Abstract
Objective
To estimate the burden of acute otitis media (AOM) on Canadian families.
Design
Telephone survey using random-digit dialing.
Setting
All Canadian provinces between May and June 2008.
Participants
Caregivers of 1 or more children aged 6 months to 5 years.
Main outcome measures
Caregivers’ reports on the number of AOM episodes experienced by the child in the past 12 months, as well as disease characteristics, health services and medication use, time spent on medical consultations (including travel), and time taken off from work to care for the sick children.
Results
A total of 502 eligible caregivers were recruited, 161 (32%) of whom reported at least 1 AOM episode for their children and 42 (8%) of whom reported 3 or more episodes during the past 12 months. Most children (94%, 151 of 161) visited with health professionals during their most recent AOM episodes. The average time required for medical examination was 3.1 hours in an emergency department and 1.8 hours in an outpatient clinic. Overall, 93% of episodes resulted in antibiotics use. A substantial proportion of caregivers (38%) missed work during this time; the average time taken off work was 15.9 hours.
Conclusion
In Canada, episodes of AOM are still associated with substantial use of health services and indirect costs to the caregivers.
Résumé
Objectif
Estimer le fardeau qu’impose l’otite moyenne aiguë (OMA) aux familles canadiennes.
Type d’étude
Enquête téléphonique à l’aide de numéros choisis au hasard.
Contexte
Toutes les provinces canadiennes, entre mai et juin 2008.
Participants
Soignants s’occupant d’au moins un enfant âgé entre 6 mois et 5 ans.
Principaux paramètres à l’étude
Déclarations des soignants concernant le nombre d’épisodes d’OMA subies par l’enfant au cours des 12 derniers mois, ainsi que les caractéristiques de la maladie, les médicaments et services de santé utilisés, le temps consacré aux consultations (incluant les déplacements) et le temps perdu au travail pour s’occuper des enfants malades.
Résultats
Un total de 502 soignants admissibles ont été recrutés, dont 161 (32 %) ont rapporté au moins un épisode d’OMA et 42 (8 %) au moins 3 épisodes parmi leurs enfants au cours des 12 derniers mois. La plupart des enfants (94 %, 151 sur 161) ont consulté leur professionnel de la santé durant l’épisode le plus récent. Le temps requis pour l’examen était en moyenne de 3,1 heure dans un service d’urgence et de 1,8 heure dans une clinique externe. Dans l’ensemble, 93 % des épisodes ont abouti à une prescription d’antibiotiques. Une proportion appréciable de soignants (38 %) ont dû s’absenter du travail à cette occasion; le temps perdu au travail s’élevait en moyenne à 15,9 heures.
Conclusion
Au Canada, les épisodes d‘OMA demeurent responsables d’une importante utilisation des services de santé et de coûts indirects pour les soignants.
Acute otitis media (AOM) is one of the most common bacterial infections among children and a leading cause of health care visits and antibiotic prescriptions.1 In Quebec, 11% of physicians’ insurance claims for children younger than 10 years of age are associated with a diagnosis of otitis media2; the total annual cost to the health care system of otitis media and placement of ventilation tubes is more than $10 million.3 In the first 3 years of life, 60% to 70% of children will have experienced at least 1 episode of AOM,4 and recurrent episodes of AOM are common.5
The main characteristic symptom of AOM is effusion in the middle ear, accompanied by such signs of acute illness as earache, otorrhea (ie, runny, stuffed ear), ear tugging, fever, irritability, anorexia, vomiting, or diarrhea.6 A diagnosis of AOM is the most common reason for antibiotic prescribing in childhood, even though most cases of AOM resolve spontaneously.7 In fact, results of meta-analyses indicate that antibiotics are not very useful for most children with AOM.8–10 Antimicrobial resistance to bacterial otopathogens is an increasing public health concern worldwide. In the United States, strains of Streptococcus pneumoniae that are resistant to all Food and Drug Administration–approved antibiotics for the treatment of AOM in children have emerged in recent years.11 Primary prevention of AOM through immunization is an emerging issue,12 but few vaccines have the potential to prevent AOM.13–16 Another strategy to reduce the burden of AOM is to use antibiotics more selectively. With the so-called wait-and-see approach, the use of antibiotics is deferred by 2 or 3 days, during which time only pain is treated; antibiotics are only prescribed if there is no improvement in the child’s clinical condition at the end of this period.7 In 2009, the Canadian Paediatric Society recommended the wait-and-see approach as a valid option for otherwise healthy children older than 6 months of age who have mild clinical signs and symptoms of AOM.17
Precise knowledge of the frequency and consequences of AOM is needed to evaluate interventions that aim to reduce its societal costs, and an often-neglected aspect is the burden of disease on families. To our knowledge, the burden of AOM on Canadian families has never been estimated. Previous studies have assessed the societal costs of AOM in Canada before the addition of pneumococcal conjugate vaccine to the regular childhood vaccination schedule.18,19 These studies indicated that AOM had a relatively low family and health care system unit cost; however, owing to its frequency, the estimated overall burden was high. In 2001, the cost of an episode of AOM in Canada was estimated at $321, of which 82% was borne by families.18 Studies have also shown the negative effects of otitis media on parental stress, family functioning, and quality of life of the child and his or her family.20–25
In 2008, we surveyed a random sample of Canadian families; results pertaining to the quality of life of affected children and their parents and to parental knowledge, attitudes, and beliefs regarding AOM and its prevention have been reported elsewhere.26,27 This report focuses on the frequency and severity of AOM, health services use, and absenteeism from work.
METHODS
The Ethics Board of the Centre hospitalier universitaire de Québec approved the study protocol. From May to June 2008, stratified random sampling of households in all 10 Canadian provinces was performed using random-digit dialing. A sample size of 500 was needed to provide an overall precision of plus or minus 4% in the estimate of proportions (with a 95% confidence interval). Respondents in households with at least 1 child aged 6 months to 5 years were invited to participate, and the adult most involved in the care of the child was invited to complete a telephone interview in English or French. Questions about the occurrence of AOM were prefaced with a standard definition. The child having the most recent AOM episode in the past 12 months (ie, the index child) was selected for further analysis. The caregiver was asked to report on the number of AOM episodes experienced by the child in the previous 12 months; to describe the duration, symptoms, and health services and medication use of the last episode; and to quantify time spent on medical visits and time taken off from work to take care of the sick child. Information was also obtained on the caregiver’s age and sex, education, region of residence, number of persons in the household, and other relevant characteristics (eg, 1 or 2 caregivers per household, children in shared custody). The questionnaire used in this study was based on a questionnaire used to assess the burden of chickenpox on families in another study.28 Descriptive statistics were generated for all variables using SAS version 9.1. Comparisons of categorical responses were performed using χ2 or Fisher exact tests.
RESULTS
Of the 28 374 telephone numbers randomly generated, 26 385 were reached: 12 269 were nonresidential or not in service; in 4796 households, the respondent refused to participate; and 8769 households were not eligible (ie, no child in the targeted age group). In the 551 eligible households, a caregiver was able to complete the survey in 502 cases (Figure 1). The number of respondents by province was proportional to the population weight of each province. Thirty-two percent of caregivers (161 of 502) reported at least 1 AOM episode during the past 12 months. Most caregivers were mothers (82%), 58% were aged 25 to 34 years old, and 65% had college or university degrees. In the 161 households, the mean number of AOM episodes in the past 12 months was 2.2 (range 1 to 10), with 27% of caregivers reporting 3 or more episodes. The most recent episode of AOM in each household was included for analysis, for a total of 161 cases included for further study. The mean age of the index child was 37.4 months, 50% were girls, and 37% were living in shared custody.
Figure 1.
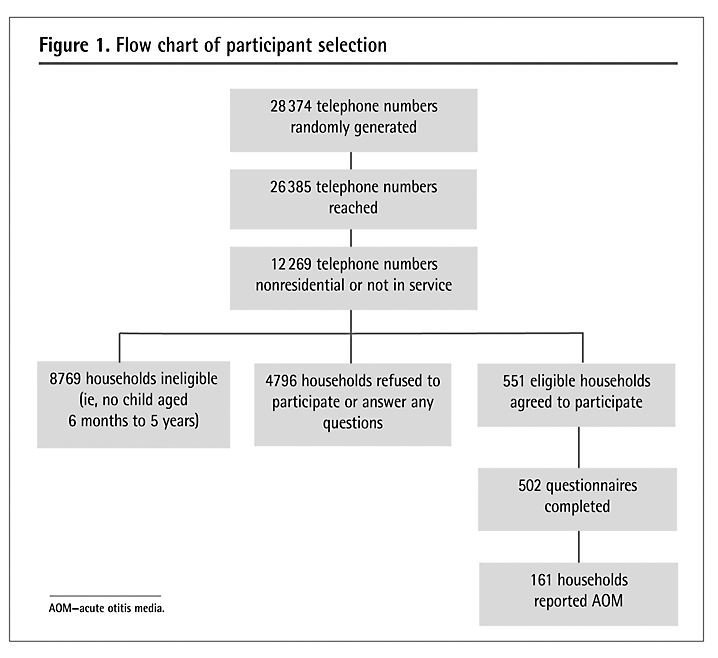
Flow chart of participant selection
AOM—acute otitis media.
Reported characteristics of AOM episodes according to age are shown in Table 1. The mean duration of AOM episodes was 5.9 days (median 4 days) with no statistically significant differences among age groups. On average, caregivers reported 2.8 symptoms during the last occurrence of AOM (median 3 symptoms). Pain, otorrhea, and hearing loss were more frequently reported among children 3 years of age and older than among younger children. In 11% of cases, a medical help line was called. By far most episodes (94%) resulted in visits to physicians, more frequently in younger than in older children (100% vs 89%, P ≤ .05). Over-the-counter or prescribed medications were used in 100% of AOM episodes. A greater number of medications was used by older than by younger children; 28% of children 3 years of age and older used 3 or more medications during the last AOM episode compared with 14% of younger children (P ≤ .05). Antibiotics were used in 93% of episodes and there was no statistically significant difference according to age. Analgesic or antipyretic drugs were used in 80% and natural products in 9% of episodes.
Table 1.
Description of episodes, health services use, and medications for AOM, by age
| CHARACTERISTICS |
AGE |
||
|---|---|---|---|
| 6 TO 36 MO,* N (%) (N = 43) | 3 TO 4 Y,* N (%) (N = 93) | ALL AGES,†N (%) (N = 161) | |
| Duration, d | |||
| • ≤ 3 | 14 (33) | 30 (32) | 52 (32) |
| • 4 to 6 | 13 (30) | 32 (34) | 55 (34) |
| • ≥ 7 | 15 (35) | 29 (31) | 51 (32) |
| • Unknown | 1 (2) | 2 (2) | 3 (2) |
| Symptoms reported | |||
| • Ear pain | 32 (74)‡ | 82 (88)‡ | 139 (86) |
| • Fever | 34 (79) | 76 (82) | 130 (81) |
| • Otorrhoea or ruptured tympanic membrane | 4 (9)‡ | 28 (30)‡ | 38 (24) |
| • Vertigo | 5 (12) | 13 (14) | 23 (14) |
| • Hearing loss | 2 (5)‡ | 23 (25)‡ | 31 (19) |
| Health services use | |||
| • Call to help line§ | 7 (16) | 8 (9) | 18 (11) |
| • Visit to physician | 43 (100)‡ | 83 (89)‡ | 151 (94) |
| • Private clinic or community health centre | 32 (74) | 68 (73) | 122 (76) |
| • Emergency room | 11 (26) | 15 (16) | 29 (18) |
| No. of medications taken | |||
| • 1 | 12 (28)‡ | 10 (11)‡ | 26 (16) |
| • 2 | 25 (58)‡ | 57 (61)‡ | 97 (60) |
| • ≥ 3 | 6 (14)‡ | 26 (28)‡ | 38 (24) |
| Type of medications taken | |||
| • Antibiotics | 41 (95) | 84 (90) | 149 (93) |
| • Antipyretics or analgesics | 31 (72) | 79 (85) | 129 (80) |
| • Ear drops | 5 (12)‡ | 26 (28)‡ | 37 (23) |
| • Natural products | 3 (7) | 9 (10) | 14 (9) |
Responses were compared between the 2 age groups using χ2 or Fisher exact tests.
Included in this group are 25 children aged 6 months to 5 years with their exact ages unknown (not included in previous 2 groups).
Differences between the 2 age groups are statistically significant (P ≤ .05).
Some caregivers who used help lines also sought care from physicians.
Of the 151 patients who received medical care, the mean distance traveled for medical visits was 13.3 km (median 10 km), and most caregivers (n = 140) used their own vehicles; public transportation was used in a small number of cases (n = 6) and the remaining 5 patients (with their caregivers) traveled on foot.
When parents brought children to the emergency department, the mean total time needed for transportation, waiting, and medical examination was 3.1 hours; 21% of parents spent a total of 4 hours or more to a maximum of 18 hours (Table 2). When the child was seen in an outpatient clinic, the average time required was 1.8 hours, with a maximum of 3 hours, excluding the time needed to get an appointment (Table 2). Work absenteeism to take care of the sick child was reported by 61 caregivers (38% of episodes), for an average of 15.9 hours (median 14 hours).
Table 2.
Time spent visiting a physician, including travel, waiting, and medical examination: N = 151.
| TIME | EMERGENCY ROOM (N = 29) | OUTPATIENT CLINIC (N = 118)* |
|---|---|---|
| HOURS, N (%) | ||
| • < 2 | 10.0 (34) | 74.0 (63) |
| • 2 < 4 | 13.0 (45) | 34.0 (29) |
| • 4 < 6 | 4.0 (14) | 5.0 (4) |
| • ≥ 6 | 2.0 (7) | 5.0 (4) |
| Maximum, h | 18.0 | 3.0 |
| Mean, h | 3.1 | 1.8 |
| Median, h | 2.0 | 1.5 |
Four cases had missing responses for time spent vising a physician.
DISCUSSION
Acute otitis media is a common occurrence in families with young children and a substantial cause of disturbance, health services use, and indirect costs. Results of this national survey showed that only 6% of children who presumably had AOM were not seen by physicians. Although the time spent on medical visits was high for the small number of children brought to the emergency department, overall results are reassuring as to the accessibility of primary health care in Canada. To our knowledge, this is the first study that estimated the burden of AOM on Canadian families. Even if estimated family costs of AOM seem relatively low, the burden of AOM on Canadian families is important; a substantial proportion of caregivers also missed an average of 2 days of work during their children’s last AOM episodes.
This study has several limitations. The occurrence of AOM was lower than what would have been expected, assuming an annual rate of 60 cases of AOM per 100 children younger than 6 years of age.19 However, the study was conducted in May to June 2008, right after the winter season when most AOM cases occur; therefore, there is no reason to believe that an important recall bias is present. It is worth noting that the 2007 to 2008 influenza season was of relatively low intensity, which might somewhat diminish the incidence of AOM.
We used a telephone survey, which can typically result in a recruitment bias toward more educated people and against young or new residents of communities who do not have household telephone numbers.29 However, it is known that in Canada most families with young children have been residents of the same community for several years and most of them have household telephone numbers. In 2008, 8% of Canadian households reported having cellular telephones only, and less than 1% did not have any telephone services.30 In addition, the survey sample was chosen by stratified random sampling of households in 5 Canadian regions, ensuring that the number of participants was proportional to each region’s population, diminishing the risk of selection bias.31
Results of randomized controlled trials have shown that antibiotic treatment is associated with a more favourable clinical course than placebo, but the overall benefit is rather small; this is a justification for the wait-and-see approach.32 Most AOM episodes analyzed in this study resulted in at least 1 medical visit. Additionally, despite the new guidelines recommending a wait-and-see approach for the management of AOM, almost all medical visits resulted in antibiotic use. Reported use of antibiotics in our study is comparable with that observed in another study conducted more than a decade ago in Ontario.33 These similarities show that no important changes have taken place in AOM treatment strategies or in parents’ decisions to seek medical consultation for their children with AOM, despite the changes to official recommendations. Similar findings were identified in previous US studies in which only a minority of family physicians and pediatricians routinely recommended the wait-and-see approach for the management of AOM, despite available scientific evidence of its safety and years of promotion.34–36 Authors of a recent study in Finland and the Netherlands suggested that changes in treatment practices for AOM require strong guidelines and education of physicians, but also a modification of parental expectations regarding the usefulness of antibiotics.37 Primary prevention using pneumococcal conjugate and influenza vaccines is a potentially more interesting and feasible avenue, and specific studies are required to demonstrate whether the immunization programs recently implemented in all Canadian provinces and territories effectively reduce AOM incidence, antibiotic use, and associated costs.
EDITOR’S KEY POINTS
Almost all cases of acute otitis media (AOM) described in this study were treated with antibiotics; extensive use of antibiotics causes resistance, which results in decreased treatment performance and meaningful economic burden.
Caregiver time is an important factor associated with the burden of AOM; travel, waiting room, and medical examination time as well as time taken off work all contribute to the indirect costs associated with this condition.
Burden of AOM on families has received limited attention when the cost-effectiveness of AOM prevention and treatment programs has been assessed in the past. Results of this study indicate that this burden remains important in a country with well-established childhood immunization programs.
POINTS DE REPÈRE DU RÉDACTEUR
Presque tous les cas d’otite moyenne aiguë (OMA) rapportés dans cette étude ont été traités par antibiotiques: une importante utilisation d’antibiotiques est une source de résistance, ce qui entraîne de moins bons résultats du traitement en plus d’un fardeau économique appréciable.
Le temps exigé des soignants est un facteur important qui s’ajoute au fardeau qu’imposent les OMA; les périodes consacrées au déplacement, à la salle d’attente et à l’examen médical en plus du temps de travail perdu contribuent tous aux coûts indirects de cette condition.
Lorsqu’on a évalué le rapport coûts/bénéfices des programmes de prévention et de traitement de l’OMA dans le passé, on s’est peu préoccupé du fardeau imposé aux familles. Les résultats de cette étude indiquent que ce fardeau demeure important dans un pays qui dispose d’un programme de vaccination pour enfants bien établi.
Footnotes
This article has been peer reviewed.
Cet article a fait l’objet d’une révision par des pairs.
This article is eligible for Mainpro-M1 credits. To earn credits, go to www.cfp.ca and click on the Mainpro link.
Contributors
All authors contributed to the concept and design of the study; data gathering, analysis, and interpretation; and preparing the manuscript for submission.
Competing interests
This study was supported by an unrestricted research grant from GlaxoSmithKline. No private company or its employees were involved in designing the study protocol and questionnaire or in collecting, analyzing, and interpreting data.
References
- 1.Klein JO. The burden of otitis media. Vaccine. 2000;19(Suppl 1):S2–8. doi: 10.1016/s0264-410x(00)00271-1. [DOI] [PubMed] [Google Scholar]
- 2.Wals PD, Carbon M, Sévin E, Deceuninck G, Ouakki M. Reduced physician claims for otitis media after implementation of pneumococcal conjugate vaccine program in the province of Quebec, Canada. Pediatr Infect Dis J. 2009;28(9):e271–5. doi: 10.1097/INF.0b013e3181bad212. [DOI] [PubMed] [Google Scholar]
- 3.Poirier B, De Wals P, Petit G, Erickson LJ, Pépin J. Cost-effectiveness of a 3-dose pneumococcal conjugate vaccine program in the province of Quebec, Canada. Vaccine. 2009;27(50):7105–9. doi: 10.1016/j.vaccine.2009.09.057. Epub 2009 Sep 26. [DOI] [PubMed] [Google Scholar]
- 4.Teele DW, Klein JO, Rosner B. Epidemiology of otitis media during the first seven years of life in children in greater Boston: a prospective, cohort study. J Infect Dis. 1989;160(1):83–94. doi: 10.1093/infdis/160.1.83. [DOI] [PubMed] [Google Scholar]
- 5.Casselbrant ML, Mandel EM. Epidemiology. In: Rosenfeld RM, Bluestone CD, editors. Evidence-based otitis media. Hamilton, ON: Decker Publishing Inc; 1999. pp. 117–36. 1999. [Google Scholar]
- 6.Jahn-Eimermacher A, du Prel JB, Schmitt HJ. Assessing vaccine efficacy for the prevention of acute otitis media by pneumococcal vaccination in children: a methodological overview of statistical practice in randomized controlled clinical trials. Vaccine. 2007;25(33):6237–44. doi: 10.1016/j.vaccine.2007.05.062. [DOI] [PubMed] [Google Scholar]
- 7.Spiro DM, Arnold DH. The concept and practice of a wait-and-see approach to acute otitis media. Curr Opin Pediatr. 2008;20(1):72–8. doi: 10.1097/MOP.0b013e3282f2fa62. [DOI] [PubMed] [Google Scholar]
- 8.Del Mar C, Glasziou P, Hayem M. Are antibiotics indicated as initial treatment for children with acute otitis media? A meta-analysis. BMJ. 1997;314(7093):1526–9. doi: 10.1136/bmj.314.7093.1526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Rosenfeld RM, Vertrees JE, Carr J, Cipolle RJ, Uden DL, Giebink GS, et al. Clinical efficacy of antimicrobial drugs for acute otitis media: metaanalysis of 5400 children from thirty-three randomized trials. J Pediatr. 1994;124(3):355–67. doi: 10.1016/s0022-3476(94)70356-6. [DOI] [PubMed] [Google Scholar]
- 10.Glasziou PP, Del Mar CB, Sanders SL, Hayem M. Antibiotics for acute otitis media in children. Cochrane Database Syst Rev. 2004;(1):CD000219. doi: 10.1002/14651858.CD000219.pub2. [DOI] [PubMed] [Google Scholar]
- 11.Pichichero ME, Casey JR. Emergence of a multiresistant serotype 19A pneumococcal strain not included in the 7-valent conjugate vaccine as an otopathogen in children. JAMA. 2007;298(15):1772–8. doi: 10.1001/jama.298.15.1772. [DOI] [PubMed] [Google Scholar]
- 12.Straetemans M, Sanders EA, Veenhoven RH, Schilder AG, Damoiseaux RA, Zielhuis GA. Pneumococcal vaccines for preventing otitis media. Cochrane Database Syst Rev. 2004;(1):CD001480. doi: 10.1002/14651858.CD001480.pub2. [DOI] [PubMed] [Google Scholar]
- 13.Manzoli L, Schioppa F, Boccia A, Villari P. The efficacy of influenza vaccine for healthy children: a meta-analysis evaluating potential sources of variation in efficacy estimates including study quality. Pediatr Infect Dis J. 2007;26(2):97–106. doi: 10.1097/01.inf.0000253053.01151.bd. [DOI] [PubMed] [Google Scholar]
- 14.De Wals P, Erickson L, Poirier B, Pépin J, Pichichero ME. How to compare the efficacy of conjugate vaccines to prevent acute otitis media. Vaccine. 2009;27(21):2877–83. doi: 10.1016/j.vaccine.2009.02.102. Epub 2009 Mar 10. [DOI] [PubMed] [Google Scholar]
- 15.Wyeth Canada . Prevnar 13 [product monograph] Montreal, QC: Wyeth Canada; 2009. Available from: www.wyeth.ca/en/products/Product%20Monographs%20PDFs/Prevnar_13_Product_Monograph_Dec_21_2009_EN.pdf. Accessed 2010 Nov 17. [Google Scholar]
- 16.Prymula R, Peeters P, Chrobok V, Kriz P, Novakova E, Kaliskova E, et al. Pneumococcal capsular polysaccharides conjugated to protein D for prevention of acute otitis media caused by both Streptococcus pneumoniae and non-typable Haemophilus influenzae: a randomised double-blind efficacy study. Lancet. 2006;367(9512):740–8. doi: 10.1016/S0140-6736(06)68304-9. [DOI] [PubMed] [Google Scholar]
- 17.Forgie S, Zhanel G, Robinson J. Management of acute otitis media. Paediatr Child Health. 2009;14(7):457–64. [PMC free article] [PubMed] [Google Scholar]
- 18.Petit G, De Wals P, Law B, Tam T, Erickson LJ, Guay M, et al. Epidemiological and economic burden of pneumococcal diseases in Canadian children. Can J Infect Dis. 2003;14(4):215–20. doi: 10.1155/2003/781794. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Morrow A, De Wals P, Petit G, Guay M, Erickson LJ. The burden of pneumococcal disease in the Canadian population before routine use of the seven-valent pneumococcal conjugate vaccine. Can J Infect Dis Med Microbiol. 2007;18(2):121–7. doi: 10.1155/2007/713576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Asmussen L, Olson LM, Sullivan SA. “You have to live it to understand it”: family experiences with chronic otitis media in children. Ambul Child Health. 1999;5:303–12. [Google Scholar]
- 21.Forgays DK, Hasazi JE, Wasserman RC. Recurrent otitis media and parenting stress in mothers of two-year-old children. J Dev Behav Pediatr. 1992;13(5):321–5. [PubMed] [Google Scholar]
- 22.Rosenfeld RM, Goldsmith AJ, Tetlus L, Balzano A. Quality of life for children with otitis media. Arch Otolaryngol Head Neck Surg. 1997;123(10):1049–54. doi: 10.1001/archotol.1997.01900100019002. [DOI] [PubMed] [Google Scholar]
- 23.Brouwer CN, Rovers MM, Maillé AR, Veenhoven RH, Grobbee DE, Sanders EA, et al. The impact of recurrent acute otitis media on the quality of life of children and their caregivers. Clin Otolaryngol. 2005;30(3):258–65. doi: 10.1111/j.1365-2273.2005.00995.x. [DOI] [PubMed] [Google Scholar]
- 24.Boruk M, Lee P, Faynzilbert Y, Rosenfeld RM. Caregiver well-being and child quality of life. Otolaryngol Head Neck Surg. 2007;136(2):159–68. doi: 10.1016/j.otohns.2006.09.005. [DOI] [PubMed] [Google Scholar]
- 25.Haggard MP, Smith SC. Impact of otitis media on child quality of life. In: Rosenfeld RM, Bluestone CD, editors. Evidence-based otitis media. Hamilton, ON: Decker Publishing Inc; 1999. pp. 375–98. [Google Scholar]
- 26.Dubé E, De Wals P, Gilca V, Boulianne N, Ouakki M, Lavoie F, et al. New vaccines offering a larger spectrum of protection against acute otitis media: will parents be willing to have their children immunized? Int J Pediatr Otorhinolaryngol. 2009;73(7):987–91. doi: 10.1016/j.ijporl.2009.03.022. Epub 2009 May 6. [DOI] [PubMed] [Google Scholar]
- 27.Dubé E, De Wals P, Gilca V, Boulianne N, Ouakki M, Lavoie F. Burden of acute otitis media: knowledge, attitudes, and beliefs of Canadian parents. Poster presented at the Canadian Paediatric Society 86th Annual Conference; 2009 Jun 23–27; Ottawa, ON. [Google Scholar]
- 28.De Wals P, Blackburn M, Guay M, Bravo G, Blanchette D, Douville-Fradet M. Burden of chickenpox on families. A study in Quebec. Can J Infect Dis. 2001;12(1):27–32. doi: 10.1155/2001/361070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Dillman DA. Mail and telephone surveys. The total design method. Hoboken, NJ: John Wiley & Sons, Inc; 1978. [Google Scholar]
- 30.Statistics Canada . Residential telephone service survey. Ottawa, ON: Statistics Canada; 2008. Available from: www.statcan.gc.ca/daily-quotidien/090615/dq090615c-eng.htm. Accessed 2010 Nov 18. [Google Scholar]
- 31.Statistics Canada . Families and households highlight tables, 2006 census. Ottawa, ON: Statistics Canada; 2007. Catalogue no. 97-551-XWE2006002. Available from: www12.statcan.ca/census-recensement/2006/dp-pd/hlt/97-553/index.cfm?Lang=E. Accessed 2010 Nov 18. [Google Scholar]
- 32.Vouloumanou EK, Karageorgopoulos DE, Kazantzi MS, Kapaskelis AM, Falagas ME. Antibiotics versus placebo or watchful waiting for acute otitis media: a meta-analysis of randomized controlled trials. J Antimicrob Chemother. 2009;64(1):16–24. doi: 10.1093/jac/dkp166. Epub 2009 May 19. [DOI] [PubMed] [Google Scholar]
- 33.Pennie RA. Prospective study of antibiotic prescribing for children. Can Fam Physician. 1998;44:1850–6. [PMC free article] [PubMed] [Google Scholar]
- 34.Finkelstein JA, Stille CJ, Rifas-Shiman SL, Goldmann D. Watchful waiting for acute otitis media: are parents and physicians ready? Pediatrics. 2005;115(6):1466–73. doi: 10.1542/peds.2004-1473. [DOI] [PubMed] [Google Scholar]
- 35.Vernacchio L, Vezina RM, Mitchell AA. Knowledge and practices relating to the 2004 acute otitis media clinical practice guideline: a survey of practicing physicians. Pediatr Infect Dis J. 2006;25(5):385–9. doi: 10.1097/01.inf.0000214961.90326.d0. [DOI] [PubMed] [Google Scholar]
- 36.Vernacchio L, Vezina RM, Mitchell AA. Management of acute otitis media by primary care physicians: trends since the release of the 2004 American Academy of Pediatrics/American Academy of Family Physicians clinical practice guideline. Pediatrics. 2007;120(2):281–7. doi: 10.1542/peds.2006-3601. [DOI] [PubMed] [Google Scholar]
- 37.Tähtinen PA, Boonacker CW, Rovers MM, Schilder AG, Huovinen P, Liuksila PR, et al. Parental experiences and attitudes regarding the management of acute otitis media—a comparative questionnaire between Finland and The Netherlands. Fam Pract. 2009;26(6):488–92. doi: 10.1093/fampra/cmp055. Epub 2009 Sep 3. [DOI] [PubMed] [Google Scholar]


