Abstract
Purpose
To evaluate and describe the kickstand modification and its use in children with lower extremity fractures.
Methods
Retrospective review identified eight children in whom the kickstand technique was used during treatment of their lower extremity fractures. The seven boys and one girl had a mean age of 11.8 years. All fractures were caused by high-energy trauma. Five of the eight tibial fractures were open fractures (one type 1, one type 2, and three type 3B), and five of the eight patients had multiple extremity fractures.
Results
Additional procedures were required in six of the eight children, four of whom had multiple lower extremity fractures. No additional pressure-relieving modalities were used in any patient. The kickstand did not affect the fracture reduction, prevent patient mobilization, or require operative adjustment in any patient, and none had any skin pressure-related complications on the heel of the affected extremity.
Conclusion
In pediatric patients with lower extremity trauma, the addition of a kickstand to the external fixator provides a simple, inexpensive, lightweight, adjustable, and adaptable method for encouraging elevation of the injured extremity, which facilitates edema control; it also allows easy neurovascular monitoring and wound care.
Keywords: Fracture, Lower extremity, Children, External fixation, Kickstand modification
Introduction
Elevation of the limb is an important part of the postoperative protocol after lower extremity trauma, but compliance may be a problem, especially in children. Keeping the limb elevated is often difficult in a cast or splint because it is uncomfortable to position the heel on a hard surface, and even a soft or padded surface becomes uncomfortable when the heel rests on a hard cast or splint. The modification of an external fixator to include a “kickstand” allows more comfortable extremity elevation, as well as ease of neurovascular monitoring and wound care. This is a straightforward, inexpensive modification that eliminates splint- and cast-related complications such as skin breakdown, compartment syndrome, and pressure ulcers, and encourages limb elevation. Although its use has been described in adult patients with a variety of fractures and reconstructive procedures [1–4], we found no reports of its use in pediatric patients.
Methods
Over a 24-month period, we used the kickstand technique in eight children to promote lower extremity elevation and prevent skin pressure complications (Table 1). The seven boys and one girl had a mean age of 11.8 years. All fractures were caused by high-energy trauma. Five of the eight tibial fractures were open fractures (one type 1, one type 2, and three type 3B), and five of the eight patients had multiple extremity fractures (Table 1). The indications for the use of external fixation were open fracture, fracture with or at high risk for compartment syndrome, and polytrauma.
Table 1.
Pediatric patients receiving the kickstand modification, including age, diagnosis, mechanism of injury, primary and additional procedures and soft-tissue complications
| Patient | Age | Diagnosis | Mechanism | Primary procedure* | Additional procedures | Soft-tissue complications |
|---|---|---|---|---|---|---|
| 1 | 12 | Closed tibia fracture | MVA | External fixation | 0 | None |
| 2 | 14 | Type 3A open tibia fracture | MVA | External fixation | 1 | None |
| 3 | 9 | Type 3B open ankle fracture | ATV | External fixation | 3 | None |
| Femur fracture | ||||||
| Contralateral closed tibia fx | ||||||
| 4 | 14 | Closed tibial shaft fracture | Ped struck** | External fixation | 1 | None |
| Shoulder dislocation | ||||||
| Humeral shaft fracture | ||||||
| Femur fracture | ||||||
| Pubic ramus fracture | ||||||
| Splenic Laceration | ||||||
| 5 | 12 | Type 3B open tibia fracture | ATV | External fixation | 10 | None |
| Multiple foot fractures | ||||||
| 5 | 12 | Type 3B open tibia fracture | ATV | Bone transport | 1 | None |
| Multiple foot fractures | ||||||
| 6 | 9 | Type 1 open tibia/fibula fx | Ped struck | External fixation | 0 | None |
| 7 | 15 | Closed tibia/fibula fracture | ATV | External fixation | 1 | None |
| Compartment syndrome | Fasciotomy leg | |||||
| 8 | 9 | Type II open tibia/fibula fx | MVA | External fixation | 3 | None |
| Medial malleolus fracture | ||||||
| Salter III distal femur fx |
* Primary procedure for kickstand, ** pedestrian struck by motor vehicle
The external fixator frames were assembled after pins were placed in the appropriate locations based on the fracture configuration and soft-tissue injuries. A delta frame was used in all patients to increase fracture stability. In one patient (patient 5), this was converted to a circular external fixator for bone transport at 4 months after injury.
The kickstand was applied at the conclusion of the surgical procedure and required 15 min or less to apply. To create the kickstand, two angled V-bars were attached to the external fixator using standard bar-to-bar clamps. The V-bars were then attached to L-bars with bar-to-bar clamps. We have found that the L-bars provide a stable base for the leg to rest on and also are compatible with soft air mattresses (Fig. 1). The estimated weight of the kickstand is 0.45 kg. Alternatively, a simpler and less expensive construct can be made by attaching a 10-cm carbon fiber to each side of the external fixator with bar-to-bar clamps.
Fig. 1.
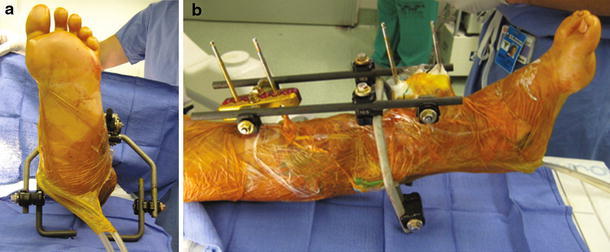
a, b The kickstand is created by attaching L-bars to the external fixator
Results
Additional procedures were required in six of the eight children, four of whom had multiple lower extremity fractures. The most severely injured child required 11 irrigation and débridements, six wound-vacuum device changes, and the application of a free flap for wound coverage. No additional pressure-relieving modalities were used in any patient. The kickstand did not affect the fracture reduction, prevent patient mobilization, or require operative adjustment in any patient, and none had any skin pressure-related complications on the heel of the affected extremity.
Illustrative case
A 14-year-old boy sustained multiple injuries in an all-terrain vehicle (ATV) accident, including a grade 3B tibial shaft fracture that was grossly contaminated with dirt, gravel, and grass (Fig. 2). He also had ipsilateral fractures of the calcaneus, navicular, and medial malleolus and a midtarsal dislocation (Fig. 3). Initial management included hemodynamic stabilization, broad-spectrum antibiotics, and surgical irrigation and débridement of his tibial wound. Because of the gross contamination of his wound, an external fixator was chosen for initial fixation of the tibial fracture and a wound-vacuum device was placed (Fig. 4). To facilitate wound care and elevation of his leg, a kickstand device was attached to the external fixator.
Fig. 2.

Grade 3B tibial shaft fracture in a 14-year-old boy
Fig. 3.

Ipsilateral fractures of the calcaneus, navicular, and medial malleolus, as well as a midtarsal dislocation
Fig. 4.
After application of external fixator
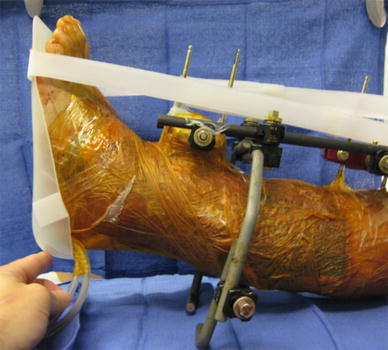
After initial stabilization, the patient had 11 additional irrigation and débridement procedures, six changes of the wound-vacuum device, and a latissimus free flap. A circular ring-type external fixator was applied for a bone transport procedure, and the kickstand device was modified for this fixator (Fig. 5). Despite severe associated soft-tissue and osseous injuries to his foot, he had no complications related to heel ulcers.
Fig. 5.

Modification of the kickstand for a circular external fixator
Discussion
External fixation may be indicated for certain lower extremity fractures in children: open fractures, fractures in patients with or at high risk for compartment syndrome, and fractures in patients with multiple trauma [5–9]. External fixation not only stabilizes the fracture, preventing further soft-tissue and neurovascular injury, but it also allows more rapid mobilization than casting or splinting and provides access for neurovascular monitoring, skin and wound care, and edema control. The addition of the kickstand to a standard external fixator encourages limb elevation, which can be a problem in pediatric patients. Placing the heel on a hard or soft surface is uncomfortable because of the contact of the heel with the surface, even with additional padding. The kickstand raises the heel to eliminate this contact, making elevation more comfortable and children more compliant with elevation instructions, which reduces the risk of skin complications such as pressure ulcers.
The kickstand technique also offers several other advantages. It allows the surgeon to easily control the amount of elevation by adjusting the length of the kickstand bars. We typically elevate the affected limb approximately 5 cm off the bed because excessive elevation can lead to knee hyperextension. The amount of elevation can be adjusted quickly without any specialized instruments in the acute hospital setting, the outpatient clinic, or physical therapy to facilitate range-of-motion exercises.
The use of the kickstand allows circumferential access to the soft tissues of the leg. This facilitates clinical neurovascular examination, wound care, and wound-vacuum device management while causing minimal discomfort to the patient. Moving an extremity or taking it out of a conventional splint can be painful, cause further neurovascular injury, and provoke anxiety in the patient, especially a child. The use of the kickstand also decreases the need for assistants when performing functions such as skin evaluation or dressing changes.
The kickstand is simple to assemble and is adaptable to almost any external fixation system and situation. It can be quickly constructed from the external fixation tray in the operating room and requires no additional equipment set or trays. In addition, components from different systems are usually compatible, which is important when patients are transferred after an external fixator has been placed at another institution. Kickstands add very little weight to the pre-existing frame, with a typical stand weighing approximately 17–20 oz (0.48–0.56 kg), and they can be removed during ambulation and physical therapy if necessary.
Depending on institutional regulations, the devices can be used multiple times as well. The cost of the kickstand varies from institution to institution. Castro-Aragon et al. [2] reviewed the costs of different systems and estimated them to range from $1,088 to $1,640, or approximately 20% of the cost of the frame itself. Similar findings were reported by Roukis et al. [4]. The cost of the additional components is relatively small in terms of the cost of treating a pressure sore once it occurs. Although it is not possible to determine an exact cost–benefit ratio of the kickstand, we believe that it is cost-effective considering its effectiveness in preventing skin complications. It has been estimated that the treatment of a pressure ulcer in the United States can cost between $10,000–$20,000, and they place a tremendous financial burden on our healthcare system. The Healthcare Cost and Utilization Project (HCUP) found that in 2003 the mean hospital charge for patients with pressure sores was $37,800 [10]. While this study consisted primarily of adult patients, many of whom had comorbid conditions, the cost to pediatric patients in terms of financial costs, treatment required, and time lost from school remains significant. Other devices, such as heel cushions and specialized mattresses, have been shown to be cost-effective at preventing pressure-related complications [11], but further studies are necessary to determine the exact cost-effectiveness of the kickstand modification in pediatric patients.
Conclusions
In pediatric patients with lower extremity trauma, the addition of a kickstand to the external fixator provides a simple, lightweight, adjustable, and adaptable method for encouraging elevation of the injured extremity, which facilitates edema control; it also allows easy neurovascular monitoring and wound care.
Conflict of interest
None.
References
- 1.Berkowitz MJ, Kim DH. Using an external fixation “kickstand” to prevent soft-tissue complications and facilitate wound management in traumatized extremities. Am J Orthop (Belle Mead NJ) 2008;37:162–164. [PubMed] [Google Scholar]
- 2.Castro-Aragon OE, Rapley JH, Trevino SG. The use of a kickstand modification for the prevention of heel decubitus ulcers in trauma patients with lower extremity external fixation. J Orthop Trauma. 2009;23:145–147. doi: 10.1097/BOT.0b013e318196bb6a. [DOI] [PubMed] [Google Scholar]
- 3.Clark J, Mills JL, Armstrong DB. A method of external fixation to offload and protect the foot following reconstruction in high-risk patients: the SALSAstand. Eplasty. 2009;9:321. [PMC free article] [PubMed] [Google Scholar]
- 4.Roukis TS, Landsman AS, Weinberg SA, Leone E. Use of a hybrid “kickstand” external fixator for pressure relief after soft-tissue reconstruction of heel defects. J Foot Ankle Surg. 2003;42:240–243. doi: 10.1016/S1067-2516(03)70036-2. [DOI] [PubMed] [Google Scholar]
- 5.Bartlett CS, 3rd, Weiner LS, Yang EC. Treatment of type II and type III open tibia fractures in children. J Orthop Trauma. 1997;11:357–362. doi: 10.1097/00005131-199707000-00010. [DOI] [PubMed] [Google Scholar]
- 6.Egol KA, Tejwani NC, Capla EL, Wolinsky PL, Koval KJ. Staged management of high-energy proximal tibia fractures (OTA types 41): The results of a prospective, standardized protocol. J Orthop Trauma. 2005;19:448–455. doi: 10.1097/01.bot.0000171881.11205.80. [DOI] [PubMed] [Google Scholar]
- 7.Grimard G, Naudie D, Laberge LC, Hamdy RC. Open fractures of the tibia in children. Clin Orthop Rel Res. 1996;332:62–70. doi: 10.1097/00003086-199611000-00009. [DOI] [PubMed] [Google Scholar]
- 8.Joveniaux P, Ohl X, Harisboure A, Berrichi A, Labatut L, Simon P, Mainard D, Vix N, Dehoux E. Distal tibia fractures: management and complications of 101 cases. Int Orthop. 2010;34:583–588. doi: 10.1007/s00264-009-0832-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Song KM, Sangoerzan B, Benirschke S, Browne R. Open fractures of the tibia in children. J Pediatr Orthop. 1996;16:635–639. doi: 10.1097/01241398-199609000-00016. [DOI] [PubMed] [Google Scholar]
- 10.Agency for Healthcare Research and Quality (2006) Number of hospital patients with pressure sores increasing (AHRQ News and Numbers, Apr 18 2006). Agency for Healthcare Research and Quality, Rockville. http://www.ahrq.gov/news/nn/nn041806.htm. Accessed 21 May 2010
- 11.Gilcreast DM, Warren JB, Yoder LH, Clark JJ, Wilson JA, Mays MZ. Research comparing three heel ulcer-prevention devices. J Wound Ostomy Continence Nurs. 2005;32:112–120. doi: 10.1097/00152192-200503000-00008. [DOI] [PubMed] [Google Scholar]


