Abstract
INTRODUCTION
The objective of this study was to investigate the impact of the 2-week wait rule on patient waiting times for the diagnosis and treatment of bladder cancer.
PATIENTS AND METHODS
Data reporting the waiting times from diagnosis to treatment for 100 consecutive patients newly diagnosed with bladder cancer immediately before and after the implementation of the 2-week wait rule were compared. The data were collected both prospectively and retrospectively from cancer multidisciplinary team meeting files and patient records. Various steps of the patient pathway were analysed including waiting times from referral to consultation as well as time to investigation and first treatment. Data were also analysed based upon tumour stage/grade and whether referrals were made on an urgent or routine basis.
RESULTS
One hundred newly diagnosed patients with bladder cancer in each group covered a period of 4–5 years (1997–2001 and 2001–2006). Following the introduction of the 2-week wait rule, there was a 47.6% reduction in the time from referral to first consultation with a specialist (42 days vs 22 days; P < 0.001). The time between first investigation and treatment has not reduced significantly. We also found that, despite the introduction of the 2-week wait rule, only 42% of the patients were diagnosed with bladder cancer using this pathway. Patients referred as ‘routine’ waited longer to be seen in hospital although there was no significant delay in receiving treatment.
CONCLUSIONS
The introduction of the 2-week wait rule has significantly reduced the time patients with bladder cancer wait for their first consultation with a specialist. However, there is no significant change in the time between first consultation and treatment.
Keywords: Bladder cancer, Two-week wait rule, Diagnosis
Bladder cancer affects 32.5 per 100,000 of the population and there are approximately 10,000 newly diagnosed cases every year in the UK.1 The 5-year survival rate in the UK for patients with invasive bladder cancer is approximately 50% following a radical cystectomy and this is lower than those reported in other European countries.2,3 In order to improve outcomes, the NHS Cancer Plan was introduced by the Department of Health in 2000 and part of this plan included the 2-week wait rule for suspected urological malignancy which itself was introduced in 20014 and ensured that patients with suspected cancer did not have to wait longer than 2 weeks in order to see a specialist. The development of a standard proforma with a list of referral criteria ensured equality between the health authorities.
Specifically for patients with suspected bladder cancer, the referral guidelines are detailed below:
Male or female adult patients of any age who present with painless macroscopic haematuria should be referred urgently.
In patients aged 50 years and older who are found to have unexplained microscopic haematuria, an urgent referral should be made.
Any patient with an abdominal mass identified clinically or on imaging that is thought to be arising from the urinary tract should be referred urgently.
The majority of patients with bladder cancer will present with either macroscopic or microscopic haematuria. Studies have reported that 24–35% of patients with macroscopic haematuria will have an underlying tumour.5 However, the significance of microscopic haematuria in detecting invasive or high-grade disease is debatable and the overall effectiveness of the 2-week wait rule is now being questioned due to the poor predictive value and the number of inappropriate referrals.6,7
It has been shown for bladder cancer that delays in treatment from the onset of symptoms have a complex relationship with survival.8 Waiting times in the patient pathway comprise several components: time taken for patient to present to their GP, time from GP referral to first specialist consultation, time to first investigation and time to treatment. Following the implementation of the 2-week wait rule, the time from GP referral to hospital appointment should be minimised such that patients do not have to wait longer than 2 weeks to see a specialist. Whether this has been successful in reducing the time for the entire patient pathway as well as minimising time to treatment is still unclear.
This study analysed the impact of the introduction of the 2-week wait rule upon the time differences within the patient pathway specifically for patients with newly diagnosed bladder cancer.
Patients and Methods
A cohort of 200 consecutive patients with newly diagnosed bladder cancer was identified from the records of multidisciplinary team (MDT) meetings and theatre records. Of these, 100 patients were diagnosed with bladder cancer between 1997 and 2001 (pre 2001) and 100 patients between 2001 and 2006 (post 2001) such that the two groups were comparable and separated by the introduction of the 2-week wait rule in 2001. Patients who were already known to have bladder cancer and underwent transurethral resection of bladder tumour (TURBT) for recurrent lesions were excluded from the study. The patient pathway was divided into three key steps, which incorporated the main time differences.
| Time period 1 (P1) | Initial patient referral to hospital visit. |
| Time period 2 (P2) | Hospital visit to TURBT. |
| Time period 3 (P3) | TURBT to MDT. |
| Time period 1–3 (P1–3) | Overall time taken for the whole pathway from initial referral to the review of histology at the MDT meeting. |
The hospital visit in our unit encompassed either a visit to the out-patient department in order to instigate investigations or to the dedicated fast-track haematuria clinic (FTH clinic) where a flexible cystoscopy and ultrasound scan was performed at a single visit. Where patients were unable to be offered an FTH clinic appointment within 2 weeks, they were offered an out-patient appointment. The MDT meeting is a compulsory part of the cancer pathway as it allows for a review of the histology and formulation of a management plan and was deemed the end-point of the pathway. The components of the pathway are illustrated in Figure 1.
Figure 1.
The patient pathway for newly diagnosed bladder cancer.
A retrospective review of the patient records was performed in order to identify and record the time differences (P1–P3) involved in the patient pathway. The demographic data were recorded as well as the presenting symptoms and the eventual stage and grade of the tumours.
A sub-analysis of the post 2001 patients was performed in order to identify the number of patients that had been referred as routine or urgent.
We classed all those referred using the 2-week wait rule, those referred with suspected cancer or urgent stated on the referral letter as ‘urgent’. All other referrals were classed as ‘routine’.
Comparisons were also made between the modes of referral for patients with invasive or high-grade disease (T1G3 or ≥ T2 disease) compared to those with low-grade, non-muscle invasive, bladder cancer.
Statistical analysis
A Student's t-test was used in order to identify significant differences in time between pre and post 2001 patients at each stage of the pathway. Patients in each group were also subdivided into muscle invasive/high-grade bladder tumours and low-grade, non-muscle invasive, bladder tumours.
Results
The study included patients (n = 200) diagnosed over a 9-year period within a single centre. The pre 2001 patients comprised 78 males and 22 females with a mean age 72.9 years (range, 47–86 years) diagnosed with bladder cancer prior to 2001. The post 2001 patients comprised 80 males and 20 females with a mean age of 71.4 years (range, 51–87 years) diagnosed with bladder cancer after 2001. Therefore, the two groups were demo graphically similar.
The overall time differences for each stage of the pathway for the pre and post 2001 groups irrespective of the mode of referral were analysed initially (Fig. 2). There is a significant difference in P1 between those patients referred before and after 2001 (P < 0.001), demonstrating that the implementation of the 2-week wait rule has reduced P1 from 42.94 ± 2.35 days (mean ± SEM) to 21.30 ± 1.19 days. Following the implementation of the 2-week wait rule, there have been no significant reductions in the waiting time from patients being listed for a TURBT to undergoing this procedure and subsequent discussion at the MDT (P2 and P3). However, there has been a significant reduction in the time taken for the whole patient pathway (P1–3) from 74.44 ± 2.78 days prior to 2001 compared to 57.34 ± 1.98 days after 2001 (P < 0.001). More specifically within the pathway itself, Group A had the longest wait at P1 42.94 days (mean) and Group B at P2 23.94 days (mean).
Figure 2.
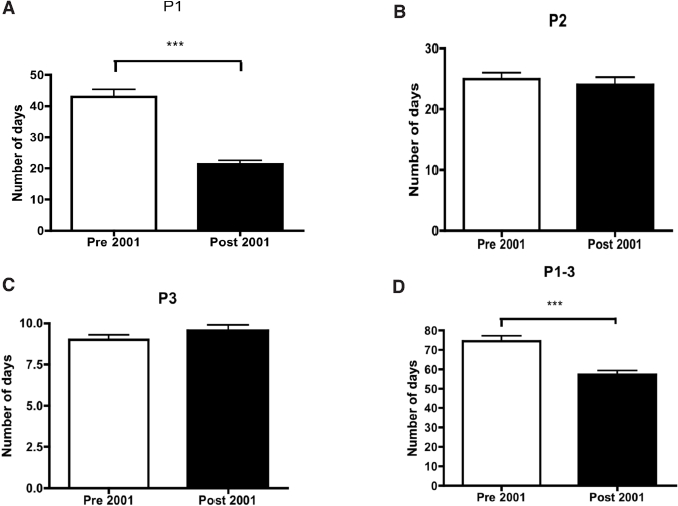
(A) A comparison of waiting times from referral to first consultation with a specialist between the pre and post 2001 patients. (B) A comparison of waiting times from first consultation and TURBT between the pre and post 2001 patients. (C) A comparison of waiting times from TURBT and discussion at MDT between pre and post 2001 patients. (D) A comparison of waiting times from referral to MDT discussion between pre and post 2001 patients.
Analysis of the referral pattern in the post 2001 cohort showed that only 42% of the referrals were ‘urgent’. Of the remaining 58%, 65% were referred as routine from primary care, 25% were emergency admissions and 10% were cross-referrals from other specialties.
Figure 3 demonstrates the difference in waiting times between urgent and routine referrals after the introduction of the 2-week wait rule (post 2001). There is a significant difference in P1 between 10.98 ± 0.735 days for the urgent group when compared to 28.50 ± 1.91 days for the routine group (P < 0.001). The waiting times P2 and P3 are similar for both groups, which would appear logical after suspicion of bladder cancer had been raised following their initial investigations one would expect the patient pathway to merge. The shorter waiting times seen at P1 in the urgent group transfer to the overall figures meaning that a significant difference is seen between the P1–3 waiting times of the urgent patients 43.12 ± 1.80 days and routine patients 67.44 ± 2.33 days (P < 0.001).
Figure 3.
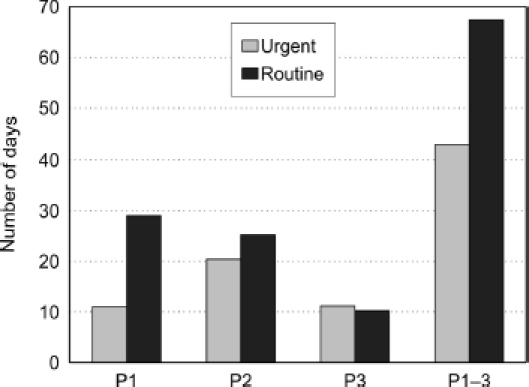
A comparison between waiting times for post 2001 patients depending whether the referral was urgent or routine.
After TURBT, tumour histology was also subdivided into invasive and high-grade (T1G3/CIS) bladder cancer or grade 1–2 non-muscle invasive bladder cancer. The distribution within pre and post 2001 cohorts according to histo-logical subtype is illustrated in Table 1.
Table 1.
Histological variation in the eventual bladder tumour diagnosed within each group
| Pre 2001 | |
| Invasive | 12 |
| Non-invasive | 68 |
| High-grade | 20 |
| Post 2001 | |
| Invasive | 21 |
| Non-invasive | 53 |
| High-grade | 26 |
A third analysis of the data was made based upon the tumour histology at TURBT in the pre and post 2001 patients as described in Table 1. The purpose of this analysis was to assess the impact of waiting times on those patients who have a worse prognosis and so would, therefore, be more likely to benefit from prompt referral, investigation and management. Notably, only 53% of patients diagnosed with high-grade or invasive bladder cancer post 2001 were referred as urgent, 87.5% of patients referred as urgent were seen within 2 weeks.
P1 for patients diagnosed with high-grade and muscle-invasive bladder cancer was shorter after 2001 (26.53 ± 2.46 days) compared to those before 2001 (39.53 ± 2.513 days; P < 0.001). There were no significant differences in P2 and P3; however, P1–3 was again significantly shorter in the post 2001 patients (59.43 ± 2.259 days) compared to 72.03 ± 4.26 days for pre 2001 patients (P = 0.0056).
The differences in waiting times depending on stage and grade is illustrated in Figure 4.
Figure 4.
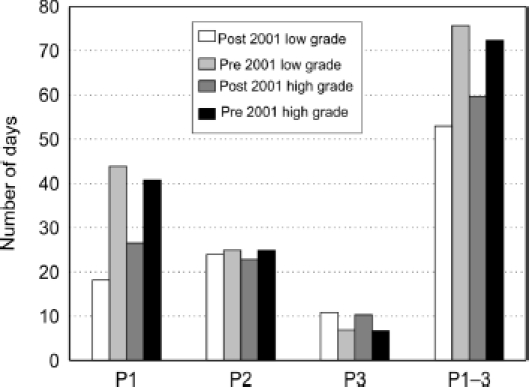
A comparison of waiting times depending upon tumour type.
Discussion
In 1996, Dickinson et al.9 surveyed all patients diagnosed with muscle-invasive bladder cancer between 1989 and 1993 in the south-west of England. The waiting time from GP referral to diagnostic cystoscopy was, on average, 59 days in 1989 and decreased to 52 days in 1993. This was deemed unsatisfactory, particularly for those with muscle-invasive bladder cancer.
Since the introduction of the NHS Cancer Plan,4 the impact on waiting times and outcomes has been questionable.6 Specifically with regards to bladder cancer, where the 2-week wait rule relies on the detection of haematuria in order to identify patients with a suspected tumour. Previous studies have reported that the incidence of bladder cancer in patients with microscopic haematuria is less than 5% and these patients may, therefore, be subjected to over-investigation.5 There is no discrepancy between investigating patients with microscopic or macroscopic haematuria; the use of a generic proforma has resulted in a change in focus with macroscopic haematuria patients being investigated through the same pathway. This has had an impact upon the number of urgent referrals.
This study has shown that, following the introduction of the 2-week wait rule in 2001, the time taken from referral to first consultation and the overall time from referral to treatment have reduced by 47.6% (P < 0.001)) and 24% (P < 0.001), respectively. The limitations of this study may have overestimated this figure as we did not take into account a delay due to the patient being unable to attend the first given appointment. In this respect, the 2-week rule has achieved its main aim; however, in our experience, only 42% of those subsequently diagnosed with bladder cancer were referred as urgent.
There remains some debate regarding the overall significance of this reduction to the prognosis of each patient. Wallace et al.8 concluded that a delay between the onset of symptoms and the patient presenting to their GP was linked to a poorer prognosis. However, other studies have questioned whether a delay of 3 months for a cystectomy following a diagnosis of bladder cancer is likely to have an impact on the overall survival rates.
Our results demonstrate that low-grade, non-muscle invasive tumours were seen significantly quicker than high-grade or invasive tumours (P < 0.001) following the introduction of the 2-week wait rule (Fig. 4). Again, this reflects the non-specific diagnostic criteria utilised by the primary care physicians which has undermined clinical judgement as physicians adhere to guidelines.
The 2-week wait rule in urology has had an impact on work-load with a larger number of patients being referred with microscopic haematuria who are unlikely to have significant pathology.10 Recent studies have shown this figure may be as high as 10:1.11 We found that no patients referred with microscopic haematuria were subsequently diagnosed with invasive bladder cancer, which questions the need for patients with microscopic haematuria to be referred as urgent. The urgent referral of patients with microscopic haematuria leads to unnecessary distress for patients waiting for investigations when, in actual fact, they are more likely to have a benign cause accounting for their haematuria. More sensitive tests are required as the severity of haematuria is not proportional to disease severity nor allow early diagnosis.
The impact on the work-load in secondary care is inevitable and some would argue that this is unsustainable with current overspending and difficulties in meeting cancer targets. This has been addressed to some degree by the development and wide-spread use of one-stop haematuria clinics.
The findings from this study reflect those conducted in breast cancer. Potter et al.7 recently conducted a prospective study for breast cancer patients and found that the volume of referrals via the 2-week wait proforma increased over a 6-year period but the percentage of patients diagnosed with breast cancer reduced from 12.8% to 7.7%. The suggestion that a two-tier system has been created resulting in a delayed diagnosis for patients referred to the routine clinic. Taking into consideration the time, effort and money involved in the scheme, it is obvious that changes need to be made and other areas of the patient pathway need to be targeted. Fentiman12 suggests that the system purely picks up more people with advanced disease rather than targeting the earlier stages of cancer development such as patient education, high-risk groups and primary prevention.
Conclusions
The introduction of the 2-week wait rule has reduced the time for the overall pathway as well as the time taken to be seen by a specialist. The awareness of haematuria as a criterion for urgent referral has improved the referral pattern although this has led to the over investigation of microscopic haematuria.
References
- 1.Office of National Statistics, editor. Cancer Statistics registrations: registrations of cancer diagnosed in 2004, England, Series MB1 no 35. London: Office of National Statistics; 2007. [Google Scholar]
- 2.May M, Helke C, Nitzke T, Vogler H, Hoschke B. Survival rates after radical cystectomy according to tumor stage of bladder carcinoma at first presentation. Urol Int. 2004;72:103–11. doi: 10.1159/000075962. [DOI] [PubMed] [Google Scholar]
- 3.Rosario DJ, Becker M, Anderson JB. The changing pattern of mortality and morbidi ty from radical cystectomy. BJU Int. 2000;85:427–30. doi: 10.1046/j.1464-410x.2000.00454.x. [DOI] [PubMed] [Google Scholar]
- 4.Department of Health, editor. The NHS Cancer Plan. London: Stationary Office; 2000. [Google Scholar]
- 5.Boman H, Hedelin H, Holmang S. The results of routine evaluation of adult patients with haematuria analysed according to referral form information with 2-year follow-up. Scand J Urol Nephrol. 2001;35:497–501. doi: 10.1080/003655901753367613. [DOI] [PubMed] [Google Scholar]
- 6.Hanna SJ, Muneer A, Khalil KH. The 2-week wait for suspected cancer: time for a rethink? Int J Clin Pract. 2005;59:1334–9. doi: 10.1111/j.1368-5031.2005.00687.x. [DOI] [PubMed] [Google Scholar]
- 7.Potter S, Govindarajulu S, Shere M, Braddon F, Curran G, et al. Referral patterns, cancer diagnoses, and waiting times after introduction of two week wait rule for breast cancer: prospective cohort study. BMJ. 2007;335:288. doi: 10.1136/bmj.39258.688553.55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wallace DM, Bryan RT, Dunn JA, Begum G, Bathers S, West Midlands Urological Research Group Delay and survival in bladder cancer. BJU Int. 2002;89:868–78. doi: 10.1046/j.1464-410x.2002.02776.x. [DOI] [PubMed] [Google Scholar]
- 9.Dickinson AJ, Howe K, Bedford C, Sanders T, Prentice A, Sibley GN. A retrospective study of the investigation and management of muscle-invasive bladder cancer in the South West Region. Br J Urol. 1996;77:70–5. doi: 10.1046/j.1464-410x.1996.82611.x. [DOI] [PubMed] [Google Scholar]
- 10.Allen D, Popert R, O'Brien T. The two-week-wait cancer initiative in urology: useful modernization? J R Soc Med. 2004;97:279–81. doi: 10.1258/jrsm.97.6.279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Coxon JP, Harris HJ, Watkin NA. A prospective audit of the implementation of the 2-week rule for assessment of suspected urological cancers. Ann R Coll Surg Engl. 2003;85:347–50. doi: 10.1308/003588403769162486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Fentiman IS. Two week wait for suspected cancer: milestone or millstone? Int J Clin Pract. 2005;59:1251–2. doi: 10.1111/j.1368-5031.2005.00728d.x. [DOI] [PubMed] [Google Scholar]


