Abstract
Much research has focused on behavioral activation and its effect on depression, but less is known about the effects of leisure activities on the two distinct affective domains of depression: positive affect (PA) and negative affect (NA). Furthermore, individual factors (i.e., stress level) may moderate the impact of behavioral activation on affect. The present study utilized a daily diary approach to examine the moderating effect of stress on the relationship between leisure satisfaction and both PA and NA. Twenty-five dementia caregivers completed activity and affect measures four times daily for 14 days. Results were analyzed using multilevel modeling, an approach that considers intra-individual differences in activity and affect over time. Results supported the hypothesis that caregivers with higher burden display a stronger association between leisure satisfaction and affect than caregivers with lower burden. Specifically, caregivers with higher burden had a stronger positive relationship between leisure satisfaction and PA and a stronger negative relationship between leisure satisfaction and NA. These findings suggest that screening caregivers for level of burden may help identify those most likely to benefit from behavioral interventions.
Keywords: Stress, mood, behavior therapy, behavioral activation, depression
INTRODUCTION
Providing care to a loved one with dementia is a stressor that has been shown to increase caregivers’ risk for psychological and physical morbidity (Schulz, O'Brien, Bookwala, & Fleissner, 1995), including depression. Previous research has found that compared to noncaregivers, caregivers of a relative with dementia are more likely to experience depressive symptoms after controlling for age, gender, income, and self-rated health (Adams, 2008). Some estimates suggest that caregivers experience almost twice as many depressive symptoms as noncaregivers (Baumgarten et al., 1992). Much research on caregiver morbidity has focused on depressive symptoms, but other research has revealed that depression consists of two affective domains referred to as positive affect (PA) and negative affect (NA) (Clark & Watson, 1991; Cook, Orvaschel, Simco, Hersen, & Joiner, 2004). PA includes level of excitement, liking, or enthusiasm, whereas NA consists of distress, irritability, anxiety and fear (Watson, Wiese, Vaidya, & Tellegen, 1999). The “Tripartite” model of depression conceptualizes depression as a combination of high NA with low PA. Several studies support this conceptualization of depression (Brown, Chorpita, & Barlow, 1998; Clark & Watson, 1991; Cook et al., 2004; Watson et al., 1995).
Behavioral activation is a treatment modality for depression with well established efficacy (Mazzucchelli, Kane, & Rees, 2009; Sturmey, 2009). In brief, behavioral theories of depression posit that depression stems from a disruption in normal behavior patterns resulting in a low rate of response-contingent positive reinforcement (Lewinsohn, Youngren, & Grosscup, 1979). This lack of positive reinforcement often leads to a heightened state of self-awareness which can create feelings of self-criticism and result in behavioral withdrawal (Lewinsohn, Hoberman, Teri, & Hautzinger, 1985). Research has demonstrated that depressed individuals, including dementia caregivers, take part in fewer pleasant activities and that their mood covaries with the frequency of their participation in pleasant and aversive events (Mausbach, Patterson, & Grant, 2008; Williamson, Shaffer, & Schulz, 1998). In response, behavior therapies aimed at increasing participation in leisure activities have been shown to be effective in reducing depression in caregivers (Coon, Thompson, Steffen, Sorocco, & Gallagher-Thompson, 2003; Gallagher-Thompson & Coon, 2007) and a variety of other populations (Mazzucchelli et al., 2009; Meeks, Young, & Looney, 2007; Miranda & Muñoz, 1994).
Although previous research has indicated that increased engagement in leisure activities is correlated with reduced depressive symptoms, less is known about the relationship between engagement in leisure activities and the two unique domains of depression, PA and NA. Recently, Mausbach, Coon, Patterson and Grant (2008) examined the correlation between leisure engagement and both PA and NA over a two-week period, during which time participants completed diary questionnaires assessing PA, NA, and leisure engagement four times each day. Results indicated that greater engagement in leisure activities may not have similar “effects” on PA and NA. Rather, greater engagement in leisure activities was significantly correlated with PA (r = .43), but the correlation between leisure activities and NA appeared dampened (r = .12).
The strength of the relationship between engagement in leisure activities and PA and NA may also differ across individuals. That is, for some individuals, engagement in pleasurable activities may have more “powerful” effects on PA and NA. One such group may be those who experience high levels of life stress, who may find themselves overwhelmed to a point of restricting their engagement in pleasant activities (Mausbach et al., 2008). In turn, they are at greater risk for depression compared to their non-stressed peers (Baumgarten et al., 1992). However, if highly stressed individuals manage to maintain engagement in pleasurable activities, they may experience greater benefit from these activities than would be expected in individuals reporting low stress. Engagement in leisure activities has been conceptualized as a way to cope with stressors by providing opportunities for distraction, self-restoration and personal transformation (Kleiber, Hutchinson, & Williams, 2002). Individuals under more stress may have a greater need for distraction or restoration and may therefore experience greater increase in PA and decrease in NA from leisure activities. Indeed, previous research supports the notion that individuals with greater psychological “need” may benefit more from relevant interventions. Rabinowitz and colleagues (2006) found that female caregivers lacking in self-efficacy for obtaining respite showed a greater decrease in depressive symptoms in response to a cognitive behavioral intervention that included leisure engagement strategies, compared to a control condition. Similarly, caregivers under high stress may have a greater need for, or place greater value on, leisure activities and may therefore show greater associated improvement in mood compared with less stressed caregivers.
The current study investigated the relationship between participation in leisure activities and affect in a sample of dementia family caregivers. Specifically, the relationship between caregivers’ level of satisfaction obtained from engagement in leisure activities and both PA and NA was examined. We also explored the hypothesis that burden moderates this relationship such that caregivers with greater burden show a stronger correlation between leisure satisfaction and affect compared to caregivers reporting lower burden.
One unique aspect of this study is its emphasis on within-person fluctuation in PA, NA, and leisure satisfaction. Much of the current literature relies on cross-sectional designs that emphasize between-person relationships, or longitudinal designs that evaluate change over long periods of time, which precludes the examination of activity and affective fluctuations within individuals temporally (Barnett & Gotlib, 1988). Many of these designs assume that the variables in question are traits that remain relatively stable at different time points and also rely heavily on participants’ ability to accurately remember their moods and activities, despite the possibility of recall bias (Shiffman, Stone, & Hufford, 2008). In contrast to these designs, the present study used a daily diary approach to evaluate the moderating effect of caregiver burden on the within-person relationship between activity and affect over time. This “experience-sampling approach” is advantageous because it enables a participant to serve as his or her own baseline and allows researchers to capture subtle shifts in each participant’s mood depending on their particular participation in activities or lack thereof (Wenze, Gunthert, & Forand, 2007). The aim of the present study was to determine if the within-person relationship between activity and affect was stronger in caregivers with high burden compared to those with low burden.
METHODS
Participants
A total of 25 participants were enrolled. All participants were informed that they were participating in a study to examine fluctuations in caregivers’ moods and activities to help inform treatments for caregivers. Participants were required to be providing informal care to a family member with a physician diagnosis of Alzheimer’s disease (AD). Additionally, participants must have been living with the care recipient, providing at least 8 hours of direct care per week, and report that the care recipient required help with at least 2 instrumental activities of daily living (IADLs, e.g., shopping, using the telephone) or 1 activity of daily living (ADLs, e.g., dressing, toileting). Participants were also required to be at least 21 years of age and report at least 3 symptoms of depression as per DSM-IV criteria (American Psychiatric Association, 2000). Three symptoms were required to ensure participants were experiencing at least mild symptoms of depression and thus some level of mood disturbance. Participants were excluded if they did not speak English, indicated they had a serious medical condition (e.g., cancer), or had plans to place their care recipient into long-term care (e.g., nursing home) over the next two months. Participants were recruited from community support groups, local senior centers and medical clinics, and senior service professionals.
Measures
After providing written, informed consent, all participants completed an in-home psychosocial assessment to gather baseline information regarding demographic characteristics of the caregiver and care recipient (e.g., age, gender), functional deficits of the care recipient (e.g., ADLs, IADLs), and measures of caregiver distress. The following measures were relevant to the current study:
Positive and Negative Affect
The Positive and Negative Affect Schedule (PANAS)(Watson, Clark, & Tellegen, 1988) was used to assess positive (PA) and negative affect (NA). The PANAS consists of 20 mood adjectives; ten assessing PA and ten assessing NA. Examples of PA are “interested,” “excited,” and “enthusiastic.” Sample NA items are “distressed,” “scared,” and “irritable.” For each adjective, participants rated the degree to which they felt that way during the past 4 hours. Response options ranged from: 1 = very slightly or not at all to 5 = extremely. The PANAS has excellent psychometric properties, with internal consistency of >0.86 for PA and >0.84 for NA (Watson et al., 1988).
Leisure Satisfaction
To assess the level of satisfaction obtained from engagement in leisure activities, all participants completed a modified version of the Pleasant Events Schedule-AD (Logsdon & Teri, 1997). The PES-AD lists 20 common leisure activities (e.g., listening to music, having meals with friends or family, exercising). At each of the 56 assessment points, participants rated the frequency with which they engaged in each activity over the past 4 hours. Response options were: 0 = not at all, 1 = 1 time, and 2 = 2 or more times. For each activity participants performed, they indicated how much they enjoyed the activity using the following options: 0 = not at all, 1 = somewhat, and 2 = a great deal. By multiplying the frequency score by the enjoyment score, we computed a total “leisure satisfaction” score for each of the 20 activities (range for each activity = 0–4). The sum of these cross products was used to create an overall leisure satisfaction score (range = 0–80). Therefore, leisure satisfaction was defined in this study as more frequent engagement in satisfying or enjoyable leisure activities. Cronbach’s alpha for the leisure satisfaction scale was 0.83.
Initial Burden
Participants completed the Zarit Burden Interview (ZBI) at baseline (Zarit, Orr, & Zarit, 1985; Zarit, Reever, & Bach-Peterson, 1980). This scale contains 22 items assessing subjective burden associated with caring for a loved one. Sample items include, “Do you feel that your social life has suffered because you are caring for your relative?” and “Do you feel strained when you are around your relative?” Response options ranged from 0 = Never to 4 = Nearly always. A total burden score was computed as the sum of the 22 items. Chronbach’s alpha for the ZBI is excellent (α = 0.92)(Knight, Fox, & Chou, 2000).
Care Recipient Functional Deficits
Caregivers indicated whether or not their care recipients required assistance with 7 ADLs (Katz, Ford, Moscowitz, Jackson, & Jaffee, 1963) and 8 IADLs (Lawton & Brody, 1969). Care recipient functional deficits were taken as the sum of ADLs and IADLs requiring assistance. Cronbach’s alpha for this sample was 0.80.
Procedures
As described in our previous report (Mausbach, Coon, Patterson, & Grant, 2008), each participant was given a diary containing the PES-AD form and the PANAS. Participants were instructed to complete these measures at the following times each day for a period of 14 days: (a) early morning (i.e., before 10 a.m.), (b) noon, (c) late afternoon (i.e., around 4 p.m.), and (d) prior to bedtime. Full compliance with the protocol resulted in a total of 56 diary entries per participant. Forms were counterbalanced to eliminate potential order effects. All participants were paid $40 for participating in this study.
Data analysis
In our previous report (Mausbach et al., 2008), we demonstrated a significant concomitant correlation between obtained pleasure (equivalent to our “leisure satisfaction” variable) and both PA and NA. The current analysis examined the moderating effect of baseline burden on the relationship between leisure satisfaction and PA and NA. All analyses of interaction effects included their corresponding main effects. Because of evidence that affective experience changes over the lifespan (Carstensen, Fung, & Charles, 2003; Carstensen, Pasupathi, Mayr, & Nesselroade, 2000), we included age as a covariate in all analyses.
Given the nested structure of our data, we used multilevel modeling to test the relationships between variables of interest. At level 1, we estimated each participant’s distinctive relationship between leisure satisfaction and affect. Each participant’s 56 repeated observations were used to generate a unique regression equation modeling the relationship between leisure satisfaction and affect. For example, our level 1 regression equation for the concomitant relationship between leisure satisfaction and NA was
where NA refers to Negative Affect and OP refers to Obtained Pleasure (i.e., leisure satisfaction) scores. For both analyses, predictor variables in level 1 equations were group-mean centered. In the example equation above, each person’s mean leisure satisfaction score was subtracted from each of his/her 56 daily observations of leisure satisfaction. The intercept, π0i is therefore participant i’s level of NA at his/her average level of leisure satisfaction. NAij is participant i’s level of NA at assessment j. π1i, the slope, is the change in participant i’s NA for every one unit increase in leisure satisfaction. eij is the error term for person i. Each person therefore has unique regression parameters, representing their own relationship between leisure satisfaction and affect.
At level 2, we estimated how burden (a between-subjects variable) affects this within-subject relationship between leisure satisfaction and affect. The level 2 equations were:
where the level 1 intercepts and slopes were modeled as a function of an intercept component, a slope component indicating the effect of burden on the level 1 intercepts and slopes, and a random error component. Prior to analyses, ZBI scores were grand mean centered. Therefore, b10 is the relationship between leisure satisfaction and affect for the average person. b11 is the change in the within person slope for every point increase on the ZBI scale.
RESULTS
Sample Characteristics
Baseline characteristics of the sample are presented in Table 1. As shown, participants were older and primarily female. Caregivers provided an average of 4.0 years of care at the time of study entry.
Table 1.
Characteristics of the Sample
| Variable | |
|---|---|
| Caregiver Age, M (SD) | 63.2 (11.4) |
| Gender, n (%) | |
| Male | 1 (4) |
| Female | 24 (96) |
| Relationship, n (%) | |
| Spouse | 17 (68) |
| Non-spouse | 8 (32) |
| Ethnicity, n (%) | |
| Caucasian | 21 (84) |
| Latina/Hispanic | 4 (16) |
| Years Caregiving, M (SD) | 4.0 (2.6) |
| Income*, n (%) | |
| < $50,000 | 12 (50) |
| ≥ $50,000 | 12 (50) |
| Hours of Care/Week, M (SD) | 56.7 (51.4) |
| Initial Burden, M (SD) | 22.3 (6.1) |
| Care Recipient Age, M (SD) | 77.0 (8.2) |
| Activities of Daily Living, M (SD) | 2.9 (2.4) |
| Instrumental Activities of Daily Living, M (SD) | 7.0 (1.6) |
Note.
One participant refused to provide income data.
Diary Compliance
Participants were highly compliant in completing their diaries. On average, participants completed 49.8 PES-AD forms (88.9%) and 51.0 PANAS forms (91.1%). Initial burden was not significantly associated with the number of diary forms completed (r = −.22; p =.296).
Slope analyses: Effects of initial burden on leisure satisfaction to affect
Positive Affect
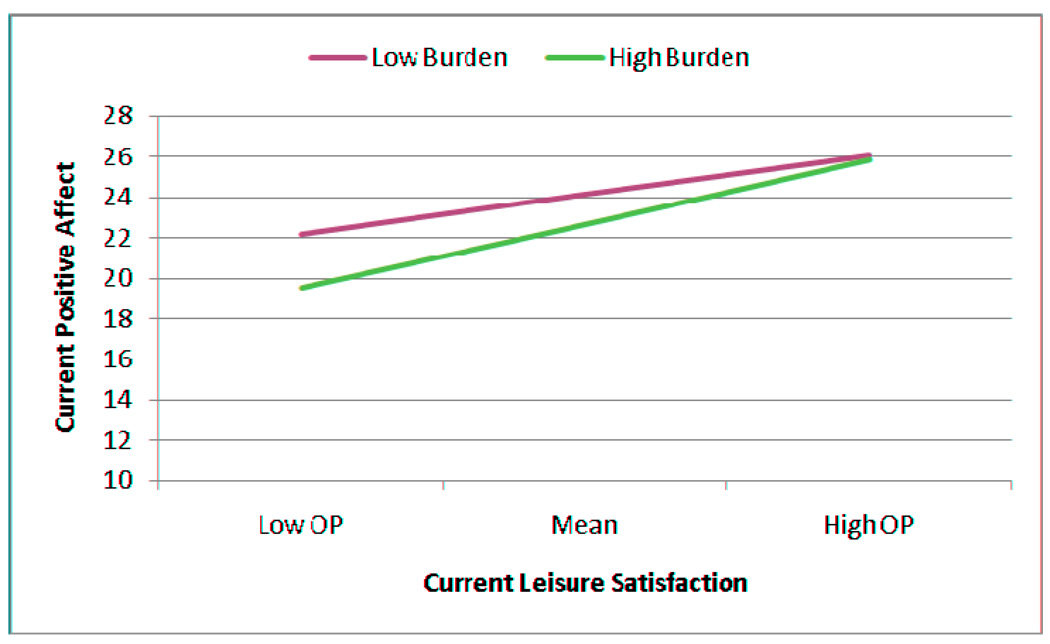
To investigate the effects of burden on the relationship between leisure satisfaction and affect, we conducted analyses in which leisure satisfaction was used to predict affect at level 1, and differences in these slopes were predicted as a function of burden at level 2. Results indicated a significant main effect for leisure satisfaction, in which greater leisure satisfaction was associated with increased PA (b = 0.420 ± 0.041; t = 10.30, df = 17.80, p < .001). However, burden moderated this relationship (b = 0.016 ± 0.007; t = 2.44, df = 16.62, p = .026). We examined this significant interaction effect by plotting the slopes for leisure satisfaction when initial burden was low (−1 SD) and when initial burden was high (+1 SD). Results of these post-hoc analyses indicated a stronger within-person association between leisure satisfaction and PA when burden was high (b = 0.521 ± 0.059; t = 8.86, df = 16.75, p < .001) than when burden was low (b = 0.320 ± 0.057; t = 5.60, df = 17.68, p < .001). A graphic depiction of these slopes appears in Figure 1. Finally, neither age (b = 0.193 ± 0.100; t = 1.93, df = 23.00, p = .066) nor burden (b = −0.117 ± 0.185; t = −0.63, df = 23.07, p = .534) was significantly related to PA.
Figure 1.
Moderating effect of initial burden on the relationship between leisure satisfaction and positive affect. Note: OP = Obtained Pleasure.
Negative Affect
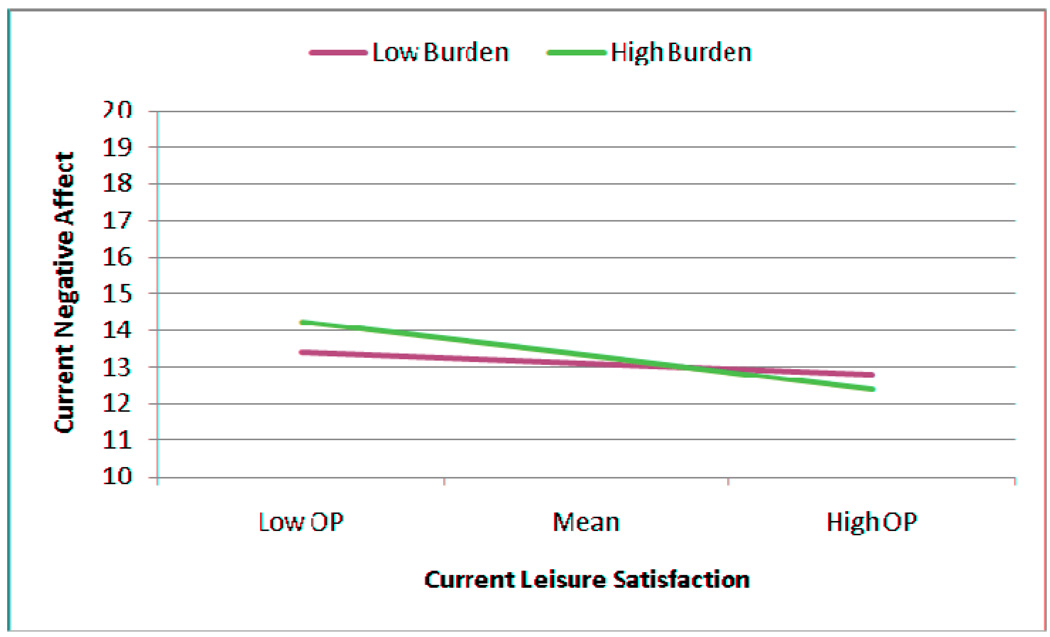
The average within-person relationship between leisure satisfaction and NA was also significant (b = −0.102 ± 0.025; t = −4.08, df = 32.95, p < .001), meaning that across the sample, greater leisure satisfaction was associated with lower levels of NA. However, this relationship was moderated by initial burden (b = −0.008 ± 0.004; t = −2.07, df = 30.38, p = .047). Post-hoc analyses indicated that when initial burden was low, leisure satisfaction was not significantly related to NA (b = −0.050 ± 0.035; t = −1.43, df = 33.95, p = .162). Conversely, when initial burden was high, leisure satisfaction was significantly related to NA (b = −0.154 ± 0.036; t = −4.31, df = 29.54, p < .001) (see Figure 2). In this analysis, age was significantly related to NA (b = −0.149 ± 0.058; t = 2.59, df = 23.79, p = .016), such that older participants reported lower NA.
Figure 2.
Moderating effect of initial burden on the relationship between leisure satisfaction and negative affect. Note: OP = Obtained Pleasure.
DISCUSSION
Whereas prior research has demonstrated significant correlations between engagement in leisure activities and reduced depressive symptoms (Jacobson et al., 1996; Lewinsohn, 1975), or between leisure activities and both PA and NA (Mausbach et al., 2008), the current study expands upon this research by examining the circumstances that moderate this relationship. Specifically, we hypothesized a stronger correlation between leisure satisfaction and affect in caregivers with greater burden compared to those with lower burden. Our results supported these hypotheses, indicating that when highly burdened caregivers experienced fluctuations in satisfaction from leisure activities, the corresponding “effect” on mood was stronger than for caregivers with low burden. Caregivers with higher burden showed a stronger increase in PA associated with increased leisure satisfaction than did caregivers with lower burden. Caregivers with higher burden also showed a decrease in NA associated with increased leisure satisfaction, whereas caregivers with lower burden showed no significant relationship between NA and leisure satisfaction.
These results have implications for caregiver interventions that incorporate behavioral activation components. Behavioral interventions seek to increase the frequency and intensity of patients’ involvement in activities that they find enjoyable, therefore, information regarding psychosocial variables that moderate the impact of leisure activities on mood may provide valuable information about which caregivers will respond best to these interventions. While we acknowledge that this was not an intervention study, our results imply that caregivers with higher burden are likely to experience a greater affective benefit as a result of increasing leisure satisfaction, as compared to caregivers with lower burden. One implication of these findings is that screening caregivers with depressive symptoms for burden may aid therapists in selecting appropriate interventions. Additionally, research has demonstrated that behavioral activation for depression is briefer than other interventions (Hopko, Lejuez, Ruggiero, & Eifert, 2003), thus, screening caregivers for burden to identify those who would benefit most may prove beneficial to the health care system by aiding in the efficient allocation of scarce resources.
As previously mentioned, a significant strength of the present study is its focus on within-person fluctuation in PA, NA, and leisure satisfaction, in contrast to much of the cross-sectional literature to date (Barnett & Gotlib, 1988). Additionally, many longitudinal designs assume that affect and leisure satisfaction are stable constructs and expose measurements of these constructs to recall bias (Shiffman et al., 2008). The present study decreased the likelihood of inaccurate data due to recall bias by obtaining multiple daily assessments. Additionally, the experience sampling approach allowed for examination of intra-individual fluctuations in these constructs over time, which is important given that caregiving stressors are often unpredictable and fluctuate throughout the day. However, it should be noted that although the experience-sampling approach is a type of longitudinal design that captures more immediate fluctuations in constructs of interest, there is no reason that similar analyses could not be conducted on longitudinal data where assessments come less frequently (e.g., once or twice per year). Perhaps the advantage of the current design is that we were able to capture more immediate fluctuations in the variables of interest, whereas in more typical longitudinal designs the assessments occur far less frequently and thus may be less likely to capture individual fluctuation. Conceivably, the ideal design may be to combine a daily diary approach with a more traditional longitudinal design, whereby each year subjects complete a two week diary so that analyses can elucidate day-to-day fluctuations repeatedly over time.
The current study is not without limitations. The small sample size means that the results require replication. Additionally, a majority of caregivers in the current sample were female and Caucasian, thus these results may require replication in ethnically diverse samples in order to establish generalizability. This analysis examined the role of burden in moderating the relationship between leisure satisfaction and PA and NA, however, demographic factors such as caregiver income may influence the impact of burden on leisure satisfaction. For example, even if caregivers are experiencing greater burden, those with higher income may have additional resources for engagement in pleasant events that are not available to lower income caregivers.
We did not collect information on potential confounding variables, including caregivers’ level of depressive symptoms and the presence other psychopathology or caregivers’ use of psychotropic medications or psychotherapy to cope with caregiving stresses. It is possible that use of antidepressant medications would affect both engagement in pleasurable activities and PA and NA. Caregivers’ participation in psychotherapy may influence all of our key variables (i.e., burden, affect, and activities), thus affecting our moderator analyses. We recommend that future research consider these factors.
Another limitation is potential noncompliance in completing the daily diary assessments. Overall, completion of assessments was high, with participants completing, on average, 88.9% of the leisure activity assessments and 91.1% of the affect assessments. Importantly, initial burden was not significantly associated with the number of assessments completed. However, given that participants completed written assessments, it is not possible to ensure that the assessments were completed at the specific times instructed; participants who appeared compliant may have engaged in “backfilling” by completing multiple assessments after the specified time, thereby reducing the accuracy of the data (Shiffman et al., 2008). In order to verify compliance with the assessment protocol, the study may require replication using electronic diaries that record the exact time of assessment completion.
In sum, we found that the relationship between leisure satisfaction and affect was strongest in caregivers experiencing greatest burden. These findings may help identify a subset of dementia caregivers (i.e., highly burdened caregivers) that may particularly benefit from engagement in leisure activities and may respond best to behavioral treatments for depression. Specifically, caregivers with higher levels of burden display a greater increase in PA and decrease in NA associated with increased leisure satisfaction than do caregivers with lower burden. Although these data originate from dementia caregivers, these findings may apply to other caregivers. Future research might examine similar relationships in other highly burdened populations such as parents of children with physical and psychological disabilities (e.g., autism, epilepsy) or spouses caring for a physically ill partner (e.g., partner with cancer or multiple sclerosis).
ACKNOWLEGEMENTS
Primary research support was provided via funding from the National Institute on Aging (NIA) through awards F32 AG23989 and R01 AG031090.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Adams KB. Specific effects of caring for a spouse with dementia: differences in depressive symptoms between caregiver and non-caregiver spouses. International Psychogeriatrics. 2008;20:508–520. doi: 10.1017/S1041610207006278. [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders (Text Revision, Trans. 4th ed.) Washington, DC: American Psychiatric Association; 2000. [Google Scholar]
- Barnett PA, Gotlib IH. Psychosocial functioning and depression: distinguishing among antecedents, concomitants, and consequences. Psychological Bulletin. 1988;104:97–126. doi: 10.1037/0033-2909.104.1.97. [DOI] [PubMed] [Google Scholar]
- Baumgarten M, Battista RN, Infante-Rivard C, Hanley JA, Becker R, Gauthier S. The psychological and physical health of family members caring for an elderly person with dementia. Journal of Clinical Epidemiology. 1992;45:61–70. doi: 10.1016/0895-4356(92)90189-t. [DOI] [PubMed] [Google Scholar]
- Brown TA, Chorpita BF, Barlow DH. Structural relationships among dimensions of the DSM-IV anxiety and mood disorders and dimensions of negative affect, positive affect, and autonomic arousal. Journal of Abnormal Psychology. 1998;107:179–192. doi: 10.1037//0021-843x.107.2.179. [DOI] [PubMed] [Google Scholar]
- Carstensen LL, Fung HH, Charles ST. Socioemotional selectivity theory and the regulation of emotion in the second half of life. Motivation and Emotion. 2003;27:103–123. [Google Scholar]
- Carstensen LL, Pasupathi M, Mayr U, Nesselroade JR. Emotional experience in everyday life across the adult life span. Journal of Personality and Social Psychology. 2000;79:644–655. [PubMed] [Google Scholar]
- Clark LA, Watson D. Tripartite model of anxiety and depression: Psychometric evidence and taxonomic implications. Journal of Abnormal Psychology. 1991;100:316–336. doi: 10.1037//0021-843x.100.3.316. [DOI] [PubMed] [Google Scholar]
- Cook JM, Orvaschel H, Simco E, Hersen M, Joiner T. A test of the tripartite model of depression and anxiety in older adult psychiatric outpatients. Psychology and Aging. 2004;19:444–451. doi: 10.1037/0882-7974.19.3.444. [DOI] [PubMed] [Google Scholar]
- Coon DW, Thompson L, Steffen A, Sorocco K, Gallagher-Thompson D. Anger and depression management: psycho-educational skill training interventions for women caregivers of a relative with dementia. The Gerontologist. 2003;43:678–689. doi: 10.1093/geront/43.5.678. [DOI] [PubMed] [Google Scholar]
- Gallagher-Thompson D, Coon DW. Evidence-based psychological treatments for distress in family caregivers of older adults. Psychology of Aging. 2007;22:37–51. doi: 10.1037/0882-7974.22.1.37. [DOI] [PubMed] [Google Scholar]
- Hopko DR, Lejuez CW, Ruggiero KJ, Eifert GH. Contemporary behavioral activation treatments for depression: Procedures, principles and progress. Clinical psychology review. 2003;23:699–717. doi: 10.1016/s0272-7358(03)00070-9. [DOI] [PubMed] [Google Scholar]
- Jacobson NS, Dobson KS, Truax PA, Addis ME, Koerner K, Gollan JK, et al. A component analysis of cognitive-behavioral treatment for depression. Journal of Consulting and Clinical Psychology. 1996;64:295–304. doi: 10.1037//0022-006x.64.2.295. [DOI] [PubMed] [Google Scholar]
- Katz S, Ford AB, Moscowitz RW, Jackson BA, Jaffee MW. Studies of illness in the aged. The index of ADL: A standardized measure of biological and psychosocial function. Journal of the American Medical Association. 1963;185:914–919. doi: 10.1001/jama.1963.03060120024016. [DOI] [PubMed] [Google Scholar]
- Kleiber DA, Hutchinson SL, Williams R. Lesiure as a resource in transcending negative life events: self-protection, self-restoration, and personal transformation. Leisure Sciences. 2002;24:219–235. [Google Scholar]
- Knight BG, Fox LS, Chou C-P. Factor structure of the burden interview. Journal of Clinical Geropsychology. 2000;6:249–258. [Google Scholar]
- Lawton MP, Brody EM. Assessment of older people: self-maintaining and instrumental activities of daily living. The Gerontologist. 1969;9:179–186. [PubMed] [Google Scholar]
- Lewinsohn PM. Engagement in pleasant activities and depression level. Journal of Abnormal Psychology. 1975;84:729–731. doi: 10.1037//0021-843x.84.6.729. [DOI] [PubMed] [Google Scholar]
- Lewinsohn PM, Hoberman HM, Teri L, Hautzinger M. An integrated theory of depression. In: Reiss S, Bootzin R, editors. Theoretical issues in behavior therapy. New York, NY: Academic Press; 1985. pp. 331–359. [Google Scholar]
- Lewinsohn PM, Youngren M, Grosscup SJ. Reinforcement and depression. In: Dupue RA, editor. The psychobiology of depressive disorders: Implications for the effects of stress. New York, NY: Academic Press; 1979. pp. 291–316. [Google Scholar]
- Logsdon RG, Teri L. The Pleasant Events Schedule-AD: Psychometric properties and relationship to depression and cognition in Alzheimer's disease patients. The Gerontologist. 1997;37:40–45. doi: 10.1093/geront/37.1.40. [DOI] [PubMed] [Google Scholar]
- Mausbach BT, Coon DW, Patterson TL, Grant I. Engagement in activities is associated with affective arousal in Alzheimer's caregivers: A preliminary examination of the temporal relations. Behavior Therapy. 2008;39:366–374. doi: 10.1016/j.beth.2007.10.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mausbach BT, Patterson TL, Grant I. Is depression in Alzheimer's caregivers really due to activity restriction? A preliminary mediational test of the activity restriction. J Behav Ther Exp Psychiatry. 2008;39:459–466. doi: 10.1016/j.jbtep.2007.12.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mazzucchelli T, Kane R, Rees C. Behavioral activation treatments for depression in adults: A meta-analysis and review. Clinical Psychology: Science and Practice. 2009;16:383–411. [Google Scholar]
- Meeks S, Young C, Looney S. Activity participation and affect among nursing home residents: Support for a behavioural model of depression. Aging & Mental Health. 2007;11:751–760. doi: 10.1080/13607860701546910. [DOI] [PubMed] [Google Scholar]
- Miranda J, Muñoz R. Intervention for minor depression in primary care patients. Psychosomatic Medicine. 1994;56:136–141. doi: 10.1097/00006842-199403000-00009. [DOI] [PubMed] [Google Scholar]
- Rabinowitz YG, Mausbach BT, Coon DW, Depp C, Thompson LW, Gallagher-Thompson D. The moderating effect of self-efficacy on intervention response in women family caregivers of older adults with dementia. American Journal of Geriatric Psychiatry. 2006;14:642–649. doi: 10.1097/01.JGP.0000192496.73673.e5. [DOI] [PubMed] [Google Scholar]
- Schulz R, O'Brien AT, Bookwala J, Fleissner K. Psychiatric and physical morbidity effects of dementia caregiving: prevalence, correlates, and causes. The Gerontologist. 1995;35:771–791. doi: 10.1093/geront/35.6.771. [DOI] [PubMed] [Google Scholar]
- Shiffman S, Stone AA, Hufford MR. Ecological momentary assessment. Annual Review of Clinical Psychology. 2008;4:1–32. doi: 10.1146/annurev.clinpsy.3.022806.091415. [DOI] [PubMed] [Google Scholar]
- Sturmey P. Behavioral activation is an evidence-based treatment for depression. Behavior Modification. 2009;33:818–829. doi: 10.1177/0145445509350094. [DOI] [PubMed] [Google Scholar]
- Watson D, Clark LA, Tellegen A. Development and validation of brief measures of positive and negative affect: The PANAS scales. Journal of Personality and Social Psychology. 1988;54:1063–1070. doi: 10.1037//0022-3514.54.6.1063. [DOI] [PubMed] [Google Scholar]
- Watson D, Weber K, Assenheimer JS, Clark LA, Strauss ME, McCormick RA. Testing a tripartite model: I. Evaluating the convergent and discriminant validity of anxiety and depression symptom scales. Journal of Abnormal Psychology. 1995;104:3–14. doi: 10.1037//0021-843x.104.1.3. [DOI] [PubMed] [Google Scholar]
- Watson D, Wiese D, Vaidya J, Tellegen A. The two general activation systems of affect: Structural findings, evolutionary considerations, and psychobiological evidence. Journal of Personality and Social Psychology. 1999;76:820–838. [Google Scholar]
- Wenze SJ, Gunthert KC, Forand NR. Influence of dysphoria on positive and negative cognitive reactivity to daily mood fluctuations. Behaviour research and therapy. 2007;45:915–927. doi: 10.1016/j.brat.2006.08.010. [DOI] [PubMed] [Google Scholar]
- Williamson GM, Shaffer DR, Schulz R. Activity restriction and prior relationship history as contributors to mental health outcomes among middle-aged and older spousal caregivers. Health Psychology. 1998;17:152–162. doi: 10.1037//0278-6133.17.2.152. [DOI] [PubMed] [Google Scholar]
- Zarit SH, Orr NK, Zarit JM. Families under stress: Caring for the patient with Alzheimer's disease and related disorders. New York, NY: University Press; 1985. [Google Scholar]
- Zarit SH, Reever KE, Bach-Peterson J. Relatives of the impaired elderly: Correlates of feeling of burden. Gerontologist. 1980;20:649–655. doi: 10.1093/geront/20.6.649. [DOI] [PubMed] [Google Scholar]