Abstract
Background
Cardiac catheterization is substantially underused among higher risk acute myocardial infarction (AMI) patients with appropriate indications but overused among patients with inappropriate indications. We sought to determine the importance of anticipated benefit and anticipated harm on the use of cardiac catheterization among older AMI patients.
Methods and Results
We performed an analysis of Medicare fee-for-service beneficiaries hospitalized with an AMI between 1998 and 2001. Multivariate models were developed to determine relative importance of anticipated benefit (baseline cardiovascular risk), anticipated harm (bleeding risk, comorbidities), and demographic factors (age, gender, race, regional invasive intensity) in predicting cardiac catheterization use within 60 days of AMI admission. Analyses were stratified by American College of Cardiology/American Heart Association Class I or II as appropriate, and Class III as inappropriate. Determinants of reduced likelihood of cardiac catheterization among 42,241 AMI patients with appropriate indications included (in order of importance): older age (likelihood χ2 1309.5), higher bleeding risk score (likelihood χ2 471.2), more comorbidities (likelihood χ2 276.6), female sex (likelihood χ2 162.9), hospitalization in low (likelihood χ2 67.9) or intermediate intensity invasive regions (likelihood χ2 22.4) (all P < 0.001), and baseline cardiovascular risk (likelihood χ2 6.4, p =0.01). Among 2,398 AMI patients with inappropriate indications, significant determinants of greater procedure likelihood included younger age, male sex, lower bleeding risk score, and fewer comorbidities.
Conclusions
Regardless of the procedure indication, the decision to perform cardiac catheterization in this population appears largely driven by demographic factors and potential harm rather than potential benefit of the procedure.
Keywords: Cardiac catheterization, acute myocardial infarction, determinants of use, Medicare beneficiaries
Introduction
An early invasive strategy improves outcomes for patients with acute myocardial infarction (AMI), especially those at higher risk for future cardiovascular events.1,2 Nevertheless, data have consistently demonstrated that selection of patients for cardiac catheterization is suboptimal. In particular, cardiac catheterization is substantially underused among higher risk patients with appropriate indications who would be expected to derive the largest benefit.3-6 In contrast, cardiac catheterization is overused among patients with inappropriate indications where invasive procedures may be considered to be ineffective.6,7 Understanding utilization patterns can improve appropriate selection of patients, which in itself would be expected to lead to better outcomes for those with AMI.
Previous studies have focused on evaluating the association of specific individual factors on cardiac catheterization, including socio-demographic predictors such as age, gender, or race, as well as market supply/availability.6,8-11 The use of cardiac catheterization after AMI is highly influenced by regional practice patterns as demonstrated by the tremendous regional variation in its use within the U.S.5,12,13 However, little insight is available on the importance of anticipated benefit and anticipated harm in the use of cardiac catheterization among AMI patients. Anticipated benefit of a therapy in the population is predominantly dependent on a patient's baseline risk of future adverse cardiovascular events; however, greater risk has been shown to paradoxically reduce the likelihood of some treatments.14-17 Anticipated harm of a therapy such as older age, a patient's bleeding risk or number of comorbidities reduces the propensity of receiving many therapies.15,18,19 No population-based study has examined the relative importance and the interplay of these complex factors in the selection of patients for cardiac catheterization after AMI. For example, it may be possible that the risk of bleeding is more important in clinical decision-making even though baseline risk is most important in estimating anticipated benefit of a therapy.
Accordingly, the main objective of this study was to examine the impact of anticipated benefit as determined by baseline cardiovascular risk, and anticipated harm as determined by the risk of bleeding and comorbidities, on utilization of cardiac catheterization after AMI. In addition, the importance of these factors will be assessed in the context of important demographic factors such as age, gender, race, and regional invasive intensity.
Methods
The National Heart Care Project
The National Heart Care project obtained data through chart abstraction of a random sample of Medicare fee-for-service beneficiaries hospitalized between March 1998 and April 1999, and March 2000 to April 2001 with a principal discharge diagnosis of AMI (International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) code 410) from each state and the District of Columbia.6,20 The study sample included patients 65 years of age and older who had a confirmed AMI (including ST-segment elevation and non-ST-segment elevation AMI) using chart abstracted information.6 Patients who were initially hospitalized at a facility without cardiac invasive capability and received a cardiac procedure within 60 days of an AMI were included in the study cohort. Admissions in which the patients were transferred in from another hospital were excluded because we lacked information that described the first hospitalization. Patients who had been hospitalized with a recurrent AMI during the study period were also excluded, so that each patient was represented in the database with only 1 index hospitalization.
Main outcome measure
The primary outcome of the study was the use of cardiac catheterization within 60 days of an AMI admission. Cardiac catheterization use was determined by linking the hospital medical records and Medicare Part A billing records for ICD-9-CM codes associated with the procedure (37.22, 37.33, 88.53-88.57), which captures cardiac procedures performed for hospitalized patients.6
Appropriateness of cardiac catheterization
Appropriateness of cardiac catheterization was based on the American College of Cardiology/American Heart Association (ACC/AHA) guidelines and criteria previously reported (Appendix 1).6,7,20-22 The strong indication group consisted of patients in whom cardiac catheterization was generally recognized as “beneficial, useful and effective” (ACC/AHA Class I). We did not include “reinfarction during hospitalization” as a Class I indicator because this data field was not captured in our dataset. The equivocal group (ACC/AHA Class II) included patients who had conditions for which the effectiveness of cardiac catheterization was unclear. The weak indication group (ACC/AHA Class III) consisted of patients for whom cardiac catheterization was considered unlikely to be effective (Appendix 1).
Determinants of cardiac catheterization use
a) Baseline cardiovascular risk
We determined baseline cardiovascular risk of hospitalized AMI patients using the Global Registry of Acute Coronary Events (GRACE) prediction risk score.23 The GRACE risk score variables include age, admission characteristics (heart rate, Killip class, systolic blood pressure, cardiac arrest at admission, ST-segment deviation), and laboratory values (serum creatinine, positive cardiac markers). Although the GRACE risk score was originally developed using an acute coronary syndrome population, it has been validated previously in other AMI cohorts.24 The plausible range of GRACE risk score is from 1 to 372, with higher score indicating higher predicted risk.
b) Bleeding risk
We calculated the predicted risk of in-hospital major bleeding among our AMI cohort using the Cardiovascular Disease Quality Improvement Initiative Registry (CRUSADE) bleeding risk score.25 The bleeding risk prediction score variables, in order of significance, are baseline hematocrit, creatinine clearance, heart rate, sex, heart failure at presentation, prior vascular disease, diabetes mellitus, and systolic blood pressure. Plausible bleeding score ranges from 1 to 96, with higher score indicating higher risk of bleeding.
We replaced missing values with median values for continuous variables to calculate risk scores for each patient. Missing data were infrequent in our cohort. Of the 16 data variables in the prediction models, most had less than 1% missing frequencies, except for serum creatinine, hematocrit, and body weight, where frequencies of missing were 2.4%, 3.0%, and 4.9%, respectively.
c) Number of chronic comorbidites
Previous studies have shown that physicians become less attentive when managing an increasing number of preexisting conditions (irrespective of type of condition).19 Therefore, we examined the number of pre-existing comorbid conditions (cardiovascular and non-cardiovascular) that were not included in the baseline risk of bleeding risk models to determine their effect on cardiac catheterization utilization such as history of AMI, stroke, chronic obstructive pulmonary disease, smoking, prior cardiac procedures, dementia, mobility, and urinary continence.
d) Regional intensity of cardiac invasive procedures
In order to account for the geographic variations in invasive practice across the United States, we classified hospital referral regions into 3 groups to represent low, intermediate, and high invasive intensity based on the number of cardiac catheterizations performed per 1,000 Medicare enrollees in each region (for example, low invasive intensive regions had the lowest tertile of cardiac catheterization use).6,26 These data were obtained from the 1999 Aggregated Surgical Discharge Data File using residential or hospital Zip codes.
Statistical analysis
We explored the association between demographic factors (age, gender, race, and regional invasive intensity), anticipated benefit (baseline cardiovascular risk) and anticipated harm (bleeding risk and number of comorbid conditions) with cardiac catheterization utilization after AMI. Our analyses were stratified by procedure indication in which we first examined predictors of underutilization among AMI patients with ACC/AHA Class I or II indications, and repeated all the analyses among patients with ACC/AHA Class III indications to determine factors associated with overutilization.
In each stratum, baseline characteristics of patients who received cardiac catheterization were compared with those who did not. We then examined the relationship between the use of cardiac catheterization with selected factors with survey logistic regression analyses. All analyses incorporated probability weights based on the inverse sampling fraction for the population size of each state, and all models were adjusted for clustering of patients at the hospital level. The contribution of each variable to the overall model was determined using Likelihood Chi-Square ratio. The discriminative ability of the model was determined by the area under the receiver operating characteristic curve.
Probability plots were constructed to illustrate how the utilization of invasive therapy was correlated with 2 significant determinants simultaneously (e.g., baseline cardiovascular risk and the number of comorbid factors) after adjusting for remaining covariates in the multivariable logistic regression models. Due to the concerns of significant correlation between predicting factors (for example, increasing age may increase baseline risk and bleeding risk), we calculated Pearson's correlation coefficient between all candidate variables and performed formal diagnostic testing. The correlations between most of the variables were negligible to small, and all the variables had Variance Inflation Factors of less than 5, indicating no evidence of multi-collinearity.
Additional analyses were undertaken to examine the robustness of our results. First, we stratified AMI based on the presence or absence of ST-segment elevation on electrocardiograms. Second, we also altered the timeframe of capturing cardiac catheterizations to 30 days (from 60 days). None of these analyses altered the determinants of cardiac catheterization.
We conducted the statistical analyses using SAS software, version 9.1 (SAS Institute, Inc., Cary, NC). All statistical tests were two-tailed and P values of < 0.05 were considered statistically significant. Use of the National Heart Care Project database was approved by the Yale University School of Medicine Human Investigation Committee.
Results
Baseline characteristics among ACC/AHA Class I and II patients
After applying inclusion and exclusion criteria, our study cohort consisted of 42,241 Medicare beneficiaries who had ACC/AHA Class I or II indications for cardiac catheterization. The mean age among those with Class I or II indications was 78.4 years; 51.2% were female; and 86.3% were white. Cardiac catheterization within 60 days of hospitalization was performed for 40.6% of patients who had Class I or II indications.
Determinants of cardiac catheterization among Class I and II patients
Demographic and clinical characteristics of AMI patients who underwent cardiac catheterization differed substantially from those who did not. Patients who received cardiac catheterization were younger, more likely to be male, had a lower GRACE score, lower bleeding risk, fewer comorbid conditions, and were more likely to be hospitalized in higher intensive regions (all P < 0.001) (Table 1). Cardiac catheterization within 60 days of hospitalization was performed for 40.6% of patients who had Class I or II indications. The cardiac catheterization rate was 46.0% for patients with ST-segment elevation myocardial infarction and 38.4% for patients with non-ST-segment elevation myocardial infarction.
Table 1. Characteristics of acute myocardial infarction patients with ACC/AHA Class I and II procedure indications based on receiving cardiac catheterization within 60 days of admission*.
| Characteristics | No cardiac catheterization | Cardiac catheterization | P value | ||
|---|---|---|---|---|---|
| #/Mean | %/SD | #/Mean | %/SD | ||
| Number of patients | 25,094 | 100 | 17,147 | 100 | |
| Demographics | |||||
| Mean age, yrs | 80.46 | 0.07 | 75.24 | 0.06 | < 0.001 |
| 65 – 74 | 6,454 | 25.1 | 8,502 | 49.1 | < 0.001 |
| 75 – 84 | 10,700 | 42.5 | 7,296 | 42.9 | |
| ≥ 85 | 7,940 | 32.4 | 1,349 | 8.0 | |
| Female | 13,782 | 55.8 | 7,466 | 44.3 | < 0.001 |
| White | 21,269 | 86.0 | 14,716 | 86.8 | 0.11 |
| Admission characteristics | |||||
| Mean systolic blood pressure, mm Hg | 143.0 | 0.28 | 145.9 | 0.35 | < 0.001 |
| Mean heart rate, beats/min | 92.4 | 0.21 | 84.5 | 0.25 | < 0.001 |
| Mean creatinine, mg/dl | 1.58 | 0.01 | 1.29 | 0.03 | < 0.001 |
| STEMI | 6,525 | 24.9 | 5,551 | 31.9 | < 0.001 |
| Anterior myocardial infarction | 8,374 | 32.4 | 6,311 | 36.2 | < 0.001 |
| Cardiac risk factors and comorbidities | |||||
| Hypertension | 17,827 | 72.2 | 11,913 | 70.9 | 0.025 |
| Diabetes | 8,635 | 35.3 | 5,014 | 30.7 | < 0.001 |
| Current smoker | 3,376 | 13.5 | 3,059 | 17.8 | < 0.001 |
| Prior myocardial infarction | 9,652 | 39.2 | 5,561 | 33.0 | < 0.001 |
| Prior CABG | 4,197 | 17.1 | 3,039 | 18.4 | 0.0090 |
| Prior PCI | 2,498 | 10.0 | 2,930 | 17.7 | < 0.001 |
| Prior stroke or TIA | 5,459 | 22.2 | 2,283 | 13.7 | < 0.001 |
| Dementia | 3,425 | 14.7 | 416 | 2.5 | < 0.001 |
| Chronic obstructive pulmonary disease | 6,385 | 26.3 | 3,394 | 20.2 | < 0.001 |
| Mean GRACE risk score | 172.8 | 0.30 | 154.5 | 0.35 | < 0.001 |
| Mean CRUSADE bleeding risk score | 54.5 | 0.10 | 48.0 | 0.11 | < 0.001 |
| Number of chronic comorbidities | < 0.001 | ||||
| 0 | 4,377 | 16.0 | 5,025 | 28.4 | |
| 1 | 6,332 | 25.0 | 4,888 | 27.8 | |
| 2 | 6,510 | 26.1 | 3,870 | 23.5 | |
| 3 | 4,517 | 18.7 | 2,148 | 12.7 | |
| ≥4 | 3,358 | 14.1 | 1,216 | 7.5 | |
| Regional invasive intensity | < 0.001 | ||||
| Low | 10,467 | 32.9 | 6,065 | 25.8 | |
| Intermediate | 8,416 | 36.9 | 5,737 | 36.8 | |
| High | 6,211 | 30.1 | 5,345 | 37.3 | |
ACC/AHA, American College of Cardiology/American Heart Association; CABG, coronary artery bypass grafting; CRUSADE, Cardiovascular Disease Quality Improvement Initiative Registry; GRACE, Global Registry of Acute Coronary Events; PCI, percutaneous coronary intervention; SD, standard deviation; STEMI, ST-elevation myocardial infarction; TIA, transient ischemic attack
See Methods section for definitions of the GRACE risk score, CRUSADE bleeding risk score, number of chronic comorbidities, and regional invasive intensity.
Table 2 illustrates the independent determinants of cardiac catheterization among AMI patients who had ACC/AHA Class I or II indications. Significant determinants of reduced likelihood of cardiac catheterization use in order of their respective contribution to the overall model included older age (likelihood χ2 1309.5, P < 0.001); higher bleeding risk score (likelihood χ2 471.2, p < 0.001); greater number of comorbid conditions (likelihood χ2 276.6, p < 0.001); female sex (likelihood χ2 162.9, p < 0.001); and hospitalization at lower intensity (likelihood χ2 67.9, p < 0.001) or intermediate intensity invasive regions (likelihood χ2 22.4, p < 0.001). GRACE risk score (likelihood χ2 6.4, p =0.01) was weakly associated with cardiac catheterization use, and race (likelihood χ2 3.4, p = 0.07) was not a significant independent predictor of use in multivariate models. The area under the receiver operating characteristic curve was 0.75, indicating good discriminative ability of the aggregated determinants to predict cardiac catheterization use.
Table 2. Relative importance of explanatory factors in the use of cardiac catheterization among ACC/AHA Class I and II AMI patients*.
| Description | Level | Odds Ratio | 95% CI | Likelihood Chi Square | P Value |
|---|---|---|---|---|---|
| Age | Each additional year | 0.917 | 0.913 - 0.921 | 1309.5 | < 0.001 |
| CRUSADE bleeding risk score | Each 5 points increase | 0.824 | 0.810 - 0.838 | 471.2 | < 0.001 |
| Number of comorbid conditions | Each additional comorbid factor | 0.816 | 0.796 - 0.836 | 276.6 | < 0.001 |
| Gender | Female | 0.679 | 0.640 - 0.721 | 162.9 | < 0.001 |
| Low regional invasive intensity | Reference (high invasive regions) | 0.582 | 0.512 - 0.661 | 67.9 | < 0.001 |
| Intermediate regional invasive intensity | Reference (high invasive regions) | 0.755 | 0.672 - 0.848 | 22.4 | < 0.001 |
| GRACE risk score | Each 10 points increase | 0.986 | 0.975 - 0.997 | 6.4 | 0.011 |
| Race | Caucasian vs. non-Caucasian | 1.092 | 0.994 - 1.200 | 3.4 | 0.066 |
ACC/AHA, American College of Cardiology/American Heart Association; AMI, acute myocardial infarction; CI, Confidence Interval; CRUSADE, Cardiovascular Disease Quality Improvement Initiative Registry; GRACE, Global Registry of Acute Coronary Events
All analyses incorporated probability weights based on the inverse sampling fraction for the population size of each state, and all models were adjusted for clustering at the hospital level. Definition of ACC/AHA classification shown in Appendix 1.
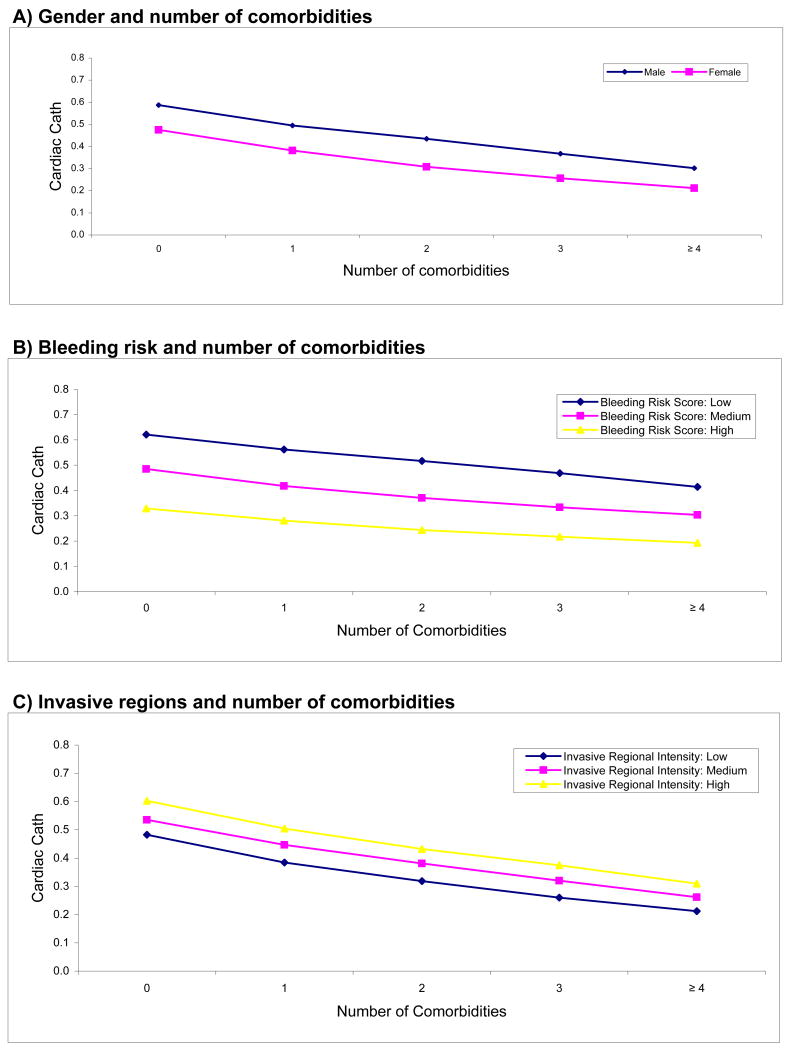
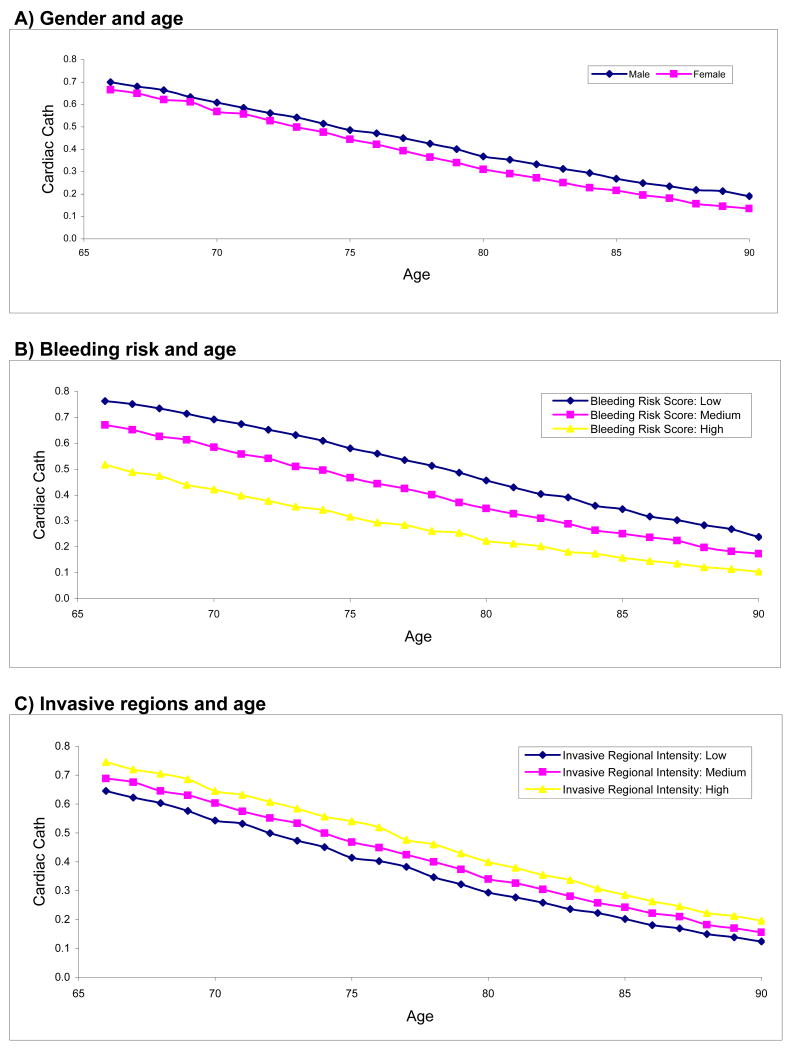
Figures 1 and 2 illustrate the independent impact of strong determinants (age, gender, bleeding risk, comorbidities, and invasive regions) on utilization of cardiac catheterization. We plotted 2 significant factors in each graph simultaneously after imputing average values for other factors to illustrate the independent and additive relationship of each variable with cardiac catheterization. No statistical interaction was detected between factors shown in Figure 1 and Figure 2 (i.e., none of the curves crossed-over). For example, in Figure 1a the estimated probability of cardiac catheterization utilization ranged from 40.5% (no comorbidity) to 21.2% (more than 4 comorbidities) among females. Among males, estimated utilization of cardiac catheterization was significantly higher at 58.8% (no comorbidity) to 30.2% (more than 4 comorbidities). In Figure 2, we plotted the estimated probability of cardiac catheterization between gender, bleeding risk, and invasive regions with age. We found a linear relationship where the likelihood of cardiac catheterization was 8.3% lower (adjusted Odds Ratio (OR) 0.917; 95% Confidence Interval (CI) 0.913 to 0.921) for each increased year in age.
Figure 1.
Estimated probability of cardiac catheterization utilization within 60 days of AMI among patients with ACC/AHA Class I and II indications according to predicting factors and number of comorbidities.
- Figure 1a) Gender and number of comorbidities
- Figure 1b) Bleeding risk and number of comorbidities
- Figure 1c) Invasive regional intensity and number of comorbidities
Figure 2.
Estimated probability of cardiac catheterization utilization within 60 days of AMI among patients with ACC/AHA Class I and II indications according to predicting factors and age.
- Figure 2a) Gender and age
- Figure 2b) Bleeding risk and age
- Figure 2c) Invasive regional intensity and age
Y axis describes the estimated probability of cardiac catheterization utilization by multivariable logistic regression models.
AMI, acute myocardial infarction; ACC, American College of Cardiology; AHA, American Heart Association
Determinants of cardiac catheterization among Class III AMI patients
There were 2,398 AMI Medicare beneficiaries who had ACC/AHA Class III indications for cardiac catheterization. The mean age was 79.0 years; 51.9% were female, 85.5% were white, with a mean GRACE score of 198 and mean bleeding score of 57. Cardiac catheterization was performed in 20.3% of patients who had ACC/AHA Class III indications.
Significant determinants of cardiac catheterization use among AMI patients with ACC/AHA Class III procedure indications were similar to the determinants in the appropriate cohort (Class I-II), with age (likelihood χ2 71.6, P < 0.001), sex (likelihood χ2 11.9, P = 0.001), bleeding risk score (likelihood χ2 43.4, P < 0.001), and fewer number of comorbid conditions (likelihood χ2 13.9, P < 0.001) being significant independent predictors of cardiac catheterization use (Table 3). Intensity of invasive region, GRACE risk score, and race were not significant independent predictors of use among AMI patients with Class III indications. The area under the receiver operating characteristic curve of the model was 0.73.
Table 3. Relative importance of explanatory factors in the use of cardiac catheterization among ACC/AHA Class III AMI patients*.
| Description | Level | OR | 95% CI | Likelihood Chi Square | P Value |
|---|---|---|---|---|---|
| Age | Each additional year | 0.922 | 0.904 - 0.939 | 71.6 | < 0.001 |
| CRUSADE bleeding risk score | Each 5 points increase | 0.772 | 0.715 - 0.834 | 43.4 | < 0.001 |
| Number of comorbid conditions | Each additional comorbid factor | 0.808 | 0.722 - 0.904 | 13.9 | < 0.001 |
| Gender | Female | 0.597 | 0.445 - 0.800 | 11.9 | 0.001 |
| Low regional invasive intensity | Reference (high invasive regions) | 0.774 | 0.548 - 1.093 | 2.1 | 0.146 |
| Intermediate regional invasive intensity | Reference (high invasive regions) | 0.740 | 0.523 - 1.047 | 2.9 | 0.089 |
| GRACE risk score | Each 10 points increase | 0.981 | 0.945 - 1.019 | 1.0 | 0.320 |
| Race | Caucasian vs. non-Caucasian | 1.435 | 0.913 - 2.254 | 2.5 | 0.117 |
ACC/AHA, American College of Cardiology/American Heart Association; CI, Confidence Interval; CRUSADE, Cardiovascular Disease Quality Improvement Initiative Registry; GRACE, Global Registry of Acute Coronary Events; OR, Odds Ratio
All analyses incorporated probability weights based on the inverse sampling fraction for the population size of each state, and all models were adjusted for clustering at the hospital level. Definition of ACC/AHA classification shown in Appendix 1.
Discussion
Our study provides important insights into clinical decision making of physicians for older AMI patients. We observed that patients' bleeding risk and number of comorbidities were substantially more predictive of the use of cardiac catheterization after AMI than their risk of dying. These results suggest that physicians are significantly more concerned about potential harm compared with potential gain when selecting patients for cardiac invasive procedures.
Our findings may also provide an explanation of why discordant patterns of cardiac catheterization continue to exist where procedures are underused among appropriate higher risk patients and overused among inappropriate lower risk patients. Practice guidelines and/or appropriateness criteria have been developed to guide physicians on the basis that a therapy is beneficial. However, most of these data are drawn from randomized studies that enrolled lower risk patients compared with those seen in clinical practice.27,28 Physicians may feel reluctant to generalize clinical trial results to patients who are at higher risk of bleeding and have multiple comorbidities, and thus may not be certain whether older patients in clinical practice would expect a net benefit from invasive procedures. In addition, a fear of malpractice liability and a selection bias in view of public reporting might have further dissuaded physicians to perform procedures among patients with higher predicted risk of harm.29,30 Future prediction tools and practice guidelines should take into account the potential risk of treatment for patients at higher risk of complications to improve the ability of patients and physicians to make informed treatment decisions. Data from clinical registries may provide insights on these higher risk patients in clinical practice.
Anticipated benefit of a therapy in the population is predominantly dependent on a patient's baseline risk of future adverse cardiovascular events; however, another important finding is that baseline cardiovascular risk was a relatively weak predictor for cardiac catheterization use after accounting for other factors. This is surprising, as many studies have consistently demonstrated that cardiac invasive procedures are used substantially less frequently among higher risk patients, an observation that has been previously termed a “treatment-risk paradox.”3,4,15-17 Although we found no correlation between number of comorbidities and cardiovascular risk, we found that bleeding risk and cardiovascular risk are moderately correlated (-0.51 among Class I/II patients, -0.36 among Class III patients). As a result, the association between baseline cardiovascular risk and cardiac catheterization in adjusted analysis (OR = 0.86) was largely attenuated after adjustment (OR = 0.99). Since none of the previous studies adjusted specifically for side effects, adjustment of harm in previous observations might have reduced the importance of the treatment-risk paradox. Similarly, a recent study found that the treatment-risk paradox was largely attenuated after accounting for patients' functional capacity and depressive symptoms, another example suggesting that many other factors can interfere with treatment decisions despite a therapy's anticipated prognostic benefits.31
Consistent with results of other investigations, we found that female patients compared with their male counterparts, and patients hospitalized in lower or intermediate invasive regions compared with those hospitalized in higher invasive regions, have lower likelihoods of receiving cardiac catheterization.6,13,32 Previously cited explanations include differences in demographics, clinical characteristics, and baseline risk, but we excluded these possibilities by accounting for all these factors in our predictive models. Other reasons to explain a gender discrepancy may include differences in symptom presentation, patient acceptance of the procedure, and physician preference due to discrepancies of potential benefits.6,13,32-34 Despite numerous debates, the exact reasons that account for lower cardiac catheterization rates for women and lower invasive regions are unclear.
Previous studies have found marked racial disparities in the use of cardiac catheterization.11,32 In contrast, we did not find significant racial differences in cardiac catheterization use for AMI patients after adjusting for other demographic factors, estimated risk and harm of the procedure. Since racial minorities traditionally have higher risk characteristics and likely also have higher potential risk of procedural complications, it is possible that anticipated harm may be in part responsible for the persistent racial differences in cardiac invasive procedure use as demonstrated in previous studies. In our study, we cannot exclude potential racial differences among patients who were transferred for cardiac catheterization because those patients were excluded.
Several potential limitations of our study merit consideration. First, we examined an older cohort of fee-for-service Medicare beneficiaries hospitalized from 1998 to 2001. This dataset was used because it contained detailed clinically abstracted information, which allowed us to calculate predicted risk scores and to categorize appropriateness of cardiac catheterizations. To our knowledge, no other cohort that has been assembled since the National Heart Care Project is truly nationally representative of the clinical practice in the United States with complete follow-up data. Although utilization of cardiac catheterization has increased in the interim across the United States, there is little evidence to suggest that utilization patterns have dramatically changed in this cohort. In fact, recent studies continue to demonstrate discrepancies in the use of cardiac invasive procedures.3,4,17 Second, we did not use other factors to predict anticipated harm such as potential for stroke or renal failure that may also be major concerns when referring patients for cardiac catheterization. However, bleeding is one of the most common complications of invasive procedures and is associated with substantial morbidity and mortality.35 Furthermore, considering other anticipated adverse effects would tend to strengthen the association of harm and utilization. Finally, the extent to which determinants of utilization reflect actual physician and patient decision-making processes is unknown, since data regarding physician and patient perspectives were not available. However, perspectives may not always accurately reflect or correspond to actual utilization patterns.
In conclusion, underutilization of cardiac catheterization among an older cohort hospitalized with AMI is largely explained by the act of omission due to concern about an adverse event rather than a focus on the potential benefit of an invasive procedure in improving outcomes. Our study challenges national societies to develop practice guidelines to estimate net benefits of cardiac invasive procedures that incorporate anticipated risk of harm.
Acknowledgments
Funding/Support: The analyses upon which this publication is based were performed under Contract Number HHSM-500-2005-CO001C, entitled “Utilization and Quality Control Quality Improvement Organization for the State (commonwealth) of Colorado” sponsored by the Centers for Medicare & Medicaid Services, an agency of the U.S. Department of Health and Human Services. The content of the publication does not necessarily reflect the views or policies of the Department of Health and Human Services, nor does mention of trade names, commercial products, or organizations imply endorsement by the U.S. government. The authors assume full responsibility for the accuracy and completeness of the ideas presented.
The Centers for Medicare & Medicaid Services did not play a role in the design and conduct of the study, or in the analysis and interpretation of the data.
Tracking Number: HIQIOSCHEARTCARE-001-OK-0506
Dr. Ko is supported by a New Investigator Award from the Canadian Institutes of Health Research and a Clinician Scientist Award from the Heart and Stroke Foundation of Ontario.
Dr. Ross is currently supported by Department of Veterans Affairs Health Services Research and Development Service project no. TRP-02-149.
Footnotes
Disclosures: None of the authors has conflicts of interest to disclose.
References
- 1.Anderson JL, Adams CD, Antman EM, Bridges CR, Califf RM, Casey DE, Jr, Chavey WE, 2nd, Fesmire FM, Hochman JS, Levin TN, Lincoff AM, Peterson ED, Theroux P, Wenger NK, Wright RS, Smith SC, Jr, Jacobs AK, Halperin JL, Hunt SA, Krumholz HM, Kushner FG, Lytle BW, Nishimura R, Ornato JP, Page RL, Riegel B. ACC/AHA 2007 guidelines for the management of patients with unstable angina/non ST-elevation myocardial infarction: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Writing Committee to Revise the 2002 Guidelines for the Management of Patients With Unstable Angina/Non ST-Elevation Myocardial Infarction): developed in collaboration with the American College of Emergency Physicians, the Society for Cardiovascular Angiography and Interventions, and the Society of Thoracic Surgeons: endorsed by the American Association of Cardiovascular and Pulmonary Rehabilitation and the Society for Academic Emergency Medicine. Circulation. 2007;116:e148–304. doi: 10.1161/CIRCULATIONAHA.107.181940. [DOI] [PubMed] [Google Scholar]
- 2.Antman EM, Hand M, Armstrong PW, Bates ER, Green LA, Halasyamani LK, Hochman JS, Krumholz HM, Lamas GA, Mullany CJ, Pearle DL, Sloan MA, Smith SC, Jr, Anbe DT, Kushner FG, Ornato JP, Jacobs AK, Adams CD, Anderson JL, Buller CE, Creager MA, Ettinger SM, Halperin JL, Hunt SA, Lytle BW, Nishimura R, Page RL, Riegel B, Tarkington LG, Yancy CW. 2007 focused update of the ACC/AHA 2004 guidelines for the management of patients with ST-elevation myocardial infarction: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines: developed in collaboration with the Canadian Cardiovascular Society endorsed by the American Academy of Family Physicians: 2007 Writing Group to Review New Evidence and Update the ACC/AHA 2004 Guidelines for the Management of Patients With ST-Elevation Myocardial Infarction, Writing on Behalf of the 2004 Writing Committee. Circulation. 2008;117:296–329. doi: 10.1161/CIRCULATIONAHA.107.188209. [DOI] [PubMed] [Google Scholar]
- 3.Bhatt DL, Roe MT, Peterson ED, Li Y, Chen AY, Harrington RA, Greenbaum AB, Berger PB, Cannon CP, Cohen DJ, Gibson CM, Saucedo JF, Kleiman NS, Hochman JS, Boden WE, Brindis RG, Peacock WF, Smith SC, Jr, Pollack CV, Jr, Gibler WB, Ohman EM. for the CRUSADE Investigators. Utilization of early invasive management strategies for high-risk patients with non-ST-segment elevation acute coronary syndromes: results from the CRUSADE Quality Improvement Initiative. JAMA. 2004;292:2096–2104. doi: 10.1001/jama.292.17.2096. [DOI] [PubMed] [Google Scholar]
- 4.Fox KA, Anderson FA, Dabbous OH, Steg PG, Lopez-Sendon JL, Van de Werf F, Budaj A, Gurfinkel EP, Goodman SG, Brieger D. Intervention in acute coronary syndromes: do patients undergo intervention on the basis of their risk characteristics? The Global Registry of Acute Coronary Events (GRACE) Heart. 2007;93:177–182. doi: 10.1136/hrt.2005.084830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ko DT, Krumholz HM, Wang Y, Foody JM, Masoudi FA, Havranek EP, You JJ, Alter DA, Stukel TA, Newman AM, Tu JV. Regional differences in process of care and outcomes for older acute myocardial infarction patients in the United States and Ontario, Canada. Circulation. 2007;115:196–203. doi: 10.1161/CIRCULATIONAHA.106.657601. [DOI] [PubMed] [Google Scholar]
- 6.Ko DT, Wang Y, Alter DA, Curtis JP, Rathore SS, Stukel TA, Masoudi FA, Ross JS, Foody JM, Krumholz HM. Regional variation in cardiac catheterization appropriateness and baseline risk after acute myocardial infarction. J Am Coll Cardiol. 2008;51:716–723. doi: 10.1016/j.jacc.2007.10.039. [DOI] [PubMed] [Google Scholar]
- 7.Ross JS, Ho V, Wang Y, Cha SS, Epstein AJ, Masoudi FA, Nallamothu BK, Krumholz HM. Certificate of need regulation and cardiac catheterization appropriateness after acute myocardial infarction. Circulation. 2007;115:1012–1019. doi: 10.1161/CIRCULATIONAHA.106.658377. [DOI] [PubMed] [Google Scholar]
- 8.Pilote L, Miller DP, Califf RM, Rao JS, Weaver WD, Topol EJ. Determinants of the use of coronary angiography and revascularization after thrombolysis for acute myocardial infarction. N Engl J Med. 1996;335:1198–1205. doi: 10.1056/NEJM199610173351606. [DOI] [PubMed] [Google Scholar]
- 9.Rathore SS, Wang Y, Radford MJ, Ordin DL, Krumholz HM. Sex differences in cardiac catheterization after acute myocardial infarction: the role of procedure appropriateness. Ann Intern Med. 2002;137:487–493. doi: 10.7326/0003-4819-137-6-200209170-00008. [DOI] [PubMed] [Google Scholar]
- 10.Every NR, Larson EB, Litwin PE, Maynard C, Fihn SD, Eisenberg MS, Hallstrom AP, Martin JS, Weaver WD. The association between on-site cardiac catheterization facilities and the use of coronary angiography after acute myocardial infarction. Myocardial Infarction Triage and Intervention Project Investigators. N Engl J Med. 1993;329:546–551. doi: 10.1056/NEJM199308193290807. [DOI] [PubMed] [Google Scholar]
- 11.Chen J, Rathore SS, Radford MJ, Wang Y, Krumholz HM. Racial differences in the use of cardiac catheterization after acute myocardial infarction. N Engl J Med. 2001;344:1443–1449. doi: 10.1056/NEJM200105103441906. [DOI] [PubMed] [Google Scholar]
- 12.Pilote L, Califf RM, Sapp S, Miller DP, Mark DB, Weaver WD, Gore JM, Armstrong PW, Ohman EM, Topol EJ. Regional variation across the United States in the management of acute myocardial infarction. GUSTO-1 Investigators. Global Utilization of Streptokinase and Tissue Plasminogen Activator for Occluded Coronary Arteries. N Engl J Med. 1995;333:565–572. doi: 10.1056/NEJM199508313330907. [DOI] [PubMed] [Google Scholar]
- 13.Stukel TA, Lucas FL, Wennberg DE. Long-term outcomes of regional variations in intensity of invasive vs medical management of Medicare patients with acute myocardial infarction. JAMA. 2005;293:1329–1337. doi: 10.1001/jama.293.11.1329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Alter DA, Manuel DG, Gunraj N, Anderson G, Naylor CD, Laupacis A. Age, risk-benefit trade-offs, and the projected effects of evidence-based therapies. Am J Med. 2004;116:540–545. doi: 10.1016/j.amjmed.2003.10.039. [DOI] [PubMed] [Google Scholar]
- 15.Ko DT, Mamdani M, Alter DA. Lipid-lowering therapy with statins in high-risk elderly patients: the treatment-risk paradox. JAMA. 2004;291:1864–1870. doi: 10.1001/jama.291.15.1864. [DOI] [PubMed] [Google Scholar]
- 16.Lee DS, Tu JV, Juurlink DN, Alter DA, Ko DT, Austin PC, Chong A, Stukel TA, Levy D, Laupacis A. Risk-treatment mismatch in the pharmacotherapy of heart failure. JAMA. 2005;294:1240–1247. doi: 10.1001/jama.294.10.1240. [DOI] [PubMed] [Google Scholar]
- 17.Yan AT, Yan RT, Tan M, Fung A, Cohen EA, Fitchett DH, Langer A, Goodman SG. Management patterns in relation to risk stratification among patients with non-ST elevation acute coronary syndromes. Arch Intern Med. 2007;167:1009–1016. doi: 10.1001/archinte.167.10.1009. [DOI] [PubMed] [Google Scholar]
- 18.Anderson RT, Ory M, Cohen S, McBride JS. Issues of aging and adherence to health interventions. Control Clin Trials. 2000;21:171S–183S. doi: 10.1016/s0197-2456(00)00075-1. [DOI] [PubMed] [Google Scholar]
- 19.Redelmeier DA, Tan SH, Booth GL. The treatment of unrelated disorders in patients with chronic medical diseases. N Engl J Med. 1998;338:1516–1520. doi: 10.1056/NEJM199805213382106. [DOI] [PubMed] [Google Scholar]
- 20.Burwen DR, Galusha DH, Lewis JM, Bedinger MR, Radford MJ, Krumholz HM, Foody JM. National and state trends in quality of care for acute myocardial infarction between 1994-1995 and 1998-1999: the Medicare Health Care Quality Improvement Program. Arch Intern Med. 2003;163:1430–1439. doi: 10.1001/archinte.163.12.1430. [DOI] [PubMed] [Google Scholar]
- 21.Guadagnoli E, Landrum MB, Peterson EA, Gahart MT, Ryan TJ, McNeil BJ. Appropriateness of coronary angiography after myocardial infarction among Medicare beneficiaries. Managed care versus fee for service. N Engl J Med. 2000;343:1460–1466. doi: 10.1056/NEJM200011163432006. [DOI] [PubMed] [Google Scholar]
- 22.Ryan TJ, Anderson JL, Antman EM, Braniff BA, Brooks NH, Califf RM, Hillis LD, Hiratzka LF, Rapaport E, Riegel BJ, Russell RO, Smith EE, 3rd, Weaver WD. ACC/AHA guidelines for the management of patients with acute myocardial infarction: executive summary. A report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Committee on Management of Acute Myocardial Infarction) Circulation. 1996;94:2341–2350. doi: 10.1161/01.cir.94.9.2341. [DOI] [PubMed] [Google Scholar]
- 23.Granger CB, Goldberg RJ, Dabbous O, Pieper KS, Eagle KA, Cannon CP, Van De Werf F, Avezum A, Goodman SG, Flather MD, Fox KA. Global Registry of Acute Coronary Events I. Predictors of hospital mortality in the Global Registry of Acute Coronary Events. Arch Intern Med. 2003;163:2345–2353. doi: 10.1001/archinte.163.19.2345. [DOI] [PubMed] [Google Scholar]
- 24.Bradshaw PJ, Ko DT, Newman AM, Donovan LR, Tu JV. Validity of the GRACE (Global Registry of Acute Coronary Events) acute coronary syndrome prediction model for six month post-discharge death in an independent data set. Heart. 2006;92:905–909. doi: 10.1136/hrt.2005.073122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Subherwal S, Bach RG, Chen AY, Gage BF, Rao SV, Newby LK, Wang TY, Gibler WB, Ohman EM, Roe MT, Pollack CV, Jr, Peterson ED, Alexander KP. Baseline risk of major bleeding in non-ST-segment-elevation myocardial infarction: the CRUSADE (Can Rapid risk stratification of Unstable angina patients Suppress ADverse outcomes with Early implementation of the ACC/AHA Guidelines) Bleeding Score. Circulation. 2009;119:1873–1882. doi: 10.1161/CIRCULATIONAHA.108.828541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Wennberg DE, Dartmouth Atlas of Cardiovascular Health Care Working Group . The Dartmouth Atlas of Cardiovascular Health Care. Chicago, Ill: AHA Press; 1999. [Google Scholar]
- 27.Jha AK, Fisher ES, Li Z, Orav EJ, Epstein AM. Racial trends in the use of major procedures among the elderly. N Engl J Med. 2005;353:683–691. doi: 10.1056/NEJMsa050672. [DOI] [PubMed] [Google Scholar]
- 28.Lee PY, Alexander KP, Hammill BG, Pasquali SK, Peterson ED. Representation of elderly persons and women in published randomized trials of acute coronary syndromes. JAMA. 2001;286:708–713. doi: 10.1001/jama.286.6.708. [DOI] [PubMed] [Google Scholar]
- 29.Studdert DM, Mello MM, Sage WM, DesRoches CM, Peugh J, Zapert K, Brennan TA. Defensive medicine among high-risk specialist physicians in a volatile malpractice environment. JAMA. 2005;293:2609–2617. doi: 10.1001/jama.293.21.2609. [DOI] [PubMed] [Google Scholar]
- 30.Moscucci M, Eagle KA, Share D, Smith D, De Franco AC, O'Donnell M, Kline-Rogers E, Jani SM, Brown DL. Public reporting and case selection for percutaneous coronary interventions: an analysis from two large multicenter percutaneous coronary intervention databases. J Am Coll Cardiol. 2005;45:1759–1765. doi: 10.1016/j.jacc.2005.01.055. [DOI] [PubMed] [Google Scholar]
- 31.McAlister FA, Oreopoulos A, Norris CM, Graham MM, Tsuyuki RT, Knudtson M, Ghali WA. Exploring the treatment-risk paradox in coronary disease. Arch Intern Med. 2007;167:1019–1025. doi: 10.1001/archinte.167.10.1019. [DOI] [PubMed] [Google Scholar]
- 32.Vaccarino V, Rathore SS, Wenger NK, Frederick PD, Abramson JL, Barron HV, Manhapra A, Mallik S, Krumholz HM. Sex and racial differences in the management of acute myocardial infarction, 1994 through 2002. N Engl J Med. 2005;353:671–682. doi: 10.1056/NEJMsa032214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Redberg RF. Gender, race, and cardiac care: why the differences? J Am Coll Cardiol. 2005;46:1852–1854. doi: 10.1016/j.jacc.2005.07.043. [DOI] [PubMed] [Google Scholar]
- 34.Rathore SS, Ordin DL, Krumholz HM. Race and sex differences in the refusal of cardiac catheterization among elderly patients hospitalized with acute myocardial infarction. Am Heart J. 2002;144:1052–1056. doi: 10.1067/mhj.2002.126122. [DOI] [PubMed] [Google Scholar]
- 35.Rao SV, Jollis JG, Harrington RA, Granger CB, Newby LK, Armstrong PW, Moliterno DJ, Lindblad L, Pieper K, Topol EJ, Stamler JS, Califf RM. Relationship of blood transfusion and clinical outcomes in patients with acute coronary syndromes. JAMA. 2004;292:1555–1562. doi: 10.1001/jama.292.13.1555. [DOI] [PubMed] [Google Scholar]