Abstract
Objective
Determination of skeletal age is essential for predicting eventual leg length discrepancies and predicting the accurate timing for surgical intervention in order to correct any discrepancy. To our knowledge, there has not been an interdisciplinary comparison of the degree of agreement in determining skeletal bone age.
Materials and methods
We evaluated 30 left hand/wrist radiographs (children aged 16 months to 10 years 6 months) on two separate occasions between musculoskeletal paediatric radiologists, paediatric orthopaedic surgeons and a senior radiographer after appropriate training.
Results
All clinicians were able to reliably age patients with good intra- and interobserver agreement.
Conclusion
We suggest that following tuition, orthopaedic surgeons are able to reliably age patients from X-rays.
Keywords: Bone age measurement, Radiology teaching, Orthopaedic training
Introduction
Accurate bone age assessment is necessary for leg length equalisation surgery with epiphysiodesis [1]. Skeletal bone age estimation by comparing radiographs of patients to an atlas of standard radiographs is a common approach.
The Greulich and Pyle [2] atlas consists of radiographs of the left hand and wrists of boys and girls considered typical of the stated skeletal age. The Tanner–Whitehouse [3] method also uses radiographs of the hand and wrist, but was developed using computerised mathematical procedures.
Several methods of data analysis have evolved for determining the timing of surgical intervention to correct leg length discrepancy. These include the arithmetic method first described by White and then evaluated by Menelaus and Westh [4, 5], the growth remaining method by Green and Anderson [6, 7], the multiplier method by Paley et al. [8], and the straight line graph method by Green and Anderson [9]. More recently, Eastwood and Cole [10] designed a graphical method for determining the timing of epiphysiodesis.
Bone age assessment can be laborious. It is usually radiologists who report on skeletal bone age. We wondered if other specialties could learn to be as accurate at assessing bone age based on the Greulich and Pyle atlas for skeletal bone age determination, so that paediatric orthopaedic surgeons could take ownership of the bone age assessment. Time and financial savings might be achieved if orthopaedic clinicians were able to assess bone age without the requirement for a radiologist.
Method
Five investigators were recruited for the study. These were a consultant paediatric musculoskeletal radiologist, a consultant paediatric orthopaedic surgeon, a senior paediatric orthopaedic fellow, a radiology registrar and a senior radiographer at a specialist Children’s Hospital (Sheffield Children’s Hospital).
Training for the orthopaedic surgical team, the radiology registrar and the senior radiographer was performed by the consultant paediatric musculoskeletal radiologist. Standard left-hand radiographs for bone age assessment were used and compared to the Greulich and Pyle atlas. One morning (3 h) interactive session was employed where various subtleties were pointed out in order to make the bone assessment more accurate.
Thirty standard left hand and wrist radiographs of children who required bone age assessments were used for the study. The 30 standard radiographs included 15 male and 15 female subjects. The age range was from 13 months to 15.5 years. Thirty radiographs were used as a convenient though substantial number to examine the participants, although a formal power calculation was not performed. Two assessments of the set of 30 radiographs were performed by each investigator in a “blinded” manner at a 2-week interval. In between the intervals, the radiographs were randomised.
After consultation with a statistician, two methods were used to assess rater reliability of bone age reporting between the different specialities of orthopaedics and radiology. Intraclass correlation coefficients (ICC) were used to analyze the intra- and interrater reliability. A value of 1 indicates perfect intra- or interrater reliability. The pairedt-test and Bland–Altman plots were used to test the validity.
Results
Intrarater reliability
All five participants had excellent correlation (ICC > 0.94) between their first and second attempts. Within this, the consultant radiologist had the best intraclass correlation coefficient of 0.993 (95% CI: 0.986–0.997). The consultant orthopaedic surgeon had the least good, with 0.947 (95% CI: 0.893–0.974) (Table 1).
Table 1.
Intraclass correlation coefficients for intrarater reliability
| Intraclass correlation coefficient | 95% confidence interval | ||
|---|---|---|---|
| Lower | Upper | ||
| Ortho cons | .947 | .893 | .974 |
| Ortho Snr fellow | .983 | .965 | .992 |
| Radiol cons | .993 | .986 | .997 |
| Radiol spr | .985 | .970 | .993 |
| Radiographer | .989 | .977 | .995 |
Interrater reliability
The consultant radiologist delivered the teaching and was considered to be the most able participant to perform the bone aging. Therefore, the scores of the other participants were compared with his score. Table 2 demonstrates that the interrater reliability was excellent, with all ICCs greater than 0.94.
Table 2.
Intraclass correlation coefficient for interrater reliability (all specialties vs. consultant radiologist)
| Intraclass correlation coefficient | 95% confidence interval | ||
|---|---|---|---|
| Lower | Upper | ||
| Ortho cons 1st | .948 | .893 | .975 |
| Ortho cons 2nd | .963 | .924 | .982 |
| Ortho Snr fellow 1st | .974 | .946 | .987 |
| Ortho Snr fellow 2nd | .973 | .944 | .987 |
| Radiol spr 1st | .977 | .952 | .989 |
| Radiol spr 2nd | .947 | .891 | .974 |
| Radiographer 1st | .984 | .967 | .993 |
| Radiographer 2nd | .981 | .960 | .991 |
Validity
The validity was very good, as shown in Table 3. A mean value of 0 indicates perfect measurement accuracy compared to real age. The only value that shows a significant difference (mean 7.418, 95% CI: 0.303–14.533, P = 0.042) is the first occasion of the orthopaedic consultant, who is overestimating the real age on this occasion.
Table 3.
Paired samples test (validity vs. real age)
| Mean | 95% confidence interval of the difference | P-value | ||
|---|---|---|---|---|
| Lower | Upper | |||
| Ortho cons 1st | 7.418 | .303 | 14.533 | .042 |
| Ortho cons 2nd | −.249 | −5.041 | 4.543 | .916 |
| Ortho Snr fellow 1st | 1.218 | −4.042 | 6.478 | .639 |
| Ortho Snr fellow 2nd | 2.818 | −2.619 | 8.255 | .298 |
| Radiol cons 1st | 2.351 | −2.433 | 7.135 | .323 |
| Radiol cons 2nd | .818 | −4.079 | 5.715 | .735 |
| Radiol spr 1st | −.115 | −5.774 | 5.543 | .967 |
| Radiol spr 2nd | −2.115 | −7.626 | 3.395 | .439 |
| Radiographer 1st | −.082 | −5.240 | 5.076 | .974 |
| Radiographer 2nd | .485 | −5.084 | 6.053 | .860 |
Bland–Altman plots were constructed for all participants. The plots for the orthopaedic registrar are provided in Fig. 1. These plots further illustrate validity by demonstrating individual results for each participant. They show the difference from the real age versus increasing real age of the patient in the radiograph. The plots show that as the real age of the patient increases, the spread in the difference increases further away from zero. The plots for all participants were very similar. This finding suggests that the participants were more accurate at assessing the ages of younger patients.
Fig. 1.
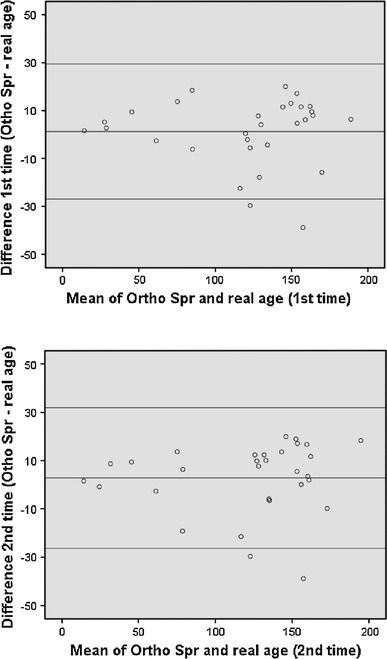
Bland–Altman plots for the orthopaedic SpR (difference vs. real age)
Discussion
Skeletal bone age assessment is crucial in planning for the equalisation of limb length discrepancies [1]. Despite the availability of several data analysis techniques for predicting remaining growth to assist in the timing of surgery, the skeletal bone age at a particular snapshot in time is still a necessary tool.
Generally all team members were able to age patients with a high degree of accuracy. The orthopaedic consultant tended to overestimate the real age during the first test. Possible reasons for this include a steep learning curve or inappropriate application of the technique.
Although the Greulich and Pyle atlas was derived during the 1930s from radiographs of white children from upper socioeconomic groups, this atlas is still in wide usage. Loder et al. [11] found that this atlas was not applicable to all children today, especially black girls, who were found to be skeletally advanced by 0.4–0.7 years. These findings were recently confirmed by Calfee et al. [12], who found that American adolescents are significantly more mature by skeletal age, as determined by the Greulich and Pyle method, than their chronological age would suggest. Cundy et al. [13] found that there was a variation of up to 2 years amongst a group of 4 radiologists when assessing for skeletal bone age, and that this variability was more pronounced in children with leg length discrepancy.
This study has some limitations. No power calculation was performed, and the number of radiographs (30) may be too small to demonstrate statistical significance. The participants were only tested immediately after the tutorial and again after a 2-week interval. Assessment could be performed at a longer interval to test whether the knowledge has been retained. It is likely that practice and experience will increase ability, although if the skills are not utilised regularly then ability may diminish.
Skeletal bone age prediction is a skilled technique. It is, however, extremely useful for orthopaedic clinicians to be able to age X-rays accurately prior to surgery. Time and money can be saved if a radiologist does not need to be involved. The aging technique does require a certain amount of training and experience, but this study shows that with adequate training, orthopaedic clinicians can learn the skills.
References
- 1.Kelly PM, Diméglio A. Lower-limb growth: how predictable are predictions? J Child Orthop. 2008;2(6):407–415. doi: 10.1007/s11832-008-0119-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Greulich W, Pyle S (1959) Radiographic atlas of the skeletal development of the hand and wrist, 2nd edn. Stanford University Press, Stanford
- 3.Tanner J, Whitehouse R, Marshall W, Cameron N, Healey MJR, Goldstein H (1975) Assessment of skeletal maturity and prediction of adult height. Academic, London
- 4.Westh R, Menelaus M. A simple calculation for the timing of epiphyseal arrest: a further report. J Bone Joint Surg Br. 1981;63:117–119. doi: 10.1302/0301-620X.63B1.7204464. [DOI] [PubMed] [Google Scholar]
- 5.Menelaus M. Correction of leg length discrepancy by epiphyseal arrest. J Bone Joint Surg Br. 1966;48:336–339. [PubMed] [Google Scholar]
- 6.Green WT, Anderson M. Skeletal age and the control of bone growth. Instr Course Lect. 1960;17:199–217. [PubMed] [Google Scholar]
- 7.Anderson M, Messner M, Green W. Distributions of lengths of the normal femur and tibia in children from 1 to 18 years of age. J Bone Joint Surg Am. 1964;46(6):1197–1202. [PubMed] [Google Scholar]
- 8.Paley D, Bhave A, Herzenberg JE, Bowen JR. Multiplier method for predicting limb-length discrepancy. J Bone Joint Surg Am. 2000;82:1432–1446. doi: 10.2106/00004623-200010000-00010. [DOI] [PubMed] [Google Scholar]
- 9.Anderson M, Green W, Messner M. Growth and predictions of growth in the lower extremities. J Bone Joint Surg Am. 1963;45:1–14. [PubMed] [Google Scholar]
- 10.Eastwood DM, Cole WG. A graphic method for timing the correction of leg-length discrepancy. J Bone Joint Surg Br. 1995;77(5):743–747. [PubMed] [Google Scholar]
- 11.Loder RT, Estle DT, Morrison K, et al. Applicability of the greulich and pyle skeletal age standards to black and white children of today. Am J Dis Child. 1993;147(12):1329–1333. doi: 10.1001/archpedi.1993.02160360071022. [DOI] [PubMed] [Google Scholar]
- 12.Calfee RP, Sutter M, Steffen JA, Goldfarb CA (2010) Skeletal and chronological ages in American adolescents: current findings in skeletal maturation. J Child Orthop 4(5):467–470 [DOI] [PMC free article] [PubMed]
- 13.Cundy P, Paterson D, Morris L, Foster B. Skeletal age estimation in leg length discrepancy. J Pediatr Orthop. 1988;5:513–515. doi: 10.1097/01241398-198809000-00002. [DOI] [PubMed] [Google Scholar]


