Childhood onset schizophrenia (COS) is a rare, severe form of schizophrenia for which definitive genetic causes remain elusive.1,2 In this study, we report a novel 4-nucleotide deletion in the UPF3B gene, predicted to create a truncated protein, transmitted from a healthy mother to two affected brothers: one with comorbid diagnoses of COS, pervasive developmental disorder not otherwise specified and attention deficit hyperactivity disorder (ADHD), and the other with autism and ADHD. This work provides evidence that UPF3B, already described as a cause of syndromic and nonsyndromic X-linked mental retardation with or without autism,3,4 is also involved in COS, autism spectrum disorders and ADHD.
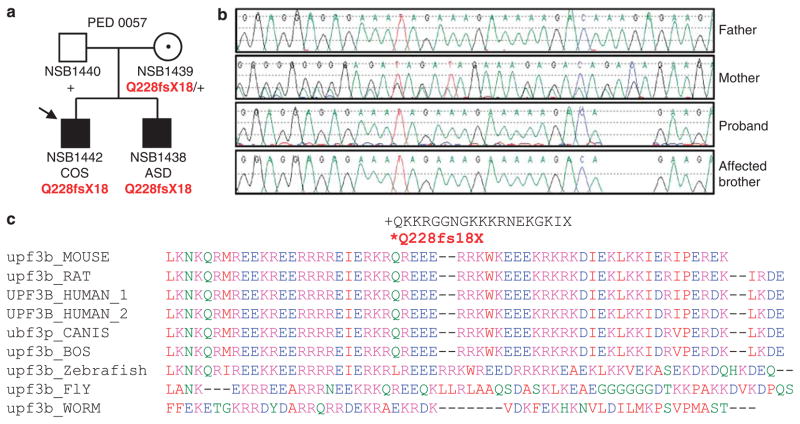
As part of the Synapse to Disease project (http://www.synapse2disease.com/en_projet.html), we sequenced several hundred genes implicated in synapse function and/or structure in 28 probands with COS to identify rare pathogenic disease-causing variants. We amplified and sequenced all coding and intronic flanking regions in UPF3B as described previously.5 PCR primers targeting the 11 exons of UPF3B (chrX:118,967,989-118,986,968, NCBI build 37.1; RefSeq NM_080632) were designed using Exon-Primer from the UCSC Genome Browser. We identified a deletion of 4 nucleotides in exon 7 of UPF3B, predicted to cause a frameshift (c.683_686delAAGA, p.Q228fsX18) and a truncated UPF3B protein in the hemizygous state in a male patient (see Figure 1). This deletion was also identified in his brother diagnosed with autism and transmitted from the unaffected mother. This mutation is located very close to another 4-bp deletion (R225fsX20), recently identified in a family with a diagnosis of FG syndrome and intellectual disability.4
Figure 1.
Identification of a 4-nucleotide deletion (c.683_686delAAGA, p.Q228fsX18) in UPF3B in two brothers with childhood onset schizophrenia (COS), autism spectrum disorder (ASD) and comorbid attention deficit hyperactivity disorder (ADHD). (a) Segregation of the protein-truncating mutation in the family. The proband is indicated by the arrow. (b) Chromatograms containing UPF3B mutation for the patient, brother, father and mother. (c) Alignment of UPF3B orthologous peptide sequences near the Q228fsX18 truncating mutation (marked by an asterisk (*)) showing amino-acid conservation of the Q228 nearby residues in several species.
Given that the asymptomatic mother was a carrier of the p.Q228fsX18 mutation identified in this study, we determined her X Chromosome Inactivation profile with the Human Androgen Receptor Gene (HUMARA) assay as described previously,6 using 200 ng of genomic DNA from peripheral blood. Only 24% of mother’s blood cells expressed the X chromosome harboring the mutation, indicating that the mother showed a moderately skewed X inactivation pattern with a preferential inactivation (76:24) of the mutated X chromosome allele.
The proband, NSB1442, was the product of an uneventful pregnancy and delivery; developmental milestones were within normal limits. When he first attended school, immediate problems with hyperactivity, immaturity, and impaired social interaction were noted; he was diagnosed with borderline cognitive ability (full scale IQ = 79), ADHD and pervasive developmental disorder not otherwise specified. He was subsequently placed in special education. At the age of 10 years, he began exhibiting paranoid ideation that people and animals were ‘out to get him,’ and he was hospitalized for one month. At the age of 12 years, he was rehospitalized as a result of inappropriate touching of female peers, aggression towards peers, and threats of violence toward himself and others. Concurrently, he reported auditory hallucinations and delusions that his thoughts and behaviors were being controlled by the voices. He was diagnosed with COS and enrolled in the COS study at the NIMH (National Institute of Mental Health) at the age of 15 years. It is also noteworthy that he received a score of 25 on the ASQ (Autism Screening Questionnaire; score > 15 = autism).7
The younger brother of the proband, NSB1438, was born with congenital pulmonary stenosis, which precipitated angioplasty attempts at ages 4 and 13 months and a pulmonary valvotomy at 33 months. He had delayed developmental milestones as he did not begin to walk until 16 months and spoke only a few words by 33 months of age. His vocabulary increased by age 3 3/4 years, but he demonstrated significant difficulty with language comprehension, as shown by echolalia and failure to respond to verbal commands/directions with verbal responses. At this time, he also demonstrated significant impulsivity and, after assessment by a special education institution, received diagnoses of ADHD, aphasic language delay, fine motor delay, social delay, and mixed pervasive developmental disorder. He has a full-scale IQ of 87 and was given a formal diagnosis of autism at age 8 years; he scored 31 on the ASQ. Presently at the age of 20 years, he has not experienced any psychotic symptoms.
This is the first report linking a protein truncating mutation in UPF3B, a member of the nonsense-mediated mRNA decay complex, as a causative factor in the development of COS, autism spectrum disorders, and ADHD in the same family. The UPF3B gene encodes a protein that is part of a postsplicing multiprotein complex involved in both mRNA nuclear export and mRNA surveillance and may have a potential function in the regulation of the expression and degradation of various mRNAs present at the synapse.3 This report adds to the growing evidence of both clinical8 and genetic9,10 overlap that is indicative of a broad neurodevelopmental phenotype, which includes autism, intellectual disability, and schizophrenia. Further investigation of association between UPF3B and related genes with schizophrenia is warranted.
Footnotes
Conflict of interest
The authors declare no conflict of interest.
References
- 1.Rapoport JL, Addington AM, Frangou S. Mol Psychiatry. 2005;10:434–449. doi: 10.1038/sj.mp.4001642. [DOI] [PubMed] [Google Scholar]
- 2.Addington AM, Rapoport JL. Curr Psychiatry Rep. 2009;11:156–161. doi: 10.1007/s11920-009-0024-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Laumonnier F, Shoubridge C, Antar C, Nguyen LS, Van Esch H, Kleefstra T, et al. Mol Psychiatry. 2009 doi: 10.1038/mp.2009.14. e-pub ahead of print 24 February 2009. [DOI] [PubMed] [Google Scholar]
- 4.Tarpey PS, Raymond FL, Nguyen LS, Rodriguez J, Hackett A, Vandeleur L, et al. Nat Genet. 2007;39:1127–1133. doi: 10.1038/ng2100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Gauthier J, Spiegelman D, Piton A, Lafreniere RG, Laurent S, St-Onge J, et al. Am J Med Genet B Neuropsychiatr Genet. 2009;150B:421–424. doi: 10.1002/ajmg.b.30822. [DOI] [PubMed] [Google Scholar]
- 6.Allen RC, Zoghbi HY, Moseley AB, Rosenblatt HM, Belmont JW. Am J Hum Genet. 1992;51:1229–1239. [PMC free article] [PubMed] [Google Scholar]
- 7.Berument SK, Rutter M, Lord C, Pickles A, Bailey A. Br J Psychiatry. 1999;175:444–451. doi: 10.1192/bjp.175.5.444. [DOI] [PubMed] [Google Scholar]
- 8.Rapoport J, Chavez A, Greenstein D, Addington A, Gogtay N. J Am Acad Child Adolesc Psychiatry. 2009;48:10–18. doi: 10.1097/CHI.0b013e31818b1c63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Itsara A, Cooper GM, Baker C, Girirajan S, Li J, Absher D, et al. Am J Hum Genet. 2009;84:148–161. doi: 10.1016/j.ajhg.2008.12.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Mefford HC, Sharp AJ, Baker C, Itsara A, Jiang Z, Buysse K, et al. N Engl J Med. 2008;359:1685–1699. doi: 10.1056/NEJMoa0805384. [DOI] [PMC free article] [PubMed] [Google Scholar]