Summary
C57BL/6 mice infected with Schistosoma mansoni naturally develop mild CD4+ T cell-mediated immunopathology characterized by small hepatic granulomas around parasite eggs. However, immunization with soluble egg antigens in CFA (SEA/CFA) markedly exacerbates the lesions by inducing a potent proinflammatory environment with high levels of IFN-γand IL-17, which are signature cytokines of distinct Th1 vs. Th17 cell lineages. To determine the relative role of these subsets in disease exacerbation, we examined mice deficient in T-bet (T-bet-/-), which is required for Th1 cell differentiation and IFN-γ production. We now report that SEA/CFA immunization caused a significant enhancement of egg-induced hepatic immunopathology in T-bet-/- mice compared to BL/6 WT controls, and analysis of their granulomas disclosed a higher proportion of activated DC and CD4+ T cells, as well as a marked influx of neutrophils. The absence of IFN-γ in the T-bet-/- mice correlated with a marked increase in IL-23p19, IL-17 and TNF-α in granulomas and MLN. In contrast, T-bet-/- mice had lower levels of IL-4, IL-5 and IL-10 and a reduction in FIZZ1 and Foxp3 expression, suggesting diminished regulatory activity, respectively, by alternatively activated macrophages and regulatory T cells. These findings demonstrate that T-bet-dependent signaling negatively regulates Th17 cell-mediated immunopathology in severe schistosomiasis.
Keywords: Helminth infection, Inflammation, Cytokines
Introduction
Infection with the helminth Schistosoma mansoni causes a major tropical infectious disease in which the main pathology is a granulomatous and fibrosing inflammation against parasite eggs lodged in the liver and intestines. The resulting tissue injury is mediated and orchestrated by CD4+ T cells specific for egg Ags and thus is immune in nature; however, it varies greatly in intensity among individuals and also mouse strains in an experimental model [1, 2]. Extensive work to understand the role of CD4+ T cell subsets and related cytokines in the initiation and regulation of the immunopathology precipitated by the schistosome eggs demonstrated that in the BL/6 stain an early proinflammatory Th1-type response gives way to a Th2-dominated environment, and that the failure of this transition results in an exacerbation of hepatic pathology and death [3-6]. However, this view was complicated by more recent observations indicating that a novel immunopathogenic pathway leading to the differentiation of proinflammatory CD4+ Th17 cells plays a major role in the development of the severe egg-induced lesions [7, 8]. Evidence for this are the high levels of IL-17 observed in the naturally high pathology CBA strain, as well as in a model of disease exacerbation induced in (normally low pathology) C57BL/6 mice by immunization with schistosome soluble egg Ag (SEA) in CFA (SEA/CFA) [6, 7].
IL-17-producing (Th17) cells are now recognized as a separate lineage of CD4+ T cells [9, 10] that are critically involved in the immunopathology associated with an increasing number of autoimmune [11-15] and infectious diseases [8, 16-19], that were previously thought to be mediated by Th1 cells, largely through the action of their signature cytokine IFN-γ. Th17 cells were first described to be dependent on IL-23 [20], an accessory cell-derived heterodimeric cytokine related to IL-12, with which it shares the subunit IL-12p40 that combines with the specific subunit IL-23p19, instead of the IL-12p35 subunit used by IL-12 [21, 22]. Subsequently, however, Th17 cells were shown to be induced by IL-6 and transforming growth factor (TGF)-β [17, 23, 24], with IL-23 serving to promote their expansion and ensure their survival. A key role of IL-23-mediated Th17 cells in severe schistosomiasis became apparent following the observation that pathology exacerbation together with high IL-17 levels in SEA/CFA-immunized BL/6 mice failed to materialize in IL-12p40-/- (incapable of making either IL-12 or IL-23) or IL-23p19-/- mice (incapable of making IL-23 only), but were not different from wild type (WT) controls in IL-12p35-/- mice (which cannot make IL-12, but do make IL-23) [7, 8].
The discovery of this second proinflammatory pathway prompted the investigation of the relative pathogenicity and possible cross control of Th1 vs. Th17 cells. One of the strategies utilized to address this issue focused on the T-box transcription factor T-bet, which is required for CD4+ Th1 cell differentiation, IFN-γ production, and overall Th1-type immunity development [25, 26]. Initial reports suggested that T-bet signaling can have opposite effects on inflammatory conditions dependent on CD4+ Th17 cells. For example, T-bet-/- mice display a marked enhancement of autoimmune myocarditis [27], whereas, in contrast, experimental autoimmune encephalomyelitis (EAE), completely fails to materialize in the absence of T-bet [28, 29]. In view of these contrasting findings, we investigated the schistosome infection in T-bet-/- mice, under conditions where the hepatic egg-induced lesions were enhanced by immunization with SEA/CFA. We now show that T-bet-/- mice displayed markedly exacerbated hepatic immunopathology when compared to similarly treated WT BL/6 mice. Despite the absence of IFN-γ, granulomas from the T-bet-/- mice revealed a higher content of activated DC and IL-17-producing CD4+ T cells together with a marked increase in Gr-1+ neutrophils.
Results
Schistosome-infected T-bet-/- mice develop a more severe, neutrophil-rich, egg-induced liver inflammation in response to SEA/CFA immunization than BL/6 mice
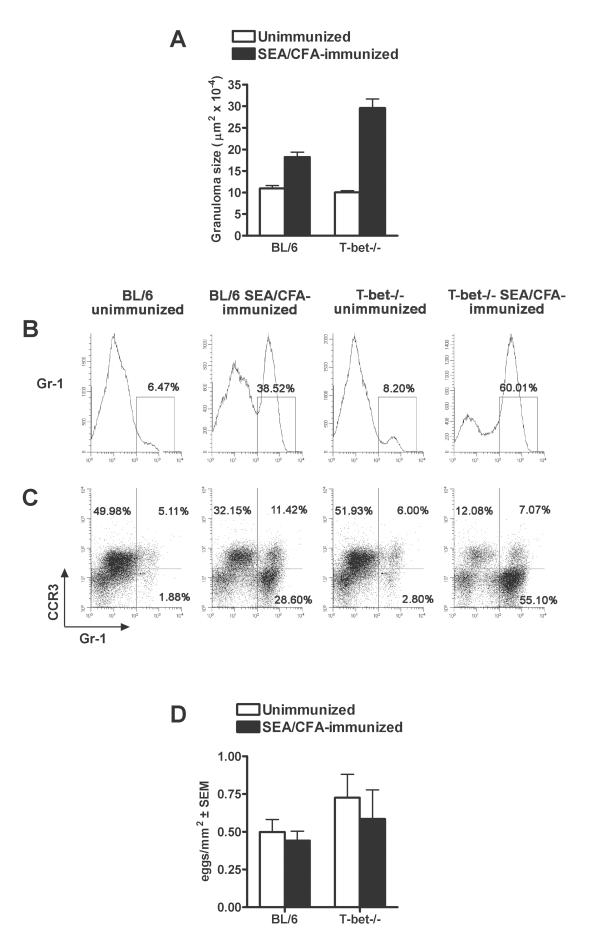
We have previously shown that immunization with SEA/CFA in BL/6 mice causes a significant exacerbation of hepatic egg-induced immunopathology and death after schistosome infection [6-8]. We now investigated the role of the Th1-specific transcription factor T-bet in the development of the severe pathology. SEA/CFA-immunized, 7 week-schistosome infected T-bet-/- mice displayed a marked exacerbation in hepatic perioval granulomatous inflammation in comparison with similarly treated BL/6 mice (figure 1A). In the T-bet-/- mice the lesions contained a considerably higher proportion of granulocytes, which together with mononuclear cells (lymphocytes, DC and macrophages) extensively infiltrated the surrounding hepatic parenchyma. Phenotypic analysis of the granuloma cells (GC) by flow cytometry confirmed that SEA/CFA immunization induced a significantly greater infiltration of Gr-1+ cells in T-bet-/- (60.01%) than in BL/6 mice (38.52%) in comparison with similar low levels of 8.20% and 6.47% in the corresponding unimmunized controls (Figure 1B). The higher number of Gr-1+ cells recruited to the lesions of the SEA/CFA-immunized T-bet-/- and BL/6 mice were mostly neutrophils, as they did not express CCR3, the receptor for the chemokine CCL11 (eotaxin) typically present on eosinophils [30, 31]. Eosinophils, however, were the dominant CCR3+ granulocytes in the granulomas of the unimmunized control groups (Figure 1C).
Figure 1. Hepatic immunopathology in infected BL/6 and T-bet-/- mice.
A. Hepatic egg granulomas after 7 weeks of infection, measured by computer assisted morphometric analysis, are significantly larger in SEA/CFA-immunized T-bet-/- mice than in BL/6 mice (p< 0.001). Data are from one experiment representative of five with 3 to 5 mice per group. B, C. Gr-1+ and Gr-1+CCR3− cell infiltration in the livers of infected BL/6 and T-bet-/- mice. GC were purified from the livers of infected mice and stained for Gr-1 and CCR3. Gr-1+ cells (B) and Gr-1+CCR3− cells (C) are markedly increased in granulomas from SEA/CFA-immunized T-bet-/- vs. BL/6 mice. Data shown are from one experiment representative of four with similar results, using pooled GC from 3 to 5 mice from each group. D. Liver egg counts. Schistosome eggs were counted on hematoxilyn and eosin-stained liver sections from 7-week infected mice as described in the Material and methods. There are no significant differences in the number of eggs present in all four groups.
These findings demonstrate that the T-bet-/- mice displayed a markedly higher inflammatory reaction in response to immunization with SEA/CFA than the BL/6 mice, although in both groups the lesions were significantly larger than in the corresponding unimmunized controls (Figures 1A). Since the possibility existed that the differing degrees of inflammation could be due to a dissimilar number of embolized eggs, we counted the number of eggs per tissue area on liver sections and found no significant differences among all the groups (Figure 1D). Therefore, the contrasting immunopathologies truly reflected differences in the intensity of inflammation.
DC and CD4+ T cells from hepatic granulomas display greater activation in SEA/CFA-immunized T-bet-/- than BL/6 mice
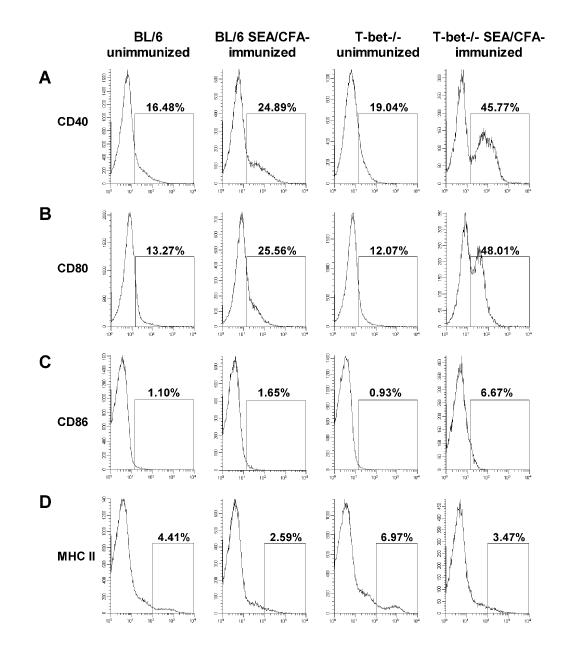
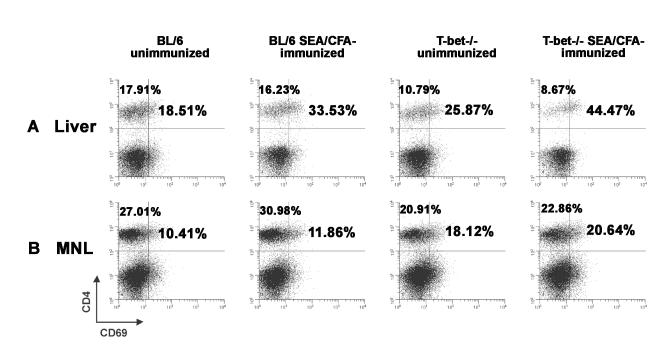
Because the outcome of egg-induced immunopathology critically depends on the nature of the underlying Ag-specific CD4+ T cells, we first examined the phenotype of DC and T cells of T-bet-/- and BL/6 mice. DC are the APC most directly linked to activating and polarizing naïve T cells to mediate diverse adaptive immune responses [32]. Flow cytometryic analysis of liver GC demonstrated that SEA/CFA immunization caused a markedly greater activation of CD11c+ DC in T-bet-/- than in BL/6 mice, as judged by the two-fold higher expression of the costimulatory molecules CD40 and CD80, and the four-fold higher expression of CD86 (Figures 2A-C). There were no significant differences in the induction of MHC class II molecule expression between the two SEA/CFA-immunized groups (Figure 2D). Interestingly, T cell activation measured by CD69 expression was greater in T-bet-/- than BL/6 mice, both SEA/CFA-immunized or unimmunized. Moreover, although there were proportionally more CD4+ T cells in MLN than in the granulomas; those co-expressing CD69 were higher in the granulomas (Figure 3A, B). Taken together, these findings demonstrate that in schistosome-infected T-bet-/- mice SEA/CFA immunization results in greater activation of both DC and CD4+ T cells than in the WT BL/6 controls.
Figure 2. Costimulatory and MHC class II molecule expression on CD11c+ DC from granulomas of infected BL/6 and T-bet-/- mice.
A-D. Liver GC were surface-stained ex vivo with anti-CD11c and anti-CD40, anti-CD80, CD86 or anti-MHC II mAb. A-C. Expression of CD40, CD80 and CD86 is higher on CD11c+ DC from SEA/CFA-immunized T-bet-/- mice than from BL/6 mice. D. MHC II expression is reduced on CD11c+ DC from both SEA/CFA-immunized mouse groups. Percentages shown are from gated CD11c+ cells expressing the indicated marker from one experiment representative of three with similar results.
Figure 3. Activation of CD4+ T cells from granulomas and MLN of infected BL/6 and T-bet-/- mice.
Liver GC and MLNC were surface-stained ex vivo with anti-CD4 and anti-CD69 mAb. A. The percentage of CD4+ T cell-expressing CD69 (upper right quadrant) is higher and the proportion of CD4+ T cells (upper quadrants) is lower in granulomas from SEA/CFA-immunized T-bet-/- mice than from BL/6 mice. B. The percentage of CD4+ T cells-expressing CD69 (upper right quadrant) is higher and the proportion of CD4+ T cells (upper quadrants) is lower in MLN from SEA/CFA-immunized T-bet-/- mice than from BL/6 mice. Percentages shown are CD4+ and CD69+ cells within the CD4+ T cell population in the lymphocyte gate. Results are from one experiment representative of four with similar results, using pooled GC and MLNC from 3 to 5 mice per group.
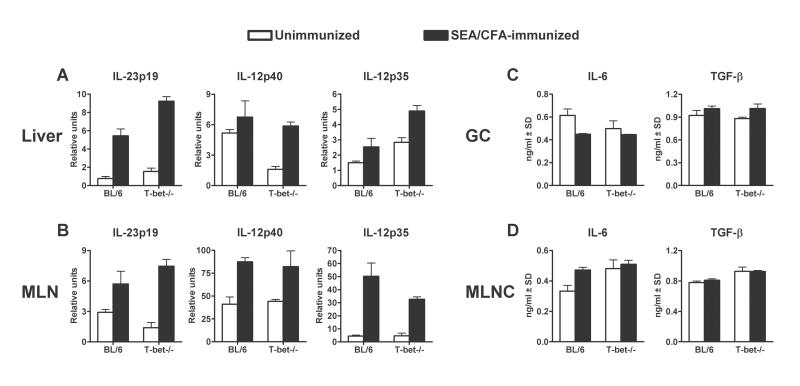
In SEA/CFA-immunized T-bet-/- mice there is an increase in IL-23p19, but not in IL-6 or TGF-β
We further investigated how exacerbation of pathology and increase in immunocyte activation in the absence of T-bet affected APC and T cell function, in particular the Th17 subset. IL-6 and TFG-β have been proposed to represent key innate cytokines required for the induction of Th17 cells, with IL-23 acting to sustain and expand the phenotype [20, 23, 24, 33]. Our previous work indicated that exacerbation of hepatic egg-induced immunopathology in SEA/CFA-immunized BL/6 mice correlated with a high IL-17 response, and that IL-17 expression in the lesional environment was dependent on IL-23 [7, 8].
SEA/CFA immunization increased IL-23p19, IL-12p40 and IL-12p35 mRNA expression in livers (Figure 4A) and MLN (Figure 4B) of both BL/6 and T-bet-/- mice.The increase of IL-23p19 was more pronounced both in livers and MLN of T-bet-/- mice, IL-12p40 did not differ between the groups, and IL-12p35 was higher in livers but lower in MLN of T-bet-/- vs. BL/6 mice. On the other hand, SEA-induced IL-6 or TGF-β production by GC (Figure 4C) and MLNC (Figure 4D) was not significantly different between SEA/CFA-immunized BL/6 and T-bet-/- mice.
Figure 4. Innate cytokine expression and production in livers and MLN of infected BL/6 and T-bet-/- mice.
Cytokine mRNA expression in livers and MLN was measured by real time RT-PCR and cytokine production in 48-h supernatants from SEA-stimulated GC and MLNC was measured by ELISA. A. mRNA levels for IL-23p19, IL-12p40 and IL-12p35 are higher in the livers from SEA/CFA-immunized mice but only IL-23p19 and IL-12p35 are significantly higher in T-bet-/- than in BL/6 mice (both p< 0.01). B. mRNA levels for IL-23p19, IL-12p40 and IL-12p35 are higher in the MLN from SEA/CFA-immunized mice but do not significantly differ between T-bet-/- and BL/6 mice. SEA-induced IL-6 and TGF-β production by GC (C) and MLNC (D) does not significantly differ between T-bet-/- and BL/6 mice. For transcript levels, bars represent the means of triplicate determinations ± SD from a pool of 3 to 5 mRNA preparations per group. Cytokine levels are expressed as means of triplicate determinations ± SD; background cytokine levels from unstimulated GC or MLNC were subtracted (except for TGF-β). Results shown are from one experiment representative of five.
In SEA/CFA-immunized T-bet-/- mice, the absence of IFN-γ correlates with a marked increase in IL-17 and TNF-α, and a decrease in IL-4, IL-5 and IL-10
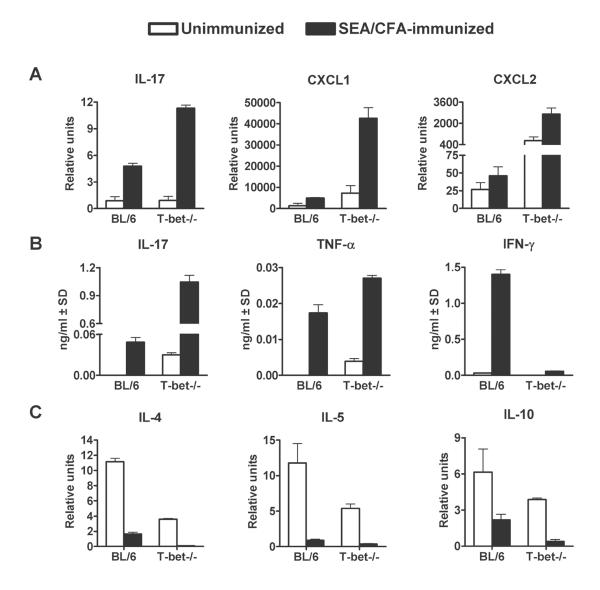
The described findings suggested that the egg-induced pathology exacerbation following SEA/CFA immunization correlated with an increase in IL-23, and that this was significantly higher in the T-bet-/- mice. We next investigated how the increase in IL-23 correlated with CD4+ T cell function in the absence of T-bet signaling. There was a considerably greater increase in IL-17 and in the neutrophil chemoattractants CXCL1 and CXCL2 mRNA levels in the livers of SEA/CFA-immunized T-bet-/- than in BL/6 mice (Figure 5A). Moreover, SEA-stimulated GC from SEA/CFA-immunized T-bet-/- mice produced significantly more IL-17 and TNF-α than those from BL/6 mice. As expected, IFN-γ was absent in T-bet-/- mice, thus confirming the need for T-bet in Th1 cell differentiation and IFN-γ production [25, 26], while SEA/CFA immunization stimulated robust IFN-γ production in the BL/6 mice (Figure 5B). In contrast, SEA/CFA immunization caused a marked decrease in liver IL-4, IL-5 and IL-10 mRNA expression (Figure 5C), although, interestingly, these cytokines were also lower in the unimmunized T-bet-/- mice than in the corresponding BL/6 group.
Figure 5. Effector cytokine expression and production in livers and GC of infected BL/6 and T-bet-/- mice.
A-C. Cytokine mRNA and production levels were measured as described in materials and methods. A. mRNA levels for IL-17, CXCL1 and CXCL2 are significantly higher in SEA/CFA-immunized T-bet-/- than in BL/6 mice (p< 0.001; p< 0.001 and p< 0.01 respectively). B. IL-17 and TNF-α production by SEA-stimulated GC is significantly higher in SEA/CFA-immunized T-bet-/- than in BL/6 mice (p< 0.01 and p< 0.001, respectively). C. mRNA levels for IL-4, IL-5 and IL-10 are lower in SEA/CFA-immunized T-bet-/- than in BL/6 mice but only IL-4 and IL-10 are significantly different (both p< 0.05). For transcript levels, bars represent the means of triplicate determinations ± SD from 3 to 5 mRNA preparations per group. Cytokine levels reflect means of triplicate determinations ± SD; minus backgrounds. Results shown are from one experiment representative of five.
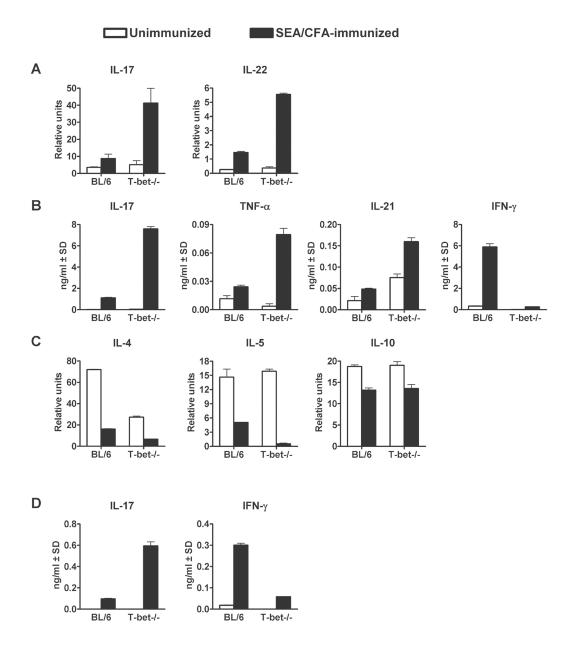
Cytokine expression in MLN tissue and SEA-induced cytokine production by MLNC generally paralleled those observed in the liver. Thus, mRNA levels for IL-17, as well as those for the Th17-related cytokine IL-22 [34] were significantly higher in the MLN from SEA/CFA-immunized T-bet-/- than BL/6 mice (Figure 6A). SEA-induced IL-17, TNF-α and IL-21 production was also significantly increased, and IFN-γ was virtually absent in the SEA/CFA-immunized T-bet-/- mice (Figure 6B). mRNA expression for IL-4, IL-5 and IL-10 (Figure 6C) was reduced after SEA/CFA immunization but only IL-4 and IL-5 levels were significantly different between T-bet-/- and BL/6 mice. Lastly, in a separate set of experiments using SEA-stimulated purified CD4+ T cells from MLN of infected mice plus normal syngeneic APC, we documented that IL-17 in both SEA/CFA-immunized mouse groups, and IFN-γ, in the case of SEA/CFA-immunized BL/6 WT, were indeed a product of the sensitized T cells (Figure 6D).
Figure 6. Effector cytokine expression and production in MLN and MLNC or purified CD4+ T cells of infected BL/6 and T-bet-/- mice.
A-D. Cytokine mRNA and production levels were measured as described in materials and methods A. mRNA levels for IL-17 and IL-22 are significantly higher in SEA/CFA-immunized T-bet-/- than in BL/6 mice (both p< 0.001). B. IL-17, TNF-α and IL-21 production by SEA-stimulated MLNC is significantly higher in SEA/CFA-immunized T-bet-/- than in BL/6 mice (p< 0.01, p< 0.001 and p< 0.001, respectively). C. mRNA levels for IL-4 and IL-5 are significantly lower in the SEA/CFA-immunized T-bet-/- than in BL/6 mice (p< 0.01 and p< 0.05, respectively). mRNA levels for IL-10 are reduced in SEA/CFA-immunized mice, but do not significantly differ between T-bet-/- and BL/6 mice. D. SEA-induced IL-17 and IFN-γ production from purified CD4+ T cells is increased after immunization with SEA/CFA and IL-17 is significantly higher in SEA/CFA-immunized T-bet-/- than in BL/6 mice (p< 0.001). For transcript levels, bars represent the means of triplicate determinations ± SD from a pool of 3 to 5 mRNA preparations per group. Cytokine levels reflect means of triplicate determinations ± SD; minus backgrounds. Results shown are from one experiment representative of five.
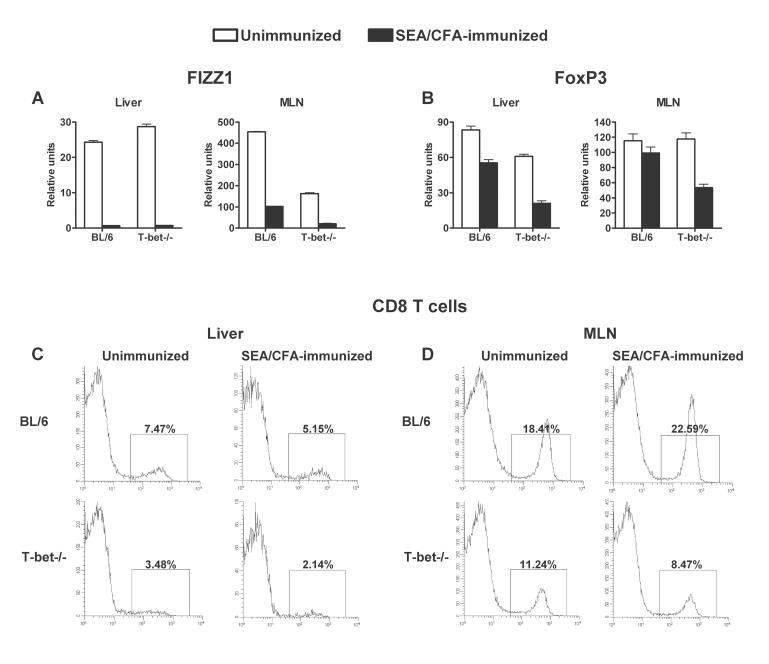
Exacerbated egg-induced immunopathology in SEA/CFA-immunized T-bet-/- mice correlates with a reduction in FIZZ1 and Foxp3 expression, and in CD8+ T cells
The significant increase in immunopathology and proinflammatory cytokine production in the SEA/CFA-immunized T-bet-/- mice suggested a possible break-down of immunoregulatory mechanisms. Th2 type responses have been shown to be critical for the development of the anti-inflammatory alternatively activated macrophages (AAM) [35, 36], and IL-10 has been associated with T regulatory cell (T reg) function [37]. Both of these cells have been postulated to control excessive inflammation against schistosome eggs [36, 38-40]. We investigated the differential expression of the secretory protein FIZZ1 (found in inflammatory zone 1), as a marker of AAM [35, 41-43], as well as the forkhead box P3 (Foxp3) transcription factor, which is a marker of T reg [37]. SEA/CFA immunization per se caused a significant drop in FIZZ1 and Foxp3 expression in liver and MLN (figure 7A, B). However, this decrease was more pronounced in T-bet-/- than in BL/6 mice, except for liver expression of FIZZ1, which was exceedingly low in both groups. We lastly examined CD8+ T cells, which also have been implicated in the down-regulation of the schistosome egg-induced immunopathology [44]. T bet-/- mice indeed had a lower percentage of CD8+ T cells in both the liver granulomas (Figure 7C) as well as the MLN (Figure 7D); this trend was further exacerbated upon immunization with SEA/CFA. Overall, these observations demonstrate that the absence of T-bet leads to a break-down of multiple possible regulatory mechanisms, resulting in an increase of immunocyte activation and Th17 cell-driven inflammation.
Figure 7. FIZZ1, Foxp3 expression and CD8+ T cells in livers and MLN from infected BL/6 and T-bet-/- mice.
A-B. mRNA expression in the livers and MLN was measured by real time RT-PCR as described in Materials and Methods. A. FIZZ1 mRNA levels are significantly lower in SEA/CFA-immunized mice, but only in the MLN are significantly different between T-bet-/- and BL/6 mice (p< 0.001) B. Foxp3 mRNA levels are lower in SEA/CFA-immunized mice but are significantly lower in the livers and MLN from T-bet-/- than BL/6 mice (p< 0.001 and p< 0.05, respectively). C-D. Liver GC and MLNC were surface stained ex vivo with anti-CD8 mAb. The percentage of CD8+ T cells is lower in granulomas and MLNC from SEA/CFA-immunized T-bet-/- mice than from BL/6 mice. Percentages shown are CD8+ T cells in the lymphocyte gate. Results are from one experiment representative of two with similar results, using pooled GC or MLNC from 3 to 5 mice per group.
Discussion
Our previous work has demonstrated that severe immunopathology in schistosomiasis, either naturally-occurring in CBA mice, or induced by immunization of BL/6 mice with SEA/CFA, is associated with a proinflammatory environment characterized by high levels of IFN-γ and IL-17 [7] indicative of the presence of Th1 and Th17 cell responses. In order to dissect the relative contribution of Th1 vs. Th17 cells to the development of severe pathology, we used T-bet-/- mice which are defective in Th1 immunity [25, 26]. Because T-bet-/- mice are on a low pathology BL/6 (H-2b) background, some mice were also immunized with SEA/CFA to examine the role of T-bet in a high pathology setting.
The most salient result of our study was the significantly exacerbated liver pathology in the SEA/CFA-immunized T-bet-/- mice, with perioval and adjacent parenchymal inflammatory lesions infiltrated by large numbers of Gr-1+ neutrophils. The exacerbated immunopathology clearly reflected a more vigorous host immune response as there were no significant differences in egg counts between the livers of T-bet-/- and BL/6 mice.
To address the basis of the enhanced inflammation resulting from the absence of T-bet, we examined phenotypic changes and function of DC and CD4+ T cells, which are cells critically involved in the immunopathological response to schistosome eggs. Our results demonstrated that in infected T-bet-/- mice, the severe SEA/CFA-induced immunopathology correlated with a markedly increased expression of CD40, CD80 and CD86 costimulatory molecules on CD11c+ DC present in hepatic granulomas. Moreover, increased CD69 expression following SEA/CFA immunization denoted enhanced activation in CD4+ T cells. CD69 expression was proportionately higher in the liver granulomas and MLN from T-bet-/- than BL/6 mice, an observation that contrasts with the notion that T-bet is required for optimal T cell activation [45] but agrees with a study on T cell differentiation in T. cruzi infection [46]. The relative role of APC vs. CD4+ T cells in the induction of severe pathology remains to be elucidated.
The heightened cell activation in the schistosome-infected mice following SEA/CFA immunization was accompanied by an increase in IL-23p19, IL-17, IL-21, IL-22, TNF-α and the leukocyte chemoattractants CXCL1 and CXCL2, however, these cytokines were significantly higher in T-bet-/- than in BL/6 mice. All these cytokines are associated with the IL-23/IL-17 axis [47, 48] although IL-21 can also be elevated in context with Th2 responses [49]. IFN-γ was only increased in BL/6 mice as in T-bet-/- mice it was predictably absent despite the induction of IL-12; however, there were no significant differences in IL-6 and TGF-β induced by SEA in GC and MLNC between both groups. In contrast, the SEA/CFA immunization caused a drop in liver and MLN IL-4, IL-5 and IL-10, with levels further reduced in the T-bet-/- mice. This observation, together with the decreased expression of the Th2-lineage associated transcription factor GATA-3 (data not shown), confirms that T-bet-/- mice do not default towards Th2 immunity [25, 26]; instead, in this model, they clearly display a higher net proinflammatory cytokine balance that correlates well with their exacerbated immunopathology.
The increased immunopathology in T-bet-/- mice correlates well with previous observations in infected IFN-γ-/- mice inasmuch as SEA/CFA immunization, also resulted in an increase in egg-induced immunopathology and IL-17 production [7]. In models of experimental arthritis, IFN-γ-/- mice similarly had exacerbated joint inflammation associated with an increase in IL-17 [50-52]. These findings are consistent with the notion that T-bet regulates excessive Th17-mediated immunopathology via IFN-γ.
A most controversial and intriguing issue, however, is that the absence of T-bet has been associated with decreased immunopathology in autoimmune arthritis [53] and in EAE [28] similarly induced by immunization with self-antigen in CFA, as well as in models of type-1 diabetes [54], lupus erythematosus [55] and inflammatory bowel disease [56]. These findings suggested that T-bet plays a vital role in the development of these inflammatory autoimmune diseases. Although at the time of these studies the underlying pathogenic T cells were thought to be of the Th1 or Th2 type, current view would argue that the previously unknown Th17 cells also had to be increased, as subsequent research clearly demonstrated their intimate involvement in the pathogenesis of those same autoimmune conditions [11-15, 33, 57, 58]. It is thus difficult to reconcile how the absence of T-bet can lead to a reduction in pathology and at the same time to an increase in Th17 cells. One possibility is that although Th17 cells are indeed generated, they are unable to reach the target organ, a situation that, because of the blood brain barrier, could be particularly true in the case of the central nervous system.
More in line with our findings in schistosomiasis, recent studies demonstrated that the loss of T-bet can result in exacerbation of pathology and increase in IL-17, as is the case in a model of autoimmune myocarditis induced by immunization with myosin peptides in CFA [27] and T. cruzi infection [46]. T-bet-/- mice also displayed increased IL-17-mediated neutrophil recruitment to the airways [59] and a more robust cardiac allograft rejection [60, 61]. The absence of T-bet, and therefore of Th1 immunity and IFN-γ production, has also been demonstrated to result in increased susceptibility to infection with organisms such as Mycobacterium tuberculosis [62], Leishmania donovani [63], Staphylococcus aureus [64] and salmonella [65] often correlating with an exacerbated, albeit less effective, inflammatory response.
To gain a better understanding of the means by which T-bet controls the exacerbation of egg-induced hepatic inflammation, we investigated AAM, T reg and CD8+ T cells, which have all been suggested to represent down-regulatory mechanisms of the immunopathology in schistosomiasis [38-40, 44]. Indeed, the greater net loss of FIZZ1 expression in the T-bet-/- mice is most consistent with impaired AAM development under conditions of decreased Th2 immunity [35]. Likewise, the decrease in Foxp3 expression together with a significant drop in mRNA levels for IL-10 suggest a greater loss of T reg function in the T-bet-/- mice. IL-10 is an anti-inflammatory cytokine widely associated with T reg [37, 66, 67] and with the down-regulation of APC as well as T cell responses that mediate the immunopathology in schistosomiasis [39, 68, 69]. Lastly, the proportion of CD8+ T cells was significantly lower in the livers and MLN of infected, SEA/CFA-immunized or unimmunized T-bet-/- mice. CD8+ cells have been associated with the down-modulation of schistosome-egg induced immunopathology [44], and it is of interest that the increased severity of autoimmune myocarditis in T-bet-/- mice was attributed to the loss of IFN-γ-production by CD8+ T cells [27]. Thus, in the absence of T-bet, the concurrent reduction of three regulatory mechanisms explains the pathology exacerbation of the schistosome infection with the heightened Th17 response likely contributing to their decline. Of note is that unimmunized T-bet-/- mice seem to be able to control pathology by virtue of higher levels of IL-10 and AAM despite their increased proportion of activated CD4+ T cells. However, immunization with SEA/CFA overpowers these regulatory mechanisms resulting in increased inflammation.
Our observations in experimental schistosomiasis clearly demonstrate that T-bet regulates, rather than promotes, Th17 cell-mediated egg-induced immunopathology by inducing Th1-type immunity and sustaining Th2 as well as immunoregulatory cell networks. However, the demonstrated regulatory effect of the Th1 response does not preclude the pathogenicity of this subset in context with other experimental settings; it merely suggests that in circumstances where two potentially pathogenic subsets could act synergistically, one adopts a regulatory role. Thus, highly individualized immune cell interactions to various Ag or pathogens, and played out in specific target tissues, dictate the final outcome of the immunopathology in each case.
Materials and Methods
Mice, infection and immunization
Age- and sex-matched C57BL/6 T-bet deficient (T-bet-/-) and C57BL/6 (BL/6, WT BL/6) mice, five to six-week-old, were purchased from The Jackson Laboratory (Bar Harbor, ME). All mice were maintained in the Animal Facility at Tufts University School of Medicine in accordance with the Association for Assessment and Accreditation of Laboratory Animal Care (AAALAC) guidelines. The corresponding protocols were reviewed and approved by the local Animal Care and Use Committee. Mice were infected by i.p. injection with 80 cercariae of Schistosoma mansoni (Puerto Rico strain), which were shed from infected Biomphalaria glabrata snails, provided to us by Dr. Fred Lewis, Biomedical Research Institute (Rockville, MD), through NIH/NIAID contract NO1-AI-55270. Some mice were immunized by s.c. injection with 50 μg of SEA emulsified in CFA (SEA/CFA), as previously described [6]. Treatment of BL/6 mice with SEA/CFA causes marked exacerbation of their egg-induced immunopathology; either SEA or CFA by themselves are ineffective in enhancing pathology [6]. SEA was prepared as previously described [70].
Cell preparations
Livers and mesenteric lymph nodes (MLN) were removed aseptically from 7-week infected mice. GC were obtained by homogenization of the livers in a Waring blender, isolation of granulomas by 1 g sedimentation, extensive washing and enzymatic digestion with 1 mg/ml of collagenase type H, from Clostridium histolyticum (Sigma Laboratories, St. Louis, MO). Single cell suspensions from MLN were prepared by teasing the tissues in complete RPMI-1640 medium (cRPMI) supplemented with 10% fetal calf serum (Aleken Biologicals, Nash, TX), 4 mM L-glutamine, 80 U/ml penicillin, 80 μg/ml streptomycin, 1 mM sodium pyruvate, 10 mM HEPES, 1× NEAA (all from Lonza, Allendale, NJ) and 0.1% 2-mercaptoethanol. Erythrocytes were lysed with Tris ammonium chloride buffer pH: 7.2 (Sigma) for 15 min on ice. Cells were washed and live cells that excluded trypan blue were counted and resuspended at the desired concentrations in cRPMI. CD4+ T cells were negatively selected from MLN cells (MLNC) using CD4 MACS columns (Miltenyi Biotec, Auburn, CA) following the manufacturer’s instructions. The resulting cell preparations were > 94% CD4+ T cells as determined by flow cytometry.
Cell cultures and cytokine determinations
Bulk cell suspensions (5 × 106 cells/ml) from hepatic granulomas and MLN, or purified CD4+ T cells from MLN (1 × 106 cells/ml) plus normal irradiated syngeneic splenic APC (4 × 106 cells/ml), were incubated in the presence or absence of 15 μg/ml of SEA. After 48 hours, the culture supernatants were removed, filtered and stored at −36°C until analyzed by ELISA. For the detection of IL-17, IFN-γ, TNF-α, IL-21 and IL-6 mAb, standard cytokines and protocols were obtained from R&D Systems, and for the detection of TGF-β, from BD-Pharmingen (San Jose, CA).
Flow cytometry analysis
GC and MLNC were washed in PBS containing 1% BSA and 0.1% NaN3 and incubated for 10 min at 4°C in the same buffer containing 0.3 mg/ml of rat-IgG (Sigma) to block non-specific binding of Ab. Cells were then stained ex vivo for flow cytometry analysis using PE-conjugated anti-CD8 mAb (clone 53-6.7); allophycocyanin (APC)-conjugated anti-CD4 (clone GK1.5) and FITC-conjugated anti-CD69 (clone H1.2F3); APC-conjugated anti-CD11c (clone HL3) and FITC-conjugated anti-CD40 (clone HM40-3), FITC-conjugated anti-CD80 (clone 16-10A1), FITC-conjugated anti-CD86 (clone GL1) or FITC-conjugated anti-MHC II (clone 2G6); FITC-conjugated anti-Gr-1 (clone RB6-8C5) mAb (all from BD-Pharmingen) and APC-conjugated anti-CCR3 mAb (clone 83101) (R&D Systems, Minneapolis, MA) following a protocol described before [71]. Labeled cells were acquired on a FACSCalibur flow cytometer using the CELLQuest software version 3.2.1 (Becton Dickinson, Franklin Lakes, NJ). Propidium iodide was added before acquisition to exclude dead cells. Data were analyzed using the WinList 5.0 software (Verity Software House, Inc.). Unstained cells and cells stained with irrelevant isotype-matched Ab were included as controls to assess the amount of non-specific staining. To determine the percentage of CD4+ T cells expressing CD69 and CD8+ T cells, lymphocyte-rich areas, comprising 9-15% of GC and 75-85% of MLNC were defined and gated based on forward light scatter (FSC) and side light scatter (SSC) characteristics of the cells (“lymphocyte gate”).
Quantitative mRNA analysis
Total RNA was isolated from individual livers and MLN of 7 week-infected mice, using the TRIzol method following the manufacturer’s instructions (Invitrogen, Carlsbad, CA). RNA from each mouse group was pooled and 1-5 μg was subjected to DNAse I treatment (Roche Molecular Biochemicals, Indianapolis, IN) to eliminate possible genomic DNA contamination, and then reverse-transcribed using the High Capacity cDNA Reverse Transcription Kit (Applied Biosystems, Foster City, CA). Real-time quantitative RT-PCR on 10 ng of cDNA from each sample was performed by Taqman analysis using an ABI 7300 instrument. GAPDH levels were measured in a separate reaction and used to normalize the data. All reagents and protocols for Taqman real-time quantitative RT-PCR were obtained from Applied Biosystems. Using the average mean cycle threshold (Ct) value for GAPDH and the gene of interest for each sample, the equation 1.8 e (Ct GAPDH - Ct gene of interest) × 104 was used to obtain normalized values [12].
Liver immunopathology and egg counts
Liver samples from 7-week infected mice were fixed in 10% buffered formalin and processed for routine histopathologic analysis. Five-μm sections stained with hematoxylin and eosin were examined by optic microscopy. The extent of granulomatous inflammation around schistosome eggs was measured by computer-assisted morphometric analysis using Image-Pro Plus software (Media Cybernetics Inc., Bethesda, MD). The lesions were assessed on coded slides by an observer unaware of the experimental setting. To reflect more accurately the true shape and dimension of the granulomas, only those with a visible central egg were counted. An average of 13 granulomas was scored per liver section. Granuloma sizes are expressed as means of areas measured in μm2 ± SEM. The schistosome egg load was assessed by counting the number of eggs present in 1 mm2 fields of liver tissue sections stained with hematoxylin and eosin. Fifty fields were counted per liver and 7 to 10 livers from two independent experiments were examined per mouse group.
Statistical analysis
ANOVA with post-test analysis was used to determine the statistical significance of the differences among groups. Results differing with a p< 0.05 were considered significant.
Acknowledgements
This work was supported by NIH US Public Health Service Grant RO1-18919.
Abbreviations
- SEA
soluble egg Ag
- GC
granuloma cells
- MLNC
mesenteric lymph node cells
Footnotes
Conflict of interest: The authors declare no financial or commercial conflict of interest.
References
- 1.Bica I, Hamer DH, Stadecker MJ. Hepatic schistosomiasis. Infect. Dis. Clin. North. Am. 2000;14:583–604. viii. doi: 10.1016/s0891-5520(05)70122-7. [DOI] [PubMed] [Google Scholar]
- 2.Cheever A, Duvall R, Hallack T, Jr, Minker R, Malley J, Malley K. Variation of hepatic fibrosis and granuloma size among mouse strains infected with Schistosoma mansoni. Am. J. Trop. Med. Hyg. 1987;37:85–97. doi: 10.4269/ajtmh.1987.37.85. [DOI] [PubMed] [Google Scholar]
- 3.Gause WC, Urban JF, Stadecker MJ. The immune response to parasitic helminths: insights from murine models. Trends Immunol. 2003;24:269–277. doi: 10.1016/s1471-4906(03)00101-7. [DOI] [PubMed] [Google Scholar]
- 4.Pearce EJ, MacDonald AS. The immunobiology of schistosomiasis. Nat.Rev. Immunol. 2002;2:499–511. doi: 10.1038/nri843. [DOI] [PubMed] [Google Scholar]
- 5.Stadecker MJ, Asahi H, Finger E, Hernandez HJ, Rutitzky LI, Sun J. The immunobiology of Th1 polarization in high-pathology schistosomiasis. Immunol. Rev. 2004;201:168–179. doi: 10.1111/j.0105-2896.2004.00197.x. [DOI] [PubMed] [Google Scholar]
- 6.Rutitzky LI, Hernandez HJ, Stadecker MJ. Th1-polarizing immunization with egg antigens correlates with severe exacerbation of immunopathology and death in schistosome infection. Proc. Natl. Acad. Sci. USA. 2001;98:13243–13248. doi: 10.1073/pnas.231258498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Rutitzky LI, da Rosa J. R. Lopes, Stadecker MJ. Severe CD4 T cell-mediated immunopathology in murine schistosomiasis is dependent on IL-12p40 and correlates with high levels of IL-17. J. Immunol. 2005;175:3920–3926. doi: 10.4049/jimmunol.175.6.3920. [DOI] [PubMed] [Google Scholar]
- 8.Rutitzky LI, Bazzone L, Shainheit MG, Joyce-Shaikh B, Cua DJ, Stadecker MJ. IL-23 Is Required for the Development of Severe Egg-Induced Immunopathology in Schistosomiasis and for Lesional Expression of IL-17. J. Immunol. 2008;180:2486–2495. doi: 10.4049/jimmunol.180.4.2486. [DOI] [PubMed] [Google Scholar]
- 9.Langrish CL, McKenzie BS, Wilson NJ, Malefyt R. de Waal, Kastelein RA, Cua DJ. IL-12 and IL-23: master regulators of innate and adaptive immunity. Immunol. Rev. 2004;202:96–105. doi: 10.1111/j.0105-2896.2004.00214.x. [DOI] [PubMed] [Google Scholar]
- 10.Park H, Li Z, Yang XO, Chang SH, Nurieva R, Wang YH, Wang Y, Hood L, Zhu Z, Tian Q, Dong C. A distinct lineage of CD4 T cells regulates tissue inflammation by producing interleukin 17. Nat. Immunol. 2005;6:1133–1141. doi: 10.1038/ni1261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Cua DJ, Sherlock J, Chen Y, Murphy CA, Joyce B, Seymour B, Lucian L, To W, Kwan S, Churakova T, Zurawski S, Wiekowski M, Lira SA, Gorman D, Kastelein RA, Sedgwick JD. Interleukin-23 rather than interleukin-12 is the critical cytokine for autoimmune inflammation of the brain. Nature. 2003;421:744–748. doi: 10.1038/nature01355. [DOI] [PubMed] [Google Scholar]
- 12.Chen Y, Langrish CL, McKenzie B, Joyce-Shaikh B, Stumhofer JS, McClanahan T, Blumenschein W, Churakovsa T, Low J, Presta L, Hunter CA, Kastelein RA, Cua DJ. Anti-IL-23 therapy inhibits multiple inflammatory pathways and ameliorates autoimmune encephalomyelitis. J. Clin. Invest. 2006;116:1317–1326. doi: 10.1172/JCI25308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Murphy CA, Langrish CL, Chen Y, Blumenschein W, McClanahan T, Kastelein RA, Sedgwick JD, Cua DJ. Divergent pro- and antiinflammatory roles for IL-23 and IL-12 in joint autoimmune inflammation. J. Exp. Med. 2003;198:1951–1957. doi: 10.1084/jem.20030896. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Nakae S, Nambu A, Sudo K, Iwakura Y. Suppression of immune induction of collagen-induced arthritis in IL-17-deficient mice. J. Immunol. 2003;171:6173–6177. doi: 10.4049/jimmunol.171.11.6173. [DOI] [PubMed] [Google Scholar]
- 15.Yen D, Cheung J, Scheerens H, Poulet F, McClanahan T, McKenzie B, Kleinschek MA, Owyang A, Mattson J, Blumenschein W, Murphy E, Sathe M, Cua DJ, Kastelein RA, Rennick D. IL-23 is essential for T cell-mediated colitis and promotes inflammation via IL-17 and IL-6. J. Clin. Invest. 2006;116:1310–1316. doi: 10.1172/JCI21404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kullberg MC, Jankovic D, Feng CG, Hue S, Gorelick PL, McKenzie BS, Cua DJ, Powrie F, Cheever AW, Maloy KJ, Sher A. IL-23 plays a key role in Helicobacter hepaticus-induced T cell-dependent colitis. J. Exp. Med. 2006;203:2485–2494. doi: 10.1084/jem.20061082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Mangan PR, Harrington LE, O’Quinn DB, Helms WS, Bullard DC, Elson CO, Hatton RD, Wahl SM, Schoeb TR, Weaver CT. Transforming growth factor-beta induces development of the T(H)17 lineage. Nature. 2006;441:231–234. doi: 10.1038/nature04754. [DOI] [PubMed] [Google Scholar]
- 18.Zelante T, De Luca A, Bonifazi P, Montagnoli C, Bozza S, Moretti S, Belladonna ML, Vacca C, Conte C, Mosci P, Bistoni F, Puccetti P, Kastelein RA, Kopf M, Romani L. IL-23 and the Th17 pathway promote inflammation and impair antifungal immune resistance. Eur. J. Immunol. 2007;37:2695–2706. doi: 10.1002/eji.200737409. [DOI] [PubMed] [Google Scholar]
- 19.Caruso R, Fina D, Paoluzi OA, Blanco G. Del Vecchio, Stolfi C, Rizzo A, Caprioli F, Sarra M, Andrei F, Fantini MC, Macdonald TT, Pallone F, Monteleone G. IL-23-mediated regulation of IL-17 production in Helicobacter pylori-infected gastric mucosa. Eur. J. Immunol. 2008;38:470–478. doi: 10.1002/eji.200737635. [DOI] [PubMed] [Google Scholar]
- 20.Aggarwal S, Ghilardi N, Xie MH, de Sauvage FJ, Gurney AL. Interleukin-23 promotes a distinct CD4 T cell activation state characterized by the production of interleukin-17. J. Biol. Chem. 2003;278:1910–1914. doi: 10.1074/jbc.M207577200. [DOI] [PubMed] [Google Scholar]
- 21.Trinchieri G, Pflanz S, Kastelein RA. The IL-12 family of heterodimeric cytokines: new players in the regulation of T cell responses. Immunity. 2003;19:641–644. doi: 10.1016/s1074-7613(03)00296-6. [DOI] [PubMed] [Google Scholar]
- 22.Brombacher F, Kastelein RA, Alber G. Novel IL-12 family members shed light on the orchestration of Th1 responses. Trends Immunol. 2003;24:207–212. doi: 10.1016/S1471-4906(03)00067-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Veldhoen M, Hocking RJ, Atkins CJ, Locksley RM, Stockinger B. TGFbeta in the context of an inflammatory cytokine milieu supports de novo differentiation of IL-17-producing T cells. Immunity. 2006;24:179–189. doi: 10.1016/j.immuni.2006.01.001. [DOI] [PubMed] [Google Scholar]
- 24.Bettelli E, Carrier Y, Gao W, Korn T, Strom TB, Oukka M, Weiner HL, Kuchroo VK. Reciprocal developmental pathways for the generation of pathogenic effector TH17 and regulatory T cells. Nature. 2006;441:235–238. doi: 10.1038/nature04753. [DOI] [PubMed] [Google Scholar]
- 25.Szabo SJ, Kim ST, Costa GL, Zhang X, Fathman CG, Glimcher LH. A novel transcription factor, T-bet, directs Th1 lineage commitment. Cell. 2000;100:655–669. doi: 10.1016/s0092-8674(00)80702-3. [DOI] [PubMed] [Google Scholar]
- 26.Szabo SJ, Sullivan BM, Stemmann C, Satoskar AR, Sleckman BP, Glimcher LH. Distinct effects of T-bet in TH1 lineage commitment and IFN-gamma production in CD4 and CD8 T cells. Science. 2002;295:338–342. doi: 10.1126/science.1065543. [DOI] [PubMed] [Google Scholar]
- 27.Rangachari M, Mauermann N, Marty RR, Dirnhofer S, Kurrer MO, Komnenovic V, Penninger JM, Eriksson U. T-bet negatively regulates autoimmune myocarditis by suppressing local production of interleukin 17. J. Exp. Med. 2006;203:2009–2019. doi: 10.1084/jem.20052222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Bettelli E, Sullivan B, Szabo SJ, Sobel RA, Glimcher LH, Kuchroo VK. Loss of T-bet, but not STAT1, prevents the development of experimental autoimmune encephalomyelitis. J. Exp. Med. 2004;200:79–87. doi: 10.1084/jem.20031819. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Gocke AR, Cravens PD, Ben LH, Hussain RZ, Northrop SC, Racke MK, Lovett-Racke AE. T-bet regulates the fate of Th1 and Th17 lymphocytes in autoimmunity. J. Immunol. 2007;178:1341–1348. doi: 10.4049/jimmunol.178.3.1341. [DOI] [PubMed] [Google Scholar]
- 30.Gao JL, Sen AI, Kitaura M, Yoshie O, Rothenberg ME, Murphy PM, Luster AD. Identification of a mouse eosinophil receptor for the CC chemokine eotaxin. Biochem. Biophys. Res. Commun. 1996;223:679–684. doi: 10.1006/bbrc.1996.0955. [DOI] [PubMed] [Google Scholar]
- 31.Nagase H, Miyamasu M, Yamaguchi M, Fujisawa T, Kawasaki H, Ohta K, Yamamoto K, Morita Y, Hirai K. Regulation of chemokine receptor expression in eosinophils. Int. Arch. Allergy Immunol. 2001;125(Suppl 1):29–32. doi: 10.1159/000053849. [DOI] [PubMed] [Google Scholar]
- 32.Banchereau J, Briere F, Caux C, Davoust J, Lebecque S, Liu YJ, Pulendran B, Palucka K. Immunobiology of dendritic cells. Annu. Rev. Immunol. 2000;18:767–811. doi: 10.1146/annurev.immunol.18.1.767. [DOI] [PubMed] [Google Scholar]
- 33.Langrish CL, Chen Y, Blumenschein WM, Mattson J, Basham B, Sedgwick JD, McClanahan T, Kastelein RA, Cua DJ. IL-23 drives a pathogenic T cell population that induces autoimmune inflammation. J. Exp. Med. 2005;201:233–240. doi: 10.1084/jem.20041257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Liang SC, Tan XY, Luxenberg DP, Karim R, Dunussi-Joannopoulos K, Collins M, Fouser LA. Interleukin (IL)-22 and IL-17 are coexpressed by Th17 cells and cooperatively enhance expression of antimicrobial peptides. J. Exp. Med. 2006;203:2271–2279. doi: 10.1084/jem.20061308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Goerdt S, Orfanos CE. Other functions, other genes: alternative activation of antigen- presenting cells. Immunity. 1999;10:137–142. doi: 10.1016/s1074-7613(00)80014-x. [DOI] [PubMed] [Google Scholar]
- 36.Anthony RM, Rutitzky LI, Urban JF, Jr., Stadecker MJ, Gause WC. Protective immune mechanisms in helminth infection. Nat. Rev. Immunol. 2007;7:975–987. doi: 10.1038/nri2199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Vignali DA, Collison LW, Workman CJ. How regulatory T cells work. Nat. Rev. Immunol. 2008;8:523–532. doi: 10.1038/nri2343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Herbert DR, Holscher C, Mohrs M, Arendse B, Schwegmann A, Radwanska M, Leeto M, Kirsch R, Hall P, Mossmann H, Claussen B, Forster I, Brombacher F. Alternative macrophage activation is essential for survival during schistosomiasis and downmodulates T helper 1 responses and immunopathology. Immunity. 2004;20:623–635. doi: 10.1016/s1074-7613(04)00107-4. [DOI] [PubMed] [Google Scholar]
- 39.Hesse M, Piccirillo CA, Belkaid Y, Prufer J, Mentink-Kane M, Leusink M, Cheever AW, Shevach EM, Wynn TA. The pathogenesis of schistosomiasis is controlled by cooperating IL-10-producing innate effector and regulatory T cells. J. Immunol. 2004;172:3157–3166. doi: 10.4049/jimmunol.172.5.3157. [DOI] [PubMed] [Google Scholar]
- 40.Taylor JJ, Mohrs M, Pearce EJ. Regulatory T cell responses develop in parallel to Th responses and control the magnitude and phenotype of the Th effector population. J. Immunol. 2006;176:5839–5847. doi: 10.4049/jimmunol.176.10.5839. [DOI] [PubMed] [Google Scholar]
- 41.Raes G, De Baetselier P, Noel W, Beschin A, Brombacher F, Hassanzadeh Gh G. Differential expression of FIZZ1 and Ym1 in alternatively versus classically activated macrophages. J. Leukoc. Biol. 2002;71:597–602. [PubMed] [Google Scholar]
- 42.Nair MG, Cochrane DW, Allen JE. Macrophages in chronic type 2 inflammation have a novel phenotype characterized by the abundant expression of Ym1 and Fizz1 that can be partly replicated in vitro. Immunol. Lett. 2003;85:173–180. doi: 10.1016/s0165-2478(02)00225-0. [DOI] [PubMed] [Google Scholar]
- 43.Loke P, Nair MG, Parkinson J, Guiliano D, Blaxter M, Allen JE. IL-4 dependent alternatively-activated macrophages have a distinctive in vivo gene expression phenotype. BMC Immunol. 2002;3:7. doi: 10.1186/1471-2172-3-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Pedras-Vasconcelos JA, Pearce EJ. Type 1 CD8+ T cell responses during infection with the helminth Schistosoma mansoni. J. Immunol. 1996;157:3046–3053. [PubMed] [Google Scholar]
- 45.Lugo-Villarino G, Maldonado-Lopez R, Possemato R, Penaranda C, Glimcher LH. T-bet is required for optimal production of IFN-gamma and antigen-specific T cell activation by dendritic cells. Proc. Natl. Acad. Sci. U S A. 2003;100:7749–7754. doi: 10.1073/pnas.1332767100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Guo S, Cobb D, Smeltz RB. T-bet inhibits the in vivo differentiation of parasite-specific CD4+ Th17 cells in a T cell-intrinsic manner. J. Immunol. 2009;182:6179–6186. doi: 10.4049/jimmunol.0803821. [DOI] [PubMed] [Google Scholar]
- 47.Laan M, Cui ZH, Hoshino H, Lotvall J, Sjostrand M, Gruenert DC, Skoogh BE, Linden A. Neutrophil recruitment by human IL-17 via C-X-C chemokine release in the airways. J. Immunol. 1999;162:2347–2352. [PubMed] [Google Scholar]
- 48.Witowski J, Pawlaczyk K, Breborowicz A, Scheuren A, Kuzlan-Pawlaczyk M, Wisniewska J, Polubinska A, Friess H, Gahl GM, Frei U, Jorres A. IL-17 stimulates intraperitoneal neutrophil infiltration through the release of GRO alpha chemokine from mesothelial cells. J. Immunol. 2000;165:5814–5821. doi: 10.4049/jimmunol.165.10.5814. [DOI] [PubMed] [Google Scholar]
- 49.Wurster AL, Rodgers VL, Satoskar AR, Whitters MJ, Young DA, Collins M, Grusby MJ. Interleukin 21 is a T helper (Th) cell 2 cytokine that specifically inhibits the differentiation of naive Th cells into interferon gamma-producing Th1 cells. J. Exp. Med. 2002;196:969–977. doi: 10.1084/jem.20020620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Irmler IM, Gajda M, Brauer R. Exacerbation of antigen-induced arthritis in IFN-gamma-deficient mice as a result of unrestricted IL-17 response. J. Immunol. 2007;179:6228–6236. doi: 10.4049/jimmunol.179.9.6228. [DOI] [PubMed] [Google Scholar]
- 51.Chu CQ, Swart D, Alcorn D, Tocker J, Elkon KB. Interferon-gamma regulates susceptibility to collagen-induced arthritis through suppression of interleukin-17. Arthritis Rheum. 2007;56:1145–1151. doi: 10.1002/art.22453. [DOI] [PubMed] [Google Scholar]
- 52.Williams AS, Richards PJ, Thomas E, Carty S, Nowell MA, Goodfellow RM, Dent CM, Williams BD, Jones SA, Topley N. Interferon-gamma protects against the development of structural damage in experimental arthritis by regulating polymorphonuclear neutrophil influx into diseased joints. Arthritis Rheum. 2007;56:2244–2254. doi: 10.1002/art.22732. [DOI] [PubMed] [Google Scholar]
- 53.Wang J, Fathman JW, Lugo-Villarino G, Scimone L, von Andrian U, Dorfman DM, Glimcher LH. Transcription factor T-bet regulates inflammatory arthritis through its function in dendritic cells. J. Clin. Invest. 2006;116:414–421. doi: 10.1172/JCI26631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Juedes AE, Rodrigo E, Togher L, Glimcher LH, von Herrath MG. T-bet controls autoaggressive CD8 lymphocyte responses in type 1 diabetes. J. Exp. Med. 2004;199:1153–1162. doi: 10.1084/jem.20031873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Peng SL, Szabo SJ, Glimcher LH. T-bet regulates IgG class switching and pathogenic autoantibody production. Proc. Natl. Acad. Sci. USA. 2002;99:5545–5550. doi: 10.1073/pnas.082114899. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Neurath MF, Weigmann B, Finotto S, Glickman J, Nieuwenhuis E, Iijima H, Mizoguchi A, Mizoguchi E, Mudter J, Galle PR, Bhan A, Autschbach F, Sullivan BM, Szabo SJ, Glimcher LH, Blumberg RS. The transcription factor T-bet regulates mucosal T cell activation in experimental colitis and Crohn’s disease. J. Exp. Med. 2002;195:1129–1143. doi: 10.1084/jem.20011956. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Kleinschek MA, Owyang AM, Joyce-Shaikh B, Langrish CL, Chen Y, Gorman DM, Blumenschein WM, McClanahan T, Brombacher F, Hurst SD, Kastelein RA, Cua DJ. IL-25 regulates Th17 function in autoimmune inflammation. J. Exp. Med. 2007;204:161–170. doi: 10.1084/jem.20061738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Wong CK, Lit LC, Tam LS, Li EK, Wong PT, Lam CW. Hyperproduction of IL-23 and IL-17 in patients with systemic lupus erythematosus: implications for Th17-mediated inflammation in auto-immunity. Clin. Immunol. 2008;127:385–393. doi: 10.1016/j.clim.2008.01.019. [DOI] [PubMed] [Google Scholar]
- 59.Fujiwara M, Hirose K, Kagami S, Takatori H, Wakashin H, Tamachi T, Watanabe N, Saito Y, Iwamoto I, Nakajima H. T-bet inhibits both TH2 cell-mediated eosinophil recruitment and TH17 cell-mediated neutrophil recruitment into the airways. J. Allergy Clin. Immunol. 2007;119:662–670. doi: 10.1016/j.jaci.2006.12.643. [DOI] [PubMed] [Google Scholar]
- 60.Burrell BE, Csencsits K, Lu G, Grabauskiene S, Bishop DK. CD8+ Th17 mediate costimulation blockade-resistant allograft rejection in T-bet-deficient mice. J. Immunol. 2008;181:3906–3914. doi: 10.4049/jimmunol.181.6.3906. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Yuan X, Paez-Cortez J, Schmitt-Knosalla I, D’Addio F, Mfarrej B, Donnarumma M, Habicht A, Clarkson MR, Iacomini J, Glimcher LH, Sayegh MH, Ansari MJ. A novel role of CD4 Th17 cells in mediating cardiac allograft rejection and vasculopathy. J. Exp. Med. 2008;205:3133–3144. doi: 10.1084/jem.20081937. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Sullivan BM, Jobe O, Lazarevic V, Vasquez K, Bronson R, Glimcher LH, Kramnik I. Increased susceptibility of mice lacking T-bet to infection with Mycobacterium tuberculosis correlates with increased IL-10 and decreased IFN-gamma production. J. Immunol. 2005;175:4593–4602. doi: 10.4049/jimmunol.175.7.4593. [DOI] [PubMed] [Google Scholar]
- 63.Rosas LE, Snider HM, Barbi J, Satoskar AA, Lugo-Villarino G, Keiser T, Papenfuss T, Durbin JE, Radzioch D, Glimcher LH, Satoskar AR. Cutting edge: STAT1 and T-bet play distinct roles in determining outcome of visceral leishmaniasis caused by Leishmania donovani. J. Immunol. 2006;177:22–25. doi: 10.4049/jimmunol.177.1.22. [DOI] [PubMed] [Google Scholar]
- 64.Hultgren OH, Verdrengh M, Tarkowski A. T-box transcription-factor-deficient mice display increased joint pathology and failure of infection control during staphylococcal arthritis. Microbes Infect. 2004;6:529–535. doi: 10.1016/j.micinf.2004.02.005. [DOI] [PubMed] [Google Scholar]
- 65.Ravindran R, Foley J, Stoklasek T, Glimcher LH, McSorley SJ. Expression of T-bet by CD4 T cells is essential for resistance to Salmonella infection. J. Immunol. 2005;175:4603–4610. doi: 10.4049/jimmunol.175.7.4603. [DOI] [PubMed] [Google Scholar]
- 66.Annacker O, Pimenta-Araujo R, Burlen-Defranoux O, Barbosa TC, Cumano A, Bandeira A. CD25+ CD4+ T cells regulate the expansion of peripheral CD4 T cells through the production of IL-10. J. Immunol. 2001;166:3008–3018. doi: 10.4049/jimmunol.166.5.3008. [DOI] [PubMed] [Google Scholar]
- 67.Maloy KJ, Salaun L, Cahill R, Dougan G, Saunders NJ, Powrie F. CD4+CD25+ T(R) cells suppress innate immune pathology through cytokine-dependent mechanisms. J. Exp. Med. 2003;197:111–119. doi: 10.1084/jem.20021345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Villanueva P. O. Flores, Chikunguwo SM, Harris TS, Stadecker MJ. Role of IL-10 on antigen-presenting cell function for schistosomal egg-specific monoclonal T helper cell responses in vitro and in vivo. J. Immunol. 1993;151:3192–3198. [PubMed] [Google Scholar]
- 69.Flores-Villanueva PO, Zheng XX, Strom TB, Stadecker MJ. Recombinant IL-10 and IL-10/Fc treatment down-regulate egg antigen-specific delayed hypersensitivity reactions and egg granuloma formation in schistosomiasis. J. Immunol. 1996;156:3315–3320. [PubMed] [Google Scholar]
- 70.Boros D, Warren K. Delayed hypersensitivity-type granuloma formation and dermal reaction induced and elicited by a soluble factor isolated from schistosoma mansoni soluble eggs. J. Exp. Med. 1970;132:488–507. doi: 10.1084/jem.132.3.488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Rutitzky LI, Mirkin GA, Stadecker MJ. Apoptosis by neglect of CD4+ Th cells in granulomas: a novel effector mechanism involved in the control of egg-induced immunopathology in murine schistosomiasis. J. Immunol. 2003;171:1859–1867. doi: 10.4049/jimmunol.171.4.1859. [DOI] [PubMed] [Google Scholar]