Abstract
Background
Myasthenia gravis (MG) is occasionally aggravated by chronic infection, of which there are many kinds.
Case Report
We report herein the case of a 56-year-old woman with MG aggravated by the activation of isolated mediastinal tuberculous lymphadenitis (MTL) during corticosteroid administration. The possibility of MTL had been disregarded in the differential diagnosis of aggravation of MG weakness, because MTL without pulmonary manifestations is uncommon even in areas where tuberculosis is endemic.
Conclusions
This case suggests that chronic infections such as tuberculosis should be considered in myasthenic patients with progressive exacerbation if definite evidence for aggravating factors of MG is not obtained.
Keywords: tuberculous lymphadenitis, myasthenia gravis, steroids
Introduction
Myasthenia gravis (MG) can be aggravated by various autoimmune or rheumatologic diseases, thyroid dysfunction, and infectious conditions. These conditions may not only interfere with immunosuppressive treatment, but they may also exacerbate myasthenic weakness by immune dysregulation.1
Tuberculous infection is common in developed countries due to an increase in immigration, the pandemic outbreak of HIV infection, and drug-resistant mycobacterium tuberculosis (Mycobacterium tuberculosis) infection.2 Most tuberculous infections are located in the lung, but reported 5-15% of such infections affect extrapulmonary tissues. In addition, lymph nodes are reportedly involved in 30-50% of patients with extrapulmonary tuberculosis, the most frequently involved site being the cervical lymph nodes.3,4 However, isolated mediastinal tuberculous lymphadenitis (MTL) without any pulmonary manifestations is extremely uncommon.
MG is known to be exacerbated during unsuspected infectious illnesses such as tuberculous infection. It has been demonstrated that corticosteroid therapy in patients with unrecognized or untreated tuberculosis can lead to the reactivation of M. tuberculosis.5 However, it is not easy to predict the possibility of isolated MTL due to the lack of constitutional tuberculous symptoms and signs. We present herein a case of myasthenic weakness aggravated by steroid-induced isolated MTL.
Case Report
A 56-year-old woman with previously well-controlled MG was admitted to our hospital because of myasthenic symptoms that had progressively aggravated over a period of several months. She did not complain of fever, weight loss, cough, sputum, or sweating at nighttime, although she did complain of mild gastric discomfort. Her history was unremarkable except for the MG, and a family history of tuberculous infection was absent. She had been diagnosed with ocular MG in a private neurology clinic 2 years previously. Her initial symptom was only fluctuating ptosis of the right eyelid, which responded to pyridostigmine (180 mg/day). At the onset of MG symptoms, the diagnosis of MG was made on the basis of increased levels of anti-acetylcholine receptor antibody (AChR-Ab, 2.3 nmol/L; normal, 0.2 nmol/L) and an abnormal decremental response (-11%, -14%, and -14% at stimulation intensities of 2, 3, and 5 Hz, respectively) in the orbicularis oculi muscle. Computed tomography (CT) of the chest revealed normal findings. Small dosages of corticosteroids (15 mg/day prednisone) and oral pyridostigmine (180-240 mg/day) had been administered to control the ocular myasthenia 7 months prior to admission to our hospital. However, this patient had been given higher dosages of oral prednisone (30 mg/day) and pyridostigmine (360 mg/day) because of uncontrolled myasthenic weakness for the 3 months prior to her admission. On admission to our hospital, a neurological examination revealed bilateral ptosis, ophthalmoplegia, diplopia, mild dysphagia, and generalized muscle weakness in all four extremities, without any respiratory symptoms. These symptoms were consistent with grade IIB according to a modified Osserman's classification. The serological AChR-Ab level was 5.4 nmol/L. We performed laboratory evaluations to determine the presence of various risk factors that can exacerbate myasthenic symptoms. The erythrocyte sedimentation rate was 69 mm/h, and the level of C-reactive protein was within the normal limits. Tests for serum creatine kinase, HIV, hepatitis B surface antigen, antinuclear antibody, antineutrophil cytoplasmic antibody, anti-SS-A/B, anti-smooth-muscle antibody, rheumatoid factor, proteins C and S, CH50/C3/C4 complement, and lupus-anticoagulant were negative. Thyroid function tests were also negative. A chest X-ray did not show any parenchymal, pleural, or mediastinal involvement. A follow-up chest CT revealed multiple enlarged lymph nodes in the anterior mediastinum without any thymic abnormalities or pulmonary tuberculosis (Fig. 1). Transbronchial needle aspiration was not performed due to the deep location of the affected lymph node. Lymph node biopsy by mediastinoscopy revealed chronic granulomatous inflammation without any malignant cells. We considered that the newly developed isolated MTL was an aggravating factor for MG. An empirical antituberculous regimen of isoniazid, rifampicin, ethambutol, and pyrazinamide was started. In addition, oral pyridostigmine (360 mg/day) combined with azathioprine (100 mg/day) and no oral prednisone were administered in order to control aggravated myasthenic weakness. Two months after mediastinal lymph node biopsy, M. tuberculosis was isolated from the biopsied specimen culture. At a 12-month follow-up examination, ocular and bulbar symptoms, and generalized muscle weakness persisted. Follow-up chest CT revealed an increase in the size of the previously observed mediastinal lymph nodes. We regarded this to be a treatment failure due to multidrug-resistant tuberculosis, and second-line antituberculosis agents including prothionamide, cycloserine, and para-aminosalicylic acid were administered for the following 24 months. Three years after the administration of second-line antituberculosis agents, the patient achieved complete clinical remission of MG symptoms, and she has been off the anticholinesterase inhibitor and azathioprine medication for more than 12 months.
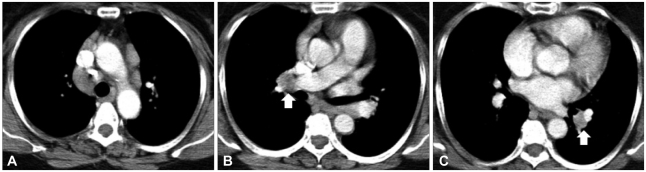
Fig. 1.
The contrast-enhanced computed tomography images of the chest in the patient with mediastinal tuberculous lymphadenitis. A: Multiple lymphadenopathies with conglomerate and homogenous enhancement in the anterior mediastinum, right lower paratracheal area, and aortopulmonary window. B and C: Enlarged lymph nodes with central low attenuation and peripheral rim enhancement in both hilar areas (arrow)
Discussion
MG is a neuromuscular transmission disorder that is characterized by easy fatigability and muscle weakness. It is an autoimmune disease that is associated with antibodies such as AChR-Ab at the neuromuscular junction. Patients with MG have an increased incidence of several associated conditions that may exacerbate the myasthenic weakness, including hyper- or hypothyroidism, occult infection, medical treatment for other disorders, emotional stress, and pregnancy.1 In our case the only MG-aggravating factor present was isolated MTL. Approximately 85% of all tuberculous infections occur in the lungs, the remaining being found in the extrapulmonary tissues. Typically 30-50% of extrapulmonary tuberculous infections affect the lymph nodes.3,4 Geldmacher et al.3 reported that lymph node involvement in extrapulmonary tuberculosis is most frequently found in the cervical lymph nodes, followed by the mediastinal, axillary, and inguinal lymph nodes, and that the incidence of lymph node tuberculosis without pulmonary involvement is approximately 5.2%, whereas that of isolated MTL is around 1.4%. Therefore, isolated MTL is not generally suspected because of the lack of constitutional symptoms, absence of an exposure history and palpable lymph nodes, and its low incidence.2,3 Thus, the diagnosis and treatment of tuberculous infections in patients with isolated MTL may often be significantly delayed. Unfortunately, it has been reported that corticosteroid therapy in patients with untreated or unrecognized tuberculosis results in overwhelming disease and consequent death.
Corticosteroids are the most commonly used and most consistently effective immunosuppressive agents in the treatment of MG. They may reduce the serum AChR-Ab level and diminish the AChR reactivity of peripheral blood lymphocytes.6 However, prolonged administration of corticosteroids often induces an increased susceptibility to infection. Patients who are given prolonged corticosteroid therapy may be at risk for the exacerbation of primary tuberculosis and the reactivation of inactive tuberculosis, although the precise risk has not been elucidated.7 In our case the patient complained of further aggravated myasthenic weakness after corticosteroid administration. It is generally known that administration of corticosteroids can lead to a transient exacerbation of myasthenic weakness within several weeks. However, the condition of our patient was inconsistent with steroid-induced exacerbation of MG because she complained of gradual myasthenic weakness over a period of several months, and the initial daily dose of oral prednisone was low.
Together these findings suggest that the possibility of tuberculous infections is often ignored in patients with various types of tuberculous infections without pulmonary symptoms or palpable lymph nodes. Therefore, in MG patients receiving long-term corticosteroid therapy, careful practical approaches to the screening of tuberculosis by chest radiography, tuberculin skin testing, and sputum examination are mandatory. In addition, further diagnostic tools such as CT or magnetic resonance imaging are required because extrapulmonary tuberculosis occasionally occurs in anatomic regions such as the lymph nodes and the skeletal or genitourinary systems. If chest CT to detect tuberculous infections had been performed sooner after the symptom aggravation in our patient, the comorbidity and treatment duration may have been reduced.
In conclusion, the possibility of chronic infections such as tuberculosis should be considered in MG patients receiving long-term corticosteroids who show progressive exacerbation of myasthenic weakness without other aggravating factors.
Footnotes
The authors have no financial conflicts of interest.
References
- 1.Drachman DB. Myasthenia gravis. N Engl J Med. 1994;330:1797–1810. doi: 10.1056/NEJM199406233302507. [DOI] [PubMed] [Google Scholar]
- 2.Venkateswaran RV, Barron DJ, Brawn WJ, Clarke JR, Desai M, Samuel M, et al. A forgotten old disease: mediastinal tuberculous lymphadenitis in children. Eur J Cardiothorac Surg. 2005;27:401–404. doi: 10.1016/j.ejcts.2004.12.014. [DOI] [PubMed] [Google Scholar]
- 3.Geldmacher H, Taube C, Kroeger C, Magnussen H, Kirsten DK. Assessment of lymph node tuberculosis in northern Germany: a clinical review. Chest. 2002;121:1177–1182. doi: 10.1378/chest.121.4.1177. [DOI] [PubMed] [Google Scholar]
- 4.Lazarus AA, Thilagar B. Tuberculous lymphadenitis. Dis Mon. 2007;53:10–15. doi: 10.1016/j.disamonth.2006.10.001. [DOI] [PubMed] [Google Scholar]
- 5.Cunba BA. Pulmonary tuberculosis and steroids. Chest. 1995;107:1486–1487. doi: 10.1378/chest.107.6.1486. [DOI] [PubMed] [Google Scholar]
- 6.Tindall RS. Humoral immunity in myasthenia gravis: effect of steroids and thymectomy. Neurology. 1980;30:554–557. doi: 10.1212/wnl.30.5.557. [DOI] [PubMed] [Google Scholar]
- 7.Cisneros JR, Murray KM. Corticosteroids in tuberculosis. Ann Pharmacother. 1996;30:1298–1303. doi: 10.1177/106002809603001115. [DOI] [PubMed] [Google Scholar]