ann. Intern. Med. 2009;150:493–496. doi: 10.7326/0003-4819-150-7-200904070-00115. [DOI] [PubMed] [Google Scholar]
- 19.Rosenthal MB. Beyond pay for performance—Emerging models of provider-payment reform. N Engl J. Med. 2008;359:1197–1200. doi: 10.1056/NEJMp0804658. [DOI] [PubMed] [Google Scholar]
- 20.Fisher ES. Building a medical neighborhood for the medical home. N Engl J. Med. 2008;359:1202–1205. doi: 10.1056/NEJMp0806233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Davis K. Paying for care episodes and care coordination. N Engl J. Med. 2007;356:1166–1168. doi: 10.1056/NEJMe078007. [DOI] [PubMed] [Google Scholar]
- 22.Yarnell KS, Pollack KI, Ostbye T, Krause KM, Michener JL. Primary care: Is there enough time for prevention? Am. J. Public Health. 2003;93:635–640. doi: 10.2105/AJPH.93.4.635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ostbye T, Yarnell KS, Krause KM, Pollack KI, Gradison M, Michener JL. Is there time for management of patients with chronic diseases in primary care? Ann. Fam. Med. 2005;3:209–214. doi: 10.1370/afm.310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Casalino LP, Nicolson S, Gans DN, et al. What does it cost physician practices to interact with health insurance plans? Health Aff. (Millwood, VA) 2009;28:533–543. doi: 10.1377/hlthaff.28.4.w533. [DOI] [PubMed] [Google Scholar]
- 25.Linzer M, Manwell LB, Williams ES, et al. Working conditions in primary care: Physician reactions and care quality. Ann. Intern. Med. 2009;151:28–36. doi: 10.7326/0003-4819-151-1-200907070-00006. [DOI] [PubMed] [Google Scholar]