Abstract
Purpose
To describe surgical outcomes using the new device in pediatric neuromuscular scoliosis.
Methods
All patients with neuromuscular disorders requiring surgery with pelvic fixation for the correction of scoliosis in the period 2002–2009 were operated by the new pelvic rod fixation device. Coronal and sagittal alignment before and after surgery until the latest follow-up were evaluated by standard X-rays. Intraoperative and postoperative complications were recorded.
Results
All 18 study patients (mean age at surgery 15 years, range 10–27) achieved solid fusion at a mean follow-up of 41 months. The coronal Cobb angle improved from 82° ± 31° (range 36–168) to 33° ± 25° at the last follow-up (range 9–95 months) (P < 0.0001). Pelvic obliquity improved from 19° ± 6° (range 10–30) to 5° ± 5° (range 0–14) (P < 0.0001). Early complications included pneumonia, urinary tract infection, disseminated intravascular coagulation (DIC), and hypovolemic shock. Three patients required debriding and received prolonged antimicrobial therapy for deep wound infection (none required implant removal). At the latest follow-up, no patient complained of lumbar pain or worsening of ambulatory status or level of activity.
Conclusion
Surgery employing the new pelvic rod fixation device allowed solid fusion and fixation with significant correction of multiplanar deformity, but the complication rate was high.
Keywords: Scoliosis, Neuromuscular, Pelvic obliquity
Introduction
Scoliosis is a very common feature in patients suffering from various neuromuscular conditions [1]. A unique C-shaped curve of the spine, rapid progression of the condition, and pelvic obliquity are also often present [2]. Since conservative treatment is rarely effective, many of these patients require surgery, including pelvic fixation and correction of pelvic obliquity [1, 2], in order to obtain a more balanced and comfortable sitting position, to resolve pain, to improve functional status, to allow for independent ambulation in a wheelchair, and to assist with nursing care [3]. There are many good surgical options for achieving these goals, but they mostly involve the correction of spinal and pelvic deformity using the same rod. Patients who undergo these procedures are reported to have a high rate of complications, including respiratory dysfunction, wound infection, pseudarthrosis, and failure of fixation [1, 2, 4–7].
Long spinal fusion to the sacrum remains one of the most demanding challenges in terms of instrumentation, and complications, such as material failure, loss of sacral fixation, loss of lumbar lordosis, and pseudarthrosis, are not unusual [4–6]. These problems most typically originate in the large lumbosacral loads, the substantial leverage applied to the sacral screws, the posterior position of spinal implants in the sagittal plane, and the frequently poor bone quality of the sacrum [4, 8]. In addition, reduction of three-dimensional pelvic obliquity requires immediate stability in all three planes [4]. We used a new pelvic rod fixation device and conducted a clinical study to evaluate the surgical outcomes using the addition of this device to an already existing system in cases of pediatric neuromuscular scoliosis.
Materials and methods
Patients
All consecutive patients suffering from neuromuscular conditions who underwent long spinal fusion with pelvic fixation in our institution between November 2002 and April 2009 were operated by the same surgeon (DO) using the Pivot Link Universal System (PLUS) (Figs. 1, 2, 3, and 4). Their medical records and radiographs were retrospectively reviewed after institutional review board approval had been obtained to conduct this study. Patients who had undergone spinal surgery in the past were excluded. Clinical evaluation and complete radiologic analyses were performed preoperatively, postoperatively, and every 6–12 months during the follow-up period.
Fig. 1.

Partially threaded iliac screws of the pelvic rod system
Fig. 2.

Pelvic rods (right and left sides)
Fig. 3.

Domino connectors for the pelvic rod system
Fig. 4.

The pelvic rod system implanted on a saw bone model
Operative procedures
A tibial cortical bone graft was harvested as described by Zeller et al. [9], after which pedicular screws or hooks were placed along the spine through a posterior approach according to the preoperative plan. Pedicular screws in S1 and/or L5 were placed either bilaterally at the same level or one screw at each level on contralateral sides, with no attachment to the main spinal rod. The posterior superior iliac spine was exposed by dividing the paraspinal muscles, and bony prominences were excised followed by countersinking and insertion of a screw into the ileum deep beneath the outer surface of the iliac wing. Either regular 7.5-mm full-threaded screws or special iliac screws (threaded only at the mid-portion of the screw, Fig. 1) were used. The iliac screw was inserted with one finger placed on the outer surface of the ileum in order to guide the screw to the preferred direction and to avoid penetration of the thin iliac cortical wall. A PediGuard (SpineGuard™, SpineGuard, Inc., San Francisco, CA) was also used for this purpose in procedures performed after 2007. Two long spinal rods were then inserted, and correction of the spinal curve was carried out by prebending the rod to allow correction by translation, followed by in situ bending techniques. The rod had to have 3–4 cm of resilience distally to allow an easy connection with the smaller special pelvic rods (Fig. 2). Two single semi-open dominos were then placed, usually with their closed ring on the pelvic rod, and the rods were inserted into the pelvic screws (ileum + S1 and/or L5), first on the concave and then on the convex side of the tilted pelvis. Since these rods are prebent, most of the sagittal correction occured during insertion of the rod to its designated place and connection to the dominos. Finally, half of the dominos’ knobs (Fig. 3) were tightened, and the rods were distracted on their concave side, thereby, correcting the coronal pelvic tilt by the sliding of the pelvic rods along the main spinal rods. For very rigid curves, this process was repeated to allow a safer and more gradual correction.
Medical data
Demographic, operative, and postoperative data were collected from medical records. The ambulatory state was classified according to the Gross Motor Function Classification System (GMFCS) [10].
Radiographic measurements
Measurements were made on 36-inch-long cassette anteroposterior and lateral radiographs of the spine with the patient standing or sitting. All films were digitized and then analyzed by the same investigator. Radiographic analysis included measurements of the Cobb angle of the major curve, pelvic obliquity (the angle between a horizontal line and a line drawn between the iliac crests), and lumbar lordosis. Patients were categorized as being hyperlordotic (>50°) or hypolordotic (<20°). Bony changes, such as radiolucent lines or sclerosis around the sacral rods or screws, were identified and recorded.
Statistical analysis
Paired-sample t-tests were used to analyze differences between preoperative and postoperative measures. All statistical tests were two-tailed, and a P-value <0.05 was considered to be significant. All statistical analyses were conducted using Excel software (Windows 2007).
Results
Demographic and clinical data
Eighteen consecutive pediatric patients (10 females and 8 males) underwent long spinal fusion to the sacrum at a mean age of 15 ± 3.7 years (range 10.6–27). All patients were available for follow-up. The mean follow-up period was 40.8 ± 25 months (range 8–86). The etiology of scoliosis was cerebral palsy in eight, myopathy in four, spinal muscular atrophy in three, muscular dystrophy in two, and Rett’s syndrome in one. Four patients were ambulatory before surgery, while 14 were dependent upon wheelchairs.
Blood loss, operation time, and length of hospitalization
Surgery in all patients consisted of long spinal fusion from T2 to the sacrum with the use of tibial cortical autografts. The mean duration of surgery was 556 ± 140 min (range 341–755). There was a decrease in the mean total hemoglobin level of 5.6 ± 1.1 g/dL (range 4.3–7.5) and 5.5 ± 3.2 units of packed red blood cells (range 0–11) were required. The patients spent 4.8 ± 4.7 days in the intensive care unit (range 1–18) and had a total hospitalization time of 12 ± 4.6 days (range 7–24).
Radiologic results
The main curve Cobb angle was a mean of 82.3° ± 31° (range 36–168) preoperatively and 30.9° ± 22.2° (range 9–95) immediately after surgery (P < 0.00001). At the latest follow-up, the Cobb angle measured 33.4° ± 25.3° (range 9–95), representing a correction of 62.4 ± 18.2%. The mean loss of correction between immediately postoperative and the latest follow-up was 2.5°. There was no significant difference between the postoperative and the latest radiograph measures in any of the parameters. Pelvic obliquity was reduced from a mean of 19.3° ± 5.8° (range 10–30) preoperatively to 5° ± 4.7° (range 0–14) postoperatively (75% correction, P < 0.0001). There was no progression of pelvic obliquity, and obliquity of <15° was achieved and maintained in all patients.
Selected radiographic and clinical results are demonstrated in Figs. 5, 6, 7, and 8. Five patients were categorized preoperatively as being hyperlordotic (mean lumbar lordosis angle of 61° ± 11°, range 50–76) and they achieved a mean sagittal correction of 20° ± 12° (range 11–41). Four of these five patients achieved a normal (<50°) lordotic curve. Two other patients were hypolordotic preoperatively (0°–17°) and their spines were corrected to a normal curve (28°–30°).
Fig. 5.

Preoperative anteroposterior X-ray spine of a 16-year-old patient with cerebral palsy. The main curve Cobb angle is 95° and the pelvic obliquity is 20°
Fig. 6.

An anteroposterior X-ray spine taken 50 months following surgical correction. The residual main curve Cobb angle is 32° and the pelvic obliquity is 2°
Fig. 7.

a Preoperative and b postoperative posterior view standing photos of a 14-year old patient with spinal muscular atrophy 3. Note correction of the scoliotic curve and pelvic obliquity
Fig. 8.
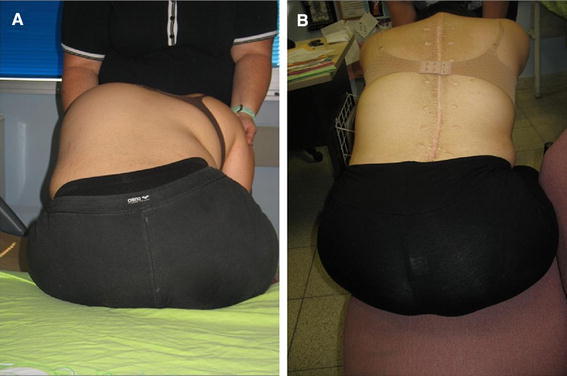
a Preoperative and b postoperative posterior view forward bending photos of a 14-year-old patient with spinal muscular atrophy 3. Note correction of the scoliotic curve and rib hump
Functional status
Four patients (22.2%) who were partially ambulatory (GMFCS level 3) and walked with crutches or a frame before the operation maintained and slightly improved their walking distance. Ten patients were GMFCS level 4, and the remaining four were GMFCS level 5. One patient with myopathy who was a nonwalker before the operation managed to walk 50 m with assistance following the operation. The four GMFCS level 5 nonambulatory patients had needed a sitting orthosis to sit upright preoperatively; they were able to sit upright with the hips flexed at 90° without bracing after the operation.
Complications
Three patients (16.7%) had early deep wound infection (Pseudomonas aeruginosa, Acinetobacter baumannii, and Staphylococcus aureus) and were successfully treated with immediate surgical debridement and long-term intravenous antimicrobial therapy. None required removal of the fixation device. Other postoperative complications included pneumonia, urinary tract infection, seroma, disseminated intravascular coagulation, and one patient with hypovolemic shock that required massive blood transfusion. All of these complications were successfully treated with no sequelae. One patient with spastic cerebral palsy had dislodgement of a D2 laminar claw due to progressive kyphosis above the level of fusion. A radiolucent area was noted around the iliac screws within 2–3 months following the operation in four patients, and long-term solid fusion was achieved in them all, both clinically and radiographically, with no progression of the radiolucent lines.
Discussion
Sacral fixation remains a surgical challenge, especially in the pediatric neuromuscular scoliosis population. The surgical device and technique must provide a comfortable and reliable platform for the correction of spinal and pelvic deformities in all three planes and a strong and stable structure for fixation. Bulky prominences that may cause skin problems must be avoided. There are many techniques currently available for this purpose [4]. The severity of the spinal and pelvic deformities, the presence and severity of osteopenia, poor skin coverage, and general medical fragility in neuromuscular scoliosis patients also contribute to the complexity of the issue [4, 11]. Biomechanically, a sitting posture produces a considerable flexion moment on the sacropelvic instrumentation as a result of the long lever arm of the fused spine, thereby, accelerating secondary failure [4]. Scoliotic curve and pelvic obliquity are to be corrected in all three planes and tailored individually to each patient to allow for a comfortable sitting posture and to prevent pressure points and decubitus ulcers as in a kyphotic or a hyperlordotic spine. The anatomy of the iliac bone can also be a cause of concern, since the ilium may be too thin to contain the rods in children with neuromuscular scoliosis [4].
Historically, pelvic fixation techniques have evolved, beginning with the Galveston technique, and followed by the Dunn–McCarthy technique, sacral screws plates and rods, iliosacral screws, and iliac screws [2].
The Galveston technique
This was described in 1984 [12] and reportedly achieved 53–81% correction of pelvic obliquity [2]. However, in comparison to fixation with iliac screws, the Galveston technique was found to provide less stable fixation, as demonstrated by the worsening of pelvic tilt during the follow-up period and loss of correction, as well as significantly more iliac anchor motion (“windshield wiper” effect) [2, 4, 13]. The Galveston technique is also associated with a high rate (up to 32%) of rod- and screw-related complications, probably due to the long lever arm and to the high loads placed on the lumbosacral area and fixation device. Also, the use of the Galveston rod requires complex three-dimensional bending [2].
The unit rod
This is a low-cost popular modification of the Galveston technique, described as being easy to use. However, its use may be complicated by perforation of the iliac bone cortex during insertion, skin ulcers caused by prominent rods, screws, or wires, and loss of correction over time [14, 15].
The Dunn–McCarthy technique
This uses an S-shaped sacral rod and has been reported to achieve good long-term results in patients with spine deformities [16]. However, mechanical complications, such as rod migration into the sacrum or rod dislodgement, were reported in 4.5% of the patients [4] and damage to the L5 nerve root was reported in up to 14% of the patients [16].
Sacral screws
These devices were reported to be an unreliable means of long spinal fixation. Both biomechanical and clinical evaluations showed that its use resulted in immediate (intraoperative) or secondary failure following pull-out of the screws. Correct screw positioning can also be difficult, especially in severe pelvic obliquity, and the use of these screws carries a potential risk of neurovascular damage. It should probably not be used for long spinal fusions [4, 6, 17].
Iliosacral screw fixation
First described by Dubousset in 1997 [6], this has been reported to be a good technique for pelvic obliquity reduction and fusion [4, 6, 18]. It offers good stability in the frontal plane, but is less effective in the correction of sagittal plane deformities [4] and was associated with iliosacral screw mobilization and disengagement that necessitated repeated surgical intervention [6, 18].
Intrasacral rod fixation
This was first described by Jackson in 1990 [6], who inserted two rods beyond the sacral screws into the lateral sacral mass distal to S3. This method has multiple points of three-dimensional stability and allows for mobilization or manipulation of the sacrum in different planes, facilitating three-dimensional reduction of pelvic obliquity. The use of the intrasacral rod was recently reported to achieve good correction of pelvic deformity in the coronal and sagittal planes, with no complications related to the rods in the pelvic area, although 7.1% of the patients suffered radicular pain at the L4, L5, and S1 levels [4]. Correction was maintained until the last follow-up, and the authors concluded that this was a stable and effective technique for pelvic fixation, relating the neurologic complications to the extensive correction that had been required during the operation [4].
Iliac screws
Phillips et al. [11] described the results of 50 patients with neuromuscular scoliosis treated with iliac screw fixation and followed up for 5 years. Those authors reported a 59% pelvic deformity correction, with 44% of their patients having suffered complications related to the loosening and breakage of rods, wires, and screws. These were more often seen in patients treated with one screw compared to those treated with two screws in each ilium [11]. Modi et al. [1] described pelvic fixation with the use of a single iliac screw connected to the main rod in the correction of scoliosis in 52 patients with cerebral palsy. Attempts to correct the pelvic obliquity of one of their ten patients who had pelvis obliquity of more than 15° failed, and the successful correction in three others deteriorated and was lost with time. They achieved a 65% correction of pelvic obliquity postoperatively for the entire cohort, but this figure dropped to only 49% at the last follow-up [1]. Hahn et al. [19] treated 20 patients with Duchenne muscular dystrophy using pedicular screws through L5 and pelvic fixation with iliac screws alone. They reported a 55% correction of pelvic tilt and significant improvement in lumbar lordosis, and that there were no complications related to the fixation devices [19]. Pedicular screws have the advantage of stabilizing all three columns of the spine and of creating a more stable construct compared with other techniques, in addition to enabling a posterior-only approach [1].
It has been described that, in cases of severe rigid pelvic obliquity and scoliotic curve, vertebral decancellation or multilevel vertebral osteotomies can be used to achieve better correction. These techniques can eliminate the need for a combined anterior and posterior approach and potentially decrease complications [20].
The new technique described is unique for a number of reasons. We believe that the use of tibial cortical bone graft contributes to the high rate of fusion that was achieved in our hands. Iliac screws and pedicular sacral screws provided a strong pelvic anchor that allowed good correction of pelvic deformity in the coronal and sagittal planes without loss of correction throughout follow-up and with only a very limited amount of movement (as demonstrated by the “windshield wiper” effect). Biomechanical works support the advantage of iliac and sacral fixation using screws over the Galveston rod-based technique in resisting flexion and extension forces [8]. The main curve coronal correction of 63% in our cohort is well within the previously reported range of 42–70% in similar works [5, 6]. Pelvic obliquity was corrected by 75% in our study group, compared with the previously reported range of 45–84% in similar patient populations using different techniques [5, 6]. The prebent configuration of the sacral rods allows for most of the correction, mainly in the sagittal plane, to take place before performing manipulations, and, thus, prevents loosening of the screws. We believe that the distraction–contraction method also contributed to this rate of successful correction while avoiding the intraoperative loosening of the pelvic screws caused by the excessive manipulations of other methods: we were able to correct coronal deformity separately from the main spinal or sagittal pelvic deformities. Furthermore, with this technique, the main and pelvic rods connect in the coronal plane, and are, therefore, not prominent and do not cause skin ulcers or delayed surgical wound closure (Fig. 4). Zahi et al. [18] also reported the use of short pelvic rods that connect to a main spinal rod and anchor the pelvis with iliosacral screws. They concluded that the use of a short rod and connectors simplifies the procedure and allows good coronal correction by using a distraction–contraction technique. The use of separate pelvic and spinal rods had been described with simultaneous correction of the pelvic and of the spinal deformities [21], mostly using translation forces. We believe that, when correction of the coronal pelvic tilt is performed last, better distribution of forces is allowed, which, of course, is especially important for neuromuscular patients, who often suffer from low bone quality and osteopenia.
The mean operative time reported in this study is somewhat prolonged compared to other reports (556 min compared to 330–420 min in the literature), probably due to the fact that it includes the time required for tibial graft harvesting [5]. In addition, our calculations included two patients who underwent a combined anterior release immediately followed by a posterior fusion operation. General postoperative complications in patients with neuromuscular scoliosis vary between 8 and 62%, and the mean estimated blood loss is 3,091 ml (range 500–8,000) following long spinal fusion [1, 5]. Infection rates are particularly high in neuromuscular patients and have a deleterious effect on outcome [7]. Our figures fall within these ranges.
Limitations of the methodology
This is a noncontrolled retrospective study. The small size of our patient population lacks power and does not allow for categorization according to etiology.
Conclusion
The use of a novel short pelvic rod and domino construction for the correction and fixation of pelvic tilt allows good correction of pelvic obliquity without compromising the ability of correcting the main scoliotic deformities in the coronal and sagittal planes. Solid fusion can generally be expected and lead to improved sitting position and weaning from orthotics in some patients. The rate of associated complications is of concern.
Acknowledgments
Esther Eshkol is thanked for her editorial assistance.
References
- 1.Modi HN, Hong JY, Mehta SS, et al. Surgical correction and fusion using posterior-only pedicle screw construct for neuropathic scoliosis in patients with cerebral palsy: a three-year follow-up study. Spine. 2009;34:1167–1175. doi: 10.1097/BRS.0b013e31819c38b7. [DOI] [PubMed] [Google Scholar]
- 2.Peelle MW, Lenke LG, Bridwell KH, et al. Comparison of pelvic fixation techniques in neuromuscular spinal deformity correction: Galveston rod versus iliac and lumbosacral screws. Spine. 2006;31:2392–2398. doi: 10.1097/01.brs.0000238973.13294.16. [DOI] [PubMed] [Google Scholar]
- 3.Cassidy C, Craig CL, Perry A, et al. A reassessment of spinal stabilization in severe cerebral palsy. J Pediatr Orthop. 1994;14:731–739. doi: 10.1097/01241398-199414060-00008. [DOI] [PubMed] [Google Scholar]
- 4.Ilharreborde B, Hoffmann E, Tavakoli S, et al. Intrasacral rod fixation for pediatric long spinal fusion: results of a prospective study with a minimum 5-year follow-up. J Pediatr Orthop. 2009;29:594–601. doi: 10.1097/BPO.0b013e3181b2b403. [DOI] [PubMed] [Google Scholar]
- 5.Teli MG, Cinnella P, Vincitorio F, et al. Spinal fusion with Cotrel–Dubousset instrumentation for neuropathic scoliosis in patients with cerebral palsy. Spine. 2006;31:E441–E447. doi: 10.1097/01.brs.0000221986.07992.fb. [DOI] [PubMed] [Google Scholar]
- 6.Miladi LT, Ghanem IB, Draoui MM, et al. Iliosacral screw fixation for pelvic obliquity in neuromuscular scoliosis. A long-term follow-up study. Spine. 1997;22:1722–1729. doi: 10.1097/00007632-199708010-00007. [DOI] [PubMed] [Google Scholar]
- 7.Sponseller PD, Shah SA, Abel MF, et al. Infection rate after spine surgery in cerebral palsy is high and impairs results: multicenter analysis of risk factors and treatment. Clin Orthop Relat Res. 2010;468(3):711–716. doi: 10.1007/s11999-009-0933-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Early S, Mahar A, Oka R, et al. Biomechanical comparison of lumbosacral fixation using Luque–Galveston and Colorado II sacropelvic fixation: advantage of using locked proximal fixation. Spine. 2005;30:1396–1401. doi: 10.1097/01.brs.0000166530.87923.5b. [DOI] [PubMed] [Google Scholar]
- 9.Zeller RD, Ghanem I, Miladi L, et al. Posterior spinal fusion in neuromuscular scoliosis using a tibial strut graft. Results of a long-term follow-up. Spine. 1994;19:1628–1631. doi: 10.1097/00007632-199407001-00012. [DOI] [PubMed] [Google Scholar]
- 10.Palisano R, Rosenbaum P, Walter S, et al. Development and reliability of a system to classify gross motor function in children with cerebral palsy. Dev Med Child Neurol. 1997;39(4):214–223. doi: 10.1111/j.1469-8749.1997.tb07414.x. [DOI] [PubMed] [Google Scholar]
- 11.Phillips JH, Gutheil JP, Knapp DR., Jr Iliac screw fixation in neuromuscular scoliosis. Spine. 2007;32:1566–1570. doi: 10.1097/BRS.0b013e318067dcff. [DOI] [PubMed] [Google Scholar]
- 12.Allen BL, Jr, Ferguson RL. The Galveston technique of pelvic fixation with L-rod instrumentation of the spine. Spine (Phila Pa 1976) 1984;9(4):388–394. doi: 10.1097/00007632-198405000-00011. [DOI] [PubMed] [Google Scholar]
- 13.Gau YL, Lonstein JE, Winter RB, et al. Luque–Galveston procedure for correction and stabilization of neuromuscular scoliosis and pelvic obliquity: a review of 68 patients. J Spinal Disord. 1991;4:399–410. doi: 10.1097/00002517-199112000-00001. [DOI] [PubMed] [Google Scholar]
- 14.Tsirikos AI, Lipton G, Chang WN, et al. Surgical correction of scoliosis in pediatric patients with cerebral palsy using the unit rod instrumentation. Spine. 2008;33:1133–1140. doi: 10.1097/BRS.0b013e31816f63cf. [DOI] [PubMed] [Google Scholar]
- 15.McCall RE, Hayes B. Long-term outcome in neuromuscular scoliosis fused only to lumbar 5. Spine. 2005;30:2056–2060. doi: 10.1097/01.brs.0000178817.34368.16. [DOI] [PubMed] [Google Scholar]
- 16.Walick KS, King JT, Johnston CE, et al. Neuropathic lower extremity pain following Dunn–McCarthy instrumentation. Spine. 2008;33:E877–E880. doi: 10.1097/BRS.0b013e3181877b99. [DOI] [PubMed] [Google Scholar]
- 17.Camp JF, Caudle R, Ashmun RD, et al. Immediate complications of Cotrel–Dubousset instrumentation to the sacro-pelvis. A clinical and biomechanical study. Spine. 1990;15:932–941. doi: 10.1097/00007632-199009000-00018. [DOI] [PubMed] [Google Scholar]
- 18.Zahi R, Vialle R, Abelin K, et al. Spinopelvic fixation with iliosacral screws in neuromuscular spinal deformities: results in a prospective cohort of 62 patients. Childs Nerv Syst. 2010;26(1):81–86. doi: 10.1007/s00381-009-0966-8. [DOI] [PubMed] [Google Scholar]
- 19.Hahn F, Hauser D, Espinosa N, et al. Scoliosis correction with pedicle screws in Duchenne muscular dystrophy. Eur Spine J. 2008;17:255–261. doi: 10.1007/s00586-007-0558-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Suh SW, Modi HN, Yang J, et al. Posterior multilevel vertebral osteotomy for correction of severe and rigid neuromuscular scoliosis: a preliminary study. Spine. 2009;34(12):1315–1320. doi: 10.1097/BRS.0b013e3181a028bc. [DOI] [PubMed] [Google Scholar]
- 21.Bridwell KH, DeWald RL, editors. The textbook of spinal surgery. 2. Philadelphia, PA: Lippincott-Raven; 1997. pp. 600–603. [Google Scholar]


