Abstract
INTRODUCTION
Recent studies have shown that closure of loop ileostomy can be performed in the day-case setting, reducing the length and cost of hospitalisation. By analysing our patients who have undergone reversal, we aimed to determine the length of hospital stay and potential factors behind stays beyond 24 h.
PATIENTS AND METHODS
A database of patients undergoing closure of loop ileostomy at one colorectal unit was examined. The times taken to discharge, morbidity and re-admission rates were recorded.
RESULTS
Eighty patients underwent reversal of ileostomy between January 2001 and January 2006. Median age was 63 years (range, 22–81 years). The median length of stay was 4 days (range, 2–32 days). The median length of stay in patients without complications was 4 days. Many appeared able to be discharged earlier. Seventy-two patients (90%) were able to tolerate a solid diet within 48 h and 54 (67.5%) had bowel function within 3 days. Six patients went home before bowel function; none of these were re-admitted. Twenty patients (25%) developed complications, which included wound infection (8%), small bowel obstruction/ileus (6%), enterocutaneous fistula (1%), anastomotic leak (1%), and late abdominal wall abscess (1%). Of the patients, 16% stayed longer than 5 days despite having no postoperative complications.
CONCLUSIONS
The majority of patients undergoing loop ileostomy reversal at our institution can be discharged earlier than they are at present. Support in the community and the implementation of modified UK day-case surgery protocols are suggested to help shorten patients' length of stay.
Keywords: Loop ileostomy reversal, Day-case surgery, Length of stay
Defunctioning loop ileostomy is an established method to divert bowel contents away from a distal anastomosis thereby attenuating the sequelae of anastomotic leakage and preventing fistula formation or use of inflamed bowel. Subsequent reversal of the ileostomy restores bowel continuity and improves the patient's overall quality of life. It has been suggested that reversal of loop ileostomy can be performed as an ambulatory procedure with early discharge protocols in order to facilitate the early discharge of patients.1,2 This not only benefits the patient, but is also a cost-effective use of healthcare resources.
We perceived that the duration of stay of patients undergoing this procedure in our facility was significantly longer than reported in the aforementioned studies. This delay possibly relates to the potential for complications or the tradition of patients remaining in hospital under observation until bowel function returns. This can take several days.
In order to investigate this hypothesis of prolonged hospital stay and the potential reasons behind this delay, we analysed the time taken to discharge for all patients undergoing reversal of a loop ileostomy. Postoperative complications and the time taken for the patient to open their bowels were the secondary end-points.
Patients and Methods
A database of all patients undergoing loop ileostomy reversal was examined and their case notes reviewed. The following data were analysed: ileostomy indication, type of anaesthetic used, grade of surgeon, time to oral fluids and feeding, time to bowel opening, length of hospital stay, and complications.
Criteria for exclusion from the study were those patients who underwent reversal as part of a multiple procedure or with concurrent laparotomy, those with spinal injuries and those with renal failure undergoing haemodialysis. The potential for prolonged stay and complications in these groups was perceived to be higher and the patients likely to not be reflective of the study group.
All patients had a standard bowel closure technique after having continuity of bowel distal to the ileostomy confirmed radiologically or clinically. Prophylactic, broad-spectrum antibiotics were administered at the induction of anaesthesia. The enteric mucosal-cutaneous junction was taken down and the adhesions between the small bowel and the anterior abdominal wall were freed with sharp dissection. Continuity was then restored by using a linear stapler (functional end-to-end technique) or interrupted absorbable monofilament suture. After return of the bowel into the abdominal cavity, the abdominal wall defect, the subcutaneous tissue and skin were closed. Nasogastric tubes were not routinely passed.
Results
Study cohort
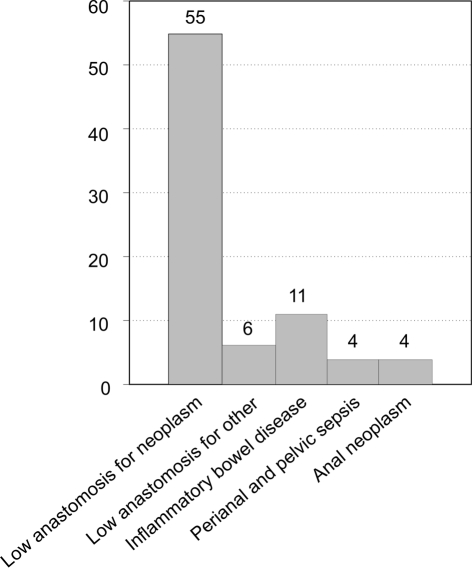
A total of 101 patients underwent reversal of loop ileostomy between January 2001 and January 2006 at our institution. Sixteen patients had undergone concurrent laparotomy, three were spinal or renal patients and the case notes for two patients were unavailable for review. Eighty patients were suitable for inclusion (45 males; median age, 63 years; range, 22–81 years). The indications for loop ileostomy formation are summarized in Figure 1. The procedure was performed under general anaesthetic in 76 patients (95%) and under spinal anaesthetic in four patients (5%). A consultant performed the operation in 66 patients (82.5%) and a specialist registrar in 14 patients (17.5%).
Figure 1.
Indications for defunctioning loop ileostomy.
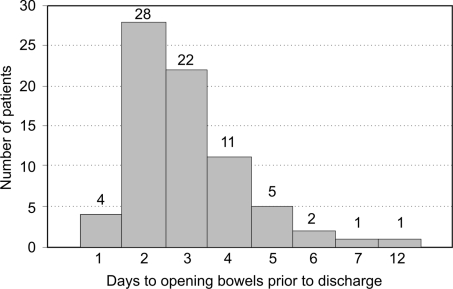
Time to discharge, oral intake and bowel opening
The median hospital stay was 4 days (range, 2–32 days). Seventy-nine patients (99%) tolerated oral fluids less than 24 h after their operation. Seventy-two patients (90%) commenced an oral diet within 48 h of their procedure with 48% of these within the first 24 h. The median time to bowel opening was 3 days (range, 0–12 days) and six patients had not opened their bowels by the date of their discharge; none of these six patients were re-admitted (Fig. 2).
Figure 2.
Time taken to open bowels after oop ileostomy reversal.
The median length of stay for patients without complications was 4 days. Twelve patients (16%) remained in hospital for more than 5 days despite having no complications and three of 11 patients who were admitted for more than 7 days had no complications.
Complications
The overall complication rate was 25%. These complications are shown in Table 1. The most common complication was wound infection (6 patients), one case of which required surgical debridement. This patient was also the only one to complain of severe pain postoperatively. Two patients were re-admitted (2.5%); one patient presented with the symptoms of small bowel obstruction 7 days after discharge and 14 days after their procedure; this was managed conservatively. Another patient suffered fresh rectal bleeding 1 week postoperatively (4 days after discharge). No cause for the bleeding was found on flexible sigmoi-doscopy and the bleeding settled with conservative treatment. One patient with ulcerative colitis presented 4 months later with an abdominal wall abscess at the site of closure. There was a 50% complication rate in patients with inflammatory bowel disease compared to a 21% complication rate in the rest of the cohort. All complications except re-admission and the abdominal wall abscess occurred within the admission period and were associated with a longer hospital stay.
Table 1.
Complications resulting from reversal of loop ileostomy
| Complication | Number of patients (%) | Range (mean) of length of stay (days) |
|---|---|---|
| Wound infection | 6(8) | 6–27 (10.8) |
| Rectal bleeding | 3(4) | N/A |
| Urinary retention | 3(4) | 3–11 (5.6) |
| Small bowel obstructiona | 2(3) | 7–10 (8.5) |
| Paralytic ileus | 2(3) | 7–11 (9) |
| Urinary tract infection | 2(3) | 5–6 (5.5) |
| Anastomotic leakb | 1 (1) | 15 |
| Enterocutaneous fistulac | 1 (1) | 32 |
| Lower respiratory tract infection | 1 (1) | 4 |
| Abdominal wall abscessd | 1 (1) | N/A |
One patient re-admitted 7 days' postoperatively. Both patients managed conservatively.
Possible leak 5 days' postoperatively. Managed conservatively.
Occurred fifth day postoperatively. Managed successfully with total parenteral nutrition and octreotide.
Occurred 4 months' postoperatively.
N/A, not applicable.
Discussion
Reversal of loop ileostomy has been shown to be possible as an ambulatory procedure and can also be performed under local anaesthetic. Our data confirm that there are wide variations in patients' lengths of stay that were perhaps not always justifiable. We propose that current practice can, therefore, be modified to enable early patient discharge in suitable patients without compromising their safety.
Kalady et al.1 showed that discharge within 23 h is possible after general and/or regional anaesthesia in a cohort of 28 carefully selected patients. Day-case selection criteria were similar to those used in the UK3 and patients were discharged with a strict postoperative care regimen. There were three re-admission episodes in this group (10.7%). Haagmans and colleagues4 performed 15 closures under local anaesthetic with a median length of stay of 2 days. One patient suffered subsequent wound infection and another small bowel obstruction, which settled conservatively. Ihedioha et al.5 used a ‘minimal general anaesthesia’ technique to perform 70 ileostomy closures with a median length of stay of 2 days. There was a high re-admission rate (10%), however, similar to the cohort of Kalady et al.
These studies show that the early discharge of patients after ileostomy reversal is feasible. In our series, patients without complications stayed in hospital for a median of 4 days. This compares favourably with other studies performed in the UK,12–14 although studies in the US show variable lengths of stay.1,15,16 In our cohort, 16% of patients had a hospital stay of 5 days or more despite having no complications suggesting that facilitating earlier discharge may reduce the length of stay further.
The concepts of enhanced recovery and early discharge include the avoidance of nasogastric tubes4 and early feeding. None of our cohort had the routine placement of a nasogastric tube and almost all had early introduction of oral intake. There is also no apparent reason why patients must remain in hospital until their bowels open. The six patients in our cohort who were discharged prior to bowel opening suffered no complications and had a mean stay of 3.5 days, which compared favourably with the rest of the group. Interestingly, one of these patients effected their own discharge on their fourth day of admission. There is a possible mindset in that surgeons want a reasonable period of time to elapse for any potentially serious complication (such as an anastomotic leak) to make itself manifest before letting the patient home. Bowel function may add re-assurance that complications are less likely.
Patients subjected to an early discharge programme should be carefully selected in accordance with modified day-case surgery guidelines (Table 2). They should also be counselled and given written instructions on wound care, analgesia requirements and on when to seek attention for impending ileus, obstruction or sepsis.1,2 This may require pre-operative input by the surgeon or specialist nurse and ensuring the availability of postoperative support and access to emergency services after discharge.
Table 2.
Recommendations for patient suitability for early discharge after closure of loop ileostomy
| Pre-operative assessment |
| Social suitability: responsible adult present for 24 h, access to telephone, access to general practitioner |
| American Society of Anaesthesiologists physical status grade 1–2 |
| Body mass index < 35 kg/m2 |
| No severe systemic organ system dysfunction |
| No type 1 diabetes or type 2 on insulin |
| Not on anticoagulation therapy |
| No anaesthesia contraindications |
| Intra-operative factors |
| No excessive blood loss |
| No conversion to laparotomy or multiple procedures |
| Fitness for discharge |
| Stable vital observations for at least an hour |
| Absence of active wound bleeding |
| No nasogastric tube |
| Pain controlled on oral analgesia |
| Passing urine |
| Able to drink fluids |
| Written and verbal instructions on wound care, analgesia and signs of sepsis and bowel obstruction |
| Emergency contact number for accident and emergency department and stoma clinical nurse specialists |
| Regular district nurse visits for wound management |
Modified from the NHS Modernisation Agency and the British Association of Day Surgery guidelines.3
Although we had a complication rate similar to some small studies,7 it was more than double that in the study of Wong and colleagues8 of 1504 patients undergoing closure of loop ileostomy after restorative proctocolectomy (11.4%). Even excluding patients with inflammatory bowel disease (50% of whom had complications in our cohort), the complication rate was 21%. A possible reason for this discrepancy is the recording of complications. Six of our patients had complications generic to any abdominal surgery requiring hospital admission (urinary retention, lower respiratory tract infection and urinary tract infection) and we included these as complications of the surgery.
Wound infection was the most common complication, occurring in 8% of patients. All patients had primary closure of their wounds, as is the practice in our unit. Wound closure technique after closure of ileostomy is variable amongst surgeons. It has been suggested that leaving ileostomy wounds to repair by secondary intention reduces the infection rate,4 but this has implications on the postoperative management of any patients who are considered for early discharge. The cohort of Haagmans et al.4 had a wound infection rate of 1 in 15 (6.7%) and this single patient had had primary closure of their stoma wound. Kalady et al.1 used a loose purse-string closure and packing to manage the wound with removal of the ribbon gauze pack and instructions on wound care prior to discharge and had an infection rate of 3.7%. Other published studies suggest no consensus, however, on whether secondary healing does decrease wound infection rates.9,10
Over 70% of the complications that occurred were minor and could be managed adequately in the community. Most major complications (leak, fistula, bowel obstruction) occurred within 5 days of surgery. The question remains as to whether the patient would have come to more harm if these complications occurred outside the hospital. Provided adequate community support is available with an easy access to specialist advice, this seems unlikely.
Study limitations
This study is retrospective and, as such, its findings are limited. Furthermore, it is not linked to a pre-determined discharge protocol. It is, however, a reliable reflection of current surgical practice and its findings may form the basis of a dedicated pathway of care based on the principles of enhanced recovery. Prospective, randomised, controlled trials comparing early discharge protocols with traditional care are required to validate our preliminary findings.
Conclusions
This study confirms that postoperative stay after closure of loop ileostomy is extremely variable with many patients staying longer in hospital than appears clinically justified. Most complications would not have been avoided if the patient had been discharged earlier. Our data would suggest there is no reason to avoid earlier discharge after ileostomy reversal provided surgeons are prepared to modify current practice, perhaps accept an increased re-admission rate and provided there is adequate community support.
Acknowledgments
The results have been presented, in part, in poster form at the British Association of Day Surgery Annual Conference in Scarborough, June 2008 and the Association of Coloproctology of Great Britain and Ireland Annual Conference, Glasgow, July 2007.
References
- 1.Kalady MF, Fields RC, Klein S, Nielsen KC, Mantyh CR, Ludwig KA. Loop ileostomy closure at an ambulatory surgery facility: a safe and cost-effective alternative to routine hospitalization. Dis Colon Rectum. 2003;46:486–90. doi: 10.1007/s10350-004-6587-0. [DOI] [PubMed] [Google Scholar]
- 2.Moran MR. Same-day surgery ileostomy closure? Am J Manag Care. 1997;3:1003–6. [PubMed] [Google Scholar]
- 3.British Association of Day Surgery. Guidelines about the discharge process and the assessment of fitness for discharge. < http://www.daysurgeryuk.org/bads/joomla/> [Accessed 2008]
- 4.Haagmans MJ, Brinkert W, Bleichrodt RP, van Goor H, Bremers AJ. Short-term outcome of loop ileostomy closure under local anesthesia: results of a feasibility study. Dis Colon Rectum. 2004;47:1930–3. doi: 10.1007/s10350-004-0686-9. [DOI] [PubMed] [Google Scholar]
- 5.Ihedioha SM, Kalmar K, Donnelly L, Macdonald A. Early discharge after closure of loop ileostomy – is it safe and achievable? Colorectal Dis. 2004;6(Suppl 1):37–85. [Google Scholar]
- 6.Wind J, Polle SW, Fung Kon Jin PH, Dejong CH, von Meyenfeldt MF, et al. Systematic review of enhanced recovery programmes in colonic surgery. Br J Surg. 2006;93:800–9. doi: 10.1002/bjs.5384. [DOI] [PubMed] [Google Scholar]
- 7.Balfour LS, Boyle K, Finan P, Burke D, Sagar P. The outcome of loop ileostomy closure: a prospective study. Br J Surg. 2002;89(Suppl 1):11. [Google Scholar]
- 8.Wong KS, Remzi FH, Gorgun E, Arrigain S, Church JM, et al. Loop ileostomy closure after restorative proctocolectomy: outcome in 1,504 patients. Dis Colon Rectum. 2005;48:243–50. doi: 10.1007/s10350-004-0771-0. [DOI] [PubMed] [Google Scholar]
- 9.Lahat G, Tulchinsky H, Goldman G, Klauzner JM, Rabau M. Wound infection after ileostomy closure: a prospective randomized study comparing primary vs. delayed primary closure techniques. Tech Coloproctol. 2005;9:206–8. doi: 10.1007/s10151-005-0228-z. [DOI] [PubMed] [Google Scholar]
- 10.Vermulst N, Vermeulen J, Hazebroek EJ, Coene PP, van der Harst E. Primary closure of the skin after stoma closure. Management of wound infections is easy without (long-term) complications. Dig Surg. 2006;23:255–8. doi: 10.1159/000095399. [DOI] [PubMed] [Google Scholar]
- 11.Gan TJ. Selective serotonin 5-HT3 receptor antagonists for postoperative nausea and vomiting: are they all the same? CNS Drugs. 2005;19:225–38. doi: 10.2165/00023210-200519030-00004. [DOI] [PubMed] [Google Scholar]
- 12.Williams LA, Sagar PM, Finan PJ, Burke D. The outcome of loop ileostomy closure: a prospective study. Colorectal Dis. 2008;10:460–4. doi: 10.1111/j.1463-1318.2007.01385.x. [DOI] [PubMed] [Google Scholar]
- 13.Amin SN, Memon MA, Armitage NC, Scholefield JH. Defunctioning loop ileosto my and stapled side-to-side closure has low morbidity. Ann R Coll Surg Engl. 2001;83:246–9. [PMC free article] [PubMed] [Google Scholar]
- 14.Hasegawa H, Radley S, Morton DG, Keighley MR. Stapled versus sutured closure of loop ileostomy: a randomized controlled trial. Ann Surg. 2000;231:202–4. doi: 10.1097/00000658-200002000-00008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Wexner SD, Taranow DA, Johansen OB, Itzkowitz F, Daniel N, Nogueras JJ, et al. Loop ileostomy is a safe option for fecal diversion. Dis Colon Rectum. 1993;36:349–54. doi: 10.1007/BF02053937. [DOI] [PubMed] [Google Scholar]
- 16.Hull TL, Kobe I, Fazio VW. Comparison of handsewn with stapled loop ileostomy closures. Dis Colon Rectum. 1996;39:1086–9. doi: 10.1007/BF02081405. [DOI] [PubMed] [Google Scholar]