ABSTRACT
Purpose: The purpose of this study was to develop a paediatric cardiopulmonary physiotherapy (CPT) discharge tool. We report on the initial stages of its development and the tool's sensibility (face/content validity, feasibility, and ease of usage).
Methods: Using a modified Delphi technique, a panel of paediatric physiotherapy clinicians and academic leaders in the area of CPT (n=25) was recruited. Four rounds of discussion among the members of the Delphi panel focused on (1) generation of discharge items, (2) reduction of items, (3) discussion of contentious items and refinement of criterion definitions, and (4) determination of scoring options for the test instrument. The sensibility of a draft of the tool was assessed using a sample of convenience (n=15).
Results: Six items (auscultation, discharge planning, mobility, oxygen saturation, secretion clearance, and signs of respiratory distress) were identified for inclusion in the tool. The global mean of all sensibility domains was 6.4 (median=6.6) of a possible 7.0.
Conclusion: Using a modified Delphi process, we developed a six-item paediatric CPT discharge planning tool with good face and content validity. Future work will determine the scoring method for using this tool, interrater reliability, and predictive validity to facilitate optimal timing of hospital discharge for paediatric CPT patients.
Key Words: cardiorespiratory physiotherapy, Delphi technique, discharge criteria, measurement, tool development
RÉSUMÉ
Objectif : L'objectif de cette étude était de créer un outil d'évaluation pour permettre d'accorder leur congé aux patients en physiothérapie cardiorespiratoire pédiatrique (PCP). Nous avons fait rapport sur les étapes initiales de conception de cet outil et sur sa sensibilité (validité apparente et validité du contenu, applicabilité et facilité d'utilisation).
Méthode : À l'aide d'une version modifiée de la technique Delphi, un groupe de physiothérapeutes cliniciens en pédiatrie et de chefs de file du milieu universitaire (n=25) a été mis sur pied. Quatre rondes de discussions ont eu lieu parmi les membres de ce groupe Delphi et ont permis, respectivement : (1) de générer les éléments permettant de justifier un congé ; (2) de réduire le nombre de ces éléments ; (3) de discuter des points litigieux et de raffiner les définitions de ces divers critères ; et (4) de préciser les possibilités de pointage pour l'outil appelé à faire l'objet de tests. La sensibilité de l'outil ayant servi d'ébauche a été évaluée à l'aide d'un échantillon de commodité (n=15).
Résultats : Six points (auscultation, planification du congé, mobilité, saturation en oxygène, dégagement des sécrétions et signes de détresse respiratoire) ont été définis pour faire partie de l'outil. La moyenne globale de tous les domaines de sensibilité était de 6,4 (point médian : 6,6) sur une possibilité de 7,0.
Conclusion : À l'aide d'une version modifiée du processus Delphi, nous avons élaboré un outil de planification des congés comportant six points et bénéficiant d'une bonne validité apparente et d'une bonne validité de contenu. Des travaux futurs permettront d'établir la méthode de pointage nécessaire à l'utilisation de cet outil, la fiabilité des inter-évaluateurs et la validité prédictive visant à faciliter le congé à un moment optimal pour les patients en physiothérapie cardiorespiratoire pédiatrique.
Mots clés : critères de congé, élaboration d'un outil, mesure, physiothérapie cardiorespiratoire, technique Delphi
INTRODUCTION
Cardiorespiratory physical therapy (CPT) is an important component of the perioperative care received by children who have undergone upper-abdominal, thoracic, or cardiac surgery. CPT aims to prevent and manage postoperative respiratory complications such as pneumonia and atelectasis. In an age of careful attention to evidence-based practice and to minimizing health care expenditures through early discharge from the acute-care setting, it is important to establish criteria to justify the delivery and/or cessation of physiotherapy (PT) services. Ambiguity in determining readiness for discharge from CPT could lead to the unnecessarily extended use of PT resources or, conversely, to premature discharge from CPT. The latter may result in increased use of health care resources through re-referral to service and in delayed achievement of outcomes for patients.
A preliminary postoperative physiotherapy discharge scoring tool (POP-DST) has been developed for the adult population,1 specifically for patients who have undergone thoracic, cardiovascular, or upper-abdominal surgery. Although children have the potential to develop similar postoperative complications to adults,2 and the biological rationale for perioperative CPT in paediatrics is similar to that in adults,3 it is not intuitive that an adult tool can automatically be applied in a paediatric population. The criteria for children may be different than those for adults, which would require the development of a new tool.
This article reports the preliminary development of a paediatric CPT discharge tool that can be used to predict whether a postoperative paediatric patient can successfully be discharged from CPT. Specifically, the article describes how the content of the tool was determined and how the sensibility (face and content validity, feasibility, and ease of usage) of the draft of the tool was evaluated.
METHODS
The research ethics boards of the Hospital for Sick Children and the University of Toronto approved this study.
Recruitment of Panellists
A Web search was conducted to identify all Canadian universities offering a PT programme (n=11) and all major Canadian paediatric acute-care centres (n=12).
Recruitment packages were sent to the CPT course instructors and to faculty researchers in the area of CPT at each of the 11 universities. The university cover letter requested the participation of academic leaders in the area of CPT. An academic leader was defined as an individual with an academic appointment in a PT programme who is responsible for providing the CPT curriculum or an individual doing research in the area of CPT.
Recruitment packages were sent to the director of PT (or equivalent) at the paediatric acute-care centres for distribution to physiotherapists on the CPT team. Clinicians were required to have a minimum of 2 years experience in paediatric physiotherapy, with CPT constituting at least 25% of their caseload, and to have completed at least one continuing-education course in CPT or a related topic. Panellists returned a signed consent form if they were willing to participate in the study.
No formal sample-size calculation is offered in the literature. Published Delphi studies have used between <20 and >2,000 panellists.4 For this study, it was decided that an initial Delphi panel of 20 members would be recruited.
Modified Delphi Technique
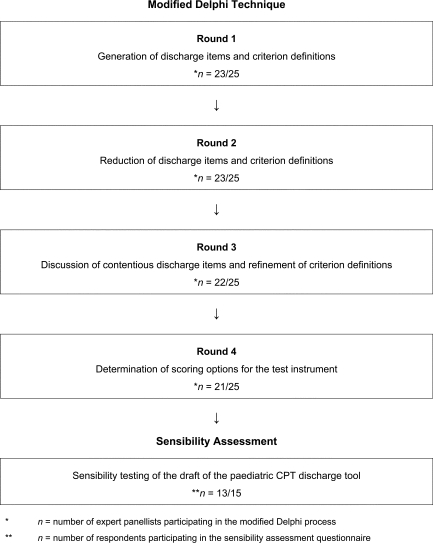
A modified Delphi technique4 was used in the item-generation and reduction phases of tool development and for consideration of potential scoring methods. Our study used questionnaires administered by e-mail to gather qualitative information from a target group of expert academics and clinicians; each questionnaire was followed by a “round” of dialogue to gather panellists' responses, which were summarized and distributed to the group for further consideration. The four rounds addressed (1) generation of discharge items; (2) reduction of items; (3) discussion of contentious items and refinement of criterion definitions; and (4) determination of scoring options for the test instrument (see Figure 1). Panellists had 2 weeks to complete the questionnaire for each round. If a completed questionnaire was not returned, one reminder e-mail was sent to encourage continued participation.
Figure 1.
Methods for tool development
Unlike the classic Delphi technique, in which the process continues until 100% consensus is achieved, the modified process continues until an a priori consensus threshold has been reached with respect to the topic of interest. A standard recommendation for an appropriate level of consensus does not exist for the Delphi technique, and suggestions in the literature range from 51% to 80%.5–9 We determined a priori that a 70% consensus threshold would be used. This threshold represents a value higher than the midpoint of the previous ranges reported, and was therefore felt to be appropriate. The Delphi technique offers many advantages over other group-consensus methods, including giving each panellist an anonymous and equal voice, involving relatively low costs, and overcoming geographical constraints.
Round 1: Generation of Discharge Items and Criterion Definitions
The purpose of round 1 was to generate all possible clinical phenomena or items appropriate for inclusion in the paediatric CPT discharge tool, as well as criterion definitions for those items. As part of the round 1 questionnaire, panellists were given a framework outlining the concept (readiness for discharge from CPT), the relevant population (children aged 2 to under 19 who are postoperative from upper-abdominal, cardiac, or thoracic surgery in a ward setting), and the purpose of the measure (to predict which children can be successfully discharged from CPT). Panellists were also given a glossary of working definitions and a list of items from the POP-DST1 for their consideration. Readiness for discharge was defined as the absence of cardiorespiratory impairments or the ability to manage those impairments independently with or without family support. The panellists were instructed to list clinical phenomena or items that they felt were appropriate for inclusion in the paediatric CPT discharge tool and to provide criterion definitions for each of those items.
Round 2: Reduction of Discharge Items and Criterion Definitions
The purpose of round 2 was to begin reducing the number of items and their criterion definitions. In this round, panellists were asked to review the items and criterion definitions generated by the panel in round 1 and to state whether or not they thought each was a clear, feasible, and appropriate item or definition to be included in the paediatric CPT discharge tool. They were also asked to make comments on or suggest revisions to any item or criterion definition as they considered necessary, especially those they found unclear, not feasible, or inappropriate. Where an item or definition did not achieve 70% consensus on its appropriateness and/or feasibility, it was eliminated. If an item or criterion definition was below the consensus threshold only with respect to clarity, it was retained, and panellists' comments/suggestions were used to improve the item descriptor or definition. For items with multiple criterion definitions, the panellists were also asked to reverse rank the top five definitions (5=most suitable definition, 1=least suitable definition) for inclusion in the paediatric CPT discharge tool. (For items with more than one but fewer than five definitions to choose from, panellists were asked to reverse rank them such that the highest number indicated the most suitable.) The reverse rankings were summed; the highest sum reflected the most preferred definition. Although the purpose of this round was to reduce the number of discharge items, panellists were also given a final opportunity to suggest any additional clinical phenomena or items and/or criterion definitions that they felt were missed during item generation in round 1.
Round 3: Discussion of Contentious Items and Refinement of Criterion Definitions
The primary purpose of round 3 was to reduce the criterion definitions to one definition per item. The secondary purpose was to confirm the panellists' opinion on the two “controversial” items that achieved only the minimum consensus threshold for retention in round 2.
Panellists were asked to review the results from round 2 and then to restate, using yes/no responses, whether they thought the two controversial items were appropriate, clear, and feasible for inclusion in the paediatric CPT discharge tool. Next, the panellists were asked to review the criterion definitions retained after round 2 for each item and to state (using yes/no responses) whether they thought each was an appropriate, feasible, and clear definition of the item it represented. Panellists were given the opportunity to make comments and/or revisions to the definitions. Finally, panellists were again asked to reverse rank the criterion definitions in terms of their suitability for inclusion in the paediatric CPT discharge tool, in order to allow for final reduction of the definitions to one per item.
Round 4: Determination of Scoring Options for the Test Instrument
The purpose of this round was to consider scoring options for the draft of the paediatric CPT discharge tool. Panellists were asked to review the results from round 3, specifically the remaining items and the single criterion definition identified for each item. A draft of the paediatric CPT discharge tool was presented for their consideration.
To address the issue of scoring, panellists were asked to consider three scoring options for the tool. Scoring option 1 (critical items approach) required panellists to identify a single item, a pair of items, or a combination of three or more items that would prevent them from discharging a paediatric patient from CPT following upper-abdominal, cardiac, or thoracic surgery. Scoring option 2 (importance/summing approach) involved weighting the items in the tool based on rankings of importance. Scoring option 3 involved the panellists' recommending a scoring method of their own.
After considering these scoring options, each panellist was asked to recommend one option. Based on their choices, each was then asked to complete a more detailed questionnaire specific to that scoring option only.
Panellists who recommended the critical items approach were asked to identify which item, pair of items, or combination of three items would prevent them from discharging a paediatric patient from postoperative CPT if the criterion definition(s) for that item or items were not met.
Panellists who recommended the importance/summing scoring approach were asked to rate the six items included in the draft of the paediatric CPT discharge tool on a six-point scale (1=least important, 6=most important). The same rating could be given to more than one item; therefore, not all ratings were necessarily used.
Panellists who recommended their own scoring method were asked to describe that method in detail.
Sensibility Assessment
Sensibility is defined as “enlightened common sense,” a mixture of common sense and a reasonable knowledge of pathophysiology and clinical reality.10–13 A sensibility assessment evaluates the purpose and framework, overt format, face validity (appropriate response categories, suitable phrasing), content validity (inappropriate inclusions or omissions), and ease of use of the tool.10–13 The purpose of this phase of the study was to complete a sensibility assessment of the draft of the paediatric CPT discharge tool.
Upon completion of round 4 of the modified Delphi process, a draft of the discharge tool, including an instructions page, was mailed to a local sample of convenience. The sample consisted of physiotherapists working on the CPT team or providing evening and weekend paediatric CPT coverage at the Hospital for Sick Children in Toronto, Canada (n=15). They were asked to review the tool and the accompanying instructions and then complete a sensibility questionnaire (adapted from the work of Rowe and Oxman,12 who developed a sensibility questionnaire to evaluate a quality-of-life instrument). We did not alter the intent of the questions from Rowe and Oxman's questionnaire12 but, rather, adapted them to include language relevant to our discharge tool. We also include three additional questions, which asked participating physiotherapists whether they felt the paediatric CPT discharge tool would be useful in (1) helping newly graduated physiotherapists determine a patient's readiness for discharge, (2) helping evening and weekend physiotherapists determine a patient's readiness for discharge, and 3) helping physiotherapists communicate with the multidisciplinary team—all intended areas of benefit from the implementation of such a tool.
The questionnaire evaluated the purpose and framework, format, face validity, content validity, and ease of use of the tool through a series of 15 items (see Table 1). Each item was rated using a seven-point Likert scale (1=unacceptable, 7=excellent).
Table 1.
Sensibility Assessment Questionnaire
| Item* | |
|---|---|
| 1 | How would you rate the tool in terms of clarity? |
| 2 | How would you rate the tool in terms of simplicity? |
| 3 | Were the instructions provided with the tool adequate? |
| 4 | How would you rate the amount of time you feel it would take to complete the paediatric CPT discharge tool? |
| 5 | How would you rate the amount of equipment needed to complete the paediatric CPT discharge tool? |
| 6 | The tool was designed to determine a postoperative paediatric patient's readiness for discharge after cardiac, thoracic, or upper-abdominal surgery. To what extent do you think this goal has been achieved? |
| 7 | How many of the items are crucial or necessary? |
| 8 | How many of the items are redundant? |
| 9 | Are there any important items that should be included in a paediatric CPT discharge tool that have not been included? |
| 10 | How likely is the discharge tool to determine when a patient is ready to be discharged from CPT after undergoing cardiac, thoracic, or upper-abdominal surgery? |
| 11 | Would the tool be acceptable to other paediatric physiotherapists in terms of the clarity of the items, the comprehensiveness of the tool, and the amount of time it would take to complete the tool? |
| 12 | Would you agree to incorporate the use of this tool into your clinical practice? |
| 13 | In your opinion, would the tool be useful to help new graduates determine a paediatric patient's readiness for discharge from CPT? |
| 14 | In your opinion, would the tool be useful to help evening and weekend physiotherapists determine a paediatric patient's readiness for discharge from CPT? |
| 15 | In your opinion, would the tool be useful to help physiotherapists communicate with multidisciplinary team members regarding a paediatric patient's readiness for discharge from CPT? |
Questions were answered using a seven-point Likert scale (1=unacceptable, 7=excellent).
Data Analysis
In round 1, the primary investigator (CE) collated the panellists' responses (items and criterion definitions) by copying and pasting them into a Microsoft Word document to avoid transcription error or bias. The collated data were reviewed by the research team, and the panellists' responses were grouped into categories based on consensus with respect to similarity of content.
In rounds 2 and 3, raw percentages of yes/no responses were calculated to determine the panel's opinion on the appropriateness, feasibility, and clarity of the items and criterion definitions generated in round 1. The panellists' rankings of the criterion definitions were summed. In order to ensure that differences in the sums of the rankings of different criterion definitions were statistically significant, p-values were calculated based on the Friedman test. If statistical significance was achieved (p<0.05) when testing all the definitions for a given item, pair-wise Wilcoxon signed rank tests were then performed to determine where the pair-wise difference was within the group of definitions. No adjustment was made for multiple comparisons.
In round 4, raw percentages of panellists' scoring-method choices were calculated to determine which scoring option was the most preferred.
Analysis of the data from the sensibility assessment was accomplished by calculating mean scores from the therapists' individual responses. Mean scores were also calculated for each individual questionnaire item. A priori hypotheses were set to evaluate the results of the questionnaire. It was determined a priori that the individual components would be judged to be sensible if the mean scores for each question were ≥6/7 and that the tool would be judged to be sensible overall if the mean scores provided by the therapists were ≥6/7. Additionally, the mean score for all the questions for each respondent had to be ≥6/7. Because of the potential for outlying data to affect the mean when working with a small sample size, median scores were also calculated.
Individual numeric responses were transcribed into the Statistical Package for Social Sciences (SPSS) version 12.0 (SPSS Inc., Chicago, IL), and proportions and means were calculated as appropriate to the data to describe the sample characteristics in each modified Delphi round and in the sensibility assessment, as described above.
RESULTS
Participants' Delphi Process
A total of 25 individuals returned signed consent forms in response to the recruitment letters. Six of the 25 panellists (24%) were academic leaders in the area of CPT, and 19 (76%) were paediatric physiotherapy clinicians. Of these, 23 (5 academic leaders and 18 clinicians) returned the demographic questionnaire and participated in at least one Delphi round. Demographic data for the panellists are given in Table 2.
Table 2.
Demographic Information for Participating Modified Delphi Panellists (n=23)
|
Academic Leaders (n=5) n (%) |
Clinicians (n=18) n (%) |
|
|---|---|---|
| Current practice location* | ||
| University | 5 (100) | 0 (0) |
| University-affiliated hospital | 1 (20) | 18 (100) |
| Non-university-affiliated hospital | 0 (0) | 0 (0) |
| Region | ||
| West | 0 (0) | 3 (17) |
| Ontario | 4 (80) | 11 (61) |
| Quebec | 0 (0) | 3 (17) |
| East | 1 (20) | 1 (5) |
| Education* | ||
| BA | 1 (20) | 1 (5) |
| BMR-PT/BScPT | 3 (60) | 17 (94) |
| Master's level | 4 (80) | 3 (17) |
| Continuing-education courses in CPT (in last 10 years) |
||
| <5 | 1 (20) | 12 (67) |
| >5 | 0 (0) | 6 (33) |
| >10 | 4 (80) | 0 (0) |
| Primary work responsibility | ||
| Academic teaching | 0 (0) | 1 (5) |
| Clinical practice | 1 (20) | 16 (89) |
| Management | 0 (0) | 1 (5) |
| Research | 4 (80) | 0 (0) |
| Time providing CPT | ||
| 0–25% | 5 (100) | 2 (11) |
| 25–49% | 0 (0) | 3 (17) |
| 50–74% | 0 (0) | 5 (28) |
| 75–100% | 0 (0) | 8 (44) |
| Time in research | ||
| 0–25% | 2 (40) | 16 (89) |
| 25–49% | 2 (40) | 2 (11) |
| 50–74% | 0 (0) | 0 (0) |
| 75–100% | 1 (20) | 0 (0) |
| Time in academic teaching | ||
| 0–25% | 2 (40) | 16 (89) |
| 25–49% | 3 (60) | 1 (5) |
| 50–74% | 0 (0) | 1 (5) |
| 75–100% | 0 (0) | 0 (0) |
| Previous consensus experience? | 4 (80) | 5 (28) |
Panellists could specify more than one practice location or degree.
Round 1: Generation of Discharge Items and Criterion Definitions
The response rate for this round was 92% (n=23/25). Two panellists did not return their completed questionnaires within the requested time frame and did not respond after the reminder e-mail was sent. The round 1 questionnaire generated a total of 43 clinical phenomena or items, 24 of which demonstrated conceptual overlap or duplication with at least one other item. In order to streamline the data, these items were grouped together for consideration after review by the research team. Chest x-ray and radiological evidence were grouped together, as were auscultation findings and breath sounds, level of activity and activity tolerance, pain and pain control, respiratory pattern and breathing pattern, oxygen saturation and pulse oximetry, mobility and ambulation, and upper-extremity movement and range of motion. Signs of respiratory distress, work of breathing, observation, and breathing effort were grouped, as were airway clearance, secretion clearance, cough, and suctioning. This left a final list of 29 clinical phenomena or items, as shown in Table 3.
Table 3.
Round 1 Results: Streamlined Clinical Phenomena
| Clinical Phenomenon / Item |
Suggested by (n) |
|---|---|
| Secretion clearance / Airway clearance / Cough / Suctioning | 23 |
| Breath sounds / Auscultation findings | 22 |
| Mobility/Ambulation | 22 |
| Oxygen saturation (SpO2) / Pulse oximetry | 19 |
| Respiratory rate | 12 |
| Signs of respiratory distress / Work of breathing / Observation / Breathing effort | 7 |
| Oxygen requirements | 5 |
| Chest X-ray / Radiological evidence | 5 |
| Pain / Pain control | 5 |
| Upper-extremity movement / Range of motion | 4 |
| Respiratory pattern / Breathing pattern | 3 |
| Activity tolerance / Level of activity | 2 |
| Heart rate | 2 |
| Activities of daily living | 1 |
| Adherence to recommended treatment plan | 1 |
| Bed mobility | 1 |
| Blood pressure | 1 |
| Chest wall mobility | 1 |
| Clinical exam | 1 |
| Dyspnea | 1 |
| Education | 1 |
| Exercise capacity | 1 |
| Family readiness to assume CR care if ongoing | 1 |
| Home environment | 1 |
| Level of function | 1 |
| Posture | 1 |
| Potential for recurrence of acute respiratory deterioration | 1 |
| Temperature | 1 |
| Therapy routine | 1 |
Multiple criterion definitions were generated for 13 of the 29 clinical phenomena / items; for example, panellists generated 22 different criterion definitions for mobility, 18 for auscultation, and 17 for oxygen saturation. Because of the large volume of data, the criterion definitions were grouped together by the research team if they were considered to address the same concept using different wording, and the panellists were presented with the streamlined criterion definitions in round 2.
Round 2: Reduction of Discharge Items and Criterion Definitions
The response rate in this round remained at 92% (23/25). A total of 20 clinical phenomena or items were eliminated in round 2 because they did not meet the 70% threshold for appropriateness and feasibility, leaving nine items for consideration in round 3, as shown in Table 4. Two of the nine items (family readiness to assume CR care if ongoing and discharge planning / education) were felt to be controversial, given that each was at the 70% threshold for either appropriateness or feasibility and below the threshold for clarity. These items were retained for consideration in round 3, but panellists were asked to restate their opinion (using yes/no responses) on the appropriateness, clarity, and feasibility of the items. Common themes were used to refine the retained items for round 3 (see boldface text in “Panellist Comments” section of Table 4). A total of 56 criterion definitions were eliminated in this round, for a variety of reasons: because the item to which the definition referred was eliminated, because 70% of the panellists did not agree that the definition was both appropriate and feasible, or because a statistically significant difference was found when the sums of the reverse rankings were tested. Comments offered by the panellists were used by the research team to improve the clarity of the definitions for consideration in future rounds. Only the final definitions are presented in the draft of the paediatric CPT discharge tool (see Appendix).
Table 4.
Round 2 Results: Retained Clinical Phenomena / Items
| Clinical Phenomenon | Appropriate (% agreement) |
Clear (% agreement) |
Feasible (% agreement) |
Panellist Comments |
|---|---|---|---|---|
| Oxygen requirements | 96 | 96 | 100 | Should be combined with item #9 (oxygen saturation). |
| Signs of respiratory distress / Work of breathing / Breathing effort |
100 | 70 | 100 | May be impacted by co-morbidities (e.g., Cardiac dysfunction). Should be combined with item #5 (respiratory rate). Should be called signs of respiratory distress. |
| Respiratory rate | 83 | 96 | 100 | Also may be impacted by cardiac co-morbidity. Should be combined with item #3 (signs of respiratory distress). It is a component of item #3. |
| Mobility | 96 | 91 | 100 | An important item. |
| Auscultation findings / Breath sounds |
100 | 83 | 100 | An important item. There are some fundamental limitations to this technique. |
| Oxygen saturation / Pulse oximetry |
100 | 91 | 96 | Need to take into account the variation in appropriate saturation for cardiac kids. Should be called oxygen saturation. Should be combined with item #2 (oxygen requirements). |
| Airway clearance / Secretion clearance / (cough, suctioning) |
100 | 78 | 96 | An important item. Should be calledsecretion clearance. |
| Family readiness to assume CR care if ongoing* |
78 | 65 | 70 | Difficult to assess—how will this be measured? Could be combined with item #29 (education). |
| Education* | 70 | 48 | 70 | May want to combine with item #19 (family readiness to assume CR care if ongoing). Should be called discharge planning. |
Percentages in the appropriate, clear, and feasible columns reflect the percentage of panellists responding “yes” for each item. Comments reflect the common themes noted from the panellists' comments. The comments in boldface type were used to refine the data for round 3.
These items were identified as “controversial” because each was at the 70% criterion for either appropriateness or feasibility.
Round 3: Discussion of Contentious Items and Refinement of Criterion Definitions
The response rate for this round was 88% (22/25); one additional panellist did not return a completed questionnaire within the requested time frame and did not respond to the reminder e-mail. In this round, items were eliminated if they did not receive 70% agreement from the panellists with respect to both appropriateness and feasibility.
Of the two items that were identified as controversial in round 2, one (family readiness to assume CR care if ongoing) was eliminated and the other (discharge planning / education) was retained. Family readiness to assume CR care if ongoing was eliminated because it did not achieve the 70% threshold for appropriateness, clarity, or feasibility (68%, 64%, and 55% respectively); discharge planning achieved the 70% threshold for appropriateness and feasibility (82% and 96% respectively) and was just below the criterion for clarity (64%). We were willing to work on improving the clarity of this item using panellists' comments and suggestions, given their consensus on the appropriateness and feasibility of this item.
The items were further refined by grouping overlapping or redundant items. Specifically, oxygen requirements and oxygen saturation were grouped together, as were signs of respiratory distress and respiratory rate. This left a total of six items for inclusion in the draft of the paediatric CPT discharge tool: auscultation, signs of respiratory distress, oxygen saturation, secretion clearance, mobility, and discharge planning.
Panellists' responses to the criterion definitions were analyzed for the six items retained for inclusion in the draft discharge tool. Further reduction of the criterion definitions was again addressed in a two-step process. In the first step, criterion definitions were eliminated if 70% agreement that they were appropriate, feasible, and clear could not be achieved. Note the inclusion of the requirement to achieve the consensus threshold for clarity in this round, as it was felt that round 2 had provided an opportunity to improve clarity based on the panellists' comments. In the second step, the reverse rankings of the remaining criterion definitions were summed to indicate the most preferred criterion definition for each item. Statistical significance was achieved (p<0.05) when testing all the definitions for a given item. Pair-wise Wilcoxon signed rank tests were then performed to determine where the pair-wise difference was within the group of definitions, and one criterion definition was identified for each item.
Round 4: Determination of Scoring Options for the Test Instrument
The response rate for this round was 84% (21/25); one additional panellist did not return a completed questionnaire within the requested time frame, and a reminder e-mail did not elicit a response. Panellists were asked to consider scoring options for the draft of the paediatric CPT discharge tool. Analysis of the round 4 data revealed that 52% (11/21) of the panellists recommended scoring method 1 (critical items approach), 43% (9/21) recommended scoring method 2 (importance/summing approach), and 5% (1/21) suggested a unique scoring method.
Analysis of the data from the questionnaire for the critical items approach revealed that 64% (7/11) of the panellists recommended using two critical items, 27% (3/11) recommended using three or more critical items, and 9% (1/11) recommended using one critical item to determine a paediatric patient's readiness for discharge from CPT after cardiac, thoracic, or upper-abdominal surgery.
Analysis of the data from the questionnaire for the importance/summing approach revealed that the sums of the ratings for the six items were not significantly different (p=0.19 based on Friedman test).
One panellist completed the questionnaire for the other suggested scoring method. This panellist recommended that all six items be weighted equally, such that a score of 6/6 would be necessary to indicate the patient's readiness for discharge.
Sensibility Testing
Of the 15 physiotherapists recruited for the sensibility testing process, 13 returned completed questionnaires. Complete demographic data on the participants are shown in Table 5. Mean and median scores were calculated for each question in the sensibility questionnaire. Of the 15 questions in the sensibility questionnaire, 14 had a mean score of 6.0 or higher (median≥6); the mean score for simplicity (item 2; see Table 1) was 5.7. The global mean for all questions was 6.4 (median=6.6). In addition, 12 of 13 questionnaire respondents had a mean score of 6 or higher; the remaining respondent's mean score was 5.5.
Table 5.
Demographic Data For Sensibility Respondents (n=13)
|
Sensibility Respondents (n=13) n (%) |
|
|---|---|
| Current practice location | |
| University | 0 (0) |
| University-affiliated hospital | 13 (100) |
| Non-university-affiliated hospital | 0 (0) |
| Region | |
| Ontario | 13 (100) |
| Education* | |
| BA | 1 (1) |
| BScPT/PTDip | 13 (100) |
| MSc | 6 (46) |
| Continuing-education courses in CPT (in last 10 years) | |
| 0–1 | 7 (54) |
| 2–4 | 6 (46) |
| Primary work responsibility | |
| Academic teaching | 0 (0) |
| Clinical practice | 13 (100) |
| Management | 0 (0) |
| Research | 0 (0) |
| Time providing CPT | |
| 0–25% | 9 (69) |
| 25–49% | 2 (15) |
| 50–74% | 1 (1) |
| 75–100% | 1 (1) |
| Time in research | |
| 0–25% | 11 (85) |
| 25–49% | 2 (15) |
| 50–74% | 0 (0) |
| 75–100% | 0 (0) |
| Time in academic teaching | |
| 0–25% | 13 (100) |
| 25–49% | 0 (0) |
| 50–74% | 0 (0) |
| 75–100% | 0 (0) |
| Previous consensus experience | 2 (15) |
Respondents could indicate more than one degree.
Incorporating Sensibility Feedback
A review of the mean scores for individual sensibility domains revealed that the simplicity domain did not achieve the a priori hypothesis of ≥6/7, with a mean of 5.7 (range: 4.0–7.0). The next lowest mean for the individual domains was for clarity, with a mean of 6.0. Although this result met the a priori hypothesis of ≥6/7, the fact that it was one of the lowest-scoring domains was cause for concern, and respondents specifically commented on the clarity of the criteria for auscultation.
The content of the tool was reformatted to improve clarity and simplicity. The criterion definitions for each item were separated more obviously, and individual checkboxes were included for each. A further effort was made to improve the clarity of the criteria for auscultation. The criteria were streamlined by incorporating consideration of breath sounds and adventitious sounds into each criterion instead of giving them as separate criteria. The instructions page was modified to reflect the changes in the tool itself.
The modified draft of the paediatric CPT discharge tool (draft 2), including an instructions page, can be found in the Appendix.
DISCUSSION
Results from this study supported the further development of a six-item paediatric CPT discharge planning tool. A large number of items (n=29) were suggested in round 1 of the modified Delphi process. Some items were suggested by the majority of panellists (e.g., mobility, n=22), while others were suggested by only one panellist (e.g., pain control). An advantage of the Delphi technique is that all items, regardless of frequency of recommendation, are included for consideration in future rounds. Furthermore, the panellists are not aware of the frequency of item suggestions, which allows for unbiased consideration of each item. One factor that may have contributed to the large number of items suggested is that the literature does not provide guidance with respect to identifying criteria that should be used when considering a paediatric patient's readiness for discharge from CPT after upper-abdominal, thoracic, or cardiac surgery. Similar factors may have also contributed to the large number of criterion definitions generated for each item in round 1. In addition, these different definitions may reflect differences in practice patterns when physiotherapists are considering a paediatric patient's readiness for discharge from CPT.
Because there was little agreement about the scoring method to be used, we were unable to develop a scoring system based on expert opinion. Further work will be required to make this determination, specifically a data-based approach that evaluates the predictive accuracy of the tool.
The a priori criteria for determining sensibility were intentionally weighted in favour of rejecting the tool, since researchers and clinicians often require impressive evidence before accepting a new tool into their practice.11,13 A tool that is not sensible is unlikely to be used by clinicians.11,13 The results of our sensibility assessment warrant proceeding with further psychometric testing of the paediatric CPT discharge tool.
Sufficient differences exist between the paediatric CPT discharge tool and the adult POP-DST1 to support the development of the paediatric CPT discharge tool. The adult tool includes five clinical phenomena or items, versus six in the paediatric tool. Both tools include auscultation, secretion clearance, mobility, and oxygen saturation; however, differences exist in the criterion definitions for each of these items. The paediatric tool includes two items, signs of respiratory distress and discharge planning, that are not used in the adult POP-DST.1 The adult tool does, however, include respiratory rate, which is included within the criterion definition for signs of respiratory distress in the paediatric tool. Discharge planning is the only item that does not demonstrate any overlap with the POP-DST.
LIMITATIONS
This study has a number of limitations. First, no formal sample-size calculation is offered in the literature, and published Delphi studies have used a wide variety of samples, ranging from 20 to 2,000 panellists;12 the size of the initial Delphi panel was relatively small (n=25), given the national recruitment approach and the task of developing a discharge tool. Two potential panellists did not return the demographic questionnaire or participate in a single Delphi round, and further attrition was seen in rounds 3 (n=1) and 4 (n=1), leaving a final panel of 21. The influence of these missing data cannot be known. Second, the Delphi panel had a limited breadth of national representation; enrolment in the panel was not stratified based on geographic area. This approach left the panel with 13% representation from western Canada, 65% from Ontario, 13% from Quebec, and 9% from eastern Canada. Furthermore, an a priori consensus threshold of 70% was used to accomplish our objectives; if the Delphi panel had been required to come to 100% agreement, further debate on the inclusion of items and/or criterion definitions might have altered the final draft of the discharge tool. Finally, a sample of convenience was used for the sensibility assessment, and the measurement properties of the questionnaire adapted from Rowe and Oxman12 were not formally evaluated prior to its use.
CONCLUSION
The main implication of this research is the identification of six clinical phenomena or items that should be considered by physiotherapists when determining a paediatric patient's readiness for discharge from CPT after upper-abdominal, cardiac, or thoracic surgery. The panel was unable to determine an appropriate scoring method for the draft of the tool. Evaluation of the interrater reliability of the individual items in the tool is currently underway. Ultimately, further research determining an appropriate scoring method and investigating the predictive validity of the tool is warranted.
KEY MESSAGES
What Is Already Known on This Topic
The literature does not provide guidance with respect to identifying criteria that should be used when considering a paediatric patient's readiness for discharge from CPT after upper-abdominal, thoracic, or cardiac surgery. A preliminary postoperative discharge scoring tool (the POP-DST) has been developed for the adult population; this tool was developed for use in an adult acute care population—specifically for patients following thoracic, cardiovascular, or upper-abdominal surgery. Although children have the potential to develop similar postoperative complications as adults and the biological rationale for perioperative CPT in paediatrics is similar to that in adults, this does not mean that an adult tool can automatically be applied to a paediatric population. The discharge criteria for children may be different from those for adults.
What This Study Adds
This research has identified six clinical phenomena or items that should be considered by physiotherapists when determining a paediatric patient's readiness for discharge from CPT after upper-abdominal, cardiac, or thoracic surgery. The study also provides the foundation for ongoing research to determine the reliability and predictive validity of the paediatric CPT discharge tool.
Biography
Cindy Ellerton was supported in part through a studentship by the Ontario Student Opportunity Trust Fund–Hospital for Sick Children Foundation Student Scholarship Program. Funding for this study was provided by the Ontario Lung Association through an Ontario Respiratory Care Society Fellowship Award.
APPENDIX 1
Instructions for the Draft of the Paediatric Cardiopulmonary Physiotherapy Discharge Tool
This is a draft of a paediatric cardiopulmonary physiotherapy discharge tool. The tool seeks to measure a child's readiness for discharge from inpatient cardiopulmonary physiotherapy after cardiac, thoracic or upper abdominal surgery. The tool is intended for use by paediatric physiotherapists in order to determine if post-operative patients are ready to be discharged from cardiopulmonary physiotherapy. The draft of the discharge tool includes 6 clinical phenomenon/items and their definitions. Physiotherapists should use the tool with children aged 2 to under 19 years who receive at least one day of CPT during an inpatient admission after thoracic, cardiac, or upper abdominal surgery (i.e., patient receives at least one day of cardiopulmonary physiotherapy treatment—manual techniques, mobilization, deep breathing exercises, education etc. … not just assessment). Physiotherapists should NOT use the tool with children aged 0 to 23 months, children who are in the intensive care unit, those that are mechanically ventilated, children who receive daily CPT as part of their normal routine even prior to their admission for surgery (e.g., cystic fibrosis), and children who present with acute musculoskeletal or neurological conditions that would impact their ability to mobilize independently. The tool can however, be used with children with chronic, but stable, neurological or orthopaedic conditions. The tool should be completed after a routine physiotherapy clinical assessment of a patient who is post-operative from cardiac, thoracic, or upper abdominal surgery is performed. The definitions for each of the items should be considered and a determination should be made if the patient meets the requirements of the definition. If the patient meets the criterion definition of a particular item, place an “X” in the “yes” box. If the patient does NOT meet the criterion definition for a particular item, place an “X” in the “no” box. It is important that an answer for each clinical phenomenon/item is recorded.
Draft of the Paediatric Cardiopulmonary Physiotherapy Discharge Tool
Auscultation
-
□
The patient demonstrates breath sounds that are within normal given age/size/pathology with no adventitia present.
-
□
The patient demonstrates breath sounds and/or adventitia consistent with pre-morbid status if known.
Patient does not meet either of the above criteria for auscultation. □
Signs of Respiratory Distress
-
□
The patient is not showing any signs of respiratory distress including but not limited to: increased respiratory rate, nasal flaring, tracheal tugging, subcostal/intercostal indrawing, or accessory muscle use.
-
□
The patient has returned to pre-morbid status if known.
Patient does not meet either of the above criteria for signs of distress. □
Oxygen Saturation
-
□
Patient is able to maintain SpO2≥93% on room air or baseline FiO2 at rest and during activity.
-
□
Patient is able to maintain pre-morbid SpO2 (if known) on room air, or baseline FiO2 at rest and during activity.
Patient does not meet either of the above criteria for oxygen saturation. □
Secretion Clearance
-
□
No secretions are present.
-
□
The patient is able to clear secretions independently with effective cough, mobilization, or prescribed breathing exercises.
-
□
The patient is able to clear secretions with the assistance of family/caregiver (including suctioning).
-
□
The patient has returned to pre-operative/baseline status where family/caregiver assistance or suctioning may have been required.
Patient does not meet any of the above criteria for secretion clearance. □
Mobility
-
□
Patient is able to mobilize independently (including bed mobility, transfers and ambulation).
-
□
The patient is able to mobilize with minimal assistance of family/caregiver (including bed mobility, transfers and ambulation).
-
□
The patient is able to move within expected parameters for their age group or has returned to pre-morbid status.
Patient does not meet any of the above criteria for mobility. □
Discharge Planning
-
□
Patient and family have received necessary information/education and appropriate follow-up services and equipment related to physiotherapy care have been arranged if required.
Patient does not meet the above criterion for discharge planning. □
Ellerton C, Davis A, Brooks D. Preliminary development and validation of a paediatric cardiopulmonary physiotherapy discharge tool. Physiother Can. 2010;preprint. doi: 10.3138/ptc.2009-30
References
- 1.Brooks D, Parsons J, Newton J, Dear C, Silaj E, Sinclair L, et al. Discharge criteria from peri-operative physical therapy. Chest. 2002;121:488–94. doi: 10.1378/chest.121.2.488. [DOI] [PubMed] [Google Scholar]
- 2.Wallis C, Prasad A. Who needs chest physiotherapy? moving from anecdote to evidence. Arch Dis Child. 1999;80:393–7. doi: 10.1136/adc.80.4.393. doi: 10.1136/adc.80.4.393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Zach MS, Oberwaldner B. Paediatric respiratory medicine. St. Louis: Mosby; 1999. [Google Scholar]
- 4.Roberts-Davis M, Read S. Clinical role clarification: using the Delphi method to establish similarities and differences between nurse practitioners and clinical nurse specialists. J Clin Nurs. 2001;10:33–43. doi: 10.1046/j.1365-2702.2001.00437.x. doi: 10.1046/j.1365-2702.2001.00437.x. [DOI] [PubMed] [Google Scholar]
- 5.Dalkey NC. The Delphi method: an experimental study of group opinion. Santa Monica, CA: RAND Corp.; 1969. [Google Scholar]
- 6.Hasson F, Keeney S, McKenna H. Research guidelines for the Delphi survey technique. J Adv Nurs. 2000;32:1008–15. doi: 10.1046/j.1365-2648.2000.01567.x. [PubMed] [Google Scholar]
- 7.Green B, Jones M, Hughes D, Williams A. Applying the Delphi technique in a study of GPs' information requirements. Health Soc Care Comm. 1999;7:198–205. doi: 10.1046/j.1365-2524.1999.00176.x. [DOI] [PubMed] [Google Scholar]
- 8.Loughlin K, Moore L. Using Delphi to achieve congruent objectives and activities in a pediatrics department. J Med Educ. 1979;54:101–6. doi: 10.1097/00001888-197902000-00006. doi: 10.1097/00001888-197902000-00006. [DOI] [PubMed] [Google Scholar]
- 9.McKenna HP. The Delphi technique: a worthwhile research approach for nursing? J Adv Nurs. 1994;19:1221–5. doi: 10.1111/j.1365-2648.1994.tb01207.x. doi: 10.1111/j.1365-2648.1994.tb01207.x. [DOI] [PubMed] [Google Scholar]
- 10.Sumsion T. The Delphi technique: an adaptive research tool. Brit J Occup Ther. 1998;61:153–6. [Google Scholar]
- 11.Feinstein AR. Clinimetrics. New Haven, CT: Yale University Press; 1987. [Google Scholar]
- 12.Feinstein AR. Clinical judgement revisited: the distraction of quantitative methods. Ann Intern Med. 1994;120:799–805. doi: 10.7326/0003-4819-120-9-199405010-00012. [DOI] [PubMed] [Google Scholar]
- 13.Rowe BH, Oxman AD. An assessment of the sensibility of a quality-of-life instrument. Am J Emerg Med. 1993;11:374–80. doi: 10.1016/0735-6757(93)90171-7. doi: 10.1016/0735-6757(93)90171-7. [DOI] [PubMed] [Google Scholar]