Abstract
INTRODUCTION
Obesity contributes to the development of knee osteoarthritis and complicates its surgical treatment. The aim of this study was to explore barriers to effective weight management in obese patients with knee osteoarthritis.
PATIENTS AND METHODS
A cross-sectional questionnaire study was performed in an elective out-patient setting and on an orthopaedic ward on patients with a body mass index (BMI) of 30 kg/m2 or over and knee osteoarthritis.
RESULTS
Of 47 patients approached, 45 agreed to participate. Forty of 45 patients (89%) had tried to lose weight at some point, 35 of 40 (87.5%) by adjusting their diet. Forty of 45 (89%) patients considered lack of motivation to be the greatest barrier to weight loss and only 13 of 45 (28%) pain in the knee. Patients with a BMI of less than 40 kg/m2 expressed a preference for dietary advice to help with weight loss, compared with those with a BMI of over 40 kg/m2 who expressed a preference for an NHS or other support group.
CONCLUSIONS
Obesity is a significant problem for many patients with knee osteoarthritis. Attendance at an orthopaedic clinic is an opportunity to address obesity, by providing information about diet and possibly support groups for morbidly obese patients. Patients may be motivated to lose weight to improve their symptoms.
Keywords: Weight loss, Obesity, Knee osteoarthritis
Obesity is a major issue in contemporary orthopaedic practice. Patients who are obese have an increased risk of developing osteoarthritis, particularly of the knee. Morbidly obese patients are at increased risk of peri-operative complications including problems with wound healing, infection, prolonged wound drainage, pulmonary embolism and deep vein thrombosis.1–4 Addressing weight management is important in improving the general health of patients in the orthopaedic clinic.5,6 However, many patients have difficulty with this. Empirical evidence suggests that most have tried weight management programmes in the past, and may have difficulty exercising because of their arthritis. The purpose of this survey was to determine what weight management strategies obese patients with knee osteoarthritis have explored in the past and what they perceive are the barriers to successful weight management.
Patients and Methods
A cross-sectional survey was undertaken in a large teaching hospital in the north east of England. Patients were selected from the clinics and ward admissions of four consultant orthopaedic surgeons specialising in lower limb arthroplas-ty, throughout the 4-week period of the study. Eligible patients were those with a body mass index (BMI) of 30 kg/m2 and over presenting with radiographic changes of knee osteoarthritis (either new or review), and were able to understand written English. Patients with other forms of arthritis were excluded. The survey instrument was a questionnaire. The questionnaire was piloted for one week and underwent minor revisions as a result before study patients were recruited. Piloted patients were not included as part of the study. The study was considered a service evaluation and did not require ethical approval.
A convenience sampling approach was used to select patients. Patients were asked if they would like to participate in clinic or on the ward, with the self-administered questionnaire being completed in private. There was a demographic section, which included items for age, gender, and self-reported weight, height and waist circumference. The next section contained questions about whether the patient had ever considered a weight loss programme, what strategies they had employed, how successful their attempts at weight loss were, what they considered to be the barriers to effective weight management and how they would approach weight management in the future.
Results
A total of 47 patients meeting the inclusion criteria were approached. Two declined to participate, leaving 45 patients (40 review and 5 new patients) who completed questionnaires. The mean age of participants was 67 years (range, 50–87 years) and the mean BMI 34 kg/m2 (range, 30–45 kg/m2). Twenty-five participants provided their waist circumference, whose mean was 40 inches (range, 36–48 inches). Twenty (44%) were male.
In the first three questions, participants were asked if their weight was a problem to them, to rate how important weight loss was to them and if they had ever tried to lose weight. Twenty-two of 45 (49%) found their weight to be a problem to them, with 23 of 45 (51%) rating weight loss as either extremely or very important. Forty of 45 (89%) had tried to lose weight at some point.
The next set of questions addressed participant's methods and attempts at weight loss. Of the patients who had tried to lose weight, 35 of 40 (87.5%) had changed their daily diet, 15 of 40 (37.5%) had tried increased exercise and 13 of 40 (32.5%) had attended a support group. The majority of patients, 22 of 40 (55%), lost less weight than expected. The mean weight loss was 9 kg (range, 2–30 kg), with only 10 of 40 (25%) managing to maintain the weight loss. The most useful method of weight loss in 29 of 40 (73%) was found to be a change of daily diet.
When the participants of this study were asked if a health professional had ever offered help with weight loss when they had consulted about another problem, 26 of 45 (58%) had received no help. Similarly, 30 of 45 (67%) had never consulted a doctor or another health professional about their weight. However, 29 of 45 (64%) thought that their weight had influenced their joint pains.
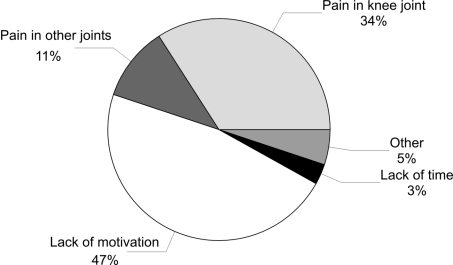
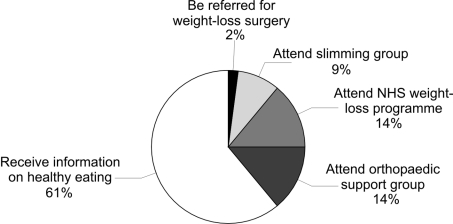
The greatest barrier to achieving a desired weight loss was a lack of motivation in 18 of 45 (40%) and in 13 of 45 (28%) pain in the knee joint (Fig. 1). The majority of patients, 24 of 45 (53%), wanted further information on weight loss strategies, with 27 of 45 (60%) stating a preference for being given information about healthy eating as their approach to losing weight (Fig. 2). Only 18 of 45 (40%) rated their likelihood of losing weight after treatment for their knee complaint as very likely or extremely likely.
Figure 1.
What do you think is the desired weight loss (n = 45)?
Figure 2.
What would be your preferred approach to losing weight (n = 45)?
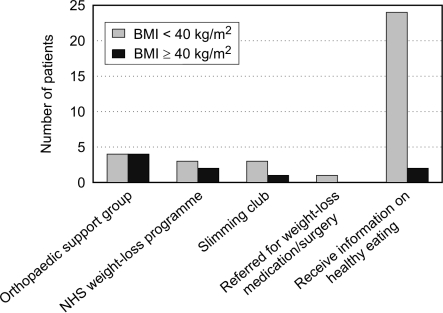
On comparison of patients' BMI and preferred method of weight loss, 6 of 9 (67%) with a BMI of 40 kg/m2 and over preferred either an orthopaedic support group or an NHS programme to aid them with weight loss compared with 6 of 36 (17%) with a BMI below 40 kg/m2. Only 2 of 9 (22 %) with a BMI of 40 kg/m2 and over rated their chance of losing weight after surgery as very likely or extremely likely, compared with 16 of 36 (44%) patients with a BMI below 40 kg/m2 (Fig. 3).
Figure 3.
What would be your preferred approach to losing weight by body mass index (n = 45)?
Discussion
The aim of this study was to explore barriers to weight management in obese patients with knee osteoarthritis. We believe this is a novel study addressing an important issue in orthopaedic practice.
We have shown that obese patients consider weight loss as important but, nevertheless, difficult. Most patients have tried to lose weight, most often by modifying their diets, but found it difficult to maintain weight loss. We found it interesting that patients reported lack of motivation rather than knee pain as being the greatest barrier to weight loss, as this runs counter to anecdotal evidence that patients report that they are unable to lose weight (particularly through exercise) until their knee pain has been treated (most often by joint replacement). It is, of course, important to emphasise that exercise is possible, even in the presence of knee arthritis.
The orthopaedic consultation provides an excellent opportunity to discuss obesity and weight loss strategies with patients who have knee arthritis. Treatment is complicated by obesity and so it is preferable to lose weight before the surgical intervention. This may be an incentive to a patient to lose weight before surgery.
The questionnaire did not ask patients if they perceived that their weight may increase the risk of them requiring knee replacement and/or having greater complications after surgery. This information may have highlighted if patients who perceived higher risks of needing surgery or developing complications after surgery were more likely to lose weight. In the absence of this association, it is not possible to ascertain if highlighting the increased incidence of peri-operative complications to patients would motivate them to lose weight and justify delaying surgery. Further qualitative work regarding what information or support would successfully motivate patients to lose weight is needed.
Although our study was small, a difference was seen between patients with a BMI of 40 kg/m2 and over and those with a BMI below 40 kg/m2, signalling that a different programme of care may be required in the morbidly obese subgroup. Based on this study, it would seem reasonable to offer patients with a BMI of less than 40 kg/m2 dietary advice. These patients appear to be more optimistic about their chances of losing weight. Heavier patients appear to express a desire for more support.
The weaknesses of this study include the fact that although the survey instrument had good face validity, it has not been formally tested for reliability and responsiveness. The number of patients recruited was small and for these reasons the results should be interpreted with caution. We believe however, that the sampled population is typical of that seen in routine orthopaedic practice.
Conclusions
Osteoarthritis of the knee is a degenerative condition and obesity plays a significant part in its development and is relevant to treatment. Although the majority of the patients who present to an out-patient clinic are typically older adults there is still willingness and sound medical evidence to support weight loss in this population. Obese patients presenting with knee osteoarthritis provide a unique opportunity to invoke change within this patient group. Further research is required from a multidisciplinary group to ascertain psychological barriers to weight loss and how we can best support and motivate these patients both before and after total knee replacement to optimise outcomes and improve their general health status. However, it should not be forgotten that the orthopaedic surgeon and his or her team hold a key position as specialists in engaging the obese patient in weight management.
Acknowledgments
The authors thank Mr Nigel Brewster, Consultant Orthopaedic Surgeon, and Mr David Weir, Consultant Orthopaedic Surgeon, (both at Department of Orthopaedic Surgery, Freeman Hospital, Newcastle upon Tyne, NE7 7DN, UK) for their participation in this study.
References
- 1.Liu B, Balkwill A, Banks E, Cooper C, Green J, Beral V. Relationship of height, weight and body mass index to the risk of hip and knee replacements in middle-aged women. Rheumatology (Oxford) 2007;46:861–7. doi: 10.1093/rheumatology/kel434. [DOI] [PubMed] [Google Scholar]
- 2.Winiarsky R, Earth P, Lotke P. Total knee arthroplasty in morbidly obese patients. J Bone Joint Surg Am. 1998;80:1770–4. doi: 10.2106/00004623-199812000-00006. [DOI] [PubMed] [Google Scholar]
- 3.Patel VP, Walsh M, Sehgal B, Preston C, DeWal H, Di Cesare PE. Factors asso ciated with prolonged wound drainage after primary total hip and knee arthro plasty. J Bone Joint Surg Am. 2007;89:33–8. doi: 10.2106/JBJS.F.00163. [DOI] [PubMed] [Google Scholar]
- 4.Mantilla CB, Horlocker TT, Schroeder DR, Berry DJ, Brown DL. Risk factors for clinically relevant pulmonary embolism and deep venous thrombosis in patients undergoing primary hip or knee arthroplasty. Anesthesiology. 2003;99:552–60. doi: 10.1097/00000542-200309000-00009. [DOI] [PubMed] [Google Scholar]
- 5.Messier SP, Loeser RF, Miller GD, Morgan TM, Rejeski WJ, et al. Exercise and dietary weight loss in overweight and obese older adults with knee osteoarthritis: the Arthritis, Diet, and Activity Promotion Trial. Arthritis Rheum. 2004;50:1501–10. doi: 10.1002/art.20256. [DOI] [PubMed] [Google Scholar]
- 6.Messier SP, Gutekunst DJ, Davis C, DeVita P. Weight loss reduces knee-joint loads in overweight and obese older adults with knee osteoarthritis. Arthritis Rheum. 2005;52:2026–32. doi: 10.1002/art.21139. [DOI] [PubMed] [Google Scholar]