ABSTRACT
Purpose: To compare the original and reduced versions of the Berg Balance Scale (BBS) and the Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC), as completed by patients following total hip arthroplasty (THA) or total knee arthroplasty (TKA), with respect to their potential utility in clinical and research settings.
Method: Patients with THA (n=26) or TKA (n=28) were evaluated before and after 5 to 7 weeks' participation in a home-based exercise programme. They were assessed using the original versions of the BBS and the WOMAC; scores for the reduced versions of the BBS and the WOMAC were extracted from the original versions.
Results: Good to excellent correlations (r≥0.80) were observed between the original and the reduced versions of the BBS and the WOMAC. The index of responsiveness, evaluated using standardized response means (SRM), was similar for the original and the reduced versions of the BBS and the WOMAC function sub-scale.
Conclusions: The reduced versions of the BBS and the WOMAC provided similar information to the original versions and were equally responsive. These reduced versions comprise fewer questions and may be completed in considerably less time, which suggests that they may be advantageous for clinical and research use.
Key Words: Berg Balance Scale, total hip arthroplasty, total knee arthroplasty, Western Ontario and McMacter Universities Osteoarthritis Index
RÉSUMÉ
Objectif : Comparer les tests réalisés à l'aide des versions originale et abrégée de l'échelle d'équilibre de Berg (EEB) et de l'indice d'évaluation de l'arthrose WOMAC des Universités Western Ontario et McMaster chez les patients à la suite d'une arthroplastie totale de la hanche ou une arthroplastie totale du genou, en ce qui a trait à leur utilité possible dans les cadres clinique et de la recherche.
Méthode : Les patients ayant subi une arthroplastie totale de la hanche (n=26) ou une arthroplastie totale du genou (n=28) ont été évalués après 5 à 7 semaines de participation à un programme d'exercices à domicile. Pour cette évaluation, on a utilisé les versions originales de l'EEB et du WOMAC. Les pointages pour les versions abrégées de l'EEB et du WOMAC ont été obtenus à partir des résultats des tests avec les échelles originales.
Résultats : Des corrélations variant de bonnes à excellentes (r≥0,80) ont été observées entre les versions originales et abrégées de l'EEB et du WOMAC. L'indice de réactivité, évalué à l'aide de moyens de réponse normalisés (standardized response means, ou SRM), était similaire pour les versions originales et abrégées de l'EEB et de la sous-échelle de fonction du WOMAC.
Conclusions : Les versions abrégées de l'EEB et du WOMAC ont fourni de l'information similaire à leurs versions originales et étaient tout aussi pertinentes. Les versions abrégées comportaient moins de questions et pouvaient être remplies en beaucoup moins de temps. Cela semble indiquer que les versions abrégées pourraient être plus avantageuses pour une utilisation clinique ou à des fins de recherche.
Mots clés : arthroplastie totale de la hanche, arthroplastie totale du genou, échelle d'équilibre de Berg, indice d'arthrose des Universités Western Ontario et McMaster
INTRODUCTION
Lengthy outcome measures place a burden on respondents assessed for their health status, as well as on practitioners who use them in their clinical documentation and researchers who base their studies on these measures. Lengthy tests and questionnaires can adversely affect respondents' willingness to complete them.1 Many outcome measures have been revised to offer shorter versions, in an effort to gather similar information while reducing the time and complexity of administration.2–4 The original 24-item Western Ontario and McMaster Universities (WOMAC) Osteoarthritis Index has been reduced to 12-item and 8-item WOMAC versions;5,6 similarly, the original 14-item Berg Balance Scale (BBS) has been reduced to a 7-item BBS.7
Although the original version of the WOMAC has been used extensively in research to assess patients' subjective opinions of their functional disability and is estimated to take about 5 to 10 minutes to complete,8 clinical experience suggests that in the case of elderly patients, it often takes longer to complete, and the questions may require further explanation. For practical reasons, if a condition-specific outcome measure such as the WOMAC is to be used routinely by therapists in clinical practice, it must be as short and simple as possible. For these reasons, three reduced versions of the WOMAC have recently been proposed;5,6,9 any advantages of one version over the others are unclear, however.
There are differences in both content and method of administration between the original WOMAC and BBS outcome measures. Whereas the WOMAC is a self-administered, disease-specific questionnaire used to assess the functionally oriented difficulty of patients presenting with osteoarthritis (OA) of the hip and/or knee, the BBS is a commonly used clinical performance test of balance. The original 14-item BBS has been widely used to assess balance in the elderly10 and in patients with brain injury,11 stroke,12 and Parkinson disease,13 as well as to examine the effect of exercise programmes on balance.14
Recently, Chou et al.7 proposed a 7-item version of the BBS (short BBS) and demonstrated that it provided a reliable and valid measure of postural balance in patients who had sustained a stroke.7 Another simplified version of the BBS was proposed by Wang et al,15 whose approach to simplifying the BBS was to shorten the scoring scale from five levels to three. Because this version continues to require performance of all 14 tasks of the original BBS, it is unlikely to reduce the burden on either the rater or the patient; therefore, we did not include it in our study.
Because the reduced versions of the WOMAC and the BBS were developed only recently, their measurement properties have not been examined thoroughly. Therefore, the purposes of the current study were (1) to compare the 7-item version of the BBS with the original BBS and (2) to compare the three reduced versions of the WOMAC (Hirsch-WOMAC, Whitehouse-WOMAC, and Tubach-WOMAC) with the original WOMAC with respect to concurrent validity, responsiveness, and absolute measurement error in patients with hip or knee arthroplasty. A finding that the reduced versions of these instruments demonstrate similar properties to the original versions would support their use.
METHODS
Participants
Fifty-four patients who had undergone total hip arthroplasty (THA) or total knee arthroplasty (TKA) and had participated in a related study of home exercise intervention programmes completed the original WOMAC and the BBS on two occasions: (1) 1 week after hospital discharge and at the start of a home exercise programme, and (2) 5 to 7 weeks after participation in the home exercise programme. All participants had primary unilateral THA or TKA as a result of hip- or knee-joint OA and had been advised by their surgeon to bear weight as tolerated following their surgery. Patients with revision THA or TKA and those who had been advised by their surgeon to partially or completely avoid bearing weight on either the operated or the non-operated leg were excluded. Patients with a neurological condition that might affect balance (e.g., hemiplegia, peripheral neuropathy, Parkinson disease, multiple sclerosis, or spinal-cord compression), as well as those considered unable to communicate or follow instructions in English, were also excluded from the study. Ethics approval was obtained from the University of Western Ontario Research Ethics Board for Health Sciences Research Involving Human Subjects, and all participants provided informed consent prior to participation.
Procedure
Patients were evaluated individually at their place of residence by a physical therapist within 1 week following hospital discharge. Author PJ and another physical therapist, each with 3 to 4 years' experience in working with patients with large joint arthroplasty, participated in the study. Participants were asked to complete a self-report questionnaire (the original version of the WOMAC) and were evaluated by their physical therapist using the BBS. The primary investigator (PJ) completed a follow-up assessment after 5 to 7 weeks' participation in a home exercise programme. There was no specific order in which the tests were completed; rather, the order was selected by each participant. All testing was completed during the afternoon hours.
Scores for the reduced test versions (Hirsch-WOMAC, Whitehouse-WOMAC, Tubach-WOMAC, and 7-item BBS) were calculated from their respective original versions rather than from a separate administration of these tests. Previous studies have used a similar method to generate and score items on reduced versions.5–7,9
Outcome Measures
Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC)
The original version of the WOMAC consists of 24 separate questions distributed among three sub-scales: (1) a pain sub-scale with five questions, (2) a stiffness sub-scale with two questions, and (3) a physical function sub-scale with 17 questions.8 Patients respond to the questions using five-point scales (0–4); the maximum score is 96. Higher scores on the WOMAC indicate greater pain and stiffness and greater difficulty in performing selected functional activities. The WOMAC has been demonstrated to have good reliability, validity, and responsiveness and has been used extensively by surgeons and physical therapists to assess patient status following surgical interventions16,17 and rehabilitation programmes.18,19
Hirsch-WOMAC
Hirsch et al.5 developed a reduced WOMAC, using Rasch analysis methodology, from the original WOMAC completed by patients with hip or knee complaints, including those who had undergone THA or TKA. The final Hirsch-WOMAC has eight items, three for pain and five for function (see Table 1). Items on the Hirsch-WOMAC are scored similarly to the original WOMAC items, using the five-point scale; higher scores indicate greater pain and functional difficulty. The Hirsch-WOMAC has been shown to be reliable and valid, with excellent correlations (r=0.94) between the pain and function sub-scales of the Hirsch-WOMAC and those of the original WOMAC.5
Table 1.
Summary of Questions Used in the Reduced Versions of the Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC)*
| Hirsch-WOMAC | Whitehouse-WOMAC | Tubach-WOMAC |
|---|---|---|
| Pain | Pain | |
| 1. Walking on flat surface | 1. Walking on flat surface | |
| 2. Going up or down stairs | 2. Going up or down stairs | |
| 4. Sitting or lying | 3. At night while in bed | |
| 4. Sitting or lying | ||
| 5. Standing upright | ||
| Function | Function | Function |
| 1. Descending stairs | 2. Ascending stairs | 1. Descending stairs |
| 7. Getting in/out of car | 3. Rising from sitting | 2. Ascending stairs |
| 10. Rising from bed | 6. Walking on flat | 3. Rising from sitting |
| 12. Lying on bed | 7. Getting in/out of car | 6. Walking on flat |
| 17. Light domestic duties | 9. Putting on socks/stockings | 7. Getting in/out of car |
| 10. Rising from bed | 8. Going shopping | |
| 14. Sitting | 9. Putting on socks/stockings | |
| 15. Getting on/off toilet |
Numbers refer to item numbers on the original WOMAC.
Whitehouse-WOMAC
Whitehouse et al.9 developed a reduced version of the original WOMAC using responses to the WOMAC items based on (1) function most likely to change after surgery, (2) function patients care about the most, and (3) function representative of a broad spectrum of activity levels from 36 orthopaedic and rheumatology health care professionals in the United Kingdom and the United States. While the pain sub-scale of the original WOMAC was not changed, the stiffness sub-scale was excluded from the reduced version. The Whitehouse-WOMAC thus has a total of 12 items—5 for pain and 7 for function (see Table 1)—that are scored using the five-point scoring system of the original WOMAC. The Whitehouse-WOMAC has been shown to be reliable and valid, with excellent correlations (r=0.96) between the Whitehouse-WOMAC and the original WOMAC based on total scores.
Tubach-WOMAC
Tubach et al.6 developed a reduced WOMAC from the physical function sub-scale of the original 24-question WOMAC,8 using an expert-based reduction approach. Development of the Tubach-WOMAC involved 1,362 patients and 399 rheumatologists, along with statistical analyses of item quality. A four-step procedure was followed: (1) items were ranked from highest to lowest importance according to patient and rheumatologist opinions; (2) items with a high proportion of missing data were excluded; (3) items for which distribution of answers showed floor and/or ceiling effects were excluded; and (4) where two items showed redundancy by inter-item correlation coefficients, the least important item of the pair was excluded. The Tubach-WOMAC has a total of eight function items (see Table 1), scored using the original five-point scoring system. The Tubach-WOMAC has also been demonstrated to be reliable and valid, with excellent correlations (r=0.96) between the reduced and original WOMAC function sub-scales.
Berg Balance Scale (BBS)
The original BBS consists of 14 simple functionally oriented balance tasks, which patients are asked to perform under the supervision of a therapist. These tasks are scored on five-point scales (0–4), yielding a maximum total score of 56; higher scores indicate better balance. The BBS has been reported to be a reliable and valid tool to assess balance in a variety of patient populations.10–14
Short BBS
The short BBS7 consists of seven of the original BBS tasks (see Table 2), scored with the original scale. The short BBS requires less than 10 minutes to administer, as opposed to 10–15 minutes for the full 14-item BBS. To our knowledge, only Chou et al.7 have investigated its validity and reliability; in their study, the short BBS was found to be reliable (α=0.97) and had excellent agreement with the original BBS (ICC=0.99).
Table 2.
Summary of Questions Used in the Short Version of the Berg Balance Scale (BBS)*
| Reduced version of the BBS |
|---|
| 8. Reaching forward with outstretched arm |
| 6. Standing with eyes closed |
| 13. Standing with one foot in front |
| 10. Turning to look behind |
| 9. Retrieving object from floor |
| 14. Standing on one foot |
| 1. Sitting to standing |
Numbers refer to item numbers on the original BBS.
Statistical Analyses
Scores on all outcome measures were treated as parametric data. Pearson product-moment correlation coefficients were calculated to determine the relationships among the original and reduced versions of the WOMAC and the BBS. The pain and function sub-scales of the original WOMAC, Hirsch-WOMAC, and Whitehouse-WOMAC were analyzed separately. The correlation coefficients were subjectively interpreted as follows: 0.90–1.0=excellent; 0.70–0.89=good; 0.40–0.69=modest; 0.20–0.39=low; <0.20=slight.20 The correlations and prediction bands were calculated using STATISTICA 7.0 software (StatSoft Inc., Tulsa, OK).
Responsiveness of the original and reduced versions of the WOMAC and the BBS was evaluated using the standardized response mean (SRM), an indicator of effect size whereby larger values suggest greater effect size and responsiveness. The SRM for each outcome measure was calculated based on average change in scores on two different occasions divided by the standard deviation of the change score.21,22 Subsequently, the 95% confidence intervals for the SRM were calculated using the standard error, which was approximated as 1 divided by the square root of n (sample size).23 The SRM assumes that the change within the data set was homogeneous.23 To test this assumption, a repeated-measures analysis of variance (ANOVA) considering two between-group factors (gender and joint) and one within-group factor (occasion) was carried out. A finding of insignificant between-group interactions would suggest that the change scores were homogeneous.
The absolute measurement error of an outcome measure is referred to as the precision of the outcome measure and is expressed in the units of measurement of the outcome measure.24 The standard error of measurement (SEM) is sometimes regarded as an adequate measure of absolute measurement error.24 The absolute measurement error for the outcome measures in the current study was calculated using SEM of the outcome measure divided by the scale range of the measure. Similar absolute measurement error for outcome measures indicates a similar degree of precision for the outcome measures.
RESULTS
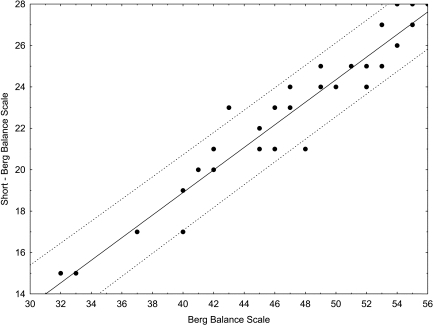
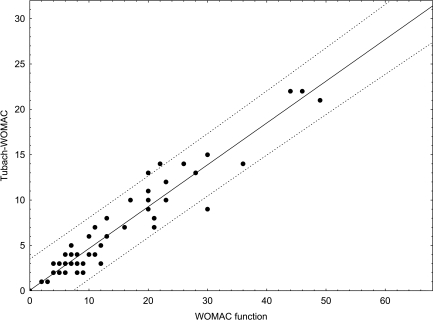
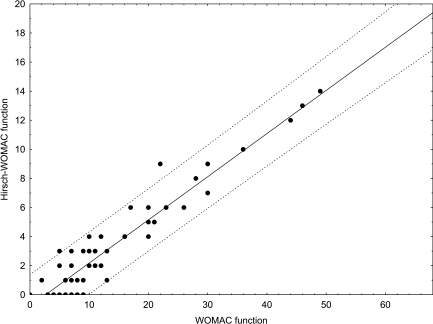
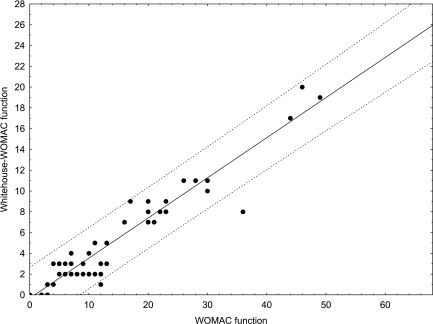
Twenty-six patients who had undergone THA (mean age: 68±8 years) and 28 patients who had undergone TKA (mean age: 64±10 years) completed the study. Scores on the original and reduced versions of the WOMAC and BBS are given in Table 3. Correlations between the pain and function sub-scales of the original WOMAC and the reduced versions of the WOMAC were good to excellent (see Table 4). Correlations between original and reduced BBS scores for occasions 1 and 2 were also good to excellent (see Table 5). The 95% prediction bands for the original and short BBS, the functional sub-scales of Hirsch-WOMAC and Whitehouse WOMAC, and the Tubach-WOMAC are shown in Figures 1–4.
Table 3.
Scores on the Original and Reduced Versions of the Berg Balance Scale (BBS) and the Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC) (n=54)
| Measure (max. score) | Occasion 1 mean±SD |
Occasion 2 mean±SD |
|---|---|---|
| BBS (56) | 34±8 | 50±6 |
| Short BBS (28) | 16±5 | 25±4 |
| WOMAC pain (20) | 8±4 | 4±4 |
| WOMAC function (68) | 36±11 | 15±11 |
| Hirsch-WOMAC pain (12) | 4±2 | 2±2 |
| Hirsch-WOMAC function (20) | 9±4 | 4±3 |
| Whitehouse-WOMAC pain (20) | 8±4 | 4±4 |
| Whitehouse-WOMAC function (28) | 13±4 | 5±5 |
| Tubach-WOMAC (32) | 16±6 | 7±5 |
Table 4.
Correlation Coefficients (95% CI) between Original and Reduced Versions of the Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC)
| WOMAC |
||||
|---|---|---|---|---|
| Occasion 1 |
Occasion 2 |
|||
| Pain | Function | Pain | Function | |
| Hirsch-WOMAC | ||||
| Pain | 0.95 (0.91, 0.97) | 0.93 (0.88, 0.96) | ||
| Function | 0.92 (0.86, 0.95) | 0.95 (0.91, 0.97) | ||
| Whitehouse-WOMAC | ||||
| Pain | 1 | 1 | ||
| Function | 0.88 (0.80, 0.93) | 0.95 (0.91, 0.97) | ||
| Tubach-WOMAC | ||||
| Function | 0.95 (0.91, 0.97) | 0.95 (0.91, 0.97) | ||
95% CI=95% confidence interval
Table 5.
Correlation Coefficients (95% CI) between Original and Reduced Versions of the Berg Balance Scale (BBS)
| BBS |
||
|---|---|---|
| Occasion 1 | Occasion 2 | |
| Short BBS | 0.92 (0.86, 0.95) | 0.97 (0.95, 0.98) |
95% CI=95% confidence interval
Figure 1.
Relationship between original and short Berg Balance Scale scores (dashed lines depict 95% prediction bands)
Figure 4.
Relationship between Western Ontario McMaster Universities Osteoarthritis Index (WOMAC) and Tubach-WOMAC function sub-scale scores (dashed lines depict 95% prediction bands)
Figure 2.
Relationship between Western Ontario McMaster Universities Osteoarthritis Index (WOMAC) and Hirsch-WOMAC function sub-scale scores (dashed lines depict 95% prediction bands)
Figure 3.
Relationship between Western Ontario McMaster Universities Osteoarthritis Index (WOMAC) and Whitehouse-WOMAC function sub-scale scores (dashed lines depict 95% prediction bands)
The assumption of homogeneous change necessary for use of the SRM analysis was satisfied by the finding of a significant effect for occasion only for both WOMAC and BBS data (BBS: F(1,50)=172.66, p<0.001; WOMAC pain: F(1,50)=56.36, p<0.001; WOMAC function: F(1,50)=143.48, p<0.001); no interaction effects were found (BBS: F(1,50)=0.92, p=0.34; WOMAC pain: F(1,50) = 1.26, p = 0.26; WOMAC function: F(1,50) = 0.69, p=0.40). SRMs for the original and reduced version of the BBS were similar and were greater than those for the original and reduced versions of the WOMAC (see Table 6). SRMs for the function sub-scales of the reduced versions of the WOMAC were similar and slightly lower than that for the function sub-scale of the original WOMAC.
Table 6.
Standardized response means for the original and reduced versions of the Berg Balance Scale (BBS) and the Western Ontario–McMaster Universities Osteoarthritis Index (WOMAC) (n = 54)
| Outcome Measures | SRM (95% CI) |
|---|---|
| BBS | 1.9 (1.64–2.16) |
| Short BBS | 1.8 (1.54–2.06) |
| WOMAC Pain | 1.0 (0.74–1.26) |
| Hirsch-WOMAC Pain | 0.9 (0.64–1.16) |
| Whitehouse-WOMAC Pain | 1.0 (0.74–1.26) |
| WOMAC function | 1.7 (1.44–1.96) |
| Hirsch-WOMAC function | 1.4 (1.14–1.66) |
| Whitehouse-WOMAC function | 1.5 (1.24–1.76) |
| Tubach-WOMAC function | 1.5 (1.24–1.76) |
SRM = standardized response mean; 95% CI = 95% confidence interval
The absolute measurement errors for the original and short BBS were similar (see Table 7). The absolute measurement errors for the function sub-scale of the original WOMAC, the function sub-scale of the Whitehouse-WOMAC, and the Tubach-WOMAC were similar. The absence of a reliability coefficient for the Hirsch-WOMAC version prevented a calculation of its measurement error.
Table 7.
Absolute Measurement Error for Original and Reduced Versions of the Berg Balance Scale (BBS) and the Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC) (n=54)
| Outcome Measure | Absolute Measurement Error |
|---|---|
| BBS | 0.02 |
| Short BBS | 0.01 |
| WOMAC function | 0.07 |
| Hirsch-WOMAC function | – |
| Whitehouse-WOMAC function | 0.06 |
| Tubach-WOMAC | 0.07 |
DISCUSSION
The current study compared the reduced and original versions of the BBS and the WOMAC with respect to concurrent validity and responsiveness. The results suggest that information provided by the reduced versions of the BBS and WOMAC is similar to that provided by the original versions of these measures in patients following THA or TKA. The reduced versions of the BBS and the WOMAC could therefore be used to assess this population of patients. Use of these reduced versions would reduce administration and scoring time relative to the original versions, making them useful in both clinical and research situations.
The current study observed good to excellent correlations between original and reduced versions of the BBS. Furthermore, the SRM and absolute measurement errors were similar for the original and reduced versions of the BBS. The SRM for the BBS in the current study (1.9) was slightly higher than that reported by Seely (SRM=1.43)25 in patients assessed on the BBS before and 3 months after TKA.
The reduced versions of the WOMAC pain and function sub-scales also produced good to excellent and similar correlations with the original WOMAC. Correlations for the pain (r=0.95 and 0.93) and function (r=0.92 and 0.95) sub-scales between the Hirsch-WOMAC and the original WOMAC in the current study were similar to those reported by Hirsch et al.5 for the three-item pain (r=0.94) and five-item function (r=0.96) sub-scales 1 year after THA or TKA. Although Whitehouse et al.9 assessed correlations between the original WOMAC and the Whitehouse-WOMAC function sub-scales using Spearman's rank correlation coefficient, correlations reported by Whitehouse et al.9 (r=0.97 and 0.96 for THA and TKA, respectively) were similar to those observed in the current study for occasion 2 (r=0.95). Correlations reported by Tubach et al.6 between the function sub-scale of the original WOMAC and the Tubach-WOMAC (r=0.95) in patients with hip or knee OA were identical to those demonstrated in the current study on both occasions (r=0.95).
The SRM for an outcome measure has commonly been calculated as the mean change in scores between two different occasions divided by the standard deviation of the change scores.21,22 The SRM for the original WOMAC function sub-scale in the current study (1.7) was similar to that reported by Seely (SRM=1.8)25 in patients assessed on the WOMAC before and 3 months after TKA. The SRM calculated by Hirsch et al.5 for the original WOMAC and Hirsch-WOMAC was based on the mean difference between preoperative and 1-year postoperative scores following THA or TKA. The SRMs for the pain sub-scale of the original WOMAC and Hirsh-WOMAC reported by Hirsch et al.5 (0.88 and 0.87, respectively) in patients following THA or TKA were similar to those observed in the current study (1.0 and 0.9, respectively). However, the SRMs reported for the function sub-scales of the original WOMAC and the Hirsch-WOMAC (0.65 and 0.62, respectively) were lower than those observed in the current study (1.7 and 1.4, respectively). Although the SRM reported by Hirsch el al.5 was lower than that observed in the current study, the SRM was found to be similar for the original WOMAC and Hirsch-WOMAC function sub-scales in the same study sample.
The SRM for the Whitehouse-WOMAC function sub-scale observed in the current study was similar to that reported by Whitehouse et al.9 (SRM=1.5) in a sample of patients 3 months after THA or TKA. The SRMs reported by Tubach et al.6 for the original WOMAC function sub-scale and the Tubach-WOMAC (0.80 and 0.84, respectively), assessed in patients with hip or knee OA, were lower than those observed in the current study (1.7 and 1.5, respectively). The SRMs for the original WOMAC function sub-scale and the Tubach-WOMAC reported by Tubach et al.6 were based on the mean change in scores over 4 weeks in patients with hip or knee OA, as compared to mean change in scores over 5 to 7 weeks in patients following THA or TKA in the current study. Based on the finding that the SRMs for the function sub-scales of the original and reduced versions of the WOMAC in the current study were higher than those reported by Hirsch et al.5 and by Tubach et al.,6 these outcome measures may be better suited to assess change in patients with THA or TKA within 5 to 7 weeks following surgery. However, further study is required to address this question.
Although correlation between the Whitehouse-WOMAC and the original WOMAC function sub-scale was slightly lower than correlation between the Hirsch-WOMAC function sub-scale and the Tubach-WOMAC for occasion 1, the correlation was similar for occasion 2. The 95% prediction bands for the Hirsch-WOMAC function sub-scale, the Whitehouse-WOMAC function sub-scale, and the Tubach-WOMAC were similar (see Figures 2–4). In addition, the SRMs for the function sub-scales of the Hirsch-WOMAC and Whitehouse-WOMAC and for the Tubach-WOMAC were similar, although slightly lower than the SRM for the original WOMAC function sub-scale. As noted above, absolute measurement error for the Hirsch-WOMAC was not calculated; however, the absolute measurement errors for the original WOMAC function sub-scale, the Whitehouse-WOMAC function sub-scale, and the Tubach-WOMAC were similar. The correlations and SRMs for the pain sub-scales of the Hirsch-WOMAC, the Whitehouse-WOMAC, and the original WOMAC were also similar.
Although patients who had undergone THA demonstrated better improvement on the outcome measures at occasion 2, there was no significant difference in scores on outcome measures between THA and TKA patients at occasion 1. The current study focused on comparing the psychometric properties of the original and reduced versions of the BBS and the WOMAC, as used by the general population of patients who have undergone THA or TKA. Combining data on THA and TKA patients for analyses in the current study provided a larger sample size to evaluate the psychometric properties of the original and reduced versions. Previous studies have also combined data on patients undergoing THA or TKA to assess the psychometric properties of outcome measures.6 Future studies are needed to determine whether and to what extent the original and reduced values are comparable between THA and TKA populations.
LIMITATIONS
A limitation of the current study is that scores for items on reduced versions of the BBS and the WOMAC were extracted from scores on original versions completed by the patients. Although this method has been used previously,5,6,9 future studies using scores collected independently for the original and reduced versions of the BBS and the WOMAC would be helpful in better understanding the relationships between them and in determining the actual time required to complete each questionnaire. In addition, it is recommended that future studies explore relationships between the original and reduced versions of the BBS and the WOMAC. Separate groups with larger sample sizes of patients undergoing THA or TKA may provide useful information on how these relationships differ between the two groups of patients. Although reduced versions of the BBS and the WOMAC could decrease the response burden for clinicians and for patients, clinicians should be aware of the loss of some detailed information contained in omitted items that appear on the original BBS and WOMAC scales.
CONCLUSION
The original and reduced versions of the BBS and the WOMAC provided similar information about balance and physical function in patients following THA or TKA and were similarly responsive. The use of reduced versions of the BBS and the WOMAC could be particularly beneficial for clinicians and researchers in health care settings. These versions include fewer questions, should take less time to administer and score, and may be associated with lower costs. The reduced versions of the BBS and the WOMAC also decrease the response burden on patients and may therefore increase their willingness to complete these measures.
KEY MESSAGES
What Is Already Known on This Topic
A reduced version of the Berg Balance Scale (BBS) and three reduced versions of the Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC) have recently been developed. Clinicians and researchers have limited information on the utility of these reduced versions of the BBS and the WOMAC.
What This Study Adds
Findings of the current study suggest that the reduced versions of the BBS and the WOMAC are highly related to their original versions and are equally responsive. These reduced versions include fewer questions and can be completed in considerably less time, which suggests that they may have advantages for both clinical and research use.
Jogi P, Spaulding SJ, Zecevic AA, Overend TJ, Kramer JF. Comparison of the original and reduced versions of the Berg Balance Scale and the Western Ontario and McMaster Universities Osteoarthritis Index in patients following hip- or knee-joint arthroplasty. Physiother Can. 2010;preprint. doi:10.3138/ptc.2009-26
REFERENCES
- 1.Saleh KJ, Radosevich DM, Kassim RA, Moussa M, Dykes D, Bottolfson H, et al. Comparison of commonly used orthopaedic outcome measures using palm-top computers and paper surveys. J Orthop Res. 2002;20:1146–51. doi: 10.1016/S0736-0266(02)00059-1. doi: 10.1016/S0736-0266(02)00059-1. [DOI] [PubMed] [Google Scholar]
- 2.Chien CW, Lin JH, Wang CH, Hsuch IP, Sheu CF, Hsieh CL. Developing a short form of the Postural Assessment Scale for people with stroke. Neurorehabil Neural Repair. 2007;21:81–90. doi: 10.1177/1545968306289297. doi: 10.1177/1545968306289297. [DOI] [PubMed] [Google Scholar]
- 3.Ware JE, Kosinski M, Keller SD. A 12-item Short-Form Health Survey: construction of scales and preliminary tests of reliability and validity. Med Care. 1996;34:220–33. doi: 10.1097/00005650-199603000-00003. [DOI] [PubMed] [Google Scholar]
- 4.Ware JE, Kosinski M, Dewey JE, Gandek B. How to score and interpret single-item health status measures: a manual for users of the SF-8 health survey. Lincoln, RI: Qualitymetric Inc.; 2001. [Google Scholar]
- 5.Hirsch PB, Gollish JD, Hawker G, Kreder H, Mahomed N, Williams JI. Information strategy: urgency rating, waiting list management and patient outcomes monitoring for primary hip/knee joint replacement. Toronto: ICES Consensus Group; 2000. Reduction of the WOMAC using Rasch methodology; pp. 68–73. [Google Scholar]
- 6.Tubach F, Baron G, Falissard B, Logert I, Dougados M, Bellamy N, et al. Using patients' and rheumatologists' opinions to specify a short form of the WOMAC function subscale. Ann Rheum Dis. 2005;64:75–9. doi: 10.1136/ard.2003.019539. doi: 10.1136/ard.2003.019539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Chou CY, Chien CW, Hsueh IP, Sheu CF, Wang CH, Hsieh CL. Developing a short form of the Berg Balance Scale for people with stroke. Phys Ther. 2006;86:195–204. [PubMed] [Google Scholar]
- 8.Bellamy N, Buchanan WW, Goldsmith H, Campbell J, Stitt L. Validation study of WOMAC: a health status instrument for measuring clinically-important patient-relevant outcomes following total hip or knee arthroplasty in osteoarthritis. J Orthop Rheumatol. 1988;1:95–108. [PubMed] [Google Scholar]
- 9.Whitehouse SL, Lingard EA, Katz JN, Learmonth ID. Development and testing of a reduced WOMAC function scale. J Bone Joint Surg. 2003;85:706–11. [PubMed] [Google Scholar]
- 10.Berg KO, Maki BE, Williams JI, Holliday PJ, Wood-Dauphinee SL. Clinical and laboratory measures of postural balance in an elderly population. Arch Phys Med Rehabil. 1992;73:1073–80. [PubMed] [Google Scholar]
- 11.Newstead AH, Hinman MR, Tomberlin JA. Reliability of the Berg Balance Scale and Balance Master limits of stability tests for individuals with brain injury. J Neurol Phys Ther. 2005;29:18–23. doi: 10.1097/01.npt.0000282258.74325.cf. [DOI] [PubMed] [Google Scholar]
- 12.Belgen B, Beninato M, Sullivan PE, Narielwalla K. The association of balance capacity and falls self-efficacy with history of falling in community-dwelling people with chronic stroke. Arch Phys Med Rehabil. 2006;87:554–61. doi: 10.1016/j.apmr.2005.12.027. doi: 10.1016/j.apmr.2005.12.027. [DOI] [PubMed] [Google Scholar]
- 13.Qutubuddin AA, Pegg PO, Cifu DX, Brown R, McNamee S, Carne W. Validating the Berg Balance Scale for patients with Parkinson's disease: a key to rehabilitation evaluation. Arch Phys Med Rehabil. 2005;86:789–92. doi: 10.1016/j.apmr.2004.11.005. doi: 10.1016/j.apmr.2004.11.005. [DOI] [PubMed] [Google Scholar]
- 14.Hess JA, Woollacott M. Effect of high-intensity strength-training on functional measures of balance ability in balance-impaired older adults. J Manip Physiol Ther. 2005;28:582–90. doi: 10.1016/j.jmpt.2005.08.013. doi: 10.1016/j.jmpt.2005.08.013. [DOI] [PubMed] [Google Scholar]
- 15.Wang CH, Hsueh IP, Sheu CF, Yao G, Hsieh CL. Psychometric properties of 2 simplified 3-level balance scales used for patients with stroke. Phys Ther. 2004;84:430–38. [PubMed] [Google Scholar]
- 16.Ritter MA, Albohm MJ, Keating EM, Faris PM, Meding JB. Comparative outcomes of total joint arthroplasty. J Arthroplasty. 1995;10:737–41. doi: 10.1016/s0883-5403(05)80068-3. doi: 10.1016/S0883-5403(05)80068-3. [DOI] [PubMed] [Google Scholar]
- 17.Jones CA, Voaklander DC, Johnston DW, Suarez-Almazor ME. The effect of age function, and quality of life after total hip and knee arthroplasty. Arch Intern Med. 2001;161:454–60. doi: 10.1001/archinte.161.3.454. doi: 10.1001/archinte.161.3.454. [DOI] [PubMed] [Google Scholar]
- 18.Beaupre LA, Davies DM, Jones CA, Cinats JG. Exercise combined with continuous passive motion or slider board therapy compared with exercise only: a randomized controlled trial of patients following total knee arthroplasty. Phys Ther. 2001;81:1029–37. [PubMed] [Google Scholar]
- 19.Deyle GD, Henderson NE, Matekel RL, Ryder MG, Garber MB, Allison SC. Effectiveness of manual physical therapy and exercise in osteoarthritis of the knee: a randomized, controlled trial. Ann Intern Med. 2000;132:173–81. doi: 10.7326/0003-4819-132-3-200002010-00002. [DOI] [PubMed] [Google Scholar]
- 20.Weber JC, Lamb DR. Statistics and research in physical education. Saint Louis, MO: CV Mosby; 1970. [Google Scholar]
- 21.Wright JG, Young NL. A comparison of different indices of responsiveness. J Clin Epidemiol. 1997;50:239–46. doi: 10.1016/s0895-4356(96)00373-3. doi: 10.1016/S0895-4356(96)00373-3. [DOI] [PubMed] [Google Scholar]
- 22.Liang MH, Fossel AH, Larson MG. Comparisons of five health status instruments for orthopedic evaluation. Med Care. 1990;7:632–42. doi: 10.1097/00005650-199007000-00008. doi: 10.1097/00005650-199007000-00008. [DOI] [PubMed] [Google Scholar]
- 23.Beaton DE, Hogg-Johnson S, Bombardier C. Evaluating changes in health status: reliability and responsiveness of five generic health status measures in workers with musculoskeletal disorders. J Clin Epidemiol. 1997;50:79–93. doi: 10.1016/s0895-4356(96)00296-x. doi: 10.1016/S0895-4356(96)00296-X. [DOI] [PubMed] [Google Scholar]
- 24.Terwee CB, Mokkink LB, Steultjens MPM, Dekker J. Performance-based methods for measuring the physical function of patients with osteoarthritis of the hip or knee: a systematic review of measurement properties. Rheumatology. 2006;45:890–902. doi: 10.1093/rheumatology/kei267. doi: 10.1093/rheumatology/kei267. [DOI] [PubMed] [Google Scholar]
- 25.Seely T. Standing balance before and after total knee arthroplasty: a pilot study [thesis] London, ON: The University of Western Ontario; 2005. [Google Scholar]