Abstract
PURPOSE
The purpose of this study was to compare the accuracy of the implant master cast according to the type (pick-up, transfer) and the length (long, short) of the impression copings.
MATERIALS AND METHODS
The metal master cast was fabricated with three internal connection type implant analogs (Osstem GS III analog), embedded parallel and with 10° of mesial angulation to the center analog. Four types of impression coping were prepared with different combinations of types (transfer, pick-up) and lengths (long, short) of the coping. The impressions were made using vinyl polysiloxane (one step, heavy + light body) with an individual tray, and 10 impressions were made for each group. Eventually, 40 experimental casts were produced. Then, the difference in the distance between the master cast and the experimental cast were measured, and the error rate was determined. The analysis of variance was performed using the SPSS (v 12.0) program (α = .05), and the statistical significance was set at P < .05.
RESULTS
The ANOVA showed that the pick-up type impression coping exhibited a significantly lower error rate than the transfer type. However, no significant difference was observed with respect to the length of the impression coping. Additionally, no significant difference was observed between the parallel and mesial angulated groups.
CONCLUSION
Within the limitations of this study, the pick-up type impression coping exhibited a more accurate implant master cast than the transfer type in parallel group. The accuracy of the implant master cast did not differ for different lengths of impression coping of at least 11 mm. Additionally, the accuracy of the implant cast was not different for the parallel and 10° mesial angulated groups.
Keywords: Impression coping, Implant angulation, Master cast accuracy
INTRODUCTION
Dental implant therapy has been widely used for the restoration of partially and fully edentulous patients.1 It is essential for long-term successful implant prostheses to achieve a passive fit between the fixture and the superstructure.2 A passive fit is defined as a very precise surface contact for the metal and it distributes functional load uniformly.3
Obtaining an absolute passive fit is practically impossible,4 and the behavior of the bone tissue around the implants supporting relatively ill-fitting prostheses remains controversial.5-8 Nonetheless, it is still universally accepted that the prosthesis misfit should be minimized,9 and accurate impressions are the first step in minimizing the misfit.
To date, many authors have investigate the factors affecting the accuracy of the implant impressions, such as the type of impression copings, the necessity and method of splinting the impression copings, surface treatment of the impression copings, direct or indirect impression techniques, the use of different impression materials, and angulated implants.10
Previous studies have concentrated on external connected implants that are positioned parallel, but generally, the implant fixture is not positioned parallel in clinical applications. Additionally, internal-connection implants have longer walls of relative parallelism that could make the withdrawal of an impression more difficult, resulting in the transfer of a higher level of stress to the impression copings during the impression procedure.11
Clinically, short impression copings are needed in situations where there is an insufficient interocclusal space, such as the posterior teeth area or patient with limited mouth opening. This impression coping has become commercially available for various implant companies. However, a smaller portion of the coping is exposed, lowering the stability of the impression coping in the impression material and, therefore, affecting the accuracy of the impression.12
There are a few studies which have investigated the influence of the length of the impression coping on the accuracy of the angulated implants.
Therefore, the purpose of this study was to investigate the effect of the type and length of the impression coping on the accuracy of the angulated internal-connected implant impression.
MATERIALS AND METHODS
Implant analogs (GS III® Fixture Lab Analog Standard, Osstem, Korea) and vinyl polysiloxane impression materials (Imprint III®, 3M ESPE, Germany) were used in this study.
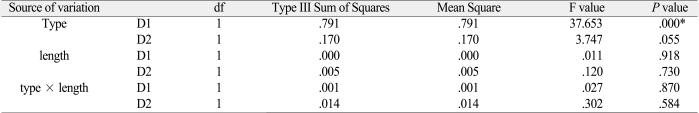
The experimental model was fabricated using Type IV gypsum (Fujirock® GC, Belgium). A torque wrench (TWMW, Osstem, Korea) was used to connect the analog and the impression copings. A measuring microscope (MF-A1010, Mitutoyo, Japan) was used to examine the distance of analogs (Fig. 1).
Fig. 1.
Measuring microscope (MF-A1010, Mitutoyo, Japan).
1. Fabrication of metal master cast
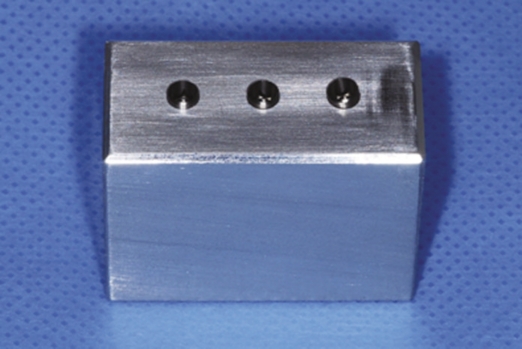
The metal master model (length: 4 cm, width: 2 cm, height: 3 cm) was fabricated using a milling aluminum block. Three holes with a depth of 9 mm were made at 10 mm intervals in order to embed the analogs. The center and lateral holes were parallel and the other one was at a 10° mesial angulation. The surface was well polished and did not affect the removal of the impression material. The analogs were positioned into the holes using a milling machine with Superbond C&B (Sun Medical, Japan). The top of the analog was positioned 1 mm above the model (Fig. 2).
Fig. 2.
Master metal model.
2. Fabrication of individual tray
After connecting the impression coping to the master model, two sheets of baseplate wax were applied to provide space for the impression material. Then the alginate (Jeltrate regular set, Hamm Moor Lane, England) impression was taken in order to reproduce the master model with putty type PVS (Exafine®, GC corperation, Japan). With this mold, the custom impression tray was fabricated using a light-polymerizing impression tray material (Lightplast, DreveDentamid, Germany) and cured in a light-curing machine (Unilux AC, Kulzer Hereaus, Netherlands) for 5 minutes. Retention holes were made on the side of the tray in order to retain the impression material, and occlusal holes were made for the guide pin of the pick-up type impression coping. Tray adhesive (VPS Tray Adhesive, 3M ESPE, Germany) was applied and dried for 15 minutes.
3. Fabrication of experimental model
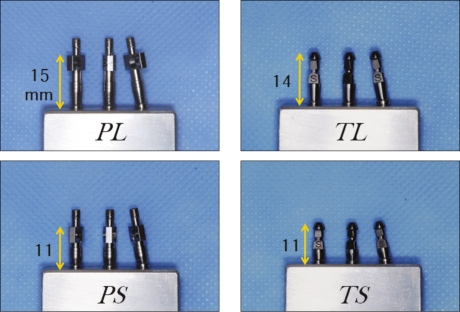
The impression copings were classified by their type and length (Fig. 3). P and T were used to represent the pick-up and transfer types of impression coping. Additionally, L and S were used to symbolize long and short coping lengths. A total of four groups (PL, PS, TL, and TS groups) were made, and in each group, 10 impressions were made so that 40 experimental models existed.
Fig. 3.
A set of impression copings.
The impression coping was connected to the metal master cast. The light body material (Imprint III®, 3M ESPE, Germany) was injected around the impression coping, and at the same time, the heavy body material (Imprint III®, Penta™, 3M ESPE, Germany) was filled in the individual tray. The tray was positioned on the model for 8 minutes (twice the time of polymerization in mouth). Then the overflow impression material was wiped away using a finger.
(1) Pick-up type (PL group, PS group)
After the polymerization, the tray was removed by loosening the guide pin with a hex driver. Then the fixture analog was connected to the impression coping that was left in the impression material.
(2) Transfer type (TL group, TS group)
The tray was removed after the polymerization of the impression material. The impression coping that was removed from master cast was connected to the analog by hand and then repositioned into the inner position of the impression material.
The Type IV dental stone was poured according to the manufacturer's instructions (water/power : 20 ml/100 g). After the stone setting, the tray was separated from the model. After at least 24 hours had elapsed, the accuracy was measured.
4. Measurement of distance
The distance between the analogs of the master model and the experimental model was measured using a measuring microscope (MF-A1010, Mitutoyo, Japan) and the Hanra measure program (Hanra precision ENG, Korea). This microscope had a magnification of 100× and an accuracy of ± 0.5 µm. D1 was defined as distance from the top center of the central analog to the top center of parallel positioned analog in the master model, and D2 was the distance to the center of mesial angulated analog in the master model (Fig. 4). And, d1 was defined as distance from the central analog to parallel positioned analog in the experimental model, and d2 was the distance to the mesial angulated analog in the experimental model.
Fig. 4.
Measuring distance.
The error rate (ER) between D (n) and d (n) was used as the experimental value. D (n) means distance in the master model, and d (n) means distance in the experimental model.

5. Statistics analysis
The SPSS program (SPSS® statistics, IBM, USA) was used to determine the mean and standard deviation of the error rate. The ANOVA test was used to determine the significance of the type, the length, and the angulation of the impression copings, and a value of P < .05 was used to judge the statistical significance.
RESULTS
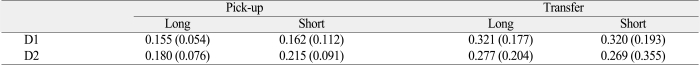
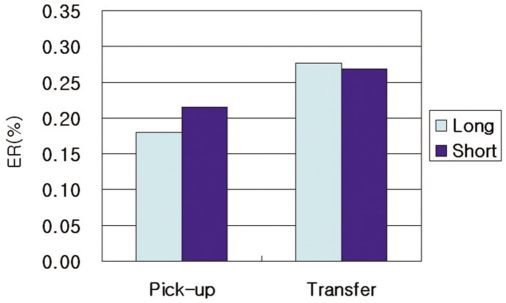
The distances between the analogs in the master model and the experimental model were measured. The error rate (ER) was calculated to compare each group (Table 1).
Table 1.
Error rate (%) between impression methods
*Mean (SD), D1: center to the parallel analog, D2: center to the mesial angulated analog
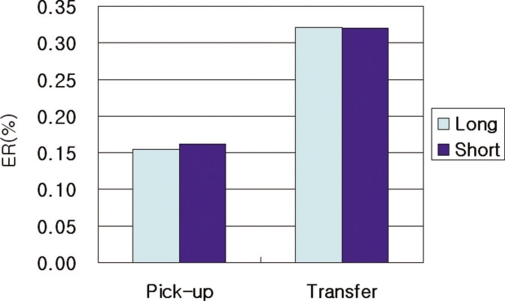
The mean (standard deviation) values in D1 were 0.155% (± 0.054) for the PL group, 0.162% (± 0.112) for the PS group, 0.321% (± 0.177) for the TL group, and 0.320% (± 0.193) for the TS group. The mean (standard deviation) values in D2 were 0.180% (± 0.076) for the PL group, 0.215% (± 0.091) for the PS group, 0.277% (± 0.204) for the TL group, and 0.269% (± 0.355) for the TS group (Fig. 5, 6).
Fig. 5.
Error rate (%) of the D1 position.
Fig. 6.
Error rate (%) of the D2 position.
The error rates in D1 and D2 decreased in the order of the PL, PS, TS, and TL groups.
A significant difference was observed between the type of impression coping in D1 (P < .05) but not in D2 (Table 2).
Table 2.
Analysis of variance for the comparison of the type and length with respect to the error rate (%)
*statistically significant difference
The lengths of the impression coping were not significantly different for both D1 and D2 (Table 2). The PL group exhibited the lowest error rates among all of the groups.
The error rates did not differ between D1 and D2.
DISCUSSION
Typically, two methods, the strain gauge method and measuring method are used to compare the accuracy of the impression. In this study, the relative difference in the distance was measured using a two-dimensional measuring microscope. The measuring method consisted of setting a measuring point as the x-axis and the y-axis and then determining the linear distance using the Pythagorean theorem: d2 = Δx2 + Δy2.
The distance between the analogs was set at 10 mm based on the clinical distance of the molars in the posterior area. The mesial angulated analog was tilted 10°. The internal connected implant used in this study could have a maximum angulation of 22° because of its 11° internal tapered surface. Therefore, a medium value of about 10° was used. The measuring point of each analog was the top center of the central analog.
The error rate was used to compare each group. Barrett13 measured the absolute distortion value of each implant using an external measurement point because a difference between the distance of the two points (10.0 and 9.8 mm) due to angulation. However, in this study, the relative displacement was measured using each implant as the other implant's measuring point in order to obtain more clinical results.14
Vinyl polysiloxane and polyether impression materials are recommended for the implant impression.15,16 In this study, the vinyl polysiloxane impression material was used in a one-step method. Wenz et al.17 reported that the one-step vinyl polysiloxane method was more accurate than the two-step method or medium body vinyl polysiloxane or polyether methods.
In this study, D1 was defined as the distance between the top middle of the center analog and the parallel positioned analog, and D2 was defined as the distance from the center to the mesial angulated analog. The TL and TS groups exhibited significantly high error rates in D1, with values of 0.321% and 0.320%, respectively (P < .05). The error rates for the PS and PL groups were 0.162 and 0.155%, respectively. The TL group exhibited the highest error rate of 0.277% in D2, followed by the TS, PS, and PL groups. No significant difference was observed between these error rates (P > .05).
In this study, the impression copings were divided into two types of coping, pick-up and transfer. The pick-up type exhibited a lower ER than the transfer type for D1 and D2 because it was fixed in the impression material and, therefore, more stable during the removal of the impression material and the pouring of gypsum. On the other hand, the transfer type was repositioned into the impression by connecting the analog out of the mouth.18-21
However the difference was not statistically significant in D2 (P = .055). The internal connected implants that were used in this study had a larger contact surface than the external connection, and the 10° mesial angulation was relatively large, especially in this system. Therefore, the impression material was easily distorted during the separation of analog, and the pick-up type of impression coping caused friction on the internal interface.11
The lengths of the impression coping were not significantly different in both D1 and D2. Lee et al.12 reported that the implant depth (4 mm) did not affect the dimensional accuracy of the putty and the light-body combination VPS impressions for the exposed length of the impression coping. These results suggested that short impression coping length (11 mm) satisfied the minimum length for the impression material, and this length can be utilized to make impression copings in the future.
In a direct comparison, the distances of D1 and D2 were not significantly different. Choi11 and Conrad et al.22 also reported the conditions were not different when two or three implants were used. However, Assuncao et al.16 and Carr18 reported that the parallel model was more accurate than the angulated implant when four or five implants were used.
Consequently, the accuracy of the master cast was mainly affected by the type of impression coping rather than the length. Therefore, accurate master casts could be fabricated using the pick-up type of impression coping, regardless of the length.
In this study, the mean error rate ranged from 0.155 - 0.321%. However, an inherent error was caused by the experimental material itself, so a careful interpretation was needed. Ma et al.23 reported that the gap between implant components is 22 - 100 µm, and Rubenstein and Ma24 reported the 23.1 - 51.7 µm gap.
This study was limited by the lack of a 3-dimensional analysis, which included the rotation of the axis, because a 2-dimensional measuring microscope was used. Furthermore, this experimental study is difficult to apply to different clinical situations. Therefore, an additional study is necessary in order to examine a multiple implant arrangement, with various angulations, depths, and other impression materials in the future.
CONCLUSION
The following conclusions were drawn from the distance measurements between the analogs in the master model and the experimental model.
The pick-up type impression coping had a more accurate model than the transfer type in the parallel group.
The accuracy of the models did not differ according to the length of the impression coping of at least 11 mm.
The parallel group and the 10° mesial angulated group were not different with respect to the accuracy of the model.
ACKNOWLEDGEMENTS
The authors thank the financial help for this research from OSSTEM Co. Korea.
References
- 1.Adell R, Lekholm U, Rockler B, Brånemark PI. A 15-year study of osseointegrated implants in the treatment of the edentulous jaw. Int J Oral Surg. 1981;10:387–416. doi: 10.1016/s0300-9785(81)80077-4. [DOI] [PubMed] [Google Scholar]
- 2.Brånemark PI. Osseointegration and its experimental background. J Prosthet Dent. 1983;50:399–410. doi: 10.1016/s0022-3913(83)80101-2. [DOI] [PubMed] [Google Scholar]
- 3.Rangert B, Jemt T, Jörneus L. Forces and moments on Brånemark implants. Int J Oral Maxillofac Implants. 1989;4:241–247. [PubMed] [Google Scholar]
- 4.Kan JY, Rungcharassaeng K, Bohsali K, Goodacre CJ, Lang BR. Clinical methods for evaluating implant framework fit. J Prosthet Dent. 1999;81:7–13. doi: 10.1016/s0022-3913(99)70229-5. [DOI] [PubMed] [Google Scholar]
- 5.Carr AB, Gerard DA, Larsen PE. The response of bone in primates around unloaded dental implants supporting prostheses with different levels of fit. J Prosthet Dent. 1996;76:500–509. doi: 10.1016/s0022-3913(96)90008-6. [DOI] [PubMed] [Google Scholar]
- 6.Jemt T, Book K. Prosthesis misfit and marginal bone loss in edentulous implant patients. Int J Oral Maxillofac Implants. 1996;11:620–625. [PubMed] [Google Scholar]
- 7.Michaels GC, Carr AB, Larsen PE. Effect of prosthetic superstructure accuracy on the osteointegrated implant bone interface. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1997;83:198–205. doi: 10.1016/s1079-2104(97)90006-8. [DOI] [PubMed] [Google Scholar]
- 8.Jemt T, Lekholm U, Johansson CB. Bone response to implant-supported frameworks with differing degrees of misfit preload: in vivo study in rabbits. Clin Implant Dent Relat Res. 2000;2:129–137. doi: 10.1111/j.1708-8208.2000.tb00003.x. [DOI] [PubMed] [Google Scholar]
- 9.Burns J, Palmer R, Howe L, Wilson R. Accuracy of open tray implant impressions: an in vitro comparison of stock versus custom trays. J Prosthet Dent. 2003;89:250–255. doi: 10.1067/mpr.2003.38. [DOI] [PubMed] [Google Scholar]
- 10.Lee H, So JS, Hochstedler JL, Ercoli C. The accuracy of implant impressions: a systematic review. J Prosthet Dent. 2008;100:285–291. doi: 10.1016/S0022-3913(08)60208-5. [DOI] [PubMed] [Google Scholar]
- 11.Choi JH, Lim YJ, Yim SH, Kim CW. Evaluation of the accuracy of implant-level impression techniques for internal-connection implant prostheses in parallel and divergent models. Int J Oral Maxillofac Implants. 2007;22:761–768. [PubMed] [Google Scholar]
- 12.Lee H, Ercoli C, Funkenbusch PD, Feng C. Effect of subgingival depth of implant placement on the dimensional accuracy of the implant impression: an in vitro study. J Prosthet Dent. 2008;99:107–113. doi: 10.1016/S0022-3913(08)60026-8. [DOI] [PubMed] [Google Scholar]
- 13.Barrett MG, de Rijk WG, Burgess JO. The accuracy of six impression techniques for osseointegrated implants. J Prosthodont. 1993;2:75–82. doi: 10.1111/j.1532-849x.1993.tb00387.x. [DOI] [PubMed] [Google Scholar]
- 14.Wee AG. Comparison of impression materials for direct multi-implant impressions. J Prosthet Dent. 2000;83:323–331. doi: 10.1016/s0022-3913(00)70136-3. [DOI] [PubMed] [Google Scholar]
- 15.Wenz HJ, Hertrampf K. Accuracy of impressions and casts using different implant impression techniques in a multi-implant system with an internal hex connection. Int J Oral Maxillofac Implants. 2008;23:39–47. [PubMed] [Google Scholar]
- 16.Assuncao WG, Filho HG, Zaniquelli O. Evaluation of transfer impressions for osseointegrated implants at various angulations. Implant Dent. 2004;13:358–366. doi: 10.1097/01.id.0000144509.58901.f7. [DOI] [PubMed] [Google Scholar]
- 17.Carr AB, Master J. The accuracy of implant verification casts compared with casts produced from a rigid transfer coping technique. J Prosthodont. 1996;5:248–252. doi: 10.1111/j.1532-849x.1996.tb00507.x. [DOI] [PubMed] [Google Scholar]
- 18.Carr AB. Comparison of impression techniques for a five-implant mandibular model. Int J Oral Maxillofac Implants. 1991;6:448–455. [PubMed] [Google Scholar]
- 19.Assif D, Fenton A, Zarb G, Schmitt A. Comparative accuracy of implant impression procedures. Int J Periodontics Restorative Dent. 1992;12:112–121. [PubMed] [Google Scholar]
- 20.Phillips KM, Nicholls JI, Ma T, Rubenstein J. The accuracy of three implant impression techniques: A three-dimensional analysis. Int J Oral Maxillofac Implants. 1994;9:533–540. [Google Scholar]
- 21.Rodney J, Johansen R, Harris W. Dimensional accuracy of two implant impression copings. J Dent Res. 1991;70:385. [Google Scholar]
- 22.Conrad HJ, Pesun IJ, DeLong R, Hodges JS. Accuracy of two impression techniques with angulated implants. J Prosthet Dent. 2007;97:349–356. doi: 10.1016/S0022-3913(07)60023-7. [DOI] [PubMed] [Google Scholar]
- 23.Ma T, Nicholls JI, Rubenstein JE. Tolerance measurements of various implant components. Int J Oral Maxillofac Implants. 1997;12:371–375. [PubMed] [Google Scholar]
- 24.Rubenstein JE, Ma T. Comparison of interface relationships between implant components for laser-welded titanium frameworks and standard cast frameworks. Int J Oral Maxillofac Implants. 1999;14:491–495. [PubMed] [Google Scholar]