Abstract
Background
Asthma exacerbations are a common cause of critical illness in children.
Objective
To determine factors associated with exacerbations in children with persistent asthma.
Methods
Regression modeling was used to identify historical, phenotypic, treatment, and time-dependent factors associated with the occurrence of exacerbations, defined by need for oral corticosteroids, emergency or hospital care in the 48-week Pediatric Asthma Controller Trial (PACT) study. Children aged 6–14 with mild to moderate persistent asthma were randomized to receive either fluticasone propionate 100 mcg BID (FP monotherapy), combination fluticasone 100 mcg AM and salmeterol BID, or montelukast 5 mg once daily.
Results
Of the 285 participants randomized, 48% had 231 exacerbations. Using a multivariate analysis, which included numerous demographic, pulmonary, and inflammatory parameters, only a history of an asthma exacerbation requiring a systemic corticosteroid in the past year (odds ratio 2.10, p<0.001) was associated with a subsequent exacerbation during the trial. During the trial, treatment with montelukast vs. FP monotherapy (OR 2.00, p=0.005), season (spring, fall, or winter vs. summer, p=<0.001), and average seasonal 5% reduction in AM peak expiratory flow (PEF) (OR 1.21, p=0.01) were each associated with exacerbations. Changes in worsening of symptoms, beta-agonist use, and low PEF track together before an exacerbation, but have poor positive predictive value of exacerbation.
Conclusion
Children with mild to moderate persistent asthma with prior exacerbations are more likely to have a repeat exacerbation despite controller treatment. Inhaled corticosteroids are superior to montelukast at modifying the exacerbation risk. Available physiologic measures and biomarkers, and diary card tracking are not reliable predictors of asthma exacerbations.
Keywords: Airway inflammation, Asthma, Bronchial hyperresponsiveness, Childhood asthma, Exacerbations
INTRODUCTION
The natural course of asthma includes episodic deterioration (exacerbations) which can result in missed school days, missed workdays by parents, urgent care or emergency department (ED) visit, hospitalizations, and mortality. In the context of a multi-center trial, children and adults with mild persistent asthma of recent onset were found to be at risk for a severe exacerbation at a 3 year cumulative prevalence of 6.5% and a yearly rate of systemic corticosteroid use of 0.21 per patient.1 Exacerbations even occur despite maintenance use of inhaled corticosteroids as noted in the 4.3 year Childhood Asthma Management Program Study (CAMP) clinical trial in which prednisone use occurred at a rate of 0.70 per patient/year even in a treatment group receiving inhaled corticosteroid, although the rate was 43% less than the placebo group.2 Exacerbations represent a distinct component of patient reported health status3 and one of the major challenges to prevent. Therefore, it is essential to understand the factors that correlate with exacerbations.
The Childhood Asthma Research and Education (CARE) Network’s 1-year randomized multi-center double-blind placebo-controlled clinical trial, Pediatric Asthma Controller Trial (PACT), evaluated the efficacy and safety of three controlled treatment regimens in achieving the best asthma control in children with persistent asthma of mild-moderate severity.4 During the run-in, participants enrolled in the study had minimal or no significant airflow limitation based on forced expiratory volume in 1 second (FEV1) % predicted; moderate to severe bronchial responsiveness to methacholine; modest exhaled nitric oxide (eNO) concentrations; and relatively good asthma control based on the Asthma Control Questionnaire (ACQ) score. PACT provided the opportunity to determine the physiologic, biologic, and temporal variables associated with asthma exacerbations in children with mild to moderate persistent asthma.
METHODS
Details of the PACT study and its procedures have been reported4 and will be briefly summarized. PACT was a multicenter 48-week randomized, double-blind, placebo-controlled, double-dummy, parallel group study of 285 children 6–14 years of age with documented mild-moderate persistent asthma, screening FEV1 ≥ 80% predicted, and methacholine reactivity. Treatments compared were fluticasone propionate 100 mcg twice daily (FP monotherapy); FP 100 mcg/salmeterol 50 mcg in the morning and salmeterol 50 mcg in the evening (PACT combination); montelukast 5 mg in the evening. Spirometric lung function tests (including maximum bronchodilator reversibility), methacholine provocation challenge, and eNO and urinary leukotriene E4 (uLTE4) measurements were performed during each study visit at baseline and serially. Total serum IgE level, peripheral eosinophil count, and serum eosinophil cationic protein (ECP) were obtained at baseline. Electronic peak expiratory flow (PEF) measurements (AM1, Jaeger-Toenies GmbH, Hoechburg, Germany), asthma symptom scores, and albuterol use were recorded manually in diaries twice daily. Adherence to inhaled medication was assessed as detailed elsewhere.4
The Institutional Review Board of the five CARE clinical centers and the Data Coordinating Center approved the study. Parents/guardians provided informed consent, with verbal assent given by children less than 7 years of age, and written assent from older children.
An asthma exacerbation was defined for this analysis as the development of acute asthma requiring systemic corticosteroids or emergency care (ED visit or hospitalization). This is a broader definition than was used for the primary analysis in which exacerbations did not include emergency care not associated with a prednisone course.4 The resulting inclusion of 2 participants who went to the ED but did not receive prednisone, did not affect the results found in this cohort with low rate of emergency care utilization. Initiation of oral prednisone therapy was based on specific guidelines or on physician discretion.4 The guidelines for initiating a prednisone course were use of > 12 puffs of albuterol in 24 hours (excluding preventive use before exercise) for diary card symptom code of 3 or PEF less than 70% of personal best before each albuterol use; diary symptom code of 3 (the most severe code) for > 48 hours or longer; or PEF dropped to less than 50% of personal best despite albuterol treatment or physician discretion.4
Statistical Analysis
Regression modeling was used to investigate associations between the occurrence of exacerbations and characteristics before randomization, treatment assignment, and time-dependent factors. A longitudinal data framework was constructed whereby the calendar year was divided into four seasons: June–August (Summer), September–November (Fall), December–February (Winter) and March–May (Spring). In this way each participant contributed 4 data points to the analysis, one from each season. The response variable in the regression models was the presence or absence of an exacerbation during each season. The longitudinal independent variables in the regression models were defined as changes from baseline. Measurements that were obtained on a daily basis (e.g. morning and evening PEF and PEF variability) were summarized for each participant as seasonal averages and defined as percentage decrease from baseline (2-week run-in period average) in order to standardize subjects relative to their pre-treatment levels. For example, if a child’s baseline PEF was 300 li/min and his average PEF from June through August was 270 li/min, then his Summer PEF decrease from baseline would be 10%. The eNO measurements taken at clinic visits were also summarized as seasonal averages over the visits that occurred during that season.
Logistic regression analysis was then applied using the generalized estimating equations approach to account for statistical dependence induced by the longitudinal nature of the data. A structured modeling building algorithm was employed in this exploratory analysis. Univariate regression models including each of the baseline and seasonal measures were first used to narrow the list of covariates (statistically significant at p < 0.05) to be incorporated into the final multivariate model.
It is important to note that exacerbations could occur at any point during a given season. If an exacerbation occurred near the end of the season, then the data values for the independent variables were comprised mainly of information collected prior to the exacerbation. However, if an exacerbation occurred near the beginning of the season, then the data values for the independent variables were comprised mainly of information collected after the exacerbation. Thus, the longitudinal variables represent circumstances that were temporally near, but not necessarily preceding, exacerbations and the results of the regression model should be interpreted as indications of associations with, rather than predictions of, exacerbations. Distinct exacerbations were defined as those occurring at least 6 days apart. There were 5 exacerbations that occurred within 2 weeks of the previous and 19 that occurred within 4 weeks of the previous. However, only 4 of those had any effect on the results because of the way our model is defined. As a result, the sensitivity analysis revealed that it did not make any difference to the results of our model. Twenty-five percent of second and third exacerbations occurred within 35 days of the previous and 50% within 67 days.
In order to explore the predictive value of daily diary data, an analysis focused on changes in symptoms, bronchodilator rescue use, and PEF immediately preceding exacerbations was also done. Asthma symptoms, including cough and wheeze, use of albuterol for rescue, and PEF percent of personal best were examined alone and in combination. These variables were chosen because they were used to guide the subject’s asthma action plan during the study. Four separate analyses were done to assess predictive value for imminent exacerbations: 3 days prior, 2 days prior, the day before and the day of initiation of corticosteroid or ED visit. All days more than 2 weeks prior to, or 2 weeks after, exacerbations were considered to be not associated with exacerbations and “negative” days. In each analysis there was only one “positive” day for each exacerbation (i.e., 3, 2, 1 or 0 days prior to initiation). Separate receiver operating characteristic (ROC) curves of the various signals were plotted for each positive and area under the ROC curve (AROCC) calculated. AROCC can be interpreted as the probability that a randomly selected “positive” day will have a worse value (higher symptoms/rescue use or lower PEF) than a randomly selected “negative” day. The best possible AROCC, 1.0, indicates a perfect signal which is always present on a positive day and never present on a negative day. The worst possible AROCC, 0.5, corresponds to a “coin-flip” signal which is just as likely to be present on a positive day as on a negative day.
RESULTS
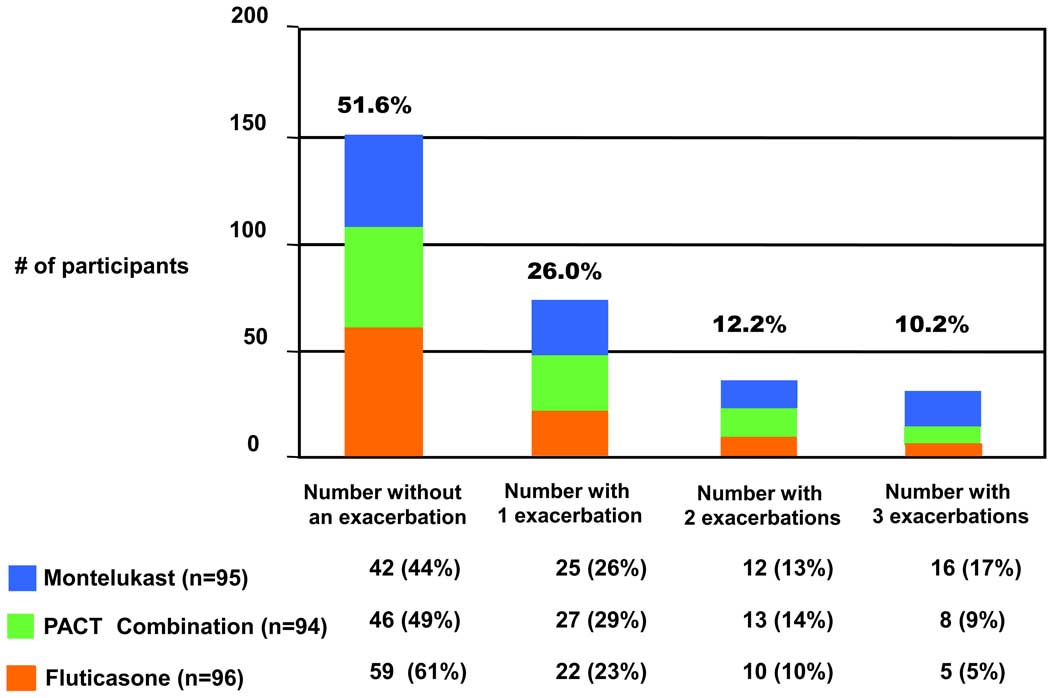
A total of 231 asthma exacerbations occurred in 48% of the participants during the course of the treatment phase. Twenty two percent (n= 64) had 2 or more exacerbations. (Figure 1) Of the exacerbations, 74 (53%), 35 (26%), and 29 (21%) were 1st, 2nd, and 3rd exacerbations, respectively. The mean±SD (median) time to the first exacerbation was 127±103 (99) days.
Figure 1.
Number of participants in the Pediatric Asthma Controller Trial with no, one, two, three exacerbations in each treatment group. 48% had at least one exacerbation and 22% had more than one exacerbation: Fewer participants in the FP monotherapy group developed an asthma exacerbation during the trial, compared to those who were treated with montelukast (p=0.009 FP monotherapy vs montelukast, p=0.09 FP monotherapy vs PACT combination, p=0.2 PACT combination vs montelukast).
Univariate analyses
Univariate logistic regression analyses were performed to identify variables before randomization and during the trial predictive of an exacerbation (Table I).
Table I.
Logistic regression analysis of factors at baseline and during the PACT trial treatment predictive of an exacerbation
| Unadjusted OR (95% CI) | P value | ||
|---|---|---|---|
| Baseline factors | |||
| Gender, Female vs. Male | 1.22 (0.85, 1.74) | 0.28 | |
| Race, Caucasian vs. NonCaucasian | 1.20 (0.76, 1.90) | 0.43 | |
| Any positive skin test, none vs. yes | 1.03 (0.66, 1.59) | 0.9 | |
| Smoke exposure, no vs. yes | 1.05 (0.67,1.67) | 0.51 | |
| Presence of pet(s) in the home | 0.77 (0.54,1.10) | 0.15 | |
| Prednisone course in the past year, none vs. any | 2.28 (1.59, 3.26) | 0.0001 | |
| Age at randomization, years | 0.89 (0.83, 0.97) | 0.007 | |
| Age at diagnosis of asthma, years | 0.94 (0.88, 0.99) | 0.03 | |
| Asthma control questionaire (ACQ) score | 1.20 (0.89, 1.63) | 0.24 | |
| FEV1 % predicted | 1.01 (0.99, 1.02) | 0.37 | |
| FEV1/FVC, ratio %predicted | 1.01 (0.99, 1.04) | 0.29 | |
| Maximum bronchodilator response, % | 1.02 (1.00, 1.04) | 0.09 | |
| FEV1 log2 PC20, mg/ml | 1.04 (0.94, 1.14) | 0.45 | |
| Exhaled nitric oxide, log10 ppb | 0.93 (0.60, 1.45) | 0.76 | |
| Urinary leukotriene E4, log10 pg/mg creatinine | 1.08 (0.51, 2.26) | 0.85 | |
| Serum IgE, log10 ku/li | 1.15 (0.90, 1.48) | 0.25 | |
| Eosinophil count, log10 % of white blood cells | 1.38 (0.84, 2.27) | 0.20 | |
| Eosinophil cationic protein, log10 mcg/li | 1.16 (0.80,1.69) | 0.43 | |
| Treatment factors | |||
| Treatment group | |||
| Montelukast | 1.91 (1.24, 2.95) | 0.003 | |
| PACT combination | 1.51 (0.97, 2.34) | 0.066 | |
| FP monotherapy | 1.00 | . | |
| Season | |||
| Spring | 2.28 (1.41, 3.67) | 0.0007 | |
| Winter | 2.28 (1.38, 3.75) | 0.0013 | |
| Fall | 3.12 (1.95, 4.99) | <0.0001 | |
| Summer | 1.00 | ||
| Exhaled nitric oxide (log10 change from baseline)* | 1.97 (1.13, 3.44) | 0.02 | |
| AM PEF (% drop from baseline)** | 1.22 (1.02, 1.46) | 0.03 | |
| PM PEF (% drop from baseline)** | 1.17 (0.99, 1.39) | 0.06 | |
Exacerbations defined as increased asthma activity requiring prednisone courses, emergency department visits, and hospitalizations. The univariate model included all candidate baseline predictors and time-dependent variables such as treatment, season, and seasonal exhaled nitric oxide and peak flow values. The eNO and PEF values are 3-month averages and then subtracted from the baseline average. In the univariate analysis, one log10-fold change in exhaled nitric oxide during the season when the exacerbation occurred corresponded to 97% increased odds of having an exacerbation. A 5% drop in AM PEF average from baseline during the season when the exacerbation occurred translated into a 22% higher risk of a subsequent exacerbation.
Factors prior to randomization associated with an exacerbation
A prior history of an exacerbation requiring a corticosteroid course (odds ratio 2.28, p=0.0001) was the most significant factor. Younger age and earlier age of asthma diagnosis were also associated with a higher risk of an exacerbation (p=0.007 and p=0.03, respectively). No other biologic or physiologic marker before randomization was associated with exacerbation risk. (Table I)
Factors during the trial associated with the occurrence of exacerbations
The impact of treatment on the risk of exacerbation was evaluated in various ways. The rates of exacerbations per patient year were 1.0 for montelukast, 0.8 for PACT combination, and 0.6 for FP monotherapy (p=0.01). Treatment with montelukast vs. FP monotherapy increased the odds of an exacerbation by almost 2 times (odds ratio 1.91, p=0.003); but treatment with PACT combination was not significantly different from either montelukast or FP monotherapy. (Table I) More than half of the participants in either the montelukast (56%) or PACT combination (51%) groups, while only 39% in the FP monotherapy group developed at least one exacerbation during the trial (p=0.004 montelukast vs FP monotherapy, p=0.09 FP monotherapy vs PACT combination, p=0.2 montelukast vs PACT combination). One or 2 exacerbations occurred equally in the three treatment groups. However, 55% of children with 3 exacerbations were from the montelukast group, 27% from the PACT combination, and only 17% from the FP monotherapy (p=0.21 PACT combination vs montelukast, p=0.6 PACT combination vs FP monotherapy, p=0.04 montelukast vs FP monotherapy). Over twice as many ED/urgent care visits for exacerbations were reported in the montelukast groups (n= 26) and the PACT combination (n= 28) compared to the FP monotherapy (n= 10) (p=0.7 PACT combination vs montelukast, p<0.001 PACT combination vs FP monotherapy, p=0.003 montelukast vs FP monotherapy.
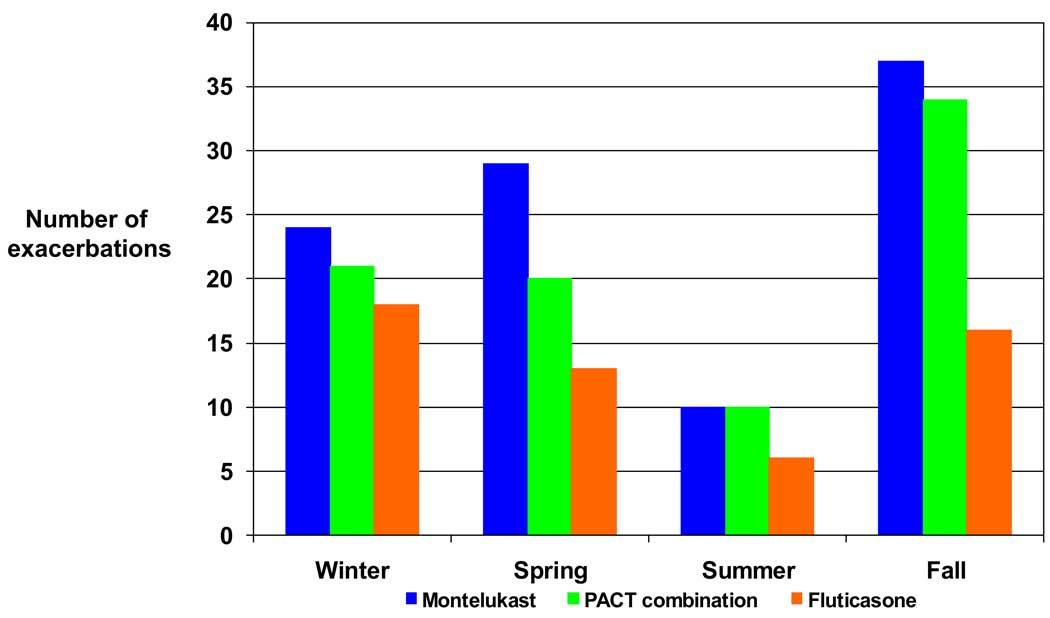
Exacerbations were seasonally related, i.e. they were 2.3 times more likely to occur in the spring (p<0.001) or winter (p=0.001) and 3.1 times more likely in the fall (p<0.0001) compared to the summer months. (Table 1 and Figure 2)
Figure 2.
Number of exacerbations in the winter (Dec–Feb), spring (Mar–May), summer (June–Aug), and fall (Sept–Nov) months Exacerbations were more likely to occur in the spring (p<0.001) or winter (p=0.001) or fall (p<0.0001) compared to the summer months.
During the treatment phase, changes in eNO and PEF from baseline were associated with an exacerbation. (Table I) The eNO increase is on the log10-scale and one log-fold increase corresponds to an odds ratio of 1.97 (p = 0.02). AM and PM PEF are expressed as average drop in AM and PM PEF, respectively, over the entire season. In this analysis, a 5% drop in average AM PEF is associated with a 1.22 increased odds of exacerbations (p=0.03).
Multivariate analyses of factors associated with exacerbations
Of the significant factors before randomization, only a history of an exacerbation in the year prior to study was independently related to an exacerbation during the study (p = 0.001). (Table II) During the course of the study, treatment group (montelukast vs. FP monotherapy; p<0.001), season (any season vs. summer) (p=0.0002), and a reduction in average AM PEF over the season (p= 0.01) were all associated with exacerbations. The interaction of season and treatment group was not significant so that exacerbations were likely to occur in any season other than summer regardless of treatment. The treatment group by AM PEF change interaction effect was also not significant. In the multivariate model, the effects of age, eNO and PM PEF were no longer significant.
Table II.
Multivariable model of factors associated with exacerbations
| Variable | Odds Ratio 95% CI | Level p-value | |
|---|---|---|---|
| Baseline factors | |||
| Prednisone course in the year prior to study | 2.10 (1.42, 3.09) | 0.0008 | |
| Age, years | 0.93 (0.85, 1.01) | 0.1 | |
| Treatment factors | |||
| Treatment group | 0.019 | ||
| Montelukast | 2.00 (1.23, 3.24) | 0.005 | |
| PACT combination | 1.51 (0.92, 2.50) | 0.1 | |
| FP monotherapy | 1.00 | ||
| Season | 0.0002 | ||
| Spring | 2.53 (1.50, 4.27) | 0.0005 | |
| Winter | 2.17 (1.24, 3.81) | 0.007 | |
| Fall | 3.01 (1.75, 5.18) | <0.0001 | |
| Summer | 1.00 | ||
| AM PEF (% decrease from baseline) | 1.21 (1.01, 1.45) | 0.01 | |
| Exhaled nitric oxide (log10 change from baseline) | 1.37 (0.72, 2.57) | 0.4 | |
Exacerbations defined as increased asthma activity requiring prednisone courses, emergency department visits, and hospitalizations. The multivariate model included variables significant in the univariate analyses at p<0.1. The eNO and PEF values are 3-month averages and then subtracted from the baseline average. In the model, a 5% drop in AM PEF average from baseline during the season when the exacerbation occurred translated into a 22% higher risk of a subsequent exacerbation.
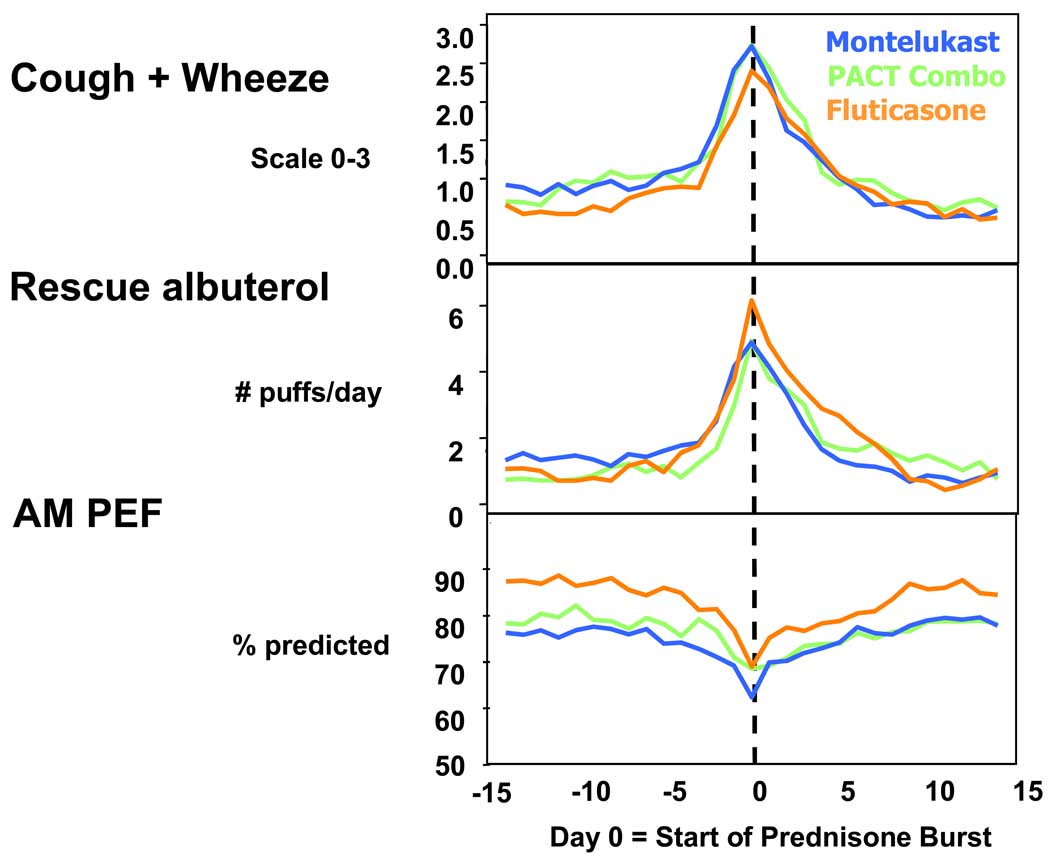
Relationship of daily asthma diary monitoring to exacerbations
The patterns of changes in morning PEF, symptom score, and albuterol use in each treatment group before and after an exacerbation are depicted in Figure 1. Gradual concurrent changes in cough and wheeze scores, albuterol rescue use, and PEF were evident between 12 to 3 days before an exacerbation and more abruptly within the 2 days prior, with not one parameter occurring earlier than others. The outcome measures (symptoms, albuterol rescue use, symptoms, and peak flows) returned to baseline level within a maximum period of ten days. This trend was apparent regardless of treatment.
Based on diary card documentation, the percentages of participants in each treatment group who reported any of the following were determined: a 2 level increase in symptom score, a 20% PEF reduction, or albuterol rescue use of at least 8 inhalations per day. By the time the patients were considered to be exacerbating, 57% in the montelukast, 70% in the PACT combination, and 51% in the FP monotherapy group reported recent changes in any of these signals. (eFigure 1) One day before the exacerbation was considered, the sensitivities of these recent changes were lower in each treatment group (49, 49, and 45%). Other important observations were higher documented recent changes in PEF reduction, worsening symptoms, and frequent albuterol use in participants from the montelukast and PACT combination groups even several days before and after Day 0. (eTable 1) Although the sensitivities of the signals based on diary card tracking are consistently low, PEF reduction was most sensitive although less specific compared to symptom score and albuterol use. Poor positive and negative predictive values for each PEF reduction, albuterol rescue use, and symptoms, were found, regardless of treatment assignment. (eTables 2 & 3)
Using AROCC, the relative utility of the PEF reduction, symptom score, and albuterol use, singly and in combination, as signals of an imminent exacerbation was determined. (Table III) The AROCCs for symptoms, PEF reduction, and albuterol rescue increased as the time to exacerbation shortened. The AROCCs for symptoms were higher than for PEF or albuterol use on the day of and days leading to an exacerbation, and there was only modest improvement on the AROCCs when PEF and/or albuterol use was combined with symptom score. Of note, even on day 0, none of the AROCCs were particularly high. These patterns were found in all treatment groups. (Table III)
Table III.
Area under the Receiver Operating Characteristic curve (AROCC) values for diary monitoring on 3 consecutive lag days prior to day 0 of an exacerbation
| TOTAL | MONTELUKAST | PACT COMBINATION | FP MONOTHERAPY | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Day/s before exacerbation | 3 | 2 | 1 | 0 | 3 | 2 | 1 | 0 | 3 | 2 | 1 | 0 | 3 | 2 | 1 | 0 |
| Symptoms | 0.66 | 0.72 | 0.83 | 0.85 | 0.60 | 0.74 | 0.86 | 0.83 | 0.71 | 0.73 | 0.86 | 0.88 | 0.58 | 0.67 | 0.76 | 0.80 |
| Albuterol rescue use | 0.57 | 0.68 | 0.78 | 0.83 | 0.65 | 0.68 | 0.79 | 0.80 | 0.56 | 0.59 | 0.74 | 0.85 | 0.63 | 0.71 | 0.80 | 0.78 |
| PEF | 0.60 | 0.68 | 0.73 | 0.77 | 0.66 | 0.71 | 0.72 | 0.73 | 0.51 | 0.61 | 0.71 | 0.80 | 0.54 | 0.68 | 0.73 | 0.74 |
| Symptoms and albuterol rescue use | 0.68 | 0.75 | 0.86 | 0.88 | 0.65 | 0.76 | 0.86 | 0.85 | 0.71 | 0.75 | 0.86 | 0.90 | 0.59 | 0.72 | 0.84 | 0.86 |
| Symptoms and PEF | 0.66 | 0.73 | 0.82 | 0.86 | 0.71 | 0.76 | 0.82 | 0.81 | 0.58 | 0.67 | 0.80 | 0.88 | 0.59 | 0.71 | 0.81 | 0.87 |
| Albuterol rescue use and PEF | 0.65 | 0.71 | 0.77 | 0.82 | 0.69 | 0.73 | 0.79 | 0.79 | 0.55 | 0.62 | 0.74 | 0.84 | 0.62 | 0.71 | 0.77 | 0.81 |
| Symptoms, albuterol rescue use, and PEF | 0.68 | 0.75 | 0.84 | 0.87 | 0.72 | 0.78 | 0.85 | 0.81 | 0.61 | 0.68 | 0.84 | 0.88 | 0.62 | 0.71 | 0.82 | 0.91 |
All days more than 2 weeks prior to, or 2 weeks after exacerbations were considered to be days not associated with the exacerbation. Receiver operating characteristic (ROC) curves of the various predictors were plotted for each day separately and area under the ROC curve (AROCC) calculated. AROCC can be interpreted as the probability that a randomly selected lag day prior to an exacerbation will have a worse value (higher symptoms/rescue use or lower PEF) than a randomly selected day not associated with the exacerbation.
DISCUSSION
Our analysis of asthma exacerbations of children with mild to moderate asthma enrolled in the PACT 1-year multi-center trial using an extensive panel of physiologic and biologic markers revealed important features associated with the occurrence of an exacerbation.
Host and environmental factors that increase the risk of asthma exacerbations in children and those which could be targeted by interventions are not well defined. Of the numerous baseline historical, phenotypic, and immunologic and atopic characteristics analyzed in this study, younger age, earlier age at asthma diagnosis, and a prior history of an exacerbation requiring a systemic corticosteroid course were found to be risk factors in the univariate analysis. A multivariable regression model was used to determine whether these factors were independently predictive of exacerbation risk. These results indicated that prior history of exacerbations was the most important risk factor. Although the association between prior exacerbation and its recurrence is consistent with other studies 3, 5–9, our study evaluated many other physiologic and biologic markers in the model (atopy, allergen sensitization, smoking exposure, lung function measures, bronchial hyperresponsiveness, inflammatory markers) and none was significantly associated with the occurrence of an exacerbation in this trial.
There are aspects of an exacerbation risk which can be tracked and modified by specific treatment. According to current asthma guidelines10, controller therapy for persistent asthma preferably inhaled corticosteroids, is recommended to reduce the risk of exacerbations. In PACT, the number of prednisone courses for children receiving inhaled corticosteroid monotherapy (0.6 per patient year) was comparable to that for children who received budesonide in the CAMP trial. 2 These exacerbation rates were within the acceptable level proposed in the National Asthma Education and Prevention Program: Expert Panel Report 3 (i.e. less than 2 exacerbations per year). 10 In this paper, we have extended several findings highlighted in the original PACT paper with respect to superiority of inhaled corticosteroid over a leukotriene receptor antagonist using other features of an exacerbation as an outcome. Compared to a leukotriene receptor antagonist, inhaled corticosteroid not only increased the time to first prednisone course (p=0.0002)4 but also reduced the rate of overall exacerbations and the number of emergent care visits by 40 to 50%. A favorable effect of inhaled corticosteroid monotherapy over PACT combination with respect to a lower rate of exacerbations and lower urgent care/ED visits was also found. In the original paper4, FP monotherapy and PACT combination had comparable effects on symptom control and time to first exacerbation,4 but other advantages of FP monotherapy over PACT combination in regard to improvements in lung function, eNO, and bronchial hyperresponsiveness were shown. Given these findings and the lack of differences in growth effects among the 3 treatment groups reported in the main PACT paper, low dose inhaled corticosteroid twice a day would be considered the preferred treatment for persistent asthma in regard to modifying the exacerbation risk.
Despite active intervention and excellent adherence to study drugs and diary card recording (i.e. adherence to study medications estimated from the Diskus® dose counter was 90% and from an Electronic Drug Exposure Monitor [eDEM®] tablet use records was 86%)4, almost half of the participants still developed an asthma exacerbation. Furthermore, about one in five children would be considered having uncontrolled asthma based on exacerbation risk criteria proposed in the current asthma guidelines (i.e. ≥ 2 exacerbations per year). 10 Hence, it is essential to find better strategies to further reduce this risk in these susceptible patients. Preventing asthma exacerbations is a major goal in the management of asthma because of the associated health risks and economic burden.
During the study, along with treatment, season and change in PEF are associated with exacerbations in a multivariate longitudinal model. Exacerbations were more likely to occur at the other seasons compared to summer, with the greatest occurrence in the fall, consistent with other studies. 11–14 The impact of season on the occurrence of exacerbation could be due to allergen or irritant (e.g. smoke and pollutant) exposure, or viral respiratory infections. In a recent case control study, the combination of both sensitization and exposure to sensitizing allergen plus viral infection was an independent risk for a hospital admission from asthma exacerbation.15 Our study highlights the independent effects of specific individual asthma patterns (i.e., history of exacerbations), treatment, and season in a three arm long-term treatment trial.
In the univariate regression analyses, other time-dependent characteristics associated with an exacerbation were changes in seasonal AM and PM PEF and eNO concentrations. (Table I) However, in the multivariate longitudinal model, once season and/or treatment effects were in the model, eNO was no longer associated with occurrence of an exacerbation. Several other analyses in this study were performed to look for an association between eNO and exacerbation. Only 15% of the exacerbations occurred within 2 weeks of a clinic visit when an eNO was obtained. The eNO concentrations were lower in the FP monotherapy group compared to the PACT combination and montelukast groups, but low correlations (close to zero) in each treatment group were found between eNO obtained at study visits and time before an exacerbation (data not shown). Not only was eNO modified by treatment, but it also varied across the seasons using a stratified analysis. Therefore, the approach expressing change in eNO as seasonal average in the longitudinal models was used. Again, once we accounted for season and treatment, eNO determined at study visits was no longer associated.
The analysis approach we used revealed seasonal associations between covariates and exacerbations at the population level, but cannot be used to infer predictive value, in the temporal sense, of exacerbations at the subject level. For example, an average seasonal reduction in AM PEF was found to be associated with an exacerbation, although the magnitude of the PEF effect and its clinical relevance are difficult to assess on a subject level. Over a 90-day average, a drop of 5% was associated with a 22% increased risk of exacerbation.
Warning signs of an exacerbation obtained from diary card information only manifest themselves when the exacerbation is very imminent, one day or less. Our pediatric study parallels the findings of Tattersfield et al that similar patterns of changes in symptom score, PEF, and bronchodilator rescue use occurred prior to and during exacerbation in an adult asthma clinical trial.16 In addition, peak flow monitoring did not enhance the predictive value for an exacerbation relative to symptoms alone. Recent evidence also supports the limited applicability of home lung function monitoring in gauging asthma activity.17,18 The limited sensitivities and predictive values of symptoms, short acting-beta-agonist rescue use, and changes in PEF alone or in combination, suggest that there may be additional factors that may reliably predict the onset of an exacerbation. None of the factors was convincing enough to make decisions given the planned logistics which were used to initiate prednisone in this clinical trial. Perhaps intervening aggressively under close medical supervision in the setting of a clinical trial reduced the power to determine this relationship. Studies in which intervention was not proactive to prevent exacerbations would probably have the capacity to better examine the associations between changes in diary card information and risk of an imminent exacerbation. Serial measures of airway inflammation may offer more sensitive real-time predictors for exacerbations, as has been suggested with other surrogate markers of disease activity including daily eNO monitoring.19 Although speculative, it is also possible that a combination of real-time measurements of airway inflammation (ie. eNO) with airflow and symptoms may have better ability to predict an exacerbation long before the occurrence of an exacerbation.20
In summary, our analysis of exacerbations in children with mild to moderate persistent asthma in a multi-center clinical trial suggests that children with prior exacerbations requiring a systemic course of corticosteroids are at high risk for future exacerbations, despite the use of long-term controller therapy. This marker of disease severity identifies a distinct asthma phenotype characterized by an exaggerated host response to common triggers that deserves further investigation for mechanisms. While exacerbation risk can be reduced by treatment, specifically inhaled corticosteroids, better indicators are needed to predict an imminent exacerbation.
Supplementary Material
Figure 3.
Plots of cough/wheeze severity score (scale 0–3), rescue albuterol rescue use (# inhalations per day), and AM PEF as % predicted of participants in the montelukast,
montelukast,  PACT combination, and
PACT combination, and  FP monotherapy groups, relative to an exacerbation.
FP monotherapy groups, relative to an exacerbation.
Acknowledgments
Supported by:
Grants 5U10HL064287, 5U10HL064288, 5U10HL064295, 5U10HL064307, 5U10HL064305, 5U10HL064313 from the National Heart, Lung, and Blood Institute; General Clinical Research Centers at Washington University School of Medicine (M01 RR00036) and National Jewish Medical and Research Center (M01 RR00051).
Abbreviations
- ACQ
Asthma Control Questionnaire
- AROCC
Area under the Receiver Operating Characteristic Curve
- BHR
Bronchial hyperresponsiveness
- CAMP
Childhood Asthma Management Program
- CARE
Childhood Asthma Research and Education
- ED
Emergency department
- ENO
Exhaled nitric oxide
- FEV1
Forced expiratory volume in 1 second
- FVC
Forced vital capacity
- PACT
Pediatric Asthma Controller Trial
- PEF
Peak expiratory flow
- PC20
Concentration of methacholine which provokes a 20% drop in FEV1
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Clinical implications
While exacerbation risk can be reduced by treatment, specifically inhaled corticosteroids, better indicators are needed to predict and thus prevent asthma exacerbations.
References
- 1.Pauwels RA, Pedersen S, Busse WW, Tan WC, Chen YZ, Ohlsson SV, et al. Early intervention with budesonide in mild persistent asthma: a randomised, double-blind trial. Lancet. 2003;361:1071–1076. doi: 10.1016/S0140-6736(03)12891-7. [DOI] [PubMed] [Google Scholar]
- 2.CAMP. Long-term effects of budesonide or nedocromil in children with asthma. Childhood Asthma Management Program Research Group. N Engl J Med. 2000;343:1054–1063. doi: 10.1056/NEJM200010123431501. [DOI] [PubMed] [Google Scholar]
- 3.Schatz M, Mosen D, Apter AJ, Zeiger RS, Vollmer WM, Stibolt TB, et al. Relationships among quality of life, severity, and control measures in asthma: an evaluation using factor analysis. J Allergy Clin Immunol. 2005;115:1049–1055. doi: 10.1016/j.jaci.2005.02.008. [DOI] [PubMed] [Google Scholar]
- 4.Sorkness CA, Lemanske RF, Jr, Mauger DT, Boehmer SJ, Chinchilli VM, Martinez FD, et al. Long-term comparison of 3 controller regimens for mild-moderate persistent childhood asthma: The Pediatric Asthma Controller Trial. J Allergy Clin Immunol. 2007;119:64–72. doi: 10.1016/j.jaci.2006.09.042. [DOI] [PubMed] [Google Scholar]
- 5.Rasmussen F, Taylor DR, Flannery EM, Cowan JO, Greene JM, Herbison GP, et al. Risk factors for hospital admission for asthma from childhood to young adulthood: a longitudinal population study. J Allergy Clin Immunol. 2002;110:220–227. doi: 10.1067/mai.2002.125295. [DOI] [PubMed] [Google Scholar]
- 6.Lieu TA, Quesenberry CP, Sorel ME, Mendoza GR, Leong AB. Computer-based models to identify high-risk children with asthma. Am J Respir Crit Care Med. 1998;157:1173–1180. doi: 10.1164/ajrccm.157.4.9708124. [DOI] [PubMed] [Google Scholar]
- 7.Farber HJ. Risk of readmission to hospital for pediatric asthma. J Asthma. 1998;35:95–99. doi: 10.3109/02770909809055410. [DOI] [PubMed] [Google Scholar]
- 8.Farber HJ, Johnson C, Beckerman RC. Young inner-city children visiting the emergency room (ER) for asthma: risk factors and chronic care behaviors. J Asthma. 1998;35:547–552. doi: 10.3109/02770909809048957. [DOI] [PubMed] [Google Scholar]
- 9.McCoy K, Shade DM, Irvin CG, Mastronarde JG, Hanania NA, Castro M, Anthonisen NR. American Lung Association Asthma Clinical Research Centers. Predicting episodes of poor asthma control in treated patients with asthma. J Allergy Clin Immunol. 2006 Dec;118:1226–1233. doi: 10.1016/j.jaci.2006.09.006. [DOI] [PubMed] [Google Scholar]
- 10.National Asthma Education and Prevention Program: Expert Panel Report 3 (EPR 3): Guidelines for the Diagnosis and Management of Asthma—Summary Report 2007. J Allergy Clin Immunol. 2007;120 Suppl:S94. doi: 10.1016/j.jaci.2007.09.043. [DOI] [PubMed] [Google Scholar]
- 11.Gergen PJ, Mitchell H, Lynn H. Understanding the seasonal pattern of childhood asthma: results from the National Cooperative Inner-City Asthma Study (NCICAS) J Pediatr. 2002;141:631–636. doi: 10.1067/mpd.2002.127510. [DOI] [PubMed] [Google Scholar]
- 12.Reeves MJ, Lyon-Callo S, Brown MD, Rosenman K, Wasilevich E, Williams SG. Using billing data to describe patterns in asthma-related emergency department visits in children. Pediatrics. 2006;117:S106–S117. doi: 10.1542/peds.2005-2000H. [DOI] [PubMed] [Google Scholar]
- 13.Silverman RA, Stevenson L, Hastings HM. Age-related seasonal patterns of emergency department visits for acute asthma in an urban environment. Ann Emerg Med. 2003;42:577–586. doi: 10.1067/s0196-0644(03)00410-4. [DOI] [PubMed] [Google Scholar]
- 14.Silverman RA, Ito K, Stevenson L, Hastings HM. The relationship of fall school opening and emergency department asthma visits in a large metropolitan area. Arch Pediatr Adolesc Med. 2005;159:818–823. doi: 10.1001/archpedi.159.9.818. [DOI] [PubMed] [Google Scholar]
- 15.Murray CS, Poletti G, Kebadze T, Morris J, Woodcock A, Johnston SL, et al. Study of modifiable risk factors for asthma exacerbations: virus infection and allergen exposure increase the risk of asthma hospital admissions in children. Thorax. 2006;61:376–382. doi: 10.1136/thx.2005.042523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Tattersfield AE, Postma DS, Barnes PJ, Svensson K, Bauer CA, O'Byrne PM, et al. Exacerbations of asthma: a descriptive study of 425 severe exacerbations. The FACET International Study Group. Am J Respir Crit Care Med. 1999;160:594–599. doi: 10.1164/ajrccm.160.2.9811100. [DOI] [PubMed] [Google Scholar]
- 17.Brouwer AF, Roorda RJ, Brand PL. Home spirometry and asthma severity in children. Eur Respir J. 2006;28:1131–1137. doi: 10.1183/09031936.06.00118205. [DOI] [PubMed] [Google Scholar]
- 18.Buist AS, Vollmer WM, Wilson SR, Frazier EA, Hayward AD. A randomized clinical trial of peak flow versus symptom monitoring in older adults with asthma. Am J Respir Crit Care Med. 2006;174:1077–1087. doi: 10.1164/rccm.200510-1606OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Pijnenburg MW, Floor SE, Hop WC, De Jongste JC. Daily ambulatory exhaled nitric oxide measurements in asthma. Pediatr Allergy Immunol. 2006;17:189–193. doi: 10.1111/j.1399-3038.2006.00394.x. [DOI] [PubMed] [Google Scholar]
- 20.Gelb AF, Flynn Taylor C, Shinar CM, Gutierrez C, Zamel N. Role of spirometry and exhaled nitric oxide to predict exacerbations in treated asthmatics. Chest. 2006;129:1492–1499. doi: 10.1378/chest.129.6.1492. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.