Abstract
INTRODUCTION
We aimed to analyse national trends in varicose vein treatment in the UK National Health Service (NHS).
PATIENTS AND METHODS
The National Hospital Episode Statistics website (<http://www.Hesonline.nhs.uk>) was interrogated for patients treated (1998–2008) in the NHS for varicose veins.
RESULTS
There has been a 34% decline in patients presenting for an intervention for varicose veins. For surgical procedures alone, the waiting times have fallen by 59%. In 2007–2008, 30,663 (72%) fewer bed days were used in comparison to 1998; accompanied by a 49% decline in the number of patients undergoing surgery. After a 47% decrease between 1998 and 2001, the number of patients requesting sclerotherapy treatment has increased by a substantial 311% over the subsequent 7 years. Transluminal procedures were used almost twice as often in 2007–2008 as in 2006–2007.
CONCLUSIONS
There has been a steady decline in the number of patients treated for varicose veins. Fewer patients are undergoing surgery but are being managed more efficiently, with an increase in day cases and a reduction in total bed days. The demand for minimally invasive procedures has increased substantially. These trends will be of great importance for the future planning of vascular surgical services.
Keywords: Varicose veins, Trends, Surgical procedures, Minimally invasive, Sclerotherapy, Radiofrequency catheter ablation
Varicose veins are a common medical problem and a frequent cause for referral and treatment within the UK NHS. It has a point prevalence of 20–25% in women and 10–15% in men over the age of 15 years. The overall prevalence has been reported as 20–60%.1 Common presenting symptoms include pain, oedema, fatigue, venous ulcers and cosmesis. The disease is a significant socio-economic burden due to direct costs to the NHS and indirectly to the economy due to the loss of manpower days. Various techniques have been described for its treatment. Over the last few years, the advent of minimally invasive techniques has been generating considerable interest as alternatives to traditional surgery. Despite this high prevalence and the vast numbers of people being treated, the criteria for each of the various treatments are not well defined.2,3 Furthermore, there is no general consensus over which intervention is the most effective in the management of varicose veins.4 In addition, there is a lack of uniformity in the provision and funding of elective varicose vein treatments throughout the UK, which seems to be due to non-uniform financial restrictions applied by Primary Care Trusts (PCTs). We, therefore, aimed to analyse national trends in the choice and selection of treatment of varicose veins between 1998 and 2008 within the NHS.
Subjects and Methods
We interrogated the data retrieved from a UK Department of Health (DH) run website <http://www.hesonline.nhs.uk> (Hospital Episode Statistics). HES is a data warehouse containing details of all admissions to NHS hospitals in England. It includes information about public and private patients treated in NHS hospitals, patients who were resident outside of England and about care delivered by treatment centres (including those in the independent sector) funded by the NHS. HES also holds details of all NHS out-patient appointments in England. We derived information variables from HES for a period of 10 years, from 1998–2008.
The diagnoses are currently coded according to International Classification of Diseases, 10th Revision (ICD-10). Surgical procedures (operations) are coded according to Office of Population, Censuses and Surveys: Classification of Surgical Operations and Procedures, 4th Revision (OPCS-4). During 2006–2007, the version of OPCS used to record procedures and interventions in HES changed from OPCS-4.2 to OPCS-4.3. This further changed in 2007–2008 to OPCS-4.4. All codes that were in OPCS-4.2 and OPCS-4.3 remain in OPCS-4.4, and new codes were added to reflect changing clinical practice. At the same time, the HES Main operation tables were renamed main procedures and interventions.
Various definitions and terminologies used in the data are described below:
Finished episodes: A count of the number of HES records, submitted on behalf of English NHS hospital providers that relate to episodes of admitted patient care that ended during the financial year (1 April to 31 March).
Waiting list: Episodes with an elective admission method indicating that the admission was from a waiting list. Planned admissions are not included (planned admission is used where a patient is waiting for treatment for clinical reasons, rather than until resources become available).
Waiting time: Waiting time in HES is the period between the date of the decision to admit and the date of actual admission. Days of deferment and suspension are not yet taken into account. The waiting-time statistics produced from HES are not comparable with the official waiting list figures. The latter provide an indication of the numbers waiting to be admitted on a particular date, and how long they have been waiting up to that date.
Length of stay: A spell is a period of continuous admitted patient care within a particular NHS trust, calculated by subtracting the admission date from the discharge date. In HES, this involves selecting records that are the last in the spell and, therefore, contain a discharge date. All ‘discharge records’ also carry an admission date because, where the spell consists of more than one episode, the admission date is carried forward from earlier episode(s) in the spell. Day cases, which have a length of stay of zero days, are excluded from this calculation.
Bed days: The sum of all the days that patients in the group occupied hospital beds during the financial year (1 April to 31 March).
The procedures (using OPCS–4 classification) analysed can be seen in Table 1.
Table 1.
Analysed treatment procedures for varicose veins (using OPCS 4 classification)
| L84 – Combined operations on varicose vein of leg |
| L84.1 Combined operations on primary long saphenous vein (LSV) |
| L84.2 Combined operations on primary short saphenous vein (SSV) |
| L84.3 Combined operations on primary long and short saphenous vein |
| L84.4 Combined operations on recurrent long saphenous vein |
| L84.5 Combined operations on recurrent short saphenous vein |
| L84.6 Combined operations on recurrent long and short saphenous vein |
| L84.8 Other specified combined operations on varicose vein of leg |
| L84.9 Unspecified combined operations on varicose vein of leg |
| L85 – Ligation of varicose veins of leg |
| L85.1 Ligation of LSV |
| L85.2 Ligation of SSV |
| L85.3 Ligation of recurrent varicose veins of leg |
| L85.8 Other specified |
| L85.9 Unspecified |
| L86 – Injection into varicose vein of leg |
| L86.1 Injection of sclerosing substance in varicose veins of leg |
| L86.2 Ultrasound-guided foam sclerotherapy for varicose vein of leg |
| L86.8 Other specified |
| L86.9 Unspecified |
| L87 – Other operations on varicose vein of leg |
| L87.1 Stripping of LSV |
| L87.2 Stripping of SSV |
| L87.3 Stripping of varicose vein of leg NEC |
| L87.4 Avulsion of varicose vein of leg |
| L87.5 Local excision of varicose vein of leg |
| L87.6 Incision of varicose vein of leg |
| L87.7 Transilluminated powered phlebectomy of varicose vein of leg |
| L87.8 Other specified |
| L87.9 Unspecified |
| L88 – Transluminal operations on varicose vein of leg |
| L88.1 Percutaneous transluminal laser ablation of long saphenous vein |
| L88.2 Radiofrequency ablation of varicose vein of leg |
| L88.3 Percutaneous transluminal laser ablation of vein NEC |
| L88.8 Other specified transluminal operations on varicose vein of leg |
| L88.9 Unspecified transluminal operations on varicose vein of leg |
Results
Total finished consultant episodes (L84, L85, L86, L87, and L88)
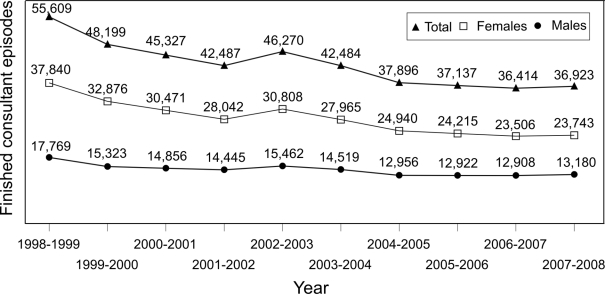
Over the last 10 years, there has been a 34% decline in the number of total (L84–L88) finished consultant episodes (FCEs) for varicose veins treatment. A total of 55,609 procedures were performed in 1998–1999 whereas only 36,923 were performed in 2007–2008 (Fig. 1). The fall in the number of female patients (37%; 37,840 to 23,743) was greater than the fall in the number of male patients (26%; 17,769 to 13,180).
Figure 1.
Finished consultant episodes (FCEs) for total procedures (L84–L88) performed for varicose vein treatment from 1998–2008, with men/women distribution.
On comparing the different age groups, the working population subgroup (15–59 years) consistently formed the bulk of the patients (about 70–80%), but there was a fall in the numbers of total FCEs (78.1% in 1998–1999 to 71.7% in 2007–2008). Whereas, in the over 60-year-old population subgroup, the proportion of total FCEs was found to be increasing (21.9% in 1998–1999 to 28.2% in 2007–2008), which explains an increase in the mean age from 48 years in 1998–1999 to 50 years in 2007–2008.
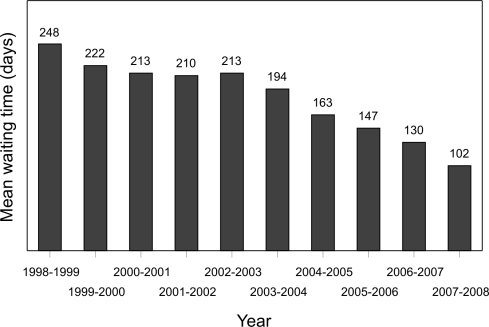
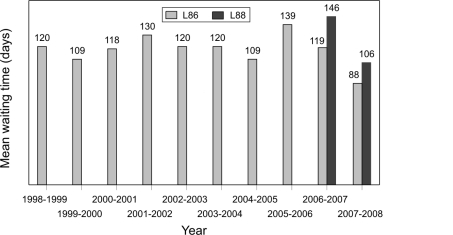
Waiting times have also declined over the examined period. The mean waiting time in 2007–2008 was 102 days as compared to 248 days in 1998–1999; a mean reduction of 146 days (59%) over the 10-year period (Fig. 2).
Figure 2.
Mean waiting times for total procedures (L84–L88) performed for varicose veins treatment from 1998–2008.
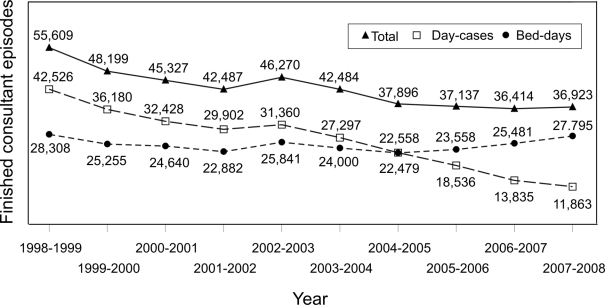
In contrast to these falling trends, there has been an increase in the proportion of the day-case procedures performed. Of the total procedures, 51% were performed as a day case in 1998–1999 whereas in 2007–2008 this increased to 75.3%. As a result of this, 30,663 bed days were saved in 2007–2008 (11,863 bed days) in comparison to 42,526 bed days used in 1998–1999 – a 72% reduction (Fig. 3). There was also a reduction in the mean length of stay from 1.6 days (1998–1999) to 1 day (2007–2008).
Figure 3.
Day cases and bed days used for total procedures (L84–L88) performed for varicose veins treatment from 1998–2008.
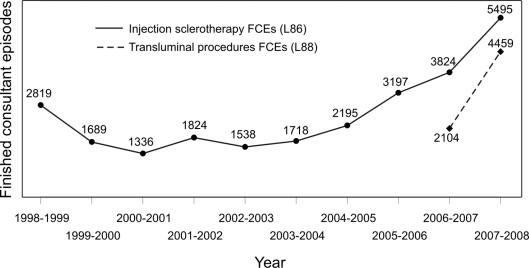
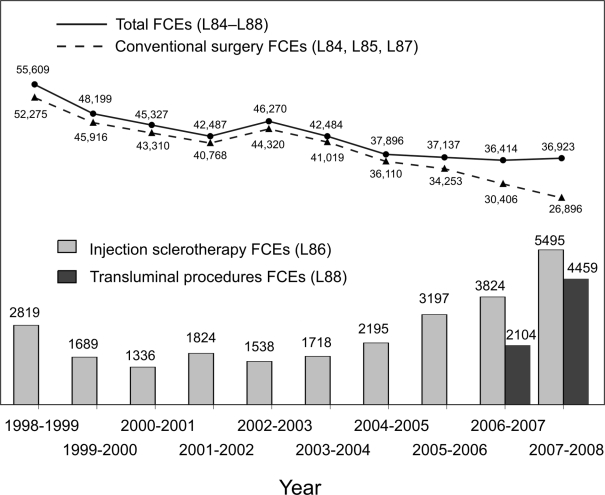
Minimally invasive procedures (L86, L88)
Until 2005–2006, injection sclerotherapy (L86) was the only minimally invasive treatment for varicose veins that was being coded (OPCS-4.2). It was only after the introduction of OPCS-4.3 (the newer version) in 2006–2007, that more codes (L88) were added for other novel treatments such as radiofrequency ablation, laser ablation, etc. For this reason, the trends in L86 and L88 have been analysed separately.
In the late 1990s, there was a falling trend in patients undergoing injection sclerotherapy (Fig. 4). Since the year 2000–2001, there has been an impressive 311% rise in the number of FCEs for this treatment. Although the procedure has more commonly been offered to the women, the proportion of men receiving the treatment is increasing. Between 2000–2001 and 2007–2008, there was an 809% increase in the number of male patients opting for this procedure, and a 231% increase in the number of female patients. About 98% of these procedures were performed as a day case in 2007–2008. Until the year 2005–2006, the waiting times for this treatment had increased over the years. On average, patients waited for approximately 139 days in the year 2005–2006 as compared to 120 days in 1998–1999. Interestingly, despite a huge increase in the total number of these procedures performed, the waiting times have come down to an average of 88 days in the last 2 years (Fig. 5). The proportion of patients of working age undergoing this treatment followed a similar fluctuation pattern which steadily increased from 71.3% in 1998–1999 to 77.4% in 2005–2006 followed by a decline to reach 64% in 2007–2008. In contrast to this, the proportion of over 60-year-old patients initially declined from 28.5% in 1998–1999 to 22.5% in 2005–2006 followed by a sharp rise to 35.7 % by 2007–2008. Therefore, the mean age has changed from 51 years in 1998–1999 to 53 years in 2007–2008.
Figure 4.
Finished consultant episodes (FCEs) for minimally invasive procedures (L86 and L88) performed for varicose vein treatment from 1998–2008.
Figure 5.
Mean waitingtimes for minimally invasive procedures (L86 and L88) performed for varicose vein treatment from 1998–2008.
The total FCEs for transluminal procedures (L88) were twice the number in 2007–2008 (4459) than in 2006–2007 (2104). Much of the contribution was from percutaneous laser ablation procedures (89% in 2007–2008) whereas radiofrequency ablation was performed in just 454 patients (11%). Most of these patients were women (63% in 2007–2008). Of these patients, 66% were from a working age group and 34% were over 60 years in age. Of the total FCEs for the patients undergoing transluminal procedures, 90% were performed as day cases. Despite the increase in the number of procedures performed, their waiting times reduced impressively from 146 days in 2006–2007 to 106 days in 2007–2008.
Conventional surgical treatment (L84, L85 and L87)
Analysing the trends of the conventional surgical methods for varicose veins, there has been a 48.5% decline since 1998–1999, more noticeably in women (51.5%) compared to men (42.5%). The mean waiting times have come down from 251 days in 1998–1999 to 147 days in 2007–2008 – a drop of 148 days (58.7%). The working population have shown a decline in demand from 78.1% in 1998–1999 to 74.3% in 2007–2008. Subsequently, the older population (> 60 years) shows a greater contribution, 26% in 2007–2008 as compared to 22% in 1998–1999. There was an increase in mean age from 47.7 years in 1998–1999 to 49.8 years in 2005–2006. In 1998–1999, 48% of these procedures were being performed as day cases, versus 68% in 2007–2008. Thus 31,353 bed days were saved in 2007–2008 – a 73.8% reduction. This 73.8% reduction of bed days is not proportional to the 48.5% reduction in the usage of this treatment and thus is clearly an indicator of improved efficiency in the English NHS.
Discussion
Treatment for varicose veins is one of the most common procedures carried out in the NHS. It accounts for a large number of out-patient visits in primary and secondary care and, as such, poses a huge burden for the NHS.5 Various treatment options are now available. The main forms of treatment used are conservative treatment, surgery and minimally invasive procedures. The minimally invasive treatments are foam sclerotherapy, endovenous laser ablation and radiofrequency ablation; all of these are supported by the National Institute for Health and Clinical Excellence (NICE).6–8 However, the provision of these treatment options varies according to locality.5,9 This variation is dependent on the level of funding provided by the primary care trusts in each region. Both standard surgical treatment and ultrasound-guided foam injection sclerotherapy have now been proven to be clinically- and cost-effective treatments for varicose veins. The incremental cost effectiveness ratio (ICER) of both of these procedures is well below the threshold normally considered appropriate for the funding of treatments within the NHS.5 ICER is the incremental cost incurred for an increment in benefit of a treatment to achieve one quality adjusted life year (QALY) and the willingness to pay (WTP) threshold is £30,000 per QALY.5 Still, there is considerable variation in the treatment options offered, within the trusts.
Over the last decade there has been major change in the management options for varicose veins in the English NHS with a consistent decline in the number of total FCEs for the treatment of varicose veins. A parallel fall in the number of FCEs for surgical management has also been noted (Fig. 6). This may be due to a combination of the reduction in referrals for treatment from the PCTs as funding for varicose vein treatment is reduced leading to fewer cases being performed, and the increasing trend for surgeons not to review patients routinely after intervention. This could potentially have a negative impact on surgical training as the surgical treatment for varicose veins has traditionally been seen as a good training operation for junior surgeons. Unfortunately, HES online data represents only NHS patients in England (including NHS private patients) and we have no data on varicose vein provision within the private sector during this time period.
Figure 6.
Trend comparison of finished consultant episodes (FCEs) for total procedures (L84–L88), conventional surgery (L84, L85 and L87), injection sclerotherapy (L86) and transluminal (L88) procedures.
Traditional surgical procedures are still the most commonly practiced form of treatment and most vascular surgeons would consider surgical treatment as the gold standard. More and more are now being performed as day cases, in line with trends for other procedures within the NHS. As well as a reduction in the total number of cases performed, there has been a reduction in the number of bed days used between 1998–1999 and 2007–2008. There has also been a reduction in the waiting times, thus indicating the energy which has been put into the English NHS to improve patient care along with the introduction of waiting time targets.
Treatments such as injection sclerotherapy have been in use for many years, but its practice in the UK has been limited and varied.10 The initial treatment of local injection and compression has been used with mixed enthusiasm and differing indications, with a variety of methods used.11 Since the introduction of ultrasound-guided techniques and the use of aerated foam, sclerotherapy has become a well-established and widely accepted treatment in the vascular surgical community.12 However, there is no level-one evidence to prove its long-term superiority to traditional surgical treatment.4,13 Despite this, foam sclerotherapy and other minimally invasive procedures are becoming increasingly popular. In response to the increasing use of these procedures, NICE guidelines have been produced on alternative forms of treatment for varicose veins including radiofrequency ablation (2003),6 endovenous laser treatment (2004),7 and foam sclerotherapy (2007).8 Injection sclerotherapy was an unpopular treatment between the 1970s and the 1990s and conventional surgery became the norm; however, this has changed over the last 10 years. There are many possible reasons for this including financial considerations, availability of theatre space, waiting time targets, and patient choice, as local anaesthetic ‘office’-style treatments seem to be more acceptable to many patients as they impact less on their work and life-style. Therefore, this change in treatment modality has probably contributed to the reduction in the waiting lists for surgery over the last 2 years.
There has been some recent debate surrounding the risks of foam sclerotherapy following the publication of an article in the New England Journal of Medicine which demonstrated systemic embolisation of foam particles.14 Most clinicians using this technique consider it to be as safe as other treatments for varicose veins. Nevertheless, more research is required to examine its cost effectiveness and a randomised controlled trial is already in progress which aims to compare foam sclerotherapy, alone or in combination, with endovenous laser therapy, with conventional surgery as a treatment for varicose veins.9 Funded by the National Institute for Health Research as a part of its HTA (Health Technology Assessment) programme, it is planned to be completed by mid-2012, focusing on the clinical and cost effectiveness of these procedures.
There currently appears to be inadequate provision for minimally invasive procedures to NHS patients. Undoubtedly there is a huge market potential for these new generation treatments. This could prove economically and medically very beneficial to the English NHS. In order to realise this potential more efficiently and to the fullest, a more structured and organised planning of resources is required.
Acknowledgments
This paper is related to a study which was presented as a platform presentation at the Venous forum, Royal Society of Medicine, London, 3–4 April 2008. The authors and title of that study are: Kanwar A, Hansrani M, Lees TA, Stansby G. Trends in Varicose Vein Therapy in England: Radical changes over the last 8 years.
References
- 1.Callam MJ. Epidemiology of varicose veins. Br J Surg. 1994;81:167–73. doi: 10.1002/bjs.1800810204. [DOI] [PubMed] [Google Scholar]
- 2.Lees TA, Beard JD, Ridler BM, Szymanska T. A survey of the current manage ment of varicose veins by members of the Vascular Surgical Society. Ann R Coll Surg Engl. 1999;81:407–17. [PMC free article] [PubMed] [Google Scholar]
- 3.Tremblay J, Lewis EW, Allen PT. Selecting a treatment for primary varicose veins. Can Med Assoc J. 1985;133:20–5. [PMC free article] [PubMed] [Google Scholar]
- 4.Rigby KA, Palfreyman SJ, Beverley C, Michaels JA. Surgery versus sclerotherapy for the treatment of varicose veins. Cochrane Database Syst Rev. 2004;(Issue 4) doi: 10.1002/14651858.CD004980. CD004980. DOI: 10.1002/14651858.CD004980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Michaels JA, Campbell WB, Brazier JE, MacIntyre JB, Palfreyman SJ, et al. Randomised clinical trial, observational study and assessment of cost-effectiveness of the treatment of varicose veins (REACTIV trial) Health Technol Assess. 2006;10(13) doi: 10.3310/hta10130. [DOI] [PubMed] [Google Scholar]
- 6.NICE. Radiofrequency ablation of varicose veins. September 2003 < http://www.nice.org.uk/nicemedia/pdf/ip/ipg008guidance.pdf>.
- 7.NICE. Endovenous laser treatment of the long saphenous vein. March 2004 < http://www.nice.org.uk/nicemedia/pdf/IPG052guidance.pdf>.
- 8.NICE. Ultrasound-guided foam sclerotherapy for varicose veins. May 2007 < http://www.nice.org.uk/nicemedia/pdf/IPG217Guidance.pdf>.
- 9.Brittenden J. Randomised controlled trial comparing foam sclerotherapy, alone or in combination with endovenous laser therapy, with conventional surgery as a treatment for varicose veins. < http://www.hta.ac.uk/project/1728.asp?src=rss>. [Google Scholar]
- 10.Darke SG, Baker SJ. Ultrasound-guided foam sclerotherapy for the treatment of varicose veins. Br J Surg. 2006;93:969–74. doi: 10.1002/bjs.5423. [DOI] [PubMed] [Google Scholar]
- 11.Tisi PV, Beverley C, Rees A. Injection sclerotherapy for varicose veins. Cochrane Database Syst Rev. 2006;(Issue 4) doi: 10.1002/14651858.CD001732.pub2. CD001732. DOI: 10.1002/14651858.CD001732.pub2. [DOI] [PubMed] [Google Scholar]
- 12.Breu FX, Guggenbichler S, Wollmann JC. 2nd European Consensus Meeting on Foam Sclerotherapy 2006, Tegernsee, Germany. Vasa. 2008;37(Suppl 71):1–29. [PubMed] [Google Scholar]
- 13.Jia X, Mowatt G, Burr JM, Cassar K, Cook J, Fraser C. Systematic review of foam sclerotherapy for varicose veins. Br J Surg. 2007;94:925–36. doi: 10.1002/bjs.5891. [DOI] [PubMed] [Google Scholar]
- 14.Ceulen RPM, Sommer A, Vernooy K. Microembolism during foam sclerotherapy of varicose veins. N Engl J Med. 2008;358:1525–6. doi: 10.1056/NEJMc0707265. [DOI] [PubMed] [Google Scholar]