Abstract
Several candidate gene studies have provided evidence for a role of host genetics in susceptibility to tuberculosis (TB). However, the results of these studies have been very inconsistent, even within a study population. Here, we review the design of these studies from a genetic epidemiological perspective, illustrating important differences in phenotype definition in both cases and controls, consideration of latent M. tuberculosis infection versus active TB disease, population genetic factors such as population substructure and linkage disequilibrium, polymorphism selection, and potential global differences in M. tuberculosis strain. These considerable differences between studies should be accounted for when examining the current literature. Recommendations are made for future studies to further clarify the host genetics of TB.
Introduction
Tuberculosis (TB), caused by Mycobacterium tuberculosis (Mtb), is a growing public health problem in the era of the HIV/AIDS pandemic. Among the one-third of the world infected by Mtb [1], almost 8 million new cases of TB occur annually, with 2 million deaths attributed to the disease each year. Only 10% of those individuals infected by Mtb go on to develop clinical disease, and disease presentation itself is heterogeneous, suggesting that host factors play a large role in disease susceptibility and natural history. An increased understanding of the host response to Mtb will facilitate the development of new vaccines and therapeutics [2].
Several studies have suggested a role for host genetics in TB susceptibility. Support for genetic susceptibility to TB in humans was first provided by twin studies [3], [4], animal models [5]–[8], then later segregation analyses [9], [10]. Countless candidate gene studies have been conducted, as well as seven genome-wide linkage scans [11]–[17]. However, there is a great deal of inconsistency across these studies. Among studies of any candidate gene, there are always several reports that provide both positive and negative evidence for an association with TB. Within genome scans, there has been replication of some results across two of the studies [14], [15], but there is very little replication across the remaining papers.
There are a number of key components of the design of these studies that may explain the inconsistency in the literature. The objective of this review is to discuss these issues, illustrated with examples from the TB genetics literature, and propose some approaches for taking a more thorough approach to the study of TB genetics.
Impact of Study Design
Phenotype Definition
The first step in any epidemiological study is to define the criteria used to diagnose disease. Then, one must define what is meant by non-diseased individuals (“controls”). In TB, this is complicated, because the pathogenesis of TB can be thought of as a two-stage process [18]. The first stage consists of latent Mtb infection (LTBI), in which Mtb establishes a productive infection but does not produce symptoms. LTBI is diagnosed by a positive tuberculin skin test (TST) and/or positive interferon-γ response assay (IGRA) in the absence of clinical signs and symptoms of full-blown disease [19], [20]. Definitive diagnosis of pulmonary TB requires the recovery of Mtb from sputum and cultivation in culture or detection of acid-fast bacilli (AFB) on smear [19], [21]. Studies have shown that AFB smear is less sensitive than culture, and that AFB smear grade could reflect differences in disease severity [21]. Smear-negative, culture-positive TB is also a problem in developing countries [21]. Thus, the method used to diagnose TB could affect the comparability of studies, and these differences could reflect variation in disease severity or even potential misclassification of disease status, generating a significant impact on the type I and type II error of studies. Here, we will first review the various diagnostic criteria used for TB disease, then the clinical characterization of study controls, and how these differences in study design may affect the interpretation of results across studies.
As stated by Möller and colleagues [22], studies of TB are “exquisitely sensitive to phenotype definition”. Different criteria have been used to diagnose TB in different study sites. Here, we focus on studies of the NRAMP1 (SLC11A1) gene, which has been studied most extensively (Table 1). To summarize, some studies have used the gold standard definition for TB diagnosis based on growth of Mtb in culture [19], though other studies only diagnosed TB patients based on positive AFB smear. Some studies had heterogeneous diagnostic criteria, classifying together cases diagnosed by smear or culture or symptoms. Other studies have combined pulmonary and extrapulmonary TB cases in the analysis [23]–[27]. Notice that of the 12 studies demonstrating an association between NRAMP1 and TB, only four used culture positivity as their diagnosis method. Could these differences in diagnostic criteria disguise differences in disease severity across populations?
Table 1. Summary of TB association genetic studies of NRAMP1/SLC11A1, including TB diagnostic criteria, characterization of controls, and whether there was an association with any SNP in the gene.
| Population (Reference) | TB Diagnostic Criteria | Characterization of Controls | Association? |
| Gambia [80] | Smear + | Healthy blood donors | Yes |
| Gambia [81] | Smear + | Healthy blood donors | |
| Malawi [82] | Smear + OR culture + OR histology | Unrelated with no history of infectious disease | Yes |
| Morocco [37] | Culture + | Healthy family members | |
| Tanzania [83] | Culture + | Blood donors | Yes |
| Guinea [36] | Microscopy (smear +? Culture +?) | Unaffected relatives | |
| South Africa [32] | Smear + OR culture + | Unrelated healthy | Yes |
| Caucasian and African American [26] | Culture + OR past diagnosis | Household members in close contact | Yes |
| Caucasian [84] | Culture + OR response to TB treatment | Clinic patients without infectious disease | Yes |
| Caucasian, African American, and Asian [27] | Culture + | Tuberculin skin test positive | |
| Cambodia [85] | Smear + | Hospital/clinic patients | Yes |
| China [86] | Smear + OR culture + OR symptoms and radiological evidence; males only | Unrelated healthy males | Yes |
| Japan [87] | Smear + OR culture + | No history of TB disease | Yes |
| Japan [88] | Smear + | Random clinic patients | Yes |
| Taiwanese [89] | Culture + | Clinic patients without pulmonary disease | |
| Japan [90] | Smear + | Healthy blood donors without history of pulmonary or inflammatory disease | |
| Thai [91] | Culture + | Healthy blood bank donors | |
| China [92] | Culture + | Hospital patients and healthy blood donors | Yes |
| Korea [93] | Culture + (unclear) | No history of TB disease | Yes |
| Japan [94] | Smear + OR culture + | Unrelated healthy | |
| Poland [38] | Culture + | TST negative |
Smear + refers to AFB smear positive. “Culture +” could include more stringent definitions such as culture positive, smear positive, and radiological evidence consistent with TB.
This table is limited to studies published in English so that case and control definitions could be determined. It is also limited to studies of pulmonary TB in all age groups.
Related to this is the definition of controls. It is unknown in many of these studies whether or not the “controls” were latently infected with Mtb, as evidenced by either a TST or IGRA. Recent studies have suggested some genes may actually be related to LTBI and not progression to TB [15], [28], [29], while other studies have suggested some genes may differentiate between LTBI and active TB disease [30], [31]. This is important in truly understanding the role of these genes in disease pathogenesis and progression. If controls are latently infected, and there is an association seen between a gene and TB, that suggests the gene influences progression from LTBI to TB. However, if controls are uninfected, it is unclear whether an association implies susceptibility for developing active disease or just acquisition of LTBI.
Finally, the selection of controls is not trivial. In a case-control study, controls should be similar to cases in every way possible except for the presence of disease. In studies of TB, this means controls should be exposed to infectious TB cases, so that they have the opportunity to acquire infection and then progress to active TB disease. Some studies conducted in TB-endemic settings assume all individuals are exposed to TB [25], [32]. However, studies have shown individuals may be persistently exposed to Mtb but never develop LTBI [15], [19]. Characterization of controls in TB genetics studies has differed widely (examples in Table 1). Many studies have utilized population controls, similar to the approach taken in recent large genome-wide association studies (GWAS) [33], i.e., by using blood bank donors. The disadvantage of this design is possible misclassification bias [34]—the chance that some of these “controls” may never become affected for TB, which is problematic when the disease is common [35]. By contrast, other studies have utilized unaffected household members [26], [31], [36], [37] or have conducted thorough clinical evaluation with TST in those without disease [27], [30], [38]; in these situations, exposure in unaffected individuals is known, so these are true controls in the epidemiological sense. Note that only one of the NRAMP1 associations was observed in studies where exposure has been quantified (Table 1).
Epidemiological Study Design
The vast majority of genetic epidemiological studies, not just for TB but for other complex traits as well, tend to be case-control studies. Such studies are easier to conduct because they do not require cooperation of the entire family, and a greater number of cases can be recruited. One major advantage of family-based designs for the study of infectious diseases is the characterization of exposure in the “controls”, as discussed above. Individuals living in the same household have a high likelihood of exposure to an infectious TB case, thereby influencing the probability that they too will develop TB [39]–[41]. As described above, epidemiological characterization of exposure is important in order to construct a valid case-control study.
Another advantage of family-based studies is the ability to account for population substructure. Hidden population stratification may result in bias (false positive results) [42] or false negative results [43]. Studies of TB genetics have been conducted in many admixed populations, including African Americans [26], [27], [44]–[46], Mexicans [30], and South African “Coloureds” [11], [14], [32], [47], [48]. Some of these studies [11], [26], [45], [46] have employed family-based designs. Other studies have examined potential population substructure by analyzing genomic control markers: one study in South Africa utilized ∼25 markers [47], [48], and another study utilized >200 markers [49]. Marchini et al. [43] point out genomic control markers will not adequately correct for population substructure if too few markers are used, but it is difficult to enumerate a sufficient number of markers in populations of African descent. It is unclear if other studies were able to account for population substructure. It may be impossible for existing study cohorts to incorporate family-based designs or retrospectively evaluate population stratification, but this clearly may explain some of the heterogeneity among studies.
Population Differences—More Than Just Geography
A typical explanation for differing results by population is population differentiation [22], [50], including genetic heterogeneity or inestimable polygenic effects. Another important genetic difference between populations is in linkage disequilibrium (LD).
Early studies of TB genetics were restricted to well-characterized markers within genes (studies of SLC11A1/NRAMP1 in Table 1 are examples). Often these markers were exonic or restriction fragment length polymorphisms. The underlying assumption of the power and design of such studies is that the polymorphism being analyzed is the causal polymorphism.
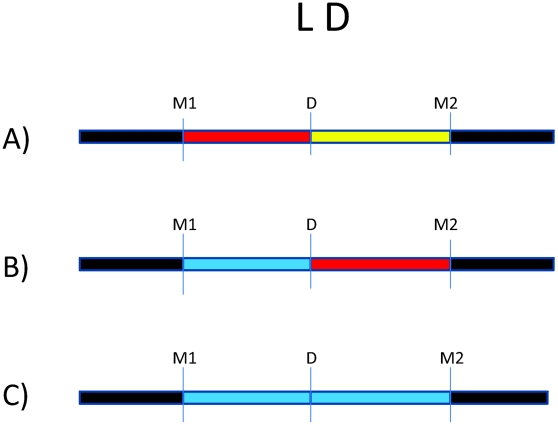
There are millions of single nucleotide polymorphisms (SNPs) throughout the genome [51], [52]. Because of the LD structure in the genome, certain SNPs can be used to “tag” haplotypes, such that one or a few SNPs capture information about LD structure [53]. Many trait-associated SNPs (>40%) are intergenic or intronic, suggesting an important role for non-coding SNPs in complex disease [54]. This serves as a reminder that disease risk alleles may actually be in LD with genotyped markers, which serve as “tags” for haplotypes on which the causal allele may reside. This is illustrated by Figure 1, where we consider an underlying disease allele that is not directly genotyped but surrounded by flanking markers. The ability to detect association with the region where the disease allele resides depends entirely on the strength of LD between the unobserved risk allele and flanking markers. As patterns of LD differ between study populations, the specific trait-associated SNPs will consequently differ.
Figure 1. Impact of variation in linkage disequilibrium (LD) in detection of disease risk alleles.
For all three scenarios, D is the underlying disease risk allele. (A) There is strong LD between D and marker #1 (M1), and weak LD between D and M2. In this situation, association will be detected with M1, depending on study power based on sample size, strength of genetic effect, and minor allele frequencies. (B) There is no LD between M1 and D but strong LD between M2 and D. Here, association will be detected only with M2 (again, depending on power). (C) There is weak LD throughout the region. Association will likely not be detected.
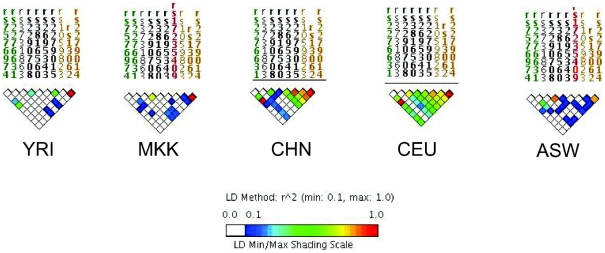
The impact of LD differences between study populations is further illustrated in Figure 2. Here, LD patterns in NRAMP1 were plotted using HapMap reference populations representative of those populations where NRAMP1 has been studied: Caucasians in Utah, United States (CEU), Yoruba in Nigeria (YRI), Maasai in Kenya (MKK), Han Chinese (CHN), and African Americans in the US Southwest (ASW). These LD plots were generated using default parameters in the Genome Variation Server (http://gvs.gs.washington.edu/GVS/), with no minor allele frequency cutoff. African populations (YRI and MKK) have very little LD because they are older populations, and their LD patterns differ. Newer populations (CEU and CHN) have much greater LD, and recently admixed populations (ASW) also exhibit LD between SNPs, but there are differences. Also note that the SNPs themselves (rs numbers) differ between populations, illustrating how different polymorphisms exist within the same genes across world populations. A perfect illustration of this phenomenon is provided by Velez et al. [26], who analyzed a number of SNPs within NRAMP1. Though they did not observe statistical association with the markers that were examined in early studies, they did observe association with intronic and exonic SNPs. If they had not conducted such extensive genotyping, they may have missed these associations.
Figure 2. Linkage disequilibrium (LD) of the NRAMP1 gene for HapMap reference populations.
Yoruba (YRI), Maasai (MKK), Han Chinese (CHN), Utah Caucasians (CEU), and African Americans (ASW) are shown. The strength of LD is illustrated using the color scale shown in the figure key.
Only a few other studies have accounted for global variations in LD by analyzing several SNPs within candidate genes of interest. Some studies have selected tag SNPs based on relevant HapMap reference populations [26], [28], [31], [46]. Other studies have sequenced genes of interest first to identify novel SNPs within the gene(s), then analyzed association with those SNPs [55]–[58]. Though other studies did not utilize LD in their selection of SNPs, they later estimated LD between markers in their dataset, and used this analysis to guide haplotype analysis [48], [49]. Since LD patterns differ by population, it should not be surprising that genetic association results differ, especially given the limited number of markers analyzed per gene. There are many implications of this variation. Differences in the strength of LD between the actual disease locus and genotyped markers will affect the power to detect association to markers (Figure 1). In populations with weaker LD such as African populations, denser SNP observed maps are necessary to detect association effects with untyped disease loci. Thus, variation in number of polymorphisms analyzed, differences in LD in the reference population, and existence of still-unknown risk alleles all complicate replication across studies.
Another controversial issue is the study of common versus rare genetic variants. The common disease–common variant (CDCV) hypothesis posits that genetic risk for common diseases will often be due to common risk alleles [59]. This is in contrast to the common disease rare variant (CDRV) hypothesis, which states that a significant proportion of common chronic diseases are influenced by the summation of effects of multiple low frequency variants in the same gene, where tagging SNPs will not be useful in identifying a single haplotype because no single haplotype exists [60]. Most candidate gene studies assume the CDCV hypothesis. Recent sequencing studies [61], [62] have detected rare SNPs in the TLR family of genes; these could be important, but massive studies will be needed in order to detect disease associations at a statistically significant threshold. In addition, copy number variants (CNVs) have recently attracted attention in their association with complex traits, such as HIV acquisition and progression and autoimmune diseases [63]. These are also considered rare variants, so we are again faced with all of the challenges of testing the CDRV hypothesis.
The above discussion focuses on population genetics of humans. Another related issue is variation in Mtb strains. Researchers have categorized Mtb into six main bacterial strain lineages that are associated with particular geographical regions [64], as well as differences in clinical presentation [65] and rate of progression to active TB disease [66]. So, not only do different diagnostic criteria, as discussed above, potentially reflect differences in disease severity, but specific Mtb strains may also influence disease severity. A recent study suggests a host genotype x Mtb genotype interaction, whereby the TLR2 genotype is associated with TB caused by the Beijing strain [67]. Very few studies have the capacity to examine this potential host by Mtb interaction, but it could easily be a potential explanation for differences between studies.
Complex Genetic Effects
Complex traits such as TB are likely influenced by several factors, including gene–gene interaction and gene–environment interaction. Few studies have investigated gene-gene interactions in the context of human TB. Many gene products (e.g., Toll-like receptors [TLRs]) are known to interact biologically [68], and interaction effects have been demonstrated in mouse models of TB [69]. A recent study identified interactions between the NOS2A gene and IFNGR1 and TLR4 [45]. Interestingly, both IFNGR1 and TLR4 showed no evidence of significant main effects in this analysis. Another study by the same research group found interaction between NRAMP1 and TLR2, but TLR2 did not itself have a significant main effect [26]. This suggests many important genes may influence TB in combination with other genes, but this could be overlooked because their individual effects did not meet criteria for statistical significance. Motsinger-Reif et al. used multifactor dimensionality reduction to identify a potential gene–gene interaction between TLR4 and the TNF-α gene (TNF) [70]. In addition, it is well known that HIV influences the pathogenesis of TB, but most genetic epidemiological studies have been restricted to HIV seronegative individuals. Our work [31] showed an interaction between HIV and the TNF receptor 1 gene. Because many studies have excluded HIV-positive individuals, this hypothesis remains relatively unexplored. Similar to the TNF-α pathway, the type I and II interferon pathways have been associated with both TB and HIV pathogenesis [71], and so should also be considered for future studies of gene–HIV interactions. The challenge of examining interaction effects is the requirement of even larger sample sizes, as discussed by Velez et al. [45].
Conclusions, Recommendations, and Future Directions
As reviewed recently by Möller et al. [22], the body of work showing statistical associations between candidate genes and TB continues to grow. This does not include potential unpublished studies that failed to find significant associations and are not readily available due to publication bias [22]. Even in the published body of literature, however, there is a great deal of inconsistency between marker-trait associations, so we are far from reaching a consensus regarding genes involved in TB risk.
This review focused on methodological reasons for inconsistency across studies. One important factor is the diagnostic criteria for TB disease, which have differed dramatically across studies. Resources available for TB diagnosis differ by country, which is confounded when there has been conflict [72]. Differences in diagnostic criteria across studies can reflect differences in TB severity and may lead to misclassification of cases as controls; this would have a significant impact on the type I and type II error of studies. It is impossible to standardize the diagnostic definitions used across all study sites, but researchers should be mindful of such differences when interpreting their findings. We strongly recommend that researchers characterize the level of exposure to Mtb in individuals without disease, which should include TST/IGRA and careful epidemiological characterization. New studies could utilize the household contact design, which facilitates the characterization of all stages of Mtb exposure, infection, and disease [41]. When the household contact study design is not feasible, spousal controls are also ideal because of persistent and prolonged exposure.
Recall that TB follows two stages of pathogenesis, and LTBI precedes TB disease. Recent studies suggest that LTBI may have unique genetic influences [15], [28], [29]. Persons with LTBI constitute a major impediment to TB control efforts [73]. Since many ongoing vaccine development efforts will focus either preventing LTBI or progression to TB, it is important to understand host factors that influence containment of Mtb infection. However, the study of the genetics of LTBI is also not trivial. Indication of T cell memory response via positive TST and/or IGRA does not necessarily imply the presence of viable Mtb bacilli. In the US as well as other public health systems, individuals with positive TST are treated as though there are viable organisms present, adding further confusion to this phenotype. According to Parrish et al., there is a 2%–23% lifetime probability of developing TB after acquisition of Mtb infection (LTBI) [73]. This illustrates the heterogeneity in this clinical group, since the risk of progression to active TB may depend on a variety of known and unknown risk factors. Furthermore, prophylaxis of LTBI with isoniazid (INH) is the standard of care in many research settings, so that many individuals with “LTBI” based on positive TST/IGRA, genetically predisposed to develop TB, may not. One way to investigate the role of host genetics in LTBI would be to compare TST (or IGRA) positive individuals that develop incident TB to those that do not. Ideally, such a study would not include individuals on INH prophylaxis, though that is unethical in many settings. For these reasons, some may argue that it is more relevant to study TB genetics, and not LTBI, from a public health standpoint.
Thus, it is essential to take a multidisciplinary approach [74] to develop an all-encompassing picture of the natural history of Mtb infection and disease. Few studies have examined the genetics of TB immunology [15], [31], [75]–[77]. Gene expression studies using microarrays may also shed light on host responses to Mtb [78]. Proteomic studies will further elucidate host factors involved in pathogenesis. These various approaches should be analyzed together to hopefully identify more meaningful clinical groups. For example, genomic, proteomic, and immunologic data, collectively, may better capture the heterogeneity in latently infected individuals.
Additional complicating factors in comparing geographically diverse studies are potential population substructure and LD differences among populations. We recommend that future studies analyze enough SNPs to capture LD in their study population. Analyses of a few markers within a gene no longer advance the field, particularly in light of LD differences between populations. Even with advances in genotyping, many studies of “old” markers continue to be published. The choice of a reference population for tag SNP selection is not trivial [62]; thus, dense SNP mapping may be necessary, particularly in studies of African populations. If it is impossible to rigorously examine genes in this way, publishing the LD patterns in the study data [28], [45], [48], [49] is a good start. Furthermore, studies in admixed populations should attempt to examine population substructure to minimize this source of bias. Populations also differ in the Mtb strain lineage that caused TB; future studies examining host gene by Mtb gene interaction are warranted. Finally, as in all genetic epidemiological studies of complex traits, genes may act in complex ways. Genes may interact with other genes and/or epidemiological factors; these potential relationships should not be overlooked. Furthermore, too many researchers (authors and journal reviewers alike) focus too much on p-values. All p-values must be reported, even if greater than 0.05. Markers with p-values greater than 0.05 may still be important in their interaction with other markers or environmental factors. Researchers should collect sufficient data to explore these meaningful biological effects.
There are GWAS of TB forthcoming. Given the issues discussed in this review, we must interpret the findings of those GWAS cautiously. Will these studies be underpowered due to the heterogeneity among TB cases and controls? A recent summary analysis of published GWAS found the reported SNP–trait associations attaining significance (p<10−5) had a median odds ratio of 1.33, with an interquartile range of 1.20–1.61 [54]; thus, the effect sizes of SNPs identified through GWAS are relatively small. Furthermore, the proportion of heritability explained by these variants ranges between 1% and 50% [79]. TB GWAS may provide new clues into the host biology of TB pathogenesis, but the overall clinical relevance of these SNPs will be limited. In addition, GWAS of other complex traits have often merged data across ongoing research studies. Because of the dramatic heterogeneity among studies described in this review, meta-analyses of TB genetic association studies should be conducted with care.
In sum, we have barely scratched the surface in understanding the genetic determinants of TB pathogenesis. Because of the significant public health impact of TB, additional studies are necessary, and should be multidisciplinary in nature. Future studies should carefully consider phenotype definition and genetic epidemiological principles when designing, analyzing, and interpreting findings. Ideally, culture confirmation for pulmonary TB should be conducted where feasible, thorough epidemiological data should be collected in individuals without TB to better understand LTBI and risk of progression to TB, and population genetic factors should be carefully characterized and considered in the analysis.
Accession Numbers for Genes Mentioned in This Paper (GeneIDs from EntrezGene)
TLR2 (7097); SLC11A1, aka NRAMP1 (6556); IFNGR1 (3459); TLR4 (7099); TNF (7124); TNFSF1A, aka TNF receptor 1 (7132); NOS2A (4843).
Acknowledgments
Thank you to Drs. Thomas Hawn and W. Henry Boom for helpful discussion. Thank you also to two anonymous reviewers, whose suggestions and challenges greatly strengthened this manuscript.
Footnotes
The author has declared that no competing interests exist.
Our research is supported in part by the National Institutes of Health grants R01HL096811 from NHLBI, Tuberculosis Research Unit (grant N01-AI95383 and HHSN266200700022C/N01-AI70022 from NIAID), and Resource Grant RR03655 from the NCRR. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.Raviglione M, Snider D, Kochi A. Global epidemiology of tuberculosis: morbidity and mortality of a worldwide epidemic. JAMA. 1995;273:220–226. [PubMed] [Google Scholar]
- 2.Kaufmann SH, Baumann S, Nasser EA. Exploiting immunology and molecular genetics for rational vaccine design against tuberculosis. Int J Tuberc Lung Dis. 2006;10:1068–1079. [PubMed] [Google Scholar]
- 3.Comstock G. Tuberculosis in twins: a re-analysis of the Prophit Study. Am Rev Resp Dis. 1978;117:621–624. doi: 10.1164/arrd.1978.117.4.621. [DOI] [PubMed] [Google Scholar]
- 4.Kallmann F, Reisner D. Twin studies on the significance of genetic factors in tuberculosis. Am Rev Tuberculosis. 1943;47:549–574. [Google Scholar]
- 5.Blackwell J, Barton C, White J, Searle S, Baker A, Williams H, Shaw M. Genomic organizaton and sequence of the human NRAMP gene: identification and mapping of a promotor region polymorphism. Mol Med. 2004;1:194–205. [PMC free article] [PubMed] [Google Scholar]
- 6.Flynn J, Goldstein M, Chan J, Triebold K, Pfeffer K, Lowenstein C, Schreiber R, Mak T, Bloom B. Tumor necrosis factor-alpha is required in the protective immune response against Mycobacterium tuberculosis in mice. Immunity. 1995;2:561–572. doi: 10.1016/1074-7613(95)90001-2. [DOI] [PubMed] [Google Scholar]
- 7.Kramnik I, Dietrick W, Demant P, Bloom B. Genetic control of resistance to experimental infection with virulent Mycobacterium tuberculosis. Proc Natl Acad Sci. 2000;97:8560–8565. doi: 10.1073/pnas.150227197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lurie M. Heredity, constitution and tuberculosis: An experimental study. Am Rev Tuberc. 1941;44:1–125. [Google Scholar]
- 9.Shaw MA, Collins A, Peacock CS, Miller EN, Black GF, Sibthorpe D, Lins-Lainson Z, Shaw JJ, Ramos F, Silveira F, Blackwell JM. Evidence that genetic susceptibility to Mycobacterium tuberculosis in a Brazilian population is under oligogenic control: linkage study of the candidate genes NRAMP1 and TNFA. Tuberc Lung Dis. 1997;78:35–45. doi: 10.1016/s0962-8479(97)90014-9. [DOI] [PubMed] [Google Scholar]
- 10.Stein CM, Nshuti L, Chiunda AB, Boom WH, Elston RC, Mugerwa RD, Iyengar SK, Whalen CC. Evidence for a major gene influence on tumor necrosis factor-alpha expression in tuberculosis: path and segregation analysis. Hum Hered. 2005;60:109–118. doi: 10.1159/000088913. [DOI] [PubMed] [Google Scholar]
- 11.Bellamy R, Beyers N, McAdam K, Ruwende C, Gie R, Samaai P, Bester D, Meyer M, Corrah T, Collin M, Camidge D, Wilkinson D, Hoal-van Helden E, Whittle H, Amos W, van Helden P, Hill A. Genetic susceptibility to tuberculosis in Africans: A genome-wide scan. Proc Natl Acad Sci. 2000;97:8005–8009. doi: 10.1073/pnas.140201897. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Jamieson S, Miller E, Black G, Peacock C, Cordell H, Howson J, Shaw M, Burgner D, Xu W, Lins-Lainson Z, Ramos F, Silveira F, Blackwell J. Evidence for a cluster of genes on chromosome 17q11-q21 controlling susceptibility to tuberculosis and leprosy in Brazilians. Genes and Immunity. 2004;5:46–57. doi: 10.1038/sj.gene.6364029. [DOI] [PubMed] [Google Scholar]
- 13.Miller E, Jamieson S, Joberty C, Fakiola M, Hudson D, Peacock C, Cordell H, Shaw M, Lins-Lainson Z, Ramos F, Silveira F, Blackwell J. Genome-wide scans for leprosy and tuberculosis susceptibility genes in Brazilians. Genes Immun. 2004;5:63–67. doi: 10.1038/sj.gene.6364031. [DOI] [PubMed] [Google Scholar]
- 14.Cooke GS, Campbell SJ, Bennett S, Lienhardt C, McAdam KP, Sow O, Gustafson P, Mwangulu F, van HP, Fine P, Hoal EG, Hill AV. Mapping of a Novel Susceptibility Locus Suggests a Role for MC3R and CTSZ in Human Tuberculosis. Am J Respir Crit Care Med. 2008;178:203–207. doi: 10.1164/rccm.200710-1554OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Stein CM, Zalwango S, Malone LL, Won S, Mayanja-Kizza H, Mugerwa RD, Leontiev DV, Thompson CL, Cartier KC, Elston RC, Iyengar SK, Boom WH, Whalen CC. Genome scan of M. tuberculosis infection and disease in Ugandans. PLoS ONE. 2008;3:e4094. doi: 10.1371/journal.pone.0004094. doi: 10.1371/journal.pone.0004094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Baghdadi JE, Orlova M, Alter A, Ranque B, Chentoufi M, Lazrak F, Archane MI, Casanova JL, Benslimane A, Schurr E, Abel L. An autosomal dominant major gene confers predisposition to pulmonary tuberculosis in adults. J Exp Med. 2006;203:1679–1684. doi: 10.1084/jem.20060269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Mahasirimongkol S, Yanai H, Nishida N, Ridruechai C, Matsushita I, Ohashi J, Summanapan S, Yamada N, Moolphate S, Chuchotaworn C, Chaiprasert A, Manosuthi W, Kantipong P, Kanitwittaya S, Sura T, Khusmith S, Tokunaga K, Sawanpanyalert P, Keicho N. Genome-wide SNP-based linkage analysis of tuberculosis in Thais. Genes Immun. 2009;10:77–83. doi: 10.1038/gene.2008.81. [DOI] [PubMed] [Google Scholar]
- 18.Comstock G. Epidemiology of tuberculosis. Am Rev Resp Dis. 1982;125:8–15. doi: 10.1164/arrd.1982.125.3P2.8. [DOI] [PubMed] [Google Scholar]
- 19.[No authors listed] Diagnostic Standards and Classification of Tuberculosis in Adults and Children. This official statement of the American Thoracic Society and the Centers for Disease Control and Prevention was adopted by the ATS Board of Directors, July 1999. This statement was endorsed by the Council of the Infectious Disease Society of America, September 1999. Am J Respir Crit Care Med. 2000;161:1376–1395. doi: 10.1164/ajrccm.161.4.16141. [DOI] [PubMed] [Google Scholar]
- 20.Nyendak M, Lewinsohn DA, Lewinsohn D. The use of interferon-gamma release assays in clinical practice. In: Davies P, Barnes PF, Gordon SB, editors. Clinical tuberculosis. London: Hodder Arnold; 2008. [Google Scholar]
- 21.Garay S. Pulmonary tuberculosis. In: Rom WN, Garay SM, editors. Tuberculosis. Philadelphia: Lippincott Williams & Wilkins; 2004. pp. 345–394. [Google Scholar]
- 22.Moller M, de Wit E, Hoal EG. Past, present and future directions in human genetic susceptibility to tuberculosis. FEMS Immunol Med Microbiol. 2010;58:3–26. doi: 10.1111/j.1574-695X.2009.00600.x. [DOI] [PubMed] [Google Scholar]
- 23.Ma X, Reich R, Wright J, Tooker H, Teeter L, Musser J, Graviss E. Association between Interleukin-8 gene alleles and human susceptbility to tuberculosis disease. J Infect Dis. 2003;188:349–355. doi: 10.1086/376559. [DOI] [PubMed] [Google Scholar]
- 24.Rossouw M, Nel HJ, Cooke GS, van Helden PD, Hoal EG. Association between tuberculosis and a polymorphic NFκB binding site in the interferon γ gene. Lancet. 2003;361:1871–1872. doi: 10.1016/S0140-6736(03)13491-5. [DOI] [PubMed] [Google Scholar]
- 25.Taype CA, Castro JC, Accinelli RA, Herrera-Velit P, Shaw MA, Espinoza JR. Association between SLC11A1 polymorphisms and susceptibility to different clinical forms of tuberculosis in the Peruvian population. Infect Genet Evol. 2006;6:361–367. doi: 10.1016/j.meegid.2006.01.002. [DOI] [PubMed] [Google Scholar]
- 26.Velez DR, Hulme WF, Myers JL, Stryjewski ME, Abbate E, Estevan R, Patillo SG, Gilbert JR, Hamilton CD, Scott WK. Association of SLC11A1 with tuberculosis and interactions with NOS2A and TLR2 in African-Americans and Caucasians. Int J Tuberc Lung Dis. 2009;13:1068–1076. [PMC free article] [PubMed] [Google Scholar]
- 27.Motsinger-Reif AA, Antas PR, Oki NO, Levy S, Holland SM, Sterling TR. Polymorphisms in IL-1beta, vitamin D receptor Fok1, and Toll-like receptor 2 are associated with extrapulmonary tuberculosis. BMC Med Genet. 2010;11:37. doi: 10.1186/1471-2350-11-37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Thye T, Browne EN, Chinbuah MA, Gyapong J, Osei I, Owusu-Dabo E, Brattig NW, Niemann S, Rusch-Gerdes S, Horstmann RD, Meyer CG. IL10 haplotype associated with tuberculin skin test response but not with pulmonary TB. PLoS ONE. 2009;4:e5420. doi: 10.1371/journal.pone.0005420. doi: 10.1371/journal.pone.0005420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Cobat A, Gallant CJ, Simkin L, Black GF, Stanley K, Hughes J, Doherty TM, Hanekom WA, Eley B, Jais JP, Boland-Auge A, van HP, Casanova JL, Abel L, Hoal EG, Schurr E, Alcais A. Two loci control tuberculin skin test reactivity in an area hyperendemic for tuberculosis. J Exp Med. 2009;206:2583–2591. doi: 10.1084/jem.20090892. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Flores-Villanueva PO, Ruiz-Morales JA, Song CH, Flores LM, Jo EK, Montano M, Barnes PF, Selman M, Granados J. A functional promoter polymorphism in monocyte chemoattractant protein-1 is associated with increased susceptibility to pulmonary tuberculosis. J Exp Med. 2005;202:1649–1658. doi: 10.1084/jem.20050126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Stein CM, Zalwango S, Chiunda AB, Millard C, Leontiev DV, Horvath AL, Cartier KC, Chervenak K, Boom WH, Elston RC, Mugerwa RD, Whalen CC, Iyengar SK. Linkage and association analysis of candidate genes for TB and TNFalpha cytokine expression: evidence for association with IFNGR1, IL-10, and TNF receptor 1 genes. Hum Genet. 2007;121:663–673. doi: 10.1007/s00439-007-0357-8. [DOI] [PubMed] [Google Scholar]
- 32.Hoal EG, Lewis LA, Jamieson SE, Tanzer F, Rossouw M, Victor T, Hillerman R, Beyers N, Blackwell JM, Van Helden PD. SLC11A1 (NRAMP1) but not SLC11A2 (NRAMP2) polymorphisms are associated with susceptibility to tuberculosis in a high-incidence community in South Africa. Int J Tuberc Lung Dis. 2004;8:1464–1471. [PubMed] [Google Scholar]
- 33.Genome-wide association study of 14,000 cases of seven common diseases and 3,000 shared controls. Nature. 2007;447:661–678. doi: 10.1038/nature05911. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Edwards BJ, Haynes C, Levenstien MA, Finch SJ, Gordon D. Power and sample size calculations in the presence of phenotype errors for case/control genetic association studies. BMC Genet. 2005;6:18. doi: 10.1186/1471-2156-6-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.McCarthy MI, Abecasis GR, Cardon LR, Goldstein DB, Little J, Ioannidis JPA, Hirschhorn JN. Genome-wide association studies for complex traits: consensus, uncertainty and challenges. Nat Rev Genet. 2008;9:356–369. doi: 10.1038/nrg2344. [DOI] [PubMed] [Google Scholar]
- 36.Cervino A, Lakiss S, Sow O, Hill A. Allelic association between the NRAMP1 gene and susceptibility to tuberculosis in Guinea-Conakry. Ann Hum Genet. 2000;64:507–512. doi: 10.1046/j.1469-1809.2000.6460507.x. [DOI] [PubMed] [Google Scholar]
- 37.El Baghdadi J, Remus N, Benslinane A, El Annaz H, Chentoufi M, Abel L, Schurr E. Variants of the human NRAMP1 gene and susceptibility to tuberculosis in Morocco. Int J Tuberc Lung Dis. 2004;7:599–602. [PubMed] [Google Scholar]
- 38.Dubaniewicz A, Jamieson SE, Dubaniewicz-Wybieralska M, Fakiola M, Nancy ME, Blackwell JM. Association between SLC11A1 (formerly NRAMP1) and the risk of sarcoidosis in Poland. Eur J Hum Genet. 2005;13:829–834. doi: 10.1038/sj.ejhg.5201370. [DOI] [PubMed] [Google Scholar]
- 39.Chapman JS, Dyerly MD. Social and other factors in intrafamilial transmission of tuberculosis. Am Rev Respir Dis. 1964;90:48–60. doi: 10.1164/arrd.1964.90.1.48. [DOI] [PubMed] [Google Scholar]
- 40.Enarson D, Chiang C-Y, Murray J. Global epidemiology of tuberculosis. In: Rom WN, Garay SM, editors. Tuberculosis. Philadelphia: Lippincott Williams & Wilkins; 2004. pp. 13–30. [Google Scholar]
- 41.Guwattude D, Nakakeeto M, Jones-Lopez E, Maganda A, Chiunda A, Mugerwa R, Ellner J, Bukenya G, Whalen C. Tuberculosis in household contacts of infectious cases in Kampala, Uganda. Am J Epidemiol. 2003;158:887–898. doi: 10.1093/aje/kwg227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Satten GA, Flanders WD, Yang Q. Accounting for unmeasured population substructure in case-control studies of genetic association using a novel latent-class model. Am J Hum Genet. 2001;68:466–477. doi: 10.1086/318195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Marchini J, Cardon LR, Phillips MS, Donnelly P. The effects of human population structure on large genetic association studies. Nat Genet. 2004;36:512–517. doi: 10.1038/ng1337. [DOI] [PubMed] [Google Scholar]
- 44.Ma X, Reich R, González A, Pan X, Fothergill A, Starke J, Teeter L, Musser J, Graviss E. No evidence for association between the polymorphism in the 3′ untranslated region of interleukin-12B and human susceptibility to tuberculosis. J Infect Dis. 2003;188:1116–1118. doi: 10.1086/378674. [DOI] [PubMed] [Google Scholar]
- 45.Velez DR, Hulme WF, Myers JL, Weinberg JB, Levesque MC, Stryjewski ME, Abbate E, Estevan R, Patillo SG, Gilbert JR, Hamilton CD, Scott WK. NOS2A, TLR4, and IFNGR1 interactions influence pulmonary tuberculosis susceptibility in African-Americans. Hum Genet. 2009;126:643–653. doi: 10.1007/s00439-009-0713-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Velez DR, Wejse C, Stryjewski ME, Abbate E, Hulme WF, Myers JL, Estevan R, Patillo SG, Olesen R, Tacconelli A, Sirugo G, Gilbert JR, Hamilton CD, Scott WK. Variants in toll-like receptors 2 and 9 influence susceptibility to pulmonary tuberculosis in Caucasians, African-Americans, and West Africans. Hum Genet. 2010;127:65–73. doi: 10.1007/s00439-009-0741-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Barreiro LB, Neyrolles O, Babb CL, Tailleux L, Quach H, McElreavey K, Helden PD, Hoal EG, Gicquel B, Quintana-Murci L. Promoter variation in the DC-SIGN-encoding gene CD209 is associated with tuberculosis. PLoS Med. 2006;3:e20. doi: 10.1371/journal.pmed.0030020. doi: 10.1371/journal.pmed.0030020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Moller M, Nebel A, Valentonyte R, Van Helden PD, Schreiber S, Hoal EG. Investigation of chromosome 17 candidate genes in susceptibility to TB in a South African population. Tuberculosis (Edinb) 2009;89:189–194. doi: 10.1016/j.tube.2008.10.001. [DOI] [PubMed] [Google Scholar]
- 49.Davila S, Hibberd ML, Hari DR, Wong HE, Sahiratmadja E, Bonnard C, Alisjahbana B, Szeszko JS, Balabanova Y, Drobniewski F, van Crevel R, van de Vosse E, Nejentsev S, Ottenhoff THM, Seielstad M. Genetic association and expression studies indicate a role of toll-like receptor 8 in pulmonary tuberculosis. PLoS Genet. 2008;4:e1000218. doi: 10.1371/journal.pgen.1000218. doi: 10.1371/journal.pgen.1000218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Deng HW. Population admixture may appear to mask, change or reverse genetic effects of genes underlying complex traits. Genetics. 2001;159:1319–1323. doi: 10.1093/genetics/159.3.1319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.International HapMap Consortium. The International HapMap Project. Nature. 2003;426:789–796. doi: 10.1038/nature02168. [DOI] [PubMed] [Google Scholar]
- 52.International HapMap Consortium. A haplotype map of the human genome. Nature. 2005;437:1299–1320. doi: 10.1038/nature04226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Gabriel SB, Schaffner SF, Nguyen H, Moore JM, Roy J, Blumenstiel B, Higgins J, Defelice M, Lochner A, Faggart M, Liu-Cordero SN, Rotimi C, Adeyemo A, Cooper R, Ward R, Lander ES, Daly MJ, Altshuler D. The structure of haplotype blocks in the human genome. Science. 2002;296:2225–2229. doi: 10.1126/science.1069424. [DOI] [PubMed] [Google Scholar]
- 54.Hindorff LA, Sethupathy P, Junkins HA, Ramos EM, Mehta JP, Collins FS, Manolio TA. Potential etiologic and functional implications of genome-wide association loci for human diseases and traits. Proc Natl Acad Sci U S A. 2009;106:9362–9367. doi: 10.1073/pnas.0903103106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Tang NL, Fan HP, Chang KC, Ching JK, Kong KP, Yew WW, Kam KM, Leung CC, Tam CM, Blackwell J, Chan CY. Genetic association between a chemokine gene CXCL-10 (IP-10, interferon gamma inducible protein 10) and susceptibility to tuberculosis. Clin Chim Acta. 2009;406:98–102. doi: 10.1016/j.cca.2009.06.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Dissanayeke SR, Levin S, Pienaar S, Wood K, Eley B, Beatty D, Henderson H, Anderson S, Levin M. Polymorphic variation in TIRAP is not associated with susceptibility to childhood TB but may determine susceptibility to TBM in some ethnic groups. PLoS ONE. 2009;4:e6698. doi: 10.1371/journal.pone.0006698. doi: 10.1371/journal.pone.0006698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Hawn TR, Dunstan SJ, Thwaites GE, Simmons CP, Thuong NT, Lan NT, Quy HT, Chau TT, Hieu NT, Rodrigues S, Janer M, Zhao LP, Hien TT, Farrar JJ, Aderem A. A polymorphism in Toll-interleukin 1 receptor domain containing adaptor protein is associated with susceptibility to meningeal tuberculosis. J Infect Dis. 2006;194:1127–1134. doi: 10.1086/507907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Thuong NT, Hawn TR, Thwaites GE, Chau TT, Lan NT, Quy HT, Hieu NT, Aderem A, Hien TT, Farrar JJ, Dunstan SJ. A polymorphism in human TLR2 is associated with increased susceptibility to tuberculous meningitis. Genes Immun. 2007;8:422–428. doi: 10.1038/sj.gene.6364405. [DOI] [PubMed] [Google Scholar]
- 59.Reich DE, Lander ES. On the allelic spectrum of human disease. Trends Genet. 2001;17:502–510. doi: 10.1016/s0168-9525(01)02410-6. [DOI] [PubMed] [Google Scholar]
- 60.Bodmer W, Bonilla C. Common and rare variants in multifactorial susceptibility to common diseases. Nat Genet. 2008;40:695–701. doi: 10.1038/ng.f.136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Ma X, Liu Y, Gowen BB, Graviss EA, Clark AG, Musser JM. Full-exon resequencing reveals toll-like receptor variants contribute to human susceptibility to tuberculosis disease. PLoS ONE. 2007;2:e1318. doi: 10.1371/journal.pone.0001318. doi: 10.1371/journal.pone.0001318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Baker A, Randhawa A, Shey M, de Kock M, Kaplan G, Adams M, Hanekom WA, Boom WH, Hawn TR, Stein CM. Comparison of genotype frequencies in Toll-like receptor genes in Ugandans, South Africans, and African HapMap populations. Presented at the American Society of Human Genetics 59th annual meeting; 20–24 October 2009; Honolulu, Hawaii, United States of America. 1808/T/Poster Board #357 2009 [Google Scholar]
- 63.McCarroll SA, Altshuler DM. Copy-number variation and association studies of human disease. Nat Genet. 2007;39:S37–S42. doi: 10.1038/ng2080. [DOI] [PubMed] [Google Scholar]
- 64.Gagneux S, Small PM. Global phylogeography of Mycobacterium tuberculosis and implications for tuberculosis product development. Lancet Infect Dis. 2007;7:328–337. doi: 10.1016/S1473-3099(07)70108-1. [DOI] [PubMed] [Google Scholar]
- 65.Thwaites G, Caws M, Chau TT, D'Sa A, Lan NT, et al. The relationship between Mycobacterium tuberculosis genotype and the clinical phenotype of pulmonary and meningeal tuberculosis. J Clin Microbiol. 2008;46:1363–1368. doi: 10.1128/JCM.02180-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.de Jong BC, Hill PC, Aiken A, Awine T, Antonio M, Adetifa IM, Jackson-Sillah DJ, Fox A, Deriemer K, Gagneux S, Borgdorff MW, McAdam KP, Corrah T, Small PM, Adegbola RA. Progression to active tuberculosis, but not transmission, varies by Mycobacterium tuberculosis lineage in The Gambia. J Infect Dis. 2008;198:1037–1043. doi: 10.1086/591504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Caws M, Thwaites G, Dunstan S, Hawn TR, Lan NT, Thuong NT, Stepniewska K, Huyen MN, Bang ND, Loc TH, Gagneux S, Van SD, Kremer K, van der SM, Small P, Anh PT, Chinh NT, Quy HT, Duyen NT, Tho DQ, Hieu NT, Torok E, Hien TT, Dung NH, Nhu NT, Duy PM, van Vinh CN, Farrar J. The influence of host and bacterial genotype on the development of disseminated disease with Mycobacterium tuberculosis. PLoS Pathog. 2008;4:e1000034. doi: 10.1371/journal.ppat.1000034. doi: 10.1371/journal.ppat.1000034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Berrington WR, Hawn TR. Mycobacterium tuberculosis, macrophages, and the innate immune response: does common variation matter? Immunol Rev. 2007;219:167–186. doi: 10.1111/j.1600-065X.2007.00545.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Bafica A, Scanga CA, Feng CG, Leifer C, Cheever A, Sher A. TLR9 regulates Th1 responses and cooperates with TLR2 in mediating optimal resistance to Mycobacterium tuberculosis. J Exp Med. 2005;202:1715–1724. doi: 10.1084/jem.20051782. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Gomez LM, Anaya JM, Vilchez JR, Cadena J, Hinojosa R, Velez L, Lopez-Nevot MA, Martin J. A polymorphism in the inducible nitric oxide synthase gene is associated with tuberculosis. Tuberculosis (Edinb) 2007;87:288–294. doi: 10.1016/j.tube.2007.03.002. [DOI] [PubMed] [Google Scholar]
- 71.Giacomini E, Remoli ME, Gafa V, Pardini M, Fattorini L, Coccia EM. IFN-beta improves BCG immunogenicity by acting on DC maturation. J Leukoc Biol. 2009;85:462–468. doi: 10.1189/jlb.0908583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Gustafson P, Gomes VF, Vieira CS, Jensen H, Seng R, Norberg R, Samb B, Naucler A, Aaby P. Tuberculosis mortality during a civil war in Guinea-Bissau. JAMA. 2001;286:599–603. doi: 10.1001/jama.286.5.599. [DOI] [PubMed] [Google Scholar]
- 73.Parrish NM, Dick JD, Bishai WR. Mechanisms of latency in Mycobacterium tuberculosis. Trends Microbiol. 1998;6:107–112. doi: 10.1016/s0966-842x(98)01216-5. [DOI] [PubMed] [Google Scholar]
- 74.Comas I, Gagneux S. The past and future of tuberculosis research. PLoS Pathog. 2009;5:e1000600. doi: 10.1371/journal.ppat.1000600. doi: 10.1371/journal.ppat.1000600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Wheeler E, Miller EN, Peacock CS, Donaldson IJ, Shaw MA, Jamieson SE, Blackwell JM, Cordell HJ. Genome-wide scan for loci influencing quantitative immune response traits in the Belem family study: comparison of methods and summary of results. Ann Hum Genet. 2006;70:78–97. doi: 10.1111/j.1529-8817.2005.00223.x. [DOI] [PubMed] [Google Scholar]
- 76.Hawn TR, Misch EA, Dunstan SJ, Thwaites GE, Lan NT, et al. A common human TLR1 polymorphism regulates the innate immune response to lipopeptides. Eur J Immunol. 2007;37:2280–2289. doi: 10.1002/eji.200737034. [DOI] [PubMed] [Google Scholar]
- 77.Shey MS, Randhawa AK, Bowmaker M, Smith E, Scriba TJ, de Kock M, Mahomed H, Hussey G, Hawn TR, Hanekom WA. Single nucleotide polymorphisms in toll-like receptor 6 are associated with altered lipopeptide- and mycobacteria-induced interleukin-6 secretion. Genes Immun. 2010;11:561–572. doi: 10.1038/gene.2010.14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Thuong NT, Dunstan SJ, Chau TT, Thorsson V, Simmons CP, Quyen NT, Thwaites GE, Thi Ngoc Lan N, Hibberd M, Teo YY, Seielstad M, Aderem A, Farrar JJ, Hawn TR. Identification of tuberculosis susceptibility genes with human macrophage gene expression profiles. PLoS Pathog. 2008;4:e1000229. doi: 10.1371/journal.ppat.1000229. doi: 10.1371/journal.ppat.1000229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Manolio TA, Collins FS, Cox NJ, Goldstein DB, Hindorff LA, Hunter DJ, McCarthy MI, Ramos EM, Cardon LR, Chakravarti A, Cho JH, Guttmacher AE, Kong A, Kruglyak L, Mardis E, Rotimi CN, Slatkin M, Valle D, Whittemore AS, Boehnke M, Clark AG, Eichler EE, Gibson G, Haines JL, Mackay TF, McCarroll SA, Visscher PM. Finding the missing heritability of complex diseases. Nature. 2009;461:747–753. doi: 10.1038/nature08494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Bellamy R, Ruwende C, Corrah T, McAdam K, Whittle H, Hill A. Variations in the NRAMP1 gene and susceptibility to tuberculosis in West Africans. N Engl J Med. 1998;338:640–644. doi: 10.1056/NEJM199803053381002. [DOI] [PubMed] [Google Scholar]
- 81.Awomoyi A, Marchant A, Howson J, McAdam K, Blackwell J, Newport M. Interleukin-10, Polymorphism in SLC11A1 (formerly NRAMP1), and susceptibility to tuberculosis. J Infect Dis. 2002;186:1808–1814. doi: 10.1086/345920. [DOI] [PubMed] [Google Scholar]
- 82.Fitness J, Floyd S, Warndorff D, Sichali L, Malema S, Crampin A, Fine P, Hill A. Large-scale candidate gene study of tuberculosis susceptibility in the Karonga district of Nothern Malawi. Am J Trop Med Hyg. 2004;71:341–349. [PubMed] [Google Scholar]
- 83.Soborg C, Andersen AB, Range N, Malenganisho W, Friis H, Magnussen P, Temu MM, Changalucha J, Madsen HO, Garred P. Influence of candidate susceptibility genes on tuberculosis in a high endemic region. Mol Immunol. 2007;44:2213–2220. doi: 10.1016/j.molimm.2006.11.002. [DOI] [PubMed] [Google Scholar]
- 84.Ma X, Wright J, Reich R, Teeter L, El Sahly H, Awe R, Musser J, Graviss E. 5′ dinucleotide repeat polymorphism of NRAMP1 and susceptibility to tuberculosis among Caucasian patients in Houston, Texas. Int J Tuberc Lung Dis. 2002;6:818–823. [PubMed] [Google Scholar]
- 85.Delgado J, Baena A, Thim S, Goldfeld A. Ethnic-specific genetic associations with pulmonary tuberculosis. J Infect Dis. 2002;186:1463–1468. doi: 10.1086/344891. [DOI] [PubMed] [Google Scholar]
- 86.Liu W, Cao W, Zhang C, Tian L, Wu X, Habbema J, Zhao Q, Zhang P, Xin Z-T, Li C, Yang H. VDR and NRAMP1 gene polymorphisms in susceptibility to pulmonary tuberculosis among the Chinese Han population: a case-control study. Int J Tuberc Lung Dis. 2004;8:428–434. [PubMed] [Google Scholar]
- 87.Abe T, Iinuma Y, Ando M, Yokoyama T, Yamamoto T, Nakashima K, Takagi N, Baba H, Hasegawa Y, Shimokata K. NRAMP1 polymorphisms, susceptibility and clinical features of tuberculosis. J Infect. 2003;46:215–220. doi: 10.1053/jinf.2002.1064. [DOI] [PubMed] [Google Scholar]
- 88.Gao P-S, Fujishima S, Mao X-Q, Remus N, Kanda M, Enomoto T, Dake Y, Bottini N, Tabuchi M, Hasegawa N, Yamaguchi K, Tiemessen C, Hopkin J, Shirakawa T, Kishi F. Genetic variants of NRAMP1 and active tuberculosis in Japanese populations. Clin Genet. 2000;58:74–76. doi: 10.1034/j.1399-0004.2000.580113.x. [DOI] [PubMed] [Google Scholar]
- 89.Liaw Y-S, Wu J-JT, Wu C-H, Hung C-C, Lee C-N, Yang P-C, Luh K-T, Kuo S-H. Variations in the NRAMP1 gene and susceptibility of tuberculosis in Taiwanese. Int J Tuberc Lung Dis. 2002;6:454–460. [PubMed] [Google Scholar]
- 90.Akahoshi M, Ishihara M, Remus N, Uno K, Miyake K, Hirota T, Nakashima K, Matsuda A, Kanda M, Enomoto T, Ohno S, Nakashima H, Casanova JL, Hopkin JM, Tamari M, Mao XQ, Shirakawa T. Association between IFNA genotype and the risk of sarcoidosis. Hum Genet. 2004;114:503–509. doi: 10.1007/s00439-004-1099-5. [DOI] [PubMed] [Google Scholar]
- 91.Vejbaesya S, Chierakul N, Luangtrakool P, Sermduangprateep C. NRAMP1 and TNF-alpha polymorphisms and susceptibility to tuberculosis in Thais. Respirology. 2007;12:202–206. doi: 10.1111/j.1440-1843.2006.01037.x. [DOI] [PubMed] [Google Scholar]
- 92.Leung KH, Yip SP, Wong WS, Yiu LS, Chan KK, Lai WM, Chow EY, Lin CK, Yam WC, Chan KS. Sex- and age-dependent association of SLC11A1 polymorphisms with tuberculosis in Chinese: a case control study. BMC Infect Dis. 2007;7:19. doi: 10.1186/1471-2334-7-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Ryu S, Park Y-K, Bai G-H, Kim S-J, Park S-N, Kang S. 3′UTR polymorphisms in the NRAMP1 gene are associated with susceptibility to tuberculosis in Koreans. Int J Tuberc Lung Dis. 2000;4:577–580. [PubMed] [Google Scholar]
- 94.Kusuhara K, Yamamoto K, Okada K, Mizuno Y, Hara T. Association of IL12RB1 polymorphisms with susceptibility to and severity of tuberculosis in Japanese: a gene-based association analysis of 21 candidate genes. Int J Immunogenet. 2007;34:35–44. doi: 10.1111/j.1744-313X.2007.00653.x. [DOI] [PubMed] [Google Scholar]