Abstract
OBJECTIVE
We examined the relationship between the presence and extent of coronary stenosis and carotid intima-media thickness (CIMT) in type 2 diabetic patients without history of coronary artery disease (CAD) but with carotid atherosclerosis.
RESEARCH DESIGN AND METHODS
A total of 91 type 2 diabetic patients underwent multi-slice computed tomography coronary angiography.
RESULTS
Max-IMT in the ≥50% stenosis group by multi-slice computed tomography coronary angiography estimation was significantly greater than the 0–25 and 25–50% stenosis group (2.68 ± 0.77 vs. 1.61 ± 0.49 mm, P < 0.0005, and 2.14 ± 0.81 mm, P < 0.05, respectively), and max-IMT in the 25–50% stenosis group was significantly greater than the 0–25% stenosis group (P < 0.05) after adjustment for age, sex, duration of type 2 diabetes, hypertension, and dyslipidemia. In the analysis for trend through the categories of max-IMT, as max-IMT increased, the percentage of ≥50% stenosis increased and the percentage of 0–25% stenosis decreased.
CONCLUSIONS
Our data suggest that max-IMT might be closely associated with the extent of coronary stenosis in type 2 diabetic patients without history of CAD but with carotid atherosclerosis.
Coronary stenosis was evaluated with selective coronary angiography, but the subjects were limited to patients with a history and/or suspicion of coronary artery disease (CAD) because of its invasiveness. Therefore, little information is available regarding the relationship between coronary stenosis and carotid intima-media thickness (CIMT) in asymptomatic type 2 diabetic patients. Recently, multi-slice computed tomography (MSCT) coronary angiography (MSCTA) enabled us to evaluate coronary stenosis accurately and noninvasively (1–3).
In this study, we performed MSCTA in patients without a history of CAD but with carotid atherosclerosis and explored the usefulness of CIMT measurement in screening for CAD in asymptomatic type 2 diabetic patients for which a useful strategy remains uncertain and controversial (4–8).
RESEARCH DESIGN AND METHODS
Study population
Among 169 type 2 diabetic inpatients in Osaka University Medical Hospital whose max-IMT was ≥1.1 mm and who did not have a history of CAD, which was defined as documentation of medication and history of myocardial infarction, angina pectoris, and/or previous coronary intervention, 91 patients consented to undergo MSCTA. The clinical characteristics of the subjects were as follows: men 67%; age 62 ± 10 years; duration of type 2 diabetes 13 ± 9 years; smoking 56% (definition of smoking was based on a questionnaire); hypertension 56%; dyslipidemia 76%; A1C 8.3 ± 1.7%; max-IMT 2.17 ± 0.83 mm; ankle-brachial pressure index (ABPI) 1.07 ± 0.14; and brachial-ankle pulse wave velocity (baPWV) 1,770 ± 394 (cm/s).
CIMT measurement
CIMT was measured using an echotomographic system (Aplio AAS-700A; Toshiba Medical Systems, Tochigi, Japan) with a 7.5-MHz linear transducer. With the longitudinal projection of the common carotid artery, the carotid bulb, and the internal carotid artery, the site of the greatest thickness including a plaque lesion was sought along both near and far walls bilaterally (max-IMT). Carotid atherosclerosis was defined as max-IMT ≥1.1 mm according to the criteria of the Japan Academy of Neurosonology (9). In addition, all measurements of CIMT were performed by experienced physicians.
MSCT coronary angiography
Imaging was performed with a 64-slice (indicated as (64) hereafter) or 320-slice (likewise indicated as (320)) MSCT scanner (Aquilion (64) or Aquilion ONE (320); Toshiba Medical Systems). MSCTA was performed with a helical (64) or volumetric (320) scan with β-blockers and sublingual nitrates if necessary. Reconstruction with phases of fewest motion artifacts was performed and images were transferred to a remote workstation for post-processing.
MSCTA images were interpreted by two experienced observers blind to the patient’s characteristics using specialized software (Ziostation; Ziosoft, Tokyo, Japan).
Using a 15-segment model according to the American Heart Association classification, presence of coronary atherosclerosis and luminal narrowing in each segment was visually graded into four classes: 0–25% stenosis, 25–50% stenosis, 50–75% stenosis, and ≥75% stenosis.
Statistical analysis
Max-IMT was compared by ANCOVA with Holm adjustments. Analysis of trend through categories of max-IMT was performed with the χ2 test for trend. The receiver operating characteristic (ROC) curve analysis was used to determine the optimal cutoff value of max-IMT for ≥50% coronary stenosis. CIs of ROC values were calculated through bootstrap resampling, and there were 2,000 bootstrap samples, according to the percentile method. The threshold of statistical significance was defined as P < 0.05.
RESULTS
MSCTA results
A total of 1,330 coronary segments were analyzed, and 17 were undiagnosable because of motion (n = 12) or calcification (n = 5). A total of 29 patients (32%) had at least one segment of ≥50% stenosis, 37 (41%) had at least one segment of 25–50% stenosis, and 25 (27%) had only 0–25% stenosis.
Relationship between CIMT and coronary stenosis
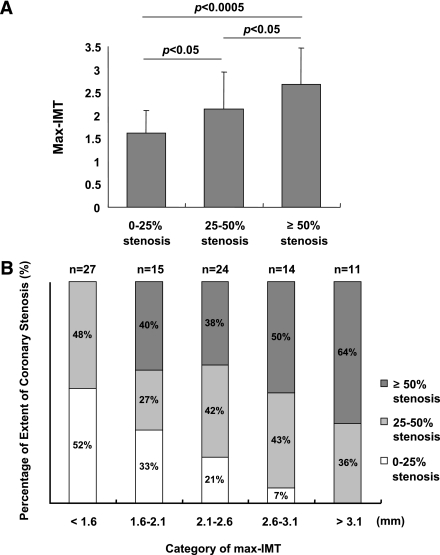
Max-IMT was significantly greater in the ≥50% stenosis group (2.68 ± 0.77 mm) compared with the 0–25% stenosis group (1.61 ± 0.49 mm) (P < 0.0005) and the 25–50% stenosis group (2.14 ± 0.81 mm) (P < 0.05), and the max-IMT of the 25–50% stenosis group was significantly greater than the 0–25% stenosis group (P < 0.05) after adjustment for age, sex, duration of type 2 diabetes, hypertension, and dyslipidemia (Fig. 1A).
Figure 1.
A: The relationship between CIMT and coronary stenosis. Max-IMT was significantly greater in the ≥50% stenosis group (2.68 ± 0.77 mm) than the 0–25% stenosis group (1.61 ± 0.49 mm) (P < 0.0005) and the 25–50% stenosis group (2.14 ± 0.81 mm) (P < 0.05). In addition, the max-IMT of the 25–50% stenosis group was significantly greater than the 0–25% stenosis group (P < 0.05). B: The extent of coronary stenosis in each max-IMT category. In the max-IMT <1.6 mm group, the percentage of ≥50% stenosis was 0%, whereas in the patients whose max-IMT was ≥1.6 mm, the percentage of ≥50% stenosis was 45%. Furthermore, in the analysis for trend through the categories of max-IMT, as max-IMT was increased, the percentage of ≥50% stenosis was increased (P < 0.00005) and the percentage of 0–25% stenosis was decreased (P < 0.0001).
In the analysis for trend through the categories of max-IMT, as max-IMT increased, the percentage of ≥50% stenosis increased (P < 0.00005) and the percentage of 0–25% stenosis decreased (P < 0.0001) (Fig. 1B).
ROC curve analysis for ≥50% stenosis
The area under the ROC curve (AUC) of max-IMT, ABPI, and baPWV were 0.78 (95% CI 0.70–0.86), 0.72 (0.63–0.83), and 0.73 (0.62–0.83), respectively. The cutoff level of max-IMT providing the maximal sum of sensitivity and specificity was 1.90 mm (95% CI 1.6–2.5). At this cutoff level, sensitivity was 0.93 (95% CI 0.71–1.00) and specificity was 0.55 (0.42–0.83). The positive predictive value was 0.49 (95% CI 0.39–0.69), and the negative predictive value was 0.94 (0.84–1.00).
When max-IMT was combined with baPWV and ABPI, the AUC of max-IMT was 0.83 (95% CI 0.75–0.92) at a max-IMT cutoff level of 1.60 mm (1.6–2.1), a baPWV cutoff level of 1,430 cm/s, and an ABPI cutoff level of 1.19. At these cutoff values, sensitivity was 0.97 (95% CI 0.87–1.00) and specificity was 0.68 (0.60–0.83). Positive predictive value was 0.58 (95% CI 0.49–0.75), and negative predictive value was 0.98 (0.92–1.00).
CONCLUSIONS
Our data suggest that max-IMT might be closely associated with the presence and extent of coronary stenosis in type 2 diabetic patients without history of CAD but with carotid atherosclerosis and that max-IMT measurement might have a passable AUC, high sensitivity, high negative predictive value, low specificity, and low positive predictive value for significant coronary stenosis. We propose a hypothesis that max-IMT measurement might be useful for distinguishing patients who need not undergo workup for coronary stenosis but that max-IMT might be insufficient to determine patients who should undergo workup for coronary stenosis. We consider this study not conclusive but hypothesis generating. When this study was designed, available information was so little to calculate an appropriate sample size. Consequently, our study population of 91 was insufficient to calculate clinically useful cutoff values with narrower 95% CIs and to compare usefulness of max-IMT, ABPI, and baPWV. Another limitation of this study was CIMT measurements, which were performed by three operators as daily clinical routine examinations and should inevitably involve operator variability. Larger replication studies need to be designed with appropriate sample size calculations, and our results may provide a rationale to conduct such studies.
Acknowledgments
No potential conflicts of interest relevant to this article were reported.
R.K. researched data and wrote the manuscript. H.K. supervised this work, contributed to the discussion, and reviewed and edited the manuscript. S.S. wrote and reviewed and edited the manuscript. K.Y., T.K., K.T., T.Y., and A.K. researched data and wrote the manuscript. N.K. researched data, planned and supervised this work, contributed to the discussion, and reviewed the manuscript. M.M. planned and supervised this work, contributed to the discussion, and reviewed the manuscript. T.-a.M. and I.S. contributed to the discussion and reviewed and edited the manuscript.
The authors thank Dr. Helena Akiko Popiel (National Center of Neurology and Psychiatry) for valuable comments on the manuscript.
References
- 1.Miller JM, Rochitte CE, Dewey M, et al. Diagnostic performance of coronary angiography by 64-row CT. N Engl J Med 2008;359:2324–2336 [DOI] [PubMed] [Google Scholar]
- 2.Budoff MJ, Dowe D, Jollis JG, et al. Diagnostic performance of 64-multidetector row coronary computed tomographic angiography for evaluation of coronary artery stenosis in individuals without known coronary artery disease: results from the prospective multicenter ACCURACY (Assessment by Coronary Computed Tomographic Angiography of Individuals Undergoing Invasive Coronary Angiography) trial. J Am Coll Cardiol 2008;52:1724–1732 [DOI] [PubMed] [Google Scholar]
- 3.Meijboom WB, Meijs MF, Schuijf JD, et al. Diagnostic accuracy of 64-slice computed tomography coronary angiography: a prospective, multicenter, multivendor study. J Am Coll Cardiol 2008;16:2135–2144 [DOI] [PubMed] [Google Scholar]
- 4.Bax JJ, Young LH, Frye RL, et al. Screening for coronary artery disease in patients with diabetes. Diabetes Care 2007;30:2729–2736 [DOI] [PubMed] [Google Scholar]
- 5.Scognamiglio R, Negut C, Ramondo A, Tiengo A, Avogaro A. Detection of coronary artery disease in asymptomatic patients with type 2 diabetes mellitus. J Am Coll Cardiol 2006;47:65–71 [DOI] [PubMed] [Google Scholar]
- 6.Wackers FJ, Young LH, Inzucchi SE, et al. Detection of silent myocardial ischemia in asymptomatic diabetic subjects: the DIAD study. Diabetes Care 2004;27:1954–1961 [DOI] [PubMed] [Google Scholar]
- 7.American Diabetes Association Standards of medical care in diabetes—2010. Diabetes Care 2010;33(Suppl. 1):S11–S61 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Buse JB, Ginsberg HN, Bakris GL, et al. Primary prevention of cardiovascular diseases in people with diabetes mellitus: a scientific statement from the American Heart Association and the American Diabetes Association. Circulation 2007;115:114–126 [DOI] [PubMed] [Google Scholar]
- 9.The Joint Committee of “The Japan Academy of Neurosonology” and “The Japan Society of Embolus Detection and Treatment” on Guideline for Neurosonology. Carotid ultrasound examination. Neurosonology 2006;19:49–69 [Google Scholar]