ABSTRACT
Purpose: The purpose of this systematic review was to evaluate the current evidence base for whole-body vibration as a treatment for low back pain (LBP).
Summary of key points: Whole-body vibration through occupational exposure has previously been recognized as an aetiological factor in LBP. Previous studies have identified whole-body vibration (WBV) as a cause of LBP in various sitting-based occupations that involve machinery and repetitive vibration. In the last decade, however, WBV has been advocated as a safe and effective treatment for LBP. Despite the growing popularity of WBV in clinical practice, this systematic review of the literature identified only two studies that investigated the effectiveness of WBV as a treatment option for LBP, and an assessment of the quality of these studies demonstrated several methodological problems that may have biased their findings. While there is emerging evidence for the effectiveness of WBV in treating some medical conditions, the evidence for WBV as a treatment for LBP remains equivocal.
Recommendations: Based on the current body of evidence, routine use of WBV to treat LBP should be undertaken with caution. Further rigorous research designed to investigate the effectiveness of WBV as a safe and high-quality treatment for LBP is required.
Key Words: evidence-based practice, low back pain, systematic review, whole-body vibration
RÉSUMÉ
Objectif : L'objectif de cette revue systématique était d'évaluer l'ensemble des preuves cliniques à l'appui du recours aux vibrations du corps entier pour le traitement des lombalgies.
Résumé des principaux points : Les vibrations du corps entier dans le cadre d'activités professionnelles ont déjà été reconnues comme facteur étiologique de la lombalgie. Des études déjà réalisées ont reconnu ces vibrations comme causes de lombalgie dans diverses activités professionnelles effectuées principalement en position assise, où il y a présence de machinerie et de vibrations répétitives. Toutefois, au cours de la dernière décennie, des pressions ont été exercées afin que les vibrations du corps entier soient considérées comme un traitement sûr et efficace de la lombalgie. Malgré la popularité croissante des vibrations du corps entier dans la pratique clinique, cette revue systématique de la documentation n'a permis de répertorier que deux études qui se sont penchées sur l'efficacité de ce traitement pour la lombalgie. Une évaluation de la qualité de ces études a révélé plusieurs problèmes de méthodologie qui en ont biaisé les résultats. Même si des faits cliniques émergents témoignent de plus en plus de l'efficacité des vibrations du corps entier pour le traitement de certains problèmes de santé, les preuves relatives à cette méthode pour le traitement des lombalgies n'apparaissent pas concluantes.
Recommandations : En fonction des faits cliniques actuels, l'utilisation régulière des vibrations du corps entier pour le traitement de la lombalgie doit être envisagée avec prudence. Des recherches plus rigoureuses dont l'objectif sera d'analyser l'efficacité de cette méthode en tant que traitement sûr et de qualité pour la lombalgie sont donc nécessaires.
Mots clés : lombalgie, pratique fondée sur l'expérience clinique, revue systématique, vibrations du corps entier
INTRODUCTION
At certain frequencies, whole-body vibration (WBV) is considered an aetiological factor for low back pain (LBP).1 Previous systematic reviews have demonstrated an association between WBV and LBP, primarily via occupational exposure.1–3 It has been proposed that fatigue of spinal stabilizing muscles may be a part of the aetiology and that other factors such as prolonged sitting combined with WBV may also contribute to the development of LBP.1,2
As a treatment technique, WBV was first introduced to clinical practice to increase bone-mineral density in people with osteoporosis.4 WBV typically involves standing and holding positions or performing exercises on a vibrating platform at a predetermined amplitude, frequency, and magnitude of oscillation.5 The use of WBV has since expanded to include improving strength and muscle activation in less active populations, such as the elderly and people recovering from stroke.3 In addition, there is evidence that WBV may be an effective adjunct to traditional strength training in both athletic and clinical populations.6,7 WBV has been demonstrated to reduce pain and fatigue levels in women with fibromyalgia syndrome and to improve postural control and mobility in people with multiple sclerosis.8,9 The use of WBV with Parkinson disease has also been evaluated, and some positive effects on gait and balance have been found.10,11
Even though WBV is an established aetiological factor for LBP, it is currently being marketed as a treatment technique for LBP.12–16 Two mechanisms for the reduction of pain have been suggested. First, LBP is known to be associated with reduced abdominal and back extensor stabilization muscle activity;17–19 it has been proposed that WBV may assist in reducing LBP by activating stretch reflexes and subsequently activating and strengthening the abdominal and back extensor muscles.20 Second, LBP is known to be associated with paravertebral muscle spasm, and it has been suggested that WBV at frequencies below 20 Hz may reduce LBP by inducing muscle relaxation.21–22
If WBV were demonstrated to be a safe and effective treatment for LBP, it could be used as an adjunctive treatment for patients who cannot participate in traditional exercise programmes. However, before WBV is adopted into clinical practice, it is important to establish its current evidence base. The aim of this systematic review is to evaluate and summarize the current available evidence for the effectiveness of WBV in treating LBP.
METHODS
Search Strategy
The Medline, CINAHL, AMED, Scopus, PEDro, and Cochrane Library databases were searched in September 2009, using the keywords whole body vibration, low back pain, treatment, intervention, and rehabilitation with appropriate truncations. No restriction was placed on the search in terms of research design, year of publication, or language. Observational studies were excluded, as they reported on the occurrence or prevalence of LBP due to exposure to WBV. Similarly, studies that did not focus on WBV as an intervention were also excluded.
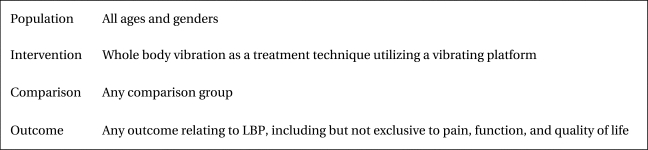
The population, intervention, comparison, and outcome (PICO) system was used to establish the suitability of studies for inclusion in this review.23 The PICO system provides a logical framework for organizing literature and framing a research question. The PICO criteria used in this review were broad, in order to account for the diverse populations affected by LBP and the range of outcome measures used to quantify LBP symptoms (see Figure 1).
Figure 1.
PICO (population, intervention, comparison, and outcome) criteria
Methodological Quality
The methodological quality of studies was appraised using the Physiotherapy Evidence Database (PEDro) scale, which consists of 10 criteria that assess internal validity. A single point was allocated for each criterion fulfilled. The first question on the PEDro scale addresses external validity and is not included in the overall PEDro score.24 The PEDro scale was chosen because it has demonstrated fair to good reliability in assessing the quality of randomized controlled trials;25 in addition, it includes three criteria that are recognized markers of internal validity: concealment of allocation, blinding of assessors, and loss of participants at follow-up.25 Two authors (LP, ZM) independently appraised the studies; any discrepancies were resolved by discussion with the third author (SK).
Data Extraction and Analysis
Data (population, intervention, comparison groups, outcome measures, and study outcomes) were extracted and analyzed by two authors (ZM, LP). WBV settings (type, magnitude, and frequency of vibration in Hertz) were extracted. The parameters of any exercise performed in conjunction with WBV (type, frequency, and duration) were also recorded. Clinical significance was established by calculating estimates of effect sizes. Statistical significance was established by reporting between-group p-values (p<0.05). Because of heterogeneity in interventions and outcome measures, a narrative review rather than a meta-analysis was performed.
RESULTS
Characteristics of Studies
This systematic review identified three randomized controlled trials, published between 2002 and 2005, conducted with different populations, intervention protocols, and control groups.20,26,27 One study involved healthy volunteers who participated in only one treatment session.26 Although this study did not evaluate the direct treatment of LBP, a clear relationship between reduced lumbrosacral proprioception and LBP in individuals with segmental lumbar instability has been established in the literature.28 Therefore, as this study informs the evidence base for WBV, its outcomes were considered relevant to this review.26 The remaining two studies involved populations with chronic LBP who participated in longer programmes. No adverse events from WBV were reported in either study. There was a great deal of variability in subject selection criteria and age of participants among the included trials. All three studies used control groups that did not involve WBV; only one study, however, used a control group that performed comparable exercises to the intervention but without WBV.26 Characteristics of the studies and details of WBV interventions are outlined in Tables 1 and 2.
Table 1.
Characteristics of Included Studies
| Study | Population | Exclusion Criteria | Comparison | Quality Score (PEDro) |
|---|---|---|---|---|
| Fontana (2005)26 |
Healthy men/women (n=25) Age: 19–21 yrs |
Pregnancy Acute thrombosis Cardiovascular conditions Open wound Joint replacement Prosthesis Spinal pathology Diabetes Epilepsy Acute migraine Acute inflammation Pacemaker Tumour |
Static semi-squat position, no vibration |
6/10 |
| Iwamoto (2005)27 |
Osteoporotic women with chronic LBP (n=50) Age: 55–88 yrs |
Knee osteoarthritis Degenerative thoracic or lumbar conditions LBP not related to osteoporosis Total knee/hip arthroplasty |
Medication only (Alendronate) |
6/10 |
| Rittweger (2002)20 | Men and women with chronic LBP (n=60) Age: 40–60 yrs |
Vertebral osteoporosis Spinal tumour Acute disc dysfunction Recent spinal fracture Acute inflammation Cauda equina syndrome Progressive neurological conditions Rheumatoid arthritis Bone-related diseases Heart failure Recent abdominal surgery Hip/knee replacement or prosthesis Aortic aneurysm Recent thrombosis Arterial disease Pregnancy |
Lumbar extension exercises, sit-ups, and leg presses |
3/10 |
LBP=low back pain
Table 2.
Interventions and Low Back Pain–Related Outcomes
| Study | Details of Intervention | Outcome: Measurement Tool | Statistical significance (between groups) |
Clinical significance (effect size) |
|---|---|---|---|---|
| Fontana (2005)26 |
WBV: 18 Hz,10 mm alternate oscillation Exercise: Static semi-squat position Co-interventions: None Duration: 5 min Programme: Single session |
Lumbopelvic proprioception Repositioning error (degrees); electro-magnetic goniometryR |
p>0.05 |
NR |
| Iwamoto (2005)27 |
WBV: 20 Hz, 0.7–4.2 mm alternate oscillation Exercise: Static semi-squat position Co-interventions: Medication (alendronate) Duration: 4 min Frequency: 1×/week Programme: 12 months |
Pain: Self-reported ordinal scale (0–10)R,V | p<0.05 | 0.45 |
| Lumbar bone-mineral density: DEXA scanR,V |
p > 0.05 |
0.009 |
||
| Rittweger (2002)20 |
WBV: 18 Hz, up to 6 mm alternate oscillation Exercise: Slow semi-squat movements Co-interventions: None Duration: 4 min, progress to 7 min Frequency: 2×/week (weeks 1–6), 1×/week (weeks 6–12) Programme: 12 weeks |
Pain: Visual analogue scaleR,V |
p>0.05 |
0.2 |
| Pain-related limitation: Pain disability indexR,V | p>0.05 | 0.07 | ||
| Isometric lumbar extension strength: LE Mark1 lumbar extension machine |
p<0.05 favouring control group |
−0.39 | ||
| Lumbar ROM: LE Mark1 lumbar extension machine | p>0.05 | NR | ||
| Depression: ADSR,V | p>0.05 | 0.19 |
WBV=whole-body vibration; Hz=hertz; DEXA=dual-energy X-ray absorptiometry; ROM=range of motion; ADS=Allgemeine Depressions Skala (German-language depression scale); NR=not reported
R provided evidence of reliability of outcome measure
V provided evidence of validity of outcome measure
Methodological Quality
Several significant concerns relating to the methodological quality of the included studies were noted. Subject and therapist blinding were impossible to achieve for pragmatic reasons; in addition, however, none of the studies reported blinding of outcome assessors. Further, only one study reported concealing the allocation of groups.26 In one study, more than 15% of participants dropped out during the intervention phase, yet an intention-to-treat analysis was not undertaken.20 In two of the three trials, intervention and control groups were not similar at baseline in terms of key prognostic variables.20,26 The individual PEDro criterion scores for each included study are presented in Table 3.
Table 3.
PEDro Scores
| Study | PEDro Criteria | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | Total | |
| Fontana (2005)26 | N/A | 1 | 1 | 0 | 0 | 0 | 0 | 1 | 1 | 1 | 1 | 6 |
| Iwamoto (2005)27 | N/A | 1 | 0 | 1 | 0 | 0 | 0 | 1 | 1 | 1 | 1 | 6 |
| Rittweger (2002)20 | N/A | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 1 | 3 |
N/A=not applicable (see Methods)
Whole-Body Vibration as a Treatment for Low Back Pain
Fontana et al. reported statistically significant within-group changes in lumbopelvic proprioception in a group assigned to a single session of WBV.26 However, they did not report a significant difference between the intervention group (WBV and holding semi-squat position) and the control group (holding semi-squat position without WBV). Insufficient data were provided to allow measures of clinical significance (effect size, confidence interval) to be calculated (see Table 2).
Iwamoto et al. evaluated the effect of a 12-month course of weekly WBV on lumbar BMD and LBP in women with osteoporosis.27 A significant difference in pain levels was reported between the intervention group (WBV and medication) and the control group (medication only) at 12-month follow-up. No significant between-group differences in lumbar BMD were reported. A moderate effect size of 0.45 (self-reported pain score) indicates that the effect of a combination of WBV and medication in specific osteoporotic populations may be clinically as well as statistically significant (see Table 2).
Rittweger et al. evaluated the effect of a 12-week course of once- to twice-weekly WBV in a chronic LBP population compared to a programme of lumbar extension exercises, sit-ups, and leg presses.20 This trial reported statistically significant within-group changes in self-reported pain and disability following a WBV intervention. However, no statistically significant between-group changes for pain- or disability-related outcomes were reported, and effect sizes were small and clinically insignificant. Significant between-group differences were reported in lumbar extension torque (strength) in favour of the control group (see Table 2). These findings do not demonstrate that WBV is any more effective than lumbar extension exercises in this population.
DISCUSSION
The importance of informing clinical practice with research evidence has been recognized in many health care settings throughout the world.29 Underpinning this requirement is the growing call for evidence-based practice to be integral to physiotherapy service delivery. Evidence-based practice involves integrating the best available research evidence, patient values, and individual clinical expertise.29 WBV as a treatment for musculoskeletal disorders has undergone an evolution from an adjunctive treatment for osteoporosis, to a strengthening technique for specific population groups, to its current use in treating LBP.3,4 Increasingly, WBV is being used both as an adjunctive treatment and as a stand-alone treatment for LBP.20,27
The findings of this systematic review indicate that the body of research supporting WBV as a viable treatment option for LBP is, at best, limited. The current body of evidence consists of three studies, one of which assesses the effectiveness of WBV for LBP only indirectly, by assessing lumbrosacral proprioception.26 Only one of the three studies found a significant between-group difference in favour of WBV, and this study used a specific population of osteoporotic women with LBP.27 Despite the paucity of the evidence and its questionable methodological quality, however, WBV is currently being used and is widely promoted in clinical practice to treat LBP, both as an adjunctive and as a stand-alone treatment.16
Limitations
Despite our best efforts, this systematic review is constrained by the limited number and poor methodological quality of the included studies. Lack of concealed allocation and appropriate blinding and high dropout rates were potential sources of bias identified in these studies. These limitations mean that key recommendations to support WBV for LBP in routine physiotherapy clinical practice cannot be made. The findings of this review suggest that there is no evidence for optimal treatment parameters for WBV (e.g., frequency, amplitude, duration, intensity, and duration of treatment). There is also a paucity of evidence relating to the cost-effectiveness, potential for harm, and long-term effectiveness of WBV. Thus, there are currently significant gaps in the literature on the overall effectiveness of WBV and the optimal method of operationalizing WBV as a safe and effective treatment for LBP.
Implications for Future Research
Further research is needed to investigate the effectiveness of WBV in specific populations with LBP. Well-designed randomized controlled trials that clearly define their population and specify the dosage parameters of WBV will assist practitioners in making evidence-based decisions about the use of WBV in clinical practice. Randomized controlled trials are time and resource intensive, however, and it is likely that, at least in the short term, the paucity of research evidence may persist. Therefore, well-designed case reports or case series might also assist in improving the evidence base on WBV for LBP. In addition, such case series may provide opportunities to validate optimal dosages for WBV in treating LBP.
CONCLUSIONS
Currently there is limited evidence to support the use of WBV to treat LBP. Physiotherapists using WBV as a treatment modality for LBP need to be aware of this limited evidence base. Routine use of WBV in clinical practice should be carefully monitored and informed by patient outcomes. It is important that ongoing, high-quality research be conducted to determine the effectiveness of WBV for LBP, including parameters for its optimal use in clinical practice. In the interim, as a stopgap measure, clinicians and consumers may benefit from well-designed case reports or case series, which are time and resource efficient. These case studies, in association with clinical expertise, can contribute to an emerging body of evidence for WBV. At present, given equivocal findings derived from a limited body of evidence, the use of WBV as a treatment modality for LBP should be undertaken with caution.
KEY MESSAGES
What Is Already Known on This Topic
Whole-body vibration (WBV) at certain frequencies is an established risk factor for low back pain (LBP). WBV is also a popular and increasingly easily accessible treatment for a variety of conditions, including LBP.
What This Study Adds
This systematic review provides a summary and analysis of the current evidence for WBV as a specific treatment for LBP. Although WBV is potentially useful in treating LBP, current research to support its use in clinical practice is limited and of poor quality. This systematic review highlights current evidence gaps and underscores the importance of conducting further research on this topic. Based on our results, WBV as a treatment for LBP should be used with caution.
Perraton L, Machotka Z, Kumar S. Whole-body vibration to treat low back pain: fact or fad? Physiother Can. 2010:preprint. doi:10.3138/ptc.2009.44
REFERENCES
- 1.Pope MH, Wilder DG, Magnusson ML. A review of studies on seated whole body vibration and low back pain. Proc IME H J Eng Med. 1999;213:435–46. doi: 10.1243/0954411991535040. doi: 10.1243/0954411991535040. [DOI] [PubMed] [Google Scholar]
- 2.Lings S, Leboeuf-Yde C. Whole-body vibration and low back pain: a systematic, critical review of the epidemiological literature 1992–1999. Int Arch Occup Environ Health. 2000;73:290–7. doi: 10.1007/s004200000118. doi: 10.1007/s004200000118. [DOI] [PubMed] [Google Scholar]
- 3.Cardinale M, Wakeling J. Whole body vibration exercise: are vibrations good for you? Brit J Sport Med. 2005;39:585–9. doi: 10.1136/bjsm.2005.016857. doi: 10.1136/bjsm.2005.016857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Rubin C, Pope M, Fritton C, Magnusson M, Hansson T, McLeod K. Transmissibility of 15-hertz to 35-hertz vibrations to the human hip and lumbar spine: determining the physiologic feasibility of delivering low-level anabolic mechanical stimuli to skeletal regions at greatest risk of fracture because of osteoporosis. Spine. 2003;28:2621–7. doi: 10.1097/01.BRS.0000102682.61791.C9. doi: 10.1097/01.BRS.0000102682.61791.C9. [DOI] [PubMed] [Google Scholar]
- 5.Cardinale M, Bosco C. The use of vibration as an exercise intervention. Exerc Sport Sci Rev. 2003;31:3–7. doi: 10.1097/00003677-200301000-00002. doi: 10.1097/00003677-200301000-00002. [DOI] [PubMed] [Google Scholar]
- 6.Luo J, McNamara B, Moran K. The use of vibration training to enhance muscle strength and power. Sport Med. 2005;35(1):23–41. doi: 10.2165/00007256-200535010-00003. doi: 10.2165/00007256-200535010-00003. [DOI] [PubMed] [Google Scholar]
- 7.Trans T, Aaboe J, Henriksen M, Christensen R, Bliddal H, Lund H. Effect of whole body vibration exercise on muscle strength and proprioception in females with knee osteoarthritis. Knee. 2009;16:256–61. doi: 10.1016/j.knee.2008.11.014. doi: 10.1016/j.knee.2008.11.014. [DOI] [PubMed] [Google Scholar]
- 8.Alentorn-Geli E, Padilla J, Moras G, Lázaro Haro C, Fernández-Solà J. Six weeks of whole-body vibration exercise improves pain and fatigue in women with fibromyalgia. J Altern Complement Med. 2008;14:975–81. doi: 10.1089/acm.2008.0050. doi: 10.1089/acm.2008.0050. [DOI] [PubMed] [Google Scholar]
- 9.Schuhfried O, Mittermaier C, Jovanovic T, Pieber K, Paternostro-Sluga T. Effects of whole-body vibration in patients with multiple sclerosis: a pilot study. Clin Rehab. 2005;19:834–42. doi: 10.1191/0269215505cr919oa. doi: 10.1191/0269215505cr919oa. [DOI] [PubMed] [Google Scholar]
- 10.Ebersbach G, Edler D, Kaufhold O, Wissel J. Whole body vibration versus conventional physiotherapy to improve balance and gait in Parkinson's disease. Arch Phys Med Rehabil. 2008;89:399–403. doi: 10.1016/j.apmr.2007.09.031. doi: 10.1016/j.apmr.2007.09.031. [DOI] [PubMed] [Google Scholar]
- 11.Turbanski S, Haas C, Schmidtbleicher D. Effects of random whole body vibration on postural control in Parkinsons disease. Res Sport Med. 2005;13:243–56. doi: 10.1080/15438620500222588. doi: 10.1080/15438620500222588. [DOI] [PubMed] [Google Scholar]
- 12.Galileo Whole Body Vibration. Benefits; [1 screen] [Internet] Hornsby Heights, Australia: Galileo Whole Body Vibration; c2008. [updated 2008 Nov 3; cited 2002 Oct 28]. Available from: http://www.galileowholebodyvibration.com.au/benefits.html. [Google Scholar]
- 13.Fit2gether. Vibrogym training; [about 15 screens]. [Internet] Glasgow, UK: Fit2gether; c2005–2010. [cited 2010 Jan 7]. Available from: http://www.fit2gether.co.uk/vibrogymtraining.html. [Google Scholar]
- 14.Victoria Physiotherapy Group. Galileo; [about 2 screens] [Internet] Perth, Australia: The Group; c2006. [cited 2010 Jan 7]. Available from: http://www.vicphysiogroup.com.au/pages/galileo.php. [Google Scholar]
- 15.Vibraflex.com [Internet] Florida: Vibraflex; c2006. [cited 2010 Jan 7]. Available from: http://www.vibraflex.com/ [Google Scholar]
- 16.Back in Motion Health Group. Whole body vibration; [about 3 screens] [Internet] Mulgrave, Australia: The Group; c2010. [cited 2010 Jan 15]. Available from: http://www.backinmotion.com.au/whole-body-vibration.php. [Google Scholar]
- 17.Hodges P, Richardson C. Inefficient muscular stabilization of the lumbar spine associated with low back pain: a motor control evaluation of transversus abdominis. Spine. 1996;21:2640–50. doi: 10.1097/00007632-199611150-00014. [DOI] [PubMed] [Google Scholar]
- 18.Hodges P, Richardson C. Altered trunk muscle recruitment in people with low back pain with upper limb movement at different speeds. Arch Phys Med Rehabil. 1999;80:1005–12. doi: 10.1016/s0003-9993(99)90052-7. doi: 10.1016/S0003-9993(99)90052-7. [DOI] [PubMed] [Google Scholar]
- 19.Hodges P. Changes in motor planning of feedforward postural responses of the trunk muscles in low back pain. Exp Brain Res. 2001;141:261–6. doi: 10.1007/s002210100873. doi: 10.1007/s002210100873. [DOI] [PubMed] [Google Scholar]
- 20.Rittweger J, Just K, Kautzsch K, Reeg P, Felsenberg D. Treatment of chronic lower back pain with lumbar extension and whole-body vibration exercise: a randomized controlled trial. Spine. 2003;27:1829–34. doi: 10.1097/00007632-200209010-00003. [DOI] [PubMed] [Google Scholar]
- 21.Fischer A, Chang C. Electromyographic evidence of paraspinal muscle spasm during sleep in patients with low back pain. Clin J Pain. 1985;1(3):147–54. doi: 10.1097/00002508-198501030-00004. [Google Scholar]
- 22.Rittweger J, Mutschelknauss M, Felsenberg D. Acute changes in neuromuscular excitability after exhaustive whole body vibration exercise as compared to exhaustion by squatting exercise. Clin Physiol Funct Imaging. 2003;23:81–6. doi: 10.1046/j.1475-097x.2003.00473.x. doi: 10.1046/j.1475-097X.2003.00473.x. [DOI] [PubMed] [Google Scholar]
- 23.Lacasse M, Lafortune V, Bartlett L, Guimond J. Answering clinical questions: what is the best way to search the Web? Can Fam Physician. 2007;53:1535–6. [PMC free article] [PubMed] [Google Scholar]
- 24.Maher CG, Sherrington C, Herbert RD, Moseley AM, Elkins M. Reliability of the PEDro scale for rating quality of randomized controlled trials. Phys Ther. 2003;83:713–21. [PubMed] [Google Scholar]
- 25.Moher D, Cook DJ, Jadad AR, Tugwell P, Moher M, Jones A, et al. Assessing the quality of reports of randomised trials: implications for the conduct of meta-analyses. Health Technol Assess. 1999;3(12):1–98. doi: 10.3310/hta3120. [PubMed] [Google Scholar]
- 26.Fontana TL, Richardson CA, Stanton WR. The effect of weightbearing exercise with low frequency, whole body vibration on lumbosacral proprioception: a pilot study on normal subjects. Aust J Physiother. 2005;51:259–63. doi: 10.1016/s0004-9514(05)70007-6. [DOI] [PubMed] [Google Scholar]
- 27.Iwamoto J, Takeda T, Sata Y, Uzawa M. Effect of whole-body vibration exercise on lumbar bone mineral density, bone turnover and chronic back pain in post-menopausal osteoporotic women treated with alendronate. Aging Clin Exp Res. 2005;17(2):157–63. doi: 10.1007/BF03324589. [DOI] [PubMed] [Google Scholar]
- 28.O'Sullivan P, Burnett A, Floyd A, Gadsdon K, Logiudice J, Miller D, et al. Lumbar repositioning deficit in a specific low back pain population. Spine. 2003;28:1074–9. doi: 10.1097/01.BRS.0000061990.56113.6F. [DOI] [PubMed] [Google Scholar]
- 29.Sackett D, Rosenberg W, Gray J, Haynes R, Richardson R. Evidence based medicine: what it is and what it isn't. Brit Med J. 1996;312:71–2. doi: 10.1136/bmj.312.7023.71. [DOI] [PMC free article] [PubMed] [Google Scholar]