Abstract
Purpose
Inflammation may play an important role in the pathogenesis of diabetic macular edema, a major cause of vision loss in persons with diabetes. The purpose of this study was to evaluate combined antiinflammatory therapy and laser approaches for treating patients with diabetic macular edema.
Methods
In this prospective, factorial, randomized, multicenter trial, we compared cyclo-oxygenase-2 inhibitor (celecoxib) with placebo and diode grid laser with standard Early Treatment Diabetic Retinopathy Study focal laser treatment in 86 participants with diabetic macular edema. The primary outcome is change in visual acuity of ≥15 letters from baseline, and the secondary outcomes include a 50% reduction in the retinal thickening of diabetic macular edema measured by optical coherence tomography and a 50% reduction in leakage severity on fluorescein angiography.
Results
Visual acuity and retinal thickening data from >2 years of follow-up did not show evidence of differences between the medical and laser treatments. However, participants assigned to the celecoxib group were more likely to have a reduction in fluorescein leakage when compared with the placebo group (odds ratio = 3.6; P < 0.01).
Conclusion
This short-term study did not find large visual function benefits of treatment with celecoxib or diode laser compared with those of standard laser treatment. A suggestive effect of celecoxib in reducing fluorescein leakage was observed.
Keywords: diabetic macular edema, celecoxib, diode grid laser photocoagulation, ETDRS type focal photocoagulation, optical coherence tomography
Macular edema as a result of diabetic retinopathy can lead to central vision loss. It is one of the major causes of visual loss in the United States,1 with ∼4.1 million Americans (age ≥40 years) estimated to have diabetic retinopathy.2 Vision-threatening diabetic retinopathy, which includes both proliferative diabetic retinopathy and diabetic macular edema (DME), is estimated to occur in ∼899,000 persons with the majority having type 2 diabetes.2 The estimated proportions of persons with diabetes affected by macular edema are type 1 diabetes, 20%; type 2 diabetes, using insulin, 25%; and type 2 diabetes, not using insulin, 14%.3 The prevalence of diabetes is expected to substantially increase by 2020 with the increasing prevalence of diabetes mellitus in the aging U.S. population.
When macular edema is established, focal laser photocoagulation reduces the risk of moderate visual loss (loss of ≥15 letters from baseline on the Early Treatment Diabetic Retinopathy Study [ETDRS] visual acuity charts) by 50%.4 However, treatment is often not associated with improvement in visual acuity. Furthermore, the focal laser burns may result in an increase in atrophy of the retinal pigment epithelium and progressive enlargement of the initial focal scars of laser photocoagulation and eventually visual loss with central scotomas and decreased color vision.5 Reduction of tissue destruction from laser burns while maintaining the beneficial treatment effect would potentially reduce this long-term risk of laser treatment.
These adverse side effects of the continuous wavelength laser used in the ETDRS technique may theoretically be diminished by using a micropulse diode laser grid, which would result in subthreshold burns with the accompanying reduction of damage from photocoagulation to the retinal pigment epithelium.6,7 This technique has been evaluated in case series without concurrent controls.8–10 This study was designed to compare the micropulse diode grid laser with the standard ETDRS focal laser technique using the continuous wavelength laser.
Animal models of diabetic retinopathy demonstrate that inflammation plays an important role in diabetic retinopathy.11 In early onset of diabetic retinopathy, up-regulation of cyclo-oxygenase-2 (COX-2) occurs in retinal cells. This results in elevated prostaglandin production, leading to an increased expression of vascular endothelial growth factor and an increased risk of vascular leakage and retinal neovascularization.12 High doses of aspirin and intermediate doses of COX-2 inhibitors (celecoxib) were apparently beneficial in early experimental diabetic retinopathy.13 Other investigations have shown that periocular celecoxib-poly (lactide-co-glycolide) microparticles inhibited elevations of retinal vascular endothelial growth factor and other factors for as long as 60 days in a diabetic animal model.14 Cyclo-oxygenase-2 inhibitors have been demonstrated to have antiangiogenic effects in a rat model of ischemic proliferative retinopathy,15 and COX-2 expression is evident in human retina of individuals with diabetes.8
These data suggest that treatment with a COX-2 inhibitor may be beneficial in the treatment of DME. The purpose of this study was to gather pilot data to evaluate the feasibility of mounting a larger multicenter study to evaluate the efficacy of celecoxib (a COX-2 inhibitor and a nonsteroid anti-inflammatory drug) and of a modified laser photocoagulation technique for the treatment of DME.
Study Design
This multicenter study was designed to investigate the feasibility and the proof-of-principle study for 2 new treatment approaches for patients with diabetic retinopathy and clinically significant macular edema (n = 100), potentially leading to initiation of a larger Phase 3 clinical trial.
Design
A total of 86 participants were enrolled from December 2002 through November 2004 at 8 centers in the United States after reviewing and signing an informed consent form approved by the respective sites' Institutional Review Boards. This study was prematurely terminated because of safety concerns of celecoxib treatment reported by other large trials.16 Eligibility criteria included age ≥18 years, evidence of type 1 or 2 diabetes, evidence of clinically significant macular edema in at least one eye that requires laser treatment, and best-corrected visual acuity of 20/400 or better using the ETDRS refraction and visual acuity measurement protocol.17 In addition, exclusion criteria included the following: retinopathy that may require scatter photocoagulation immediately, other retinal and systemic diseases that might confound the outcomes (age-related macular degeneration, uveitis, drug toxicity, sarcoidosis, inflammatory bowel disease, and so on), and a history of myocardial infarction within the previous 2 years.
Participants were randomly assigned to receive an oral dose of 400 mg (200 mg 2 times a day) of celecoxib or a matching placebo only daily for 3 months without laser, and the medical therapy of celecoxib continued until the study was stopped. All participants and the research team at each clinical site were masked to the study medication assignments. Eligible eyes of participants were randomly assigned to receive either ETDRS focal laser18 or diode grid laser photocoagulation at their 3-month visit if macular edema persisted. If both eyes were eligible, the right eye was designated as the study eye and was randomly assigned to receive one of two laser therapies with the fellow eye assigned to receive the alternate laser treatment. The first laser treatment was given when the study ophthalmologist judged that the laser treatment was medically indicated, starting 3 months after randomization to celecoxib or placebo. All laser treatments given during the first year were performed according to the randomized laser treatment assignment. After 1 year of follow-up, participants, who had their eyes initially treated with diode laser treatment, were allowed to receive ETDRS laser treatment if additional treatment was required.
The micropulse diode technique was conducted with the 810 diode laser (Iris Medical OcuLight SLx, IRIDEX Corporation, Mountain View, CA) by using the MicroPulse operating mode. The treatment consisted of 125-μm size burns using a 10% duty cycle with 0.2-second pulse envelope duration with a maximum power of 1.8 W. These were subthreshold burns that covered the entire area of macular edema with minimal clinical detection or fluorescein angiographic changes associated with these laser burns. The ETDRS focal treatment using yellow or green laser was a technique of direct laser photocoagulation (50–100 μm spot size) at microaneurysms with light burns, not necessary to whiten or darken the lesions. When no focal leakage was identified, a grid laser with light burns was administered to sufficiently cover the area of edema. The burns were spaced greater than one burn width apart with the sparing of the 500 μm from the center of the fovea.
Study visits were scheduled 3 and 6 months after enrollment and every 6 months thereafter for a total of 3 years of follow-up. At each study visit, a comprehensive ophthalmic examination was conducted including best-corrected visual acuity, slit-lamp biomicroscopy, dilated fundus examination, retinal thickness with the optical coherence tomography (Stratus OCT, Carl Zeiss Meditec, Dublin, CA), and fluorescein angiography (FA). Laser photocoagulation therapy was considered for all participants with clinically significant macular edema at each study visit. The study design and study data were reviewed and monitored by the National Eye Institute's Data and Safety Monitoring Committee.
Outcomes
The designated primary outcome was a ≥15-letter score improvement in best-corrected visual acuity from baseline to the third year. The secondary outcome was a significant reduction of macular edema at the end of the third year. A significant reduction was defined as a 50% reduction in retinal thickening as measured by optical coherence tomography and a 50% reduction in leakage area as measured by FA. The optical coherence tomographies and FAs were graded by the Fundus Photograph Reading Center at the University of Wisconsin, whose graders were also masked to the assignment of the medical therapy.19,20 An additional secondary outcome was the number of laser treatments required during the course of the study. Safety measurements, including laboratory tests and adverse event assessments, were also collected. Because of the premature study termination, outcomes through the second year were analyzed. This early termination also reduced the power of the study because the projected sample size of 100 was not achieved.
Change in Recruitment and Follow-Up
On December 17, 2004, the National Institutes of Health suspended the use of celecoxib for all participants in a large colorectal cancer prevention clinical trial, the Adenoma Prevention with Celecoxib Trial, because analyses by the trial's Data Safety and Monitoring Committee found a two- to threefold increased risk of major fatal and nonfatal cardiovascular events for participants taking celecoxib compared with those in the placebo group.21 In accordance with the Data and Safety Monitoring Committee's action on other National Institutes of Health-supported studies using a COX-2 inhibitor, the National Eye Institute Data and Safety Monitoring Committee thoroughly reviewed all the reported adverse events as well as the main study results on December 20, 2004, and recommended that the National Eye Institute close the enrollment of participants and also suspend the use of celecoxib or placebo for all enrolled participants. The participants were followed for 1 year after discontinuing the study drug. This resulted in curtailed follow-up, especially for participants who were enrolled late in the study, and lowered the power of the study evaluating the long-term effects of study treatments.
Statistical Methods
The cross-sectional analyses of the primary and secondary outcomes for each study visit were examined using two-sample mean and proportion comparison tests. The generalized estimating equation method was used to adjust the difference between the two groups for the correlation between bilateral outcomes.22 When a statistically significant difference existed between the two groups, the extended generalized estimating equation method was applied to investigate the trends and variations in the outcome measures during the course of the study.23 To allow for the unequal length of follow-up of each participant, the proportional hazard model for the first occurrence of event of interest was also considered if the result from the generalized estimating equation model was statistically significant. Parsimonious and well-fitted models for each outcome were derived by backward variable selection of the following variables: age and baseline level of each outcome. All the data analyses were conducted using SAS version 8.2 (SAS Institute, Inc., Cary, NC).
Results
Baseline Demographics and Characteristics
Eighty-six participants with diabetic retinopathy and clinically significant macular edema were enrolled (Table 1). Forty-seven participants were randomly assigned to the placebo group (34% women and 74% white) and 39 participants to the celecoxib group (43% women and 59% white) (Figure 1). The median ages for the placebo and celecoxib participants were 61 and 58 years, respectively. All the participants have received diabetic treatments, including insulin, oral medication, or diet (94% and 92% of placebo and celecoxib participants, respectively, on insulin or oral medication for at least 1 year). Participants with both eyes eligible for the study numbered 14 in the placebo group and 9 in the celecoxib group. The median visual acuity score and retinal thickening (thickness −175 μm) at the center subfield at baseline was 75 letters (20 of 32) and 135 μm and 82 letters (20 of 25) and 85 μm for the placebo and celecoxib groups, respectively. There was an imbalance of the retinal thickness between the placebo and celecoxib groups.
Table 1. Participant Demographic and Baseline Characteristics by Treatment Group.
| Placebo | Celecoxib | |
|---|---|---|
| Randomized participants | 47 (100%) | 39 (100%) |
| Sex, female | 16 (34%) | 17 (43%) |
| Race, white | 35 (74%) | 23 (59%) |
| Age (median years) | 61 | 58 |
| ≥1-year diabetic treatment of insulin or oral medication | 44 (94%) | 36 (92%) |
| Number of eyes* | 61 | 48 |
| VA (median letter score) | 75 | 82 |
| Retinal thickening at the center subfield (median)† | 135 | 85 |
| Laser type assigned for eligible eyes | ||
| Diode | 31 | 25 |
| ETDRS | 30 | 23 |
| Laser type given for eligible eyes by randomization | ||
| Diode | 18 | 13 |
| ETDRS | 23 | 13 |
Both eyes are eligible in 23 participants (14 in the placebo group and 9 in the celecoxib group).
Retinal thickening at the center subfield is excessive thickness >175 (the difference of retinal thickness between the study participants and a normal subject).
VA, visual acuity.
Fig. 1.
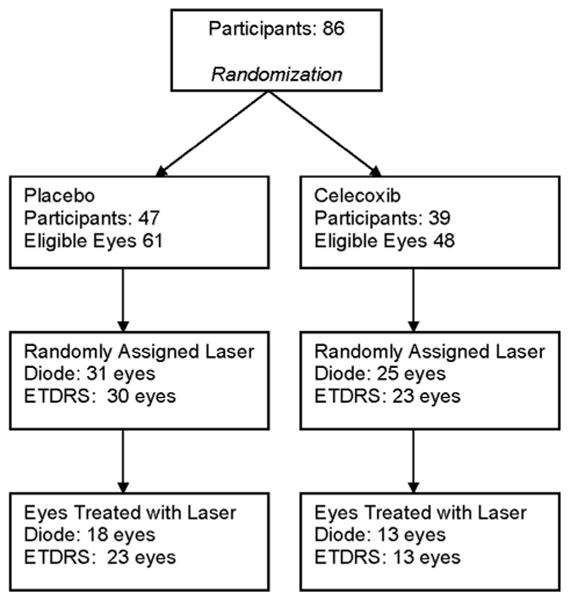
The enrollment and randomization of the study participants.
Follow-Up and Duration of Drug Treatment
Among the 86 enrolled participants, 78 (91%) participants (43 in the placebo group and 31 in the celecoxib group) completed 1 year of follow-up and 54 (63%) participants (29 in the placebo group and 25 in the celecoxib group) finished the 2-year follow-up visit (Table 2).
Table 2. Participants' Follow-Up and Duration on Study Therapy Before Mandated Discontinuation by Treatment Group.
| Placebo | Celecoxib | P | |
|---|---|---|---|
| Randomized participants | 47 (100%) | 39 (100%) | |
| Follow-up (months)* | |||
| <12 | 2 (4%) | 6 (15%) | |
| ≥12–<24 | 16 (34%) | 8 (21%) | |
| ≥24 | 29 (62%) | 25 (64%) | |
| Duration (months) on drug treatment† | |||
| <12 | 21 (45%) | 18 (46%) | |
| ≥12–<24 | 24 (51%) | 19 (49%) | |
| ≥24 | 2 (4%) | 2 (5%) | |
| Serious cardiovascular events | |||
| Entire follow-up‡ | 9 (19%) | 3 (8%) | 0.225 |
| CTSA§ | 6 (13%) | 2 (5%) | 0.283 |
Follow-up is based on the most recent clinical/ophthalmic examination visit.
Follow-up before mandatory discontinuation of masked and randomized study medication (either placebo or celecoxib).
Follow-up until study closeout.
Cross-Trials Safety Analysis (CTSA, this includes this study of diabetic retinopathy and other studies of randomized, controlled trials of celecoxib for adenoma of the gastrointestinal system, breast cancer, and for Alzheimer disease) has adjudicated cardiovascular adverse events from randomization to 1 year after study therapy discontinuation (January 31, 2005); 1 death because of stroke of a placebo participant is not included.
Before cessation of the study therapy on December 31, 2004, 47 participants (26 in the placebo group and 21 in the celecoxib group) had received study medication for at least 1 year. Until study closeout, 9 placebo participants (19%) and 3 celecoxib participants (8%) experienced a serious, cardiovascular adverse event (exact P = 0.225). The data from this trial collected through January 31, 2005, have been analyzed with the data from 5 other randomized, controlled trials of celecoxib supported by the National Cancer Institute in a project called the Cross-Trials Safety Analysis for the risk of serious cardiovascular events caused by the use of celecoxib.15 This small study has too few participants to yield clinically meaningful data (Table 2).
Visual Acuity
Table 3 (Figure 2) compares mean changes in visual acuity by treatment group (placebo or celecoxib) at each study visit. No significant differences were detected in mean visual acuity. Additionally, the rates of vision loss of ≥3 lines from baseline to 1 and 2 years were also similar (P = 0.82 and P = 0.66 for comparison of mean changes, respectively). During the first year, 7 placebo participants (12%) and 3 celecoxib participants (8%) lost ≥3 lines of vision. Three placebo participants (5%) and 2 celecoxib participants (5%) gained ≥3 lines of vision. Overall, the drug-treated group and placebo group do not differ significantly in visual acuity results (either improvement or worsening) at any of the time points.
Table 3. Visual Acuity by Treatment Group.
| Month | Treatment Group | Number of Eyes (Participants) | Mean/Median Change in Letter Score* | 95% CI for Mean | P† | Gain of ≥15-Letter Score | Loss of ≥15-Letter Score |
|---|---|---|---|---|---|---|---|
| 6 | Placebo | 57 (44) | −1.42/−1.0 | −3.41−0.56 | 0.45 | 1/57 (1.8%) | 2/57 (3.5%) |
| Celecoxib | 40 (34) | −3.15/−2.0 | −7.34−1.04 | 2/40 (5.0%) | 3/40 (7.5%) | ||
| 12 | Placebo | 56 (43) | −2.25/−1.0 | −5.08−0.58 | 0.82 | 3/56 (5.4%) | 7/56 (12.5%) |
| Celecoxib | 37 (31) | −2.89/−1.0 | −7.66−1.88 | 2/37 (5.4%) | 3/37 (8.1%) | ||
| 18 | Placebo | 51 (39) | −1.86/−1.0 | −4.91−1.19 | 0.47 | 3/51 (5.9%) | 6/51 (11.8%) |
| Celecoxib | 35 (29) | −3.77/−2.0 | −8.33−0.78 | 0/35 (0%) | 3/35 (8.6%) | ||
| 24 | Placebo | 35 (28) | −1.42/−1.0 | −5.84−2.99 | 0.66 | 2/35 (5.7%) | 5/35 (14.3%) |
| Celecoxib | 29 (25) | −3.03/0.0 | −8.99−2.92 | 3/29 (10.3%) | 4/29 (13.8%) |
Change is the difference from baseline. Positive (negative) values indicate the increase (decrease) in visual acuity letter score.
The significance level of the treatment group effect in an analysis of variance for repeated measures; data to incorporate the correlation between bilateral outcomes.
CI, confidence interval.
Fig. 2.
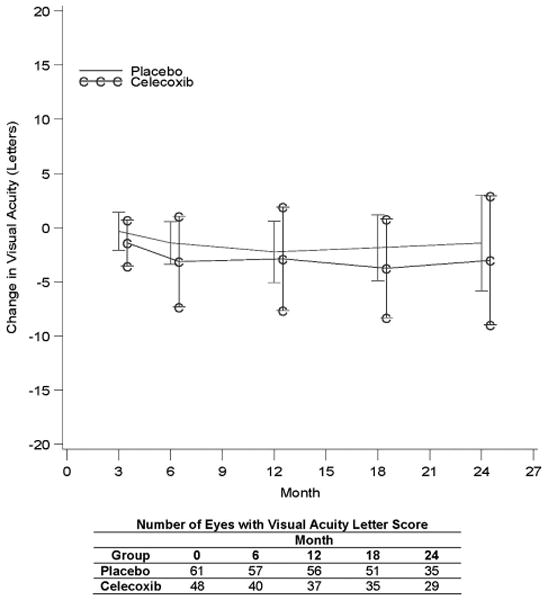
The mean change in visual acuity in participants assigned to celecoxib or placebo.
Laser Treatments
Fifty-eight participants needed at least one laser treatment for their macular edema (nine participants needed laser treatment in both eyes and received different laser treatments in each). More specifically, 41 eyes of 34 participants in the placebo group (34 of 47 [72%]) and 26 eyes of 24 participants in the celecoxib group (24 of 39 [62%]) required at least 1 laser treatment throughout the follow-up period. The participants in the placebo group had slightly higher rates of requiring laser treatments than those participants in the celecoxib group, but this was not statistically significant (odds ratio [OR] = 1.63; P = 0.36 for participants and OR = 1.73; P = 0.15 for eyes). After the 1-year follow-up visit, the investigator was permitted to treat the participants with either lasers (11 participants switched from diode laser to ETDRS laser). Table 4 compares the proportion of laser retreatment among the laser-treated eyes. The proportion was estimated from a binomial probability distribution with the denominator being the number of opportunities to receive laser retreatment before the last visit. These analyses do not provide evidence that celecoxib reduces the need for laser retreatment (P ≥ 0.54).
Table 4. Laser Retreatments Among Laser-Treated Eyes.
| Number of Eyes With Laser Retreatment | Placebo (%)* | Celecoxib (%)* | OR† | P |
|---|---|---|---|---|
| Diode (19 placebo; 10 celecoxib) | 43 | 42 | 0.96 | 0.90 |
| ETDRS (22 placebo; 16 celecoxib) | 55 | 56 | 1.20 | 0.54 |
| Total (41 placebo; 26 celecoxib) | 49 | 51 | 1.11 | 0.65 |
Rates were estimated using a binomial probability model with the number of opportunities to receive laser retreatments before last visit.
Reference group is placebo.
Fluorescein Angiographic Leakage Severity
The number of participants eligible for the analysis of fluorescein leakage was decreased because the FAs of 4 participants were not gradable, and 6 participants had stage 1 or less in severity of macular edema at baseline, making them ineligible for analysis of the reduction of FA leakage by 2 steps. At the first-year follow-up visit, participants in the celecoxib group had a higher chance of having reduced FA leakage severity than did the participants in the placebo group (43% vs 26% complete case analysis; 33% vs 22% intention-to-treat analysis), but this difference was not statistically significant (exact P > 0.19). At the second-year follow-up visit, 3 of 24 (12%) participants in the placebo group and 9 of 20 (45%) participants in the celecoxib group experienced a ≥2-step reduction in leakage severity (exact P = 0.02). These statistically significant effects of celecoxib on the 2-step leakage severity reduction also appear in the intention-to-treat analysis that treats all missing outcomes as failures. Although the statistical significance levels are diminished, the effects are still suggestive in the most conservative analysis (OR = 4.11; exact P = 0.057 at year 2).
Table 5 presents repeated measures analyses of a ≥2-step reduction in leakage severity. Celecoxib participants had reduced leakage severity with a higher likelihood than did placebo participants (unadjusted OR = 2.45; P = 0.054 and unadjusted OR = 3.31; P = 0.002 for 1- and 2-year results, respectively). Adjusting for baseline leakage severity, follow-up year, and laser treatment, the reduction in leakage associated with celecoxib remains significant at 2 years (OR = 3.52; P = 0.002). Repeated measure analyses based on the entire follow-up data set have similar results. Figure 3 displays Kaplan–Meier estimates of the incidence of the first event of a ≥2-step reduction in leakage severity. Cox proportional hazards model, for the time to the first occurrence of a ≥2-step reduction in leakage severity, shows that there is a 1.8 times higher chance of reduction in leakage severity (P = 0.067) in participants assigned to the celecoxib group than that in participants assigned to the placebo group. Figure 4 shows the typical increased fluorescein leakage in the study eye of a participant at baseline (Figure 4A). There was a reduction in the fluorescein leakage of 2 steps along the severity scale at 24 months (Figure 4B).
Table 5. The Reduction of Fluorescein Leakage by 2 or More Steps in Eyes With at Least Stage 2 Severity of Macular Edema at Baseline in Those Subjects Assigned to Celecoxib Treatment*.
| Month | Covariate Adjustment Factors | OR† | 95% CI for OR | P |
|---|---|---|---|---|
| 12 | None | 2.45 | 0.99−6.09 | 0.054 |
| Baseline severity and year | 2.43 | 0.98−6.07 | 0.056 | |
| Baseline severity, year, and laser treated | 2.47 | 0.99−6.15 | 0.052 | |
| 24 | None | 3.31 | 1.54−7.12 | 0.002 |
| Baseline severity and year | 3.50 | 1.59−7.67 | 0.002 | |
| Baseline severity, year, and laser treated | 3.52 | 1.61−7.71 | 0.002 | |
| 36 | None | 3.60 | 1.71−7.59 | 0.001 |
| Baseline severity and year | 3.74 | 1.73−8.10 | 0.001 | |
| Baseline severity, year, and laser treated | 3.75 | 1.73−8.11 | 0.001 |
Analysis of variance model for repeated measures.
Reference group is placebo.
CI, confidence interval.
Fig. 3.
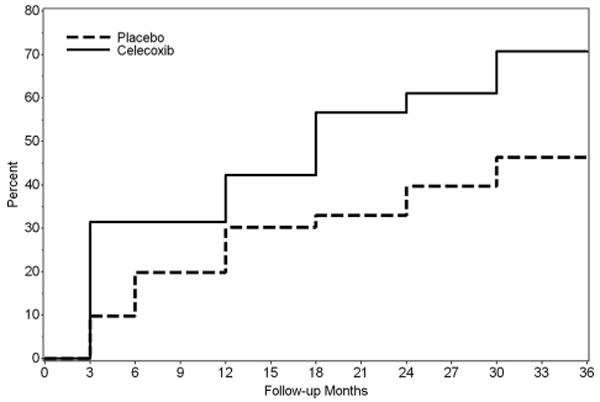
Life table estimates of the time to progression in fluorescein leakage in participants assigned to celecoxib or placebo.
Fig. 4.
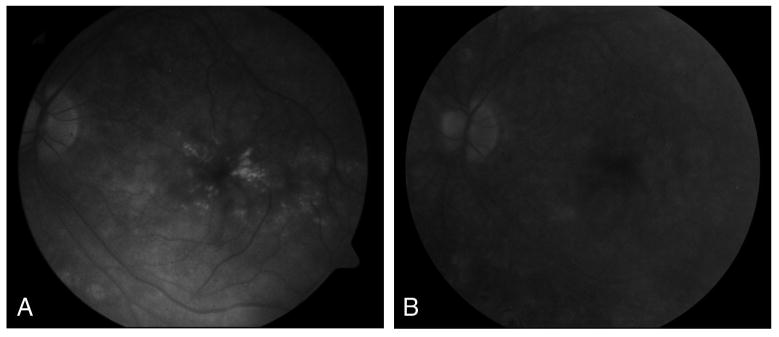
At baseline (A), the clinically significant macular edema of this left study eye of a 31-year-old man with a 16-year history of diabetes had fluorescein leakage that was reduced significantly at 24 months. He did not receive laser photocoagulation during the course of the study (B).
Retinal Thickening Measured on Optical Coherence Tomography
Retinal thickening measurements at the center subfield, the excessive thickness compared with that of a normal eye (defined as 175 μm), are right skewed and subject to high variation and therefore transformation may be required (e.g., log transformation); however, the results based on this transformation (not shown) do not differ from those based on raw scales. Participants in both treatment groups presented with reduced retinal thickening by ∼26 μm to 31 μm on average during the first year (P = 0.66 in Table 6) and by >64 μm during the second year (P = 0.94 in Table 6). In the first year, 4 of 40 eyes in the placebo group (10%) and 5 of 27 eyes in the celecoxib group (18%) had a ≥50% reduction in retinal thickening. Eleven eyes (27%) of the placebo participants and 8 eyes (30%) of the celecoxib participants had at least a 25% reduction in the first year. These reduction rates do not differ between the two treatment groups (P ≥ 0.26 for either size reduction). Within the specific laser type, both treatment groups showed a similar degree of reduction (∼30 μm) in retinal thickening. Overall, there are no statistically significant differences in changes in retinal thickening by treatment group or laser treatment.
Table 6. Retinal Thickening of Eligible Study Eyes by Treatment Group*.
| Month | Treatment Group | Number of Eyes | Change in Retinal Thickening† | Relative Change in Retinal Thickening† | |||
|---|---|---|---|---|---|---|---|
| Median/Mean | 95% CI for Mean | P‡ | 50% Reduction | 25% Reduction | |||
| 12 | Placebo | 40 | −14.0/−25.7 | −53.1−1.7 | 0.66 | 4/40 (10%) | 11/40 (27.5%) |
| Celecoxib | 27 | −8.0/−30.7 | −71.5−10.1 | 5/27 (18.5%) | 8/27 (29.6%) | ||
| 18 | Placebo | 37 | −11.0/−23.5 | −59.8−12.8 | 0.60 | 7/37 (18.9%) | 11/37 (29.7%) |
| Celecoxib | 21 | −11.0/−36.4 | −90.4−17.5 | 5/21 (23.8%) | 6/21 (28.6%) | ||
| 24 | Placebo | 24 | −36.0/−63.7 | −99.9−27.4 | 0.94 | 7/24 (29%) | 11/24 (45.8%) |
| Celecoxib | 21 | −40.0/−65.5 | −117.8−13.2 | 5/16 (23.8%) | 7/21 (33.3%) | ||
Retinal thickening at the center subfield is excessive thickness >175 (the difference of retinal thickness between the study participants and a normal subject).
Negative (positive) sign indicates the decrease (increase) of retinal thickening.
Significance level of the treatment group effect in an analysis of variance for repeated measures data to incorporate the correlation between bilateral outcomes.
CI, confidence interval.
Discussion
The results of this pilot study suggest that it is feasible to mount a multicenter study to evaluate the role of medical and laser therapies for the treatment of DME. However, the COX-2 inhibitor chosen for this study, celecoxib, was associated with an increased risk of cardiovascular disease in other clinical trials. The increased risk observed in several large trials makes it difficult to launch a large clinical trial in persons with diabetes who are already at an increased risk for cardiovascular disease.
This pilot study has insufficient power to evaluate the potential beneficial effect of both the medical and laser treatment approaches. Although the early discontinuation of celecoxib in this study may have reduced any measurable beneficial effects, these data did not provide evidence of the treatment effects from these therapeutic strategies. The inflammatory pathways found in the animal data are compelling, and it is intriguing that the medical therapy with the COX-2 inhibitor resulted in an apparently greater reduction in fluorescein leakage compared with the placebo group. These leakage results were verified by regrading the leakage at the centralized reading center with similar results. This apparent reduction in fluorescein leakage suggests that COX-2 inhibitors or other anti-inflammatory treatments may have a role in therapy for DME.
Focal laser photocoagulation treatment given in the focal ETDRS fashion is the only therapy currently demonstrated to be beneficial for the treatment of DME. The ETDRS showed that this treatment reduced the 3-year rate of moderate vision loss (≥3 lines of acuity loss) by 50%.6 However, only 17% of the treated eyes that had baseline acuity worse than 20/40 experienced moderate visual gain (≥3 lines of acuity improvement).6 Our results from the laser arm showed that there were no large differences detected between the two laser techniques evaluated in this study. It should also be noted that during the first year, 11 of those assigned to diode laser were switched to the ETDRS type of treatment.
This pilot study was too small and its follow-up too short to evaluate whether some of the possible side effects of laser photocoagulation such as enlargement of laser burns, increases in scotomas, and decreased vision can be attenuated with diode laser treatment. Studies with longer duration and larger numbers of participants would be required to answer this question.
The current investigations of possible therapies for DME have included intravitreal triamcinolone,24 oral protein kinase C inhibitors,25 intravitreal aptamers,26,27 antibodies directed against vascular endothelial growth factor,28,29 and vitrectomy.30 Intravitreal triamcinolone injection does address the issue of inflammation, but intravitreal injections are accompanied by the potential adverse effects of raised intraocular pressure, the development of cataract, and the rare possibility of endophthalmitis. A recently completed trial of intravitreal triamcinolone injections versus DME confirmed the importance of laser photocoagulation after 2 years of follow-up.31 Intravitreal steroids may have some short-term beneficial effect, and the effects of combined steroids and laser are yet to be fully evaluated. Studies are also underway to evaluate the use of intravitreal antivascular endothelial growth factor therapy for DME.
Laboratory data and observational studies suggest that inflammation may play a potential role in the pathogenesis of diabetic macular retinopathy. Although this study failed to provide evidence that COX-2 inhibitors may be effective in the treatment of DME, there was some evidence of a reduction of fluorescein leakage, and future investigations of anti-inflammatory agents for the treatment of DME seem warranted.
Acknowledgments
Supported by the National Eye Institute or National Institutes of Health intramural program. The study medication and funds for the examinations of the participants enrolled in the extramural clinics were provided by Pharmacia.
References
- 1.The Eye Disease Prevalence Research Group Causes and prevalence of visual impairment among adults in the United States. Arch Ophthalmol. 2004;122:477–485. doi: 10.1001/archopht.122.4.477. [DOI] [PubMed] [Google Scholar]
- 2.The Eye Disease Prevalence Research Group The prevalence of diabetic retinopathy among adults in the United States. Arch Ophthalmol. 2004;122:552–563. doi: 10.1001/archopht.122.4.552. [DOI] [PubMed] [Google Scholar]
- 3.Klein R, Klein B, Moss SE, Davis MD, DeMets DL. The Wisconsin epidemiologic study of diabetic retinopathy. IV. Diabetic macular edema. Ophthalmology. 1984;91:1464–474. doi: 10.1016/s0161-6420(84)34102-1. [DOI] [PubMed] [Google Scholar]
- 4.Photocoagulation for diabetic macular edema. Early Treatment Diabetic Retinopathy Study report number 1. Early Treatment Diabetic Retinopathy Study Research Group. Arch Ophthalmol. 1985;103:1796–1806. [PubMed] [Google Scholar]
- 5.Schatz H, Maderia D, McDonald HR, Johnson RN. Progressive enlargement of laser scars following grid laser photocoagulation for diffuse diabetic macular edema. Arch Ophthalmol. 1991;109:1549–1551. doi: 10.1001/archopht.1991.01080110085041. [DOI] [PubMed] [Google Scholar]
- 6.Mainster MA. Decreasing retinal photocoagulation damage: principles and techniques. Semin Ophthalmol. 1999;14:200–209. doi: 10.3109/08820539909069538. [DOI] [PubMed] [Google Scholar]
- 7.Roider J. Laser treatment of retinal diseases by subthreshold laser effects. Semin Ophthalmol. 1999;14:19–26. doi: 10.3109/08820539909056059. [DOI] [PubMed] [Google Scholar]
- 8.Roider J, Brinkmann R, Wirbelauder C, Laqua H, Birngruber R. Subthreshold (retinal pigment epithelium) photocoagulation in macular diseases: a pilot study. Br J Ophthalmol. 2000;84:40–47. doi: 10.1136/bjo.84.1.40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Luttrull JK, Musch DC, Mainster MA. Subthreshold diode micropulse photocoagulation for the treatment of clinically significant diabetic macular edema. Br J Ophthalmol. 2005;89:74–80. doi: 10.1136/bjo.2004.051540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Sivaprasad S, Sandhu R, Tandon A, Sayed-Ahmed K, McHugh DA. Subthreshold micropulse diode laser photocoagulation for clinically significant diabetic macular oedema: a three-year follow-up. Clin Experiment Ophthalmol. 2007;7:640–644. doi: 10.1111/j.1442-9071.2007.01566.x. [DOI] [PubMed] [Google Scholar]
- 11.Johnson EI, Dunlop ME, Larkins RG. Increased vasodilatory prostaglandin production in the diabetic rat retinal vasculature. Curr Eye Res. 1999;18:79–82. doi: 10.1076/ceyr.18.2.79.5386. [DOI] [PubMed] [Google Scholar]
- 12.Aiello LP, Avery RL, Arrigg PG, et al. Vascular endothelial growth factor in ocular fluid of patients with diabetic retinopathy and other retinal disorders. N Engl J Med. 1994;331:1480–1487. doi: 10.1056/NEJM199412013312203. [DOI] [PubMed] [Google Scholar]
- 13.Joussen AM, Poulaki V, Mitsiades N, et al. Nonsteroidal anti-inflammatory drugs prevent early diabetic retinopathy via TNF-alpha suppression. FASEB J. 2002;16:438–440. doi: 10.1096/fj.01-0707fje. [DOI] [PubMed] [Google Scholar]
- 14.Amrite AC, Ayalasomayajula SP, Cheruvu NPS, Kompella UB. Single periocular injection of celecoxib-PLGA microparticles inhibits diabetes induced elevations of retinal PGE2, VEGF, and vascular leakage. Invest Ophthalmol Vis Sci. 2006;47:1149–1160. doi: 10.1167/iovs.05-0531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Sennlaub F, Valamanesh F, Vazquez-Tello A, et al. Cyclooxygenase-2 in human and experimental ischemic proliferative retinopathy. Circulation. 2003;108:198–204. doi: 10.1161/01.CIR.0000080735.93327.00. [DOI] [PubMed] [Google Scholar]
- 16.Solomon SD, Wittes J, Finn PV, et al. Cardiovascular risk of celecoxib in 6 randomized placebo-controlled trials: the cross trial safety analysis. Circulation. 2008;117:2104–2113. doi: 10.1161/CIRCULATIONAHA.108.764530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ferris FL, Kassoff A, Bresnick GH, Bailey I. New visual acuity charts for clinical research. Am J Ophthalmol. 1982;94:91–96. [PubMed] [Google Scholar]
- 18.Treatment techniques and clinical guidelines for photocoagulation of diabetic macular edema. Early Treatment Diabetic Retinopathy Study Report Number 2. Early Treatment Diabetic Retinopathy Study Research Group. Ophthalmology. 1987;94:761–774. doi: 10.1016/s0161-6420(87)33527-4. [DOI] [PubMed] [Google Scholar]
- 19.Davis MD, Bressler SB, Aiello LP, et al. Comparison of time-domain OCT and fundus photographic assessments of retinal thickening in eyes with diabetic macular edema. Invest Ophthalmol Vis Sci. 2008;49:1745–1752. doi: 10.1167/iovs.07-1257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Classification of diabetic retinopathy from fluorescein angiograms. ETDRS report number 11. Early Treatment Diabetic Retinopathy Study Research Group. Ophthalmology. 1991;98:807–822. [PubMed] [Google Scholar]
- 21.Solomon SD, McMurray JJV, Pfeffet MA, et al. Cardiovascular risk associated with celecoxib in a clinical trial for colorectal adenoma prevention. N Engl J Med. 2005;352:1071–1080. doi: 10.1056/NEJMoa050405. [DOI] [PubMed] [Google Scholar]
- 22.Liang KY, Zeger SL. Longitudinal data analysis using generalized linear model. Biometrika. 1986;73:13–22. [Google Scholar]
- 23.Zhao LP, Prentice RL. Correlated binary regression using a quadratic exponential model. Biometrika. 1990;77:642–648. [Google Scholar]
- 24.Martidis A, Duker JS, Greenberg PB, et al. Intravitreal triamcinolone for refractory diabetic macular edema. Ophthalmology. 2002;109:920–927. doi: 10.1016/s0161-6420(02)00975-2. [DOI] [PubMed] [Google Scholar]
- 25.The PKC-DRS Study Group The effect of ruboxistaurin on visual loss in patients with moderately severe to very severe nonproliferative diabetic retinopathy: initial results of the Protein Kinase C beta Inhibitor Diabetic Retinopathy Study (PKC-DRS) multicenter randomized clinical trial. Diabetes. 2005;54:2188–2197. doi: 10.2337/diabetes.54.7.2188. [DOI] [PubMed] [Google Scholar]
- 26.Cunningham ET, Adamis AP, Altaweel M. A phase II randomized double-masked trial of pegaptanib, an anti-vascular endothelial growth factor aptamer, for diabetic macular edema. Ophthalmology. 2005;112:1747–1757. doi: 10.1016/j.ophtha.2005.06.007. [DOI] [PubMed] [Google Scholar]
- 27.Cunningham ET, Jr, Adamis AP, Altaweel M, Macugen Diabetic Retinopathy Study Group A phase II randomized double-masked trial of an anti-vascular endothelial growth factor aptamer, for diabetic macular edema. Ophthalmology. 2005;112:1747–1757. doi: 10.1016/j.ophtha.2005.06.007. [DOI] [PubMed] [Google Scholar]
- 28.Haritoglou C, Kook D, Neubauer A, et al. Intravitreal bevacizumab (Avastin) therapy for persistent diffuse diabetic macular edema. Retina. 2006;26:999–1005. doi: 10.1097/01.iae.0000247165.38655.bf. [DOI] [PubMed] [Google Scholar]
- 29.Nguyen QD, Tatlipinar S, Shah SM, et al. Vascular endothelial growth factor is a critical stimulus for diabetic macular edema. Am J Ophthalmol. 2006;142:961–969. doi: 10.1016/j.ajo.2006.06.068. [DOI] [PubMed] [Google Scholar]
- 30.Pendergast SD, Hassan TS, Williams GA, et al. Vitrectomy for diffuse diabetic macular edema associated with a taut premacular posterior hyaloid. Am J Ophthalmol. 2000;130:178–186. doi: 10.1016/s0002-9394(00)00472-4. [DOI] [PubMed] [Google Scholar]
- 31.Diabetic Retinopathy Clinical Research Network A randomized trial comparing intravitreal triamcinolone acetonide and focal/grid photocoagulation for diabetic macular edema. Ophthalmology. 2008;115:1445–1446. doi: 10.1016/j.ophtha.2008.06.015. [DOI] [PMC free article] [PubMed] [Google Scholar]


