Abstract
INTRODUCTION
Traditionally, the cervicomastoidfacial (CMF) incision is used to excise benign tumours of the parotid gland. The rhytidectomy or modified facelift (MF) incision allows an alternative approach which leaves no visible neck scar. The objective of this study was to establish the frequency of each surgical approach used and identify any difference in complication and patient satisfaction between the two incisions for benign conditions of the parotid gland.
PATIENTS AND METHODS
A retrospective analysis of 101 case notes for patients who underwent parotidectomy by both ENT and maxillofacial departments between January 2006 and February 2008 was undertaken. All histologically confirmed cases of malignancy were excluded. For each incision, immediate postoperative complications were obtained from the notes. A postal patient outcome evaluation questionnaire sought information regarding persistent and late complications as well as a visual analogue scar satisfaction score for both incisions.
RESULTS
Overall, 79 parotidectomies were included (59 CMF incisions, 20 MF incisions). Of CMF incisions, 34% suffered facial weakness immediately postoperatively versus 20% of MF incisions. Of CMF incisions, 4% suffered postoperative haematomas versus none following MF incisions. In the study cohort, 47 (60%) responded to the postal feedback questionnaire (33 CMF versus 14 MF respondents). Information regarding immediate and late postoperative ipsilateral facial paraesthe-sia and gustatory sweating was obtained. Mean visual analogue scar satisfaction scores were 9.4 for CMF incisions and 8.9 for MF incisions.
CONCLUSIONS
Immediate and late complications for CMF and MF approaches for benign disease parotidectomy were comparable, but scar satisfaction following MF incision was not greater than CMF incisions.
Keywords: Parotidectomy, Rhytidectomy, Parotid neoplasm, Treatment outcome
Indications for parotidectomy include benign and malignant tumours as well as inflammatory conditions of the parotid gland.1 Traditionally, the cervicomastoidfacial incision (alternatively known as the modified Blair incision) is used for surgery of the parotid gland which offers excellent surgical access to the parotid gland, but leaves a visible scar in the neck. Alternatively, for suspected benign tumours, a more cosmetic modified facelift (rhytidectomy) incision can be considered which leaves no visible neck scar.2 At the Luton & Dunstable Hospital, parotidectomy is performed by ear nose and throat (ENT) and maxillofacial surgeons. We retrospectively analysed parotidectomies performed by both departments over a 2-year period. The aim of this study was to establish the frequency of each surgical approach used and to identify any difference in complication and patient satisfaction of the operative scar between the two incisions.
Patients and Methods
A retrospective analysis of case notes for patients who underwent parotidectomy by both ENT and maxillofacial departments between January 2006 and February 2008 was undertaken. All operations were either performed or supervised by a consultant. Only benign indications for parotidectomy were considered for this study; thus, histologically confirmed cases of malignancy were excluded. The numbers of patients who underwent parotidectomy via a cervicomastoidfacial and modified facelift incision were counted. For each incision, details regarding immediate postoperative facial nerve weakness and wound haematoma were obtained from the notes. A patient-outcome evaluation questionnaire was posted to all included patients at least 6 months following their parotid surgery. Information regarding facial paraesthesia and gustatory sweating was sought, as well as a satisfaction score of their operative scar on a 0–10 visual analogue scale (VAS), where 0 indicates very unhappy and 10 very happy. Outcome data were compared for both incisions.
Results
Between January 2006 and February 2008, 101 parotidectomies were performed collectively by both departments (62 by maxillofacial and 39 by ENT). After excluding all histologically confirmed cases of malignancy, data for 79 parotidectomies were considered. Of these 79 cases, 59 (75%) were performed via a cervicomastoidfacial incision and 20 (25%) were performed via a modified facelift incision. All 79 patients were sent a patient-outcome evaluation questionnaire, of which 47 were returned (response rate of 60%). These 47 respondents included 33 cervicomastoidfacial incisions and 14 modified facelift incisions. Table 1 lists patient demographics and immediate postoperative complications, the latter of which are illustrated in Figure 1. Table 2 lists patient feedback from respondents, with graphical representations in Figures 2 and 3. No statistical testing of outcome results were performed due to poor numbers involved in the study and disparity in patient numbers between the modified facelift and cervicomastoid incision groups.
Table 1.
Patient demographics and immediate documented postoperative complications
| Cervicomastoidfacial (n = 59) | Modified facelift (n = 20) | |||
|---|---|---|---|---|
| Number | % | Number | % | |
| M:F | 29:30 | 11:9 | ||
| Age range years (mean) | 17–82 (51) | 17–75 (44) | ||
| Facial palsy | 20 | 34 | 4 | 20 |
| Wound haematoma | 4 | 7 | 0 | 0 |
| Patient feedback | 33 | 56 | 14 | 70 |
Figure 1.
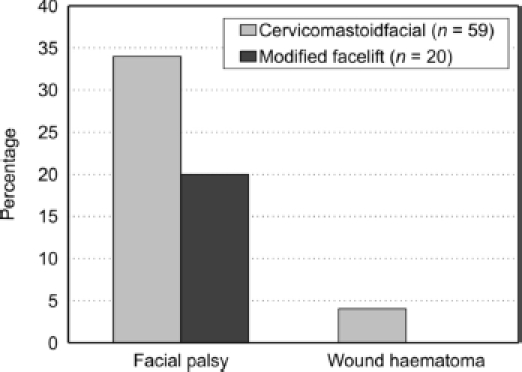
Immediate postoperative complications.
Table 2.
Postal questionnaire feedback
| Cervicomastoid-facial (n = 33) | Modified facelift (n = 14) | |||
|---|---|---|---|---|
| Number | % | Number | % | |
| Immediate postoperative paraesthesia | 33 | 100 | 13 | 93 |
| Paraesthesia recovery | ||||
| Complete | 8 | 24 | 3 | 22 |
| Partial | 19 | 58 | 9 | 64 |
| None | 6 | 18 | 1 | 7 |
| Gustatory sweating | 9 | 27 | 1 | 7 |
| Mean scar satisfaction | 9.4 | 8.9 | ||
Figure 2.
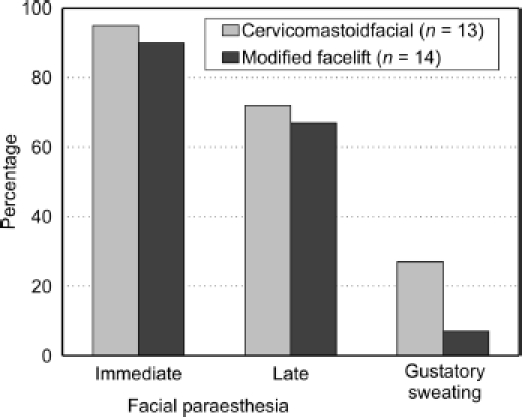
Postal questionnaire feedback of persistent and late post-operative complications.
Figure 3.
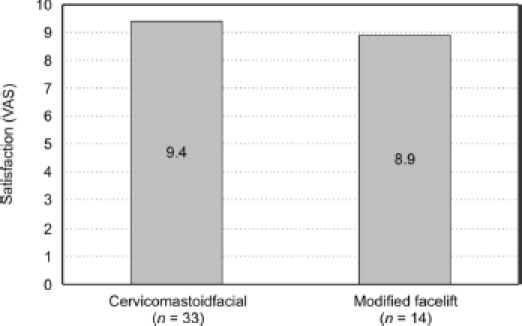
Mean visual analogue satisfaction score of postoperative scar.
Discussion
In the interest of cosmesis, a modified facelift (rhytidectomy) incision for exposing the parotid gland was first described in 1967.3 Studies have demonstrated that for benign indications for parotidectomy, a modified facelift incision can be performed with a similar incidence of complication and length of surgery when compared with the cervicomastoidfacial incision.2 Both incisions commence as a pre-auricular incision, winding underneath the ear lobe to the mastoid tip. The cervicomastoidfacial incision then curves downwards along a skin crease in the neck approximately 3 cm below the mandible (Fig. 4). The modified facelift incision alternatively extends superiorly from the mastoid tip, along the postauricular sulcus, up to the occipital hairline and then descends just inside and parallel to this hairline for a variable distance depending on the access required (Fig. 4). The modified facelift is technically more challenging as access to the gland is more difficult, but it provides a cosmetically superior scar. Due to increased technicality, the modified facelift incision is recommended only for suspected benign lesions of the parotid gland.2
Figure 4.
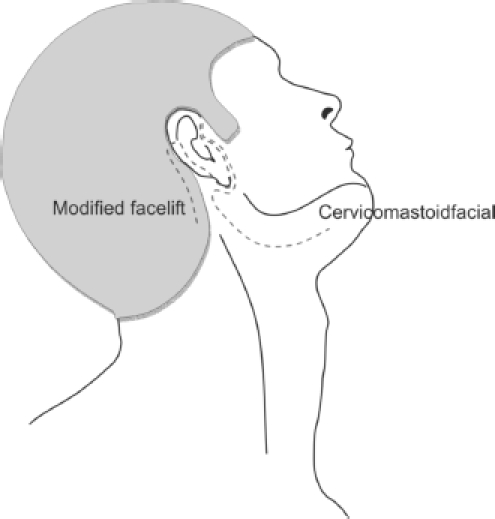
Schematic diagram illustrating the course of the modified facelift incision and the cervicomastoidfacial incision.
Of the 101 parotidectomies considered for this study, 22 were histologically diagnosed as malignant neoplasms and were excluded. The remaining 79 histologically confirmed benign neoplasms formed the study cohort. This ratio of incidence of malignant to benign parotid gland neoplasm (22% to 78%, respectively) correlates well with existing literature.4 Of the 79 benign parotid neoplasms excised, only 25% were performed via a modified facelift approach with the remainder performed via a cervicomastoidfacial incision. The latter is, therefore, the more popular incision used within both ENT and maxillofacial departments and probably reflects the improved surgical access offered by this incision. Immediate postoperative complications of lower motor neurone facial palsy (complete and partial) and wound haematoma also correlate well with the existing literature1,5 but are surprisingly higher for cervicomastoidfacial incisions compared with modified facelift incisions. The large disparity in numbers within the two groups probably accounts for this observation.
Of the 79 included patients, 47 (60%) responded to the postal feedback questionnaire, comprised of 33 cervicomastoidfacial and 14 modified facelift incisions. The time of feedback collection ranged between 6–30 months following surgery for included patients. Again, there is a large difference in numbers between the two groups. All respondents bar one in the modified facelift incision group reported either total or partial numbness/paraesthesia about the ipsilateral cheek and ear immediately postoperatively. This improved to 76% still affected in the cervicomastoidfacial incision group versus 71% for modified facelift incisions at the time of feedback collection, which is comparable in both groups. Documented, subjective, post-parotidectomy numbness and paraesthesia varies in the literature. One study documented a similar incidence of 94% subjective numbness and paraesthesia immediately post partidectomy,6 whereas another study reported only 66.2% short-term impaired sensation reducing to 30.6% at 1 year.5 Gustatory sweating affected more patients following a cervicomastoidfacial incision (27%) than a modified facelift approach (7%). This difference may, in part, be explained by the fact that the modified facelift approach will tend to be favoured for smaller, posteriorly placed benign tumours, requiring less parotid gland dissection and less disruption to its parasympathetic nerve supply. It is difficult to correlate this to that published in the literature as there is large variation in incidence of gustatory sweating between studies which range from 4–57%.5–7 The modified facelift incision is performed to avoid a neck scar and, therefore, improve cosmetic outcome, but no study has yet measured or compared patient satisfaction of the surgical scar for each approach. Both surgical incisions scored highly in terms of patient satisfaction of postoperative scar on a visual analogue scale, but was surprisingly higher for cervicomastoidfacial incisions (9.4) than modified facelift incisions (8.9). This suggests that the neck scar left by the cervicomastoidfacial incision is not a concern for the patient.
Study limitations
There are many limitations to this study in that numbers were small, only one-quarter of patients underwent modified facelift and only 60% responded to our feedback questionnaire. Although our results provide a preliminary insight contrasting complication rates and satisfaction between the two parotidectomy approaches, a larger, prospective, randomised, controlled trial with ethical approval is required to generate greater and equal numbers in each cohort. This will enable fair comparisons to be made, strengthened with statistical testing of any differences observed.
Conclusions
In this study, we have demonstrated that patients who underwent parotidectomy for benign tumours via the modified facelift approach experienced lower, although similar, rates of complication with regards to immediate facial palsy, wound haematoma, ipsilateral facial paraesthesia and gustatory sweating to the cervicomastoidfacial approach. However, the modified facelift approach did not improve patient satisfaction of the postoperative scar compared with cervicomastoidfacial incisions. Although this study supports the modified facelift incision as a safe approach for parotidectomy for benign disease of the parotid gland, it conveys no cosmetic advantage over the cervicomastoid facial incision. A larger, prospective, randomised, controlled trial is required to prove this definitively; if true, the choice of a modified facelift incision to provide a cosmeti-cally superior scar should be questioned, given the increased technical difficulty of parotidectomy via this approach.
References
- 1.Bova R, Saylor A, Coman W. Parotidectomy: review of treatment and outcomes. Aust NZ J Surg. 2004;74:563–8. doi: 10.1111/j.1445-2197.2004.02988.x. [DOI] [PubMed] [Google Scholar]
- 2.Terris JD, Tuffo KM, Fee WE. Modified facelift incision for parotidectomy. J Laryngol Otol. 1994;108:574–8. doi: 10.1017/s002221510012746x. [DOI] [PubMed] [Google Scholar]
- 3.Appiani A. Surgical management of parotid tumours. Revista Argentina de Cirugia. 1967;21:236. [Google Scholar]
- 4.Johns ME, Goldsmith MM. Incidence, diagnosis and classification of salivary gland tumours. Oncology. 1989;3:47–56. [PubMed] [Google Scholar]
- 5.Marshall AH, Quraishi SM, Bradley PJ. Patients' perspectives on the short and long term outcomes following surgery for benign parotid neoplasms. J Laryngol Otol. 2003;117:624–9. doi: 10.1258/002221503768199960. [DOI] [PubMed] [Google Scholar]
- 6.Nitzan D, Kronenberg J, Horowitz Z, Wolf M, Bedrin L, et al. Quality of life following parotidectomy for malignant and benign disease. Plast Reconstr Surg. 2004;114:1060–7. doi: 10.1097/01.prs.0000135326.50939.c1. [DOI] [PubMed] [Google Scholar]
- 7.Guntinas-Lichius O, Gabriel B, Kluusman P. Risk of facial palsy and Frey's syndrome after conservative parotidectomy for benign disease: analysis of 610 operations. Acta Otolaryngol. 2006;126:1104–9. doi: 10.1080/00016480600672618. [DOI] [PubMed] [Google Scholar]


