Abstract
INTRODUCTION
The management of open tibial fractures in children represents a unique reconstructive challenge. The aim of the study was to evaluate the management of paediatric open tibial fractures with particular regard to soft tissue management.
PATIENTS AND METHODS
A retrospective case-note analysis was performed for all children presenting with an open tibial fracture at a single institution over a 20-year period for 1985 to 2005.
RESULTS
Seventy children were reviewed of whom 41 were males and 29 females. Overall, 91% (n = 64) of children suffered their injury as a result of a vehicle-related injury. The severity of the fracture with respect to the Gustilo classification was: Grade I, 42% (n = 29); Grade II, 24% (n = 17); Grade III, 34% (n = 24; 7 Grade 3a, 16 Grade 3b, 1 Grade 3c). The majority of children were treated with external fixation and conservative measures, with a mean hospital in-patient stay of 13.3 days. Soft tissue cover was provided by plastic surgeons in 31% of all cases. Four cases of superficial wound infection occurred (6%), one case of osteomyelitis and one case of flap failure. The limb salvage was greater than 98%.
CONCLUSIONS
In this series, complications were associated with delayed involvement of plastic surgeons. Retrospective analysis has shown a decreased incidence of open tibial fractures which is reported in similar studies. Gustilo grade was found to correlate with length of hospital admission and plastic surgery intervention. We advocate, when feasible, the use of local fas-ciocutaneous flaps (such as distally based fasciocutaneous and adipofascial flaps), which showed a low complication rate in children.
Keywords: Open tibial fracture, Soft tissue management, Children, Fasciocutaneous flaps
The management of open tibial fractures in children represents a unique reconstructive challenge compared with those in adults.1 Compared with similar injuries in adults, open tibial fractures in children have a better prognosis with regards to time to union, remodelling potential and infection.2,3 However, fractures in children have the ability to disturb growth and may have a profound psychological effect on the child. One must consider the time spent absent from school and the impact that reconstruction can have on aesthetic appearance, especially in girls.
The recently published British Orthopaedic Association/British Association of Plastic, Reconstructive and Aesthetic Surgeons (BOA/BAPRAS)4 guidelines form an excellent resource for all clinicians involved in the management of this condition. This study aims to promote awareness and adherence to these guidelines and outline the need for a combined and co-ordinated approach between senior plastic and orthopaedic surgeons. The national guidelines highlight the importance of other specialities (including radiology and microbiology) in providing optimal multidisciplinary management of a complex problem.
We have reviewed our experience over 20 years with open tibial fractures in children. Our institute is a specialist tertiary paediatric hospital with facilities on-site for both paediatric, plastic and orthopaedic surgery. In particular, we evaluated the soft tissue management and outcomes, and compared these with similar published series both in children and in adults.3,5,6
Patients and Methods
Seventy children were treated over a 20-year period. All children were admitted to the Royal Hospital for Sick Children, Edinburgh, either as direct referrals or from peripheral hospitals. Data from the first decade (January 1985 to December 1994) were published previously by Stewart et al.2 Data from the second decade up to December 2004 were analysed separately according to the same criteria. Retrospective case-note review of each patient was performed and the following were recorded: demographic information; length of hospital stay; Gustilo grade; initial management; time to debridement; soft tissue coverage; neurovascular compromise; section of tibial involved; complications; associated morbidity. Gustilo grading classification was obtained from the operative report. Wound debridement and lavage were performed under general anaesthetic. Contaminated and devitalised tissue was excised followed by irrigation of the wound with a sterile saline solution.
Results
Epidemiology
Of the 70 children reviewed, 59% (n = 41) were male and 41% (n = 29) were female. The average age was 8 years and 2 months (range, 2–14 years). As demonstrated in similar studies,2,3,6 the most common accident was a child being hit by a motor vehicle: Some 90% (63/70) of the children were admitted as a result of a vehicle-related injury.
Tibial fractures
Twenty-nine patients (42%) suffered Gustilo Grade I fractures, 17 (24%) Grade II fractures and 24 (34%) Grade III fractures. Within the Grade III fractures, seven (29%) children suffered Grade IIIa, 16 (67%) suffered Grade IIIb and one (4%) suffered Grade IIIc. Fractures were distributed in the proximal third (n = 5), middle third (n = 24; 34%) and distal third (n = 41; 59%).
Hospital policy within the department states that the initial debridement should be carried out by a consultant orthopaedic surgeon.
Initial management
The initial management of patients has varied little over the years with resuscitation being undertaken alongside treatment of associated injuries. Initial management plans included, analgesia, splintage, tetanus prophylaxis, and sterile dressings to cover the wound. All patients received broad-spectrum antibiotics until the fracture was covered.
Fracture management
In the first decade, the majority of children had their fractures managed conservatively with the application of a plaster cast (76%). In the second decade, this number was lower, at 26%. From 1995 to 2004, 67% of children were managed by external fixation, an increase from 16% in the previous decade.
Soft tissue management
Plastic surgery intervention was required in 31 % (n = 21) of children in this study. Overall, 91% (n = 48) of the Grade I–IIIa fractures were treated by conservative, primary or delayed closure. Only 8% (n = 4) of children were treated with split thickness skin grafts and one with a local flap.
Of the 16 Gustilo Grade 3b fractures, adequate soft tissue cover was achieved by the use of 15 local flaps (with or without skin grafts) and one free flap. The one grade IIIc fracture resulted in a below-knee amputation (Tables 1 and 2).
Table 1.
Soft tissue management for each Gustilo fracture grade
| Grade I | Grade II | Grade IIIa | Grade IIIb | Grade IIIc | |
|---|---|---|---|---|---|
| Conservative | 21 | 3 | 1 | ||
| Primary closure | 4 | 10 | 2 | ||
| Delayed closure | 4 | 2 | 1 | ||
| SSG only | 1 | 1 | 2 | ||
| Local flaps ± SSG | 1 | 15 | |||
| Free tissue transfer | 2 | ||||
| Amputation | 1 |
SSG, split thickness skin graft.
The total of 71 interventions is due to the fact that one of the free flaps undertaken failed and, as a result, a local flap was performed to cover the defect.
Table 2.
Flaps used to reconstruct Grade III injuries
| Flap | Number | |
|---|---|---|
| Distally based fasciocutaneous flap | 6 | |
| Adipofascial flap | 5 | |
| Proximally based fasciocutaneous flap | 3 | |
| Gastrocnemius flap (myocutaneous) | 1 | |
| Cross leg distally based fasciocutaneous | 1 | |
| Free latissimus dorsi flap | 1 | |
| Free rectus abdominis flap | 1 |
Complications
Four children suffered superficial wound infections. Two of these children suffered Grade II fractures and the other two were Grade III fractures, all of the patients responded to treatment with antibiotics. This reflects an overall 6% superficial wound infection rate.
Two free flaps were undertaken for soft tissue cover in Grade IIIb fractures. One latissimus dorsi flap was performed successfully. One free rectus abdominis flap failed and a local fasciocutaneous flap was undertaken to provide adequate soft tissue cover. The children who were referred via peripheral hospitals suffered skin necrosis, in each of these cases we attribute this complication to unrecognised degloving due to delay in plastic surgery involvement.
Complications associated with the use of local flaps were minimal, with only two flaps showing superficial wound infections. An angiogram after the failure of the free rectus abdominis showed that a compromise of the arterial tree was responsible. One child had a failure of a skin graft that healed after debridement and re-grafting. Another child had an incomplete graft take at the flap donor site.
The failure of the free rectus abdominis flap was a complication which required daily communication between the plastic and the orthopaedic team. Due to the significant bone loss associated with the fracture (80% of the bone circumference) combined with acute shortening, it was decided that the application of a Ilizarov frame (Fig. 1) was necessary. Following this decision, a more proximal tibial corticotomy was performed to allow lengthening and, finally, the fracture was closed with a lateral fasciocutaneous flap.
Figure 1.
Child in Ilizarov frame after lateral fasciocutaneous flap.
One patient who was managed in a peripheral hospital with external fixation and split thickness skin grafting went onto develop osteomyelitis. This patient was successfully treated by radical debridement; an ipsilateral fibular flap for bone loss and a proximally based fasciocutaneous flap to reconstruct the soft tissue defect.
In this series, no child developed compartment syndrome or non-union of fractures and there were no deaths. The child who suffered a Grade IIIc fracture had a below-knee amputation; thus, there was a limb salvage rate of above 98%.
Discussion
The updated national guidelines4 on the management of open tibial fractures is an essential resource for all professionals who deal with this condition. This report emphasises the need for a combined approach and effective communication between senior orthopaedic and plastic surgeons.
In our institute, we are fortunate that both specialist orthopaedic and plastic surgeons are available on site, but this should not be a barrier to effective communication and a combined approach.
The national guidelines suggest a move away from the Gustilo and Anderson grading, due to poor inter-observer reliability, and a move towards the AO system. The national guidelines also propose co-amoxiclav (1.2 g/8-hourly) or a cephalosporin (1.5 g/8-hourly) as the antibiotic of choice until first debridement.4 Guidelines suggest that antibiotic prophylaxis should be commenced as soon as possible and certainly within 3 h. Guidelines also advise on the early involvement of microbiology for advice.4
We believe that changes in fracture management are a reflection of the reconfiguration of services within our hospital. Prior to 1995, paediatric elective orthopaedics was at a different hospital; thus, the primary management of paediatric fractures rested with paediatric surgeons. Prior to 1995, orthopaedic input had to be requested by paediatric surgeons. In 1995, paediatric orthopaedics moved onsite to the Royal Hospital for Sick Children. Plastic surgeons have always been available on-site to provide assistance in the management of complex, open tibial fractures.
Naique et al.7 compared outcomes of adult open tibial fractures managed in either specialist or peripheral centres. They concluded that there was a higher complication rate when managed in peripheral centres and advocated the direct referral of open tibial fractures to specialist centres where both plastic and orthopaedics surgeons are available. The new guidelines highlight the difficulties in such an algorithmic approach, owing to geographical constraints, lack of resources and other areas of clinical controversy. National guidelines4 advocate that, when managing complex open fractures in institutes without both plastic and orthopaedic surgeons, an immediate referral is made to the nearest specialist centre. National guidelines4 also state that, if possible, the primary surgical treatment should take place at the specialist centre.
Toms et al.,8 via a postal survey, concluded that only 57% of orthopaedic consultants were aware of the BOA/BAPRAS 1997 guidelines. They also concluded that less than 29% of orthopaedic consultants would choose to consult a plastic surgeon pre-operatively in the management of this condition and only 43% would seek any involvement from plastic surgeons at all. This is of concern, as there is much evidence5,9,10 to suggest that delayed soft tissue cover has an adverse effect on prognosis. Indeed, this is the case with our results, where all children who suffered from skin necrosis were initially managed in peripheral hospitals resulting in a delay in plastic surgery involvement and a higher complication rate.
The lack of early pre-operative communication between plastic and orthopaedic surgeons may directly affect the treatment options available to the plastic surgeon. Early communication between specialities or a joint orthopaedic and plastic initial debridement can prevent damage to perforating vessels which may be needed in soft-tissue reconstruction. This may occur as a result of incisions made by extending wounds or during fasciotomies. Early consultation with plastic surgeons can allow for the provision of micro vascular procedures which have significant demands on both theatre and consultant time. Effective communication between plastic and orthopaedic teams enabled successful management of the child with a failed rectus abdominis flap as described above.
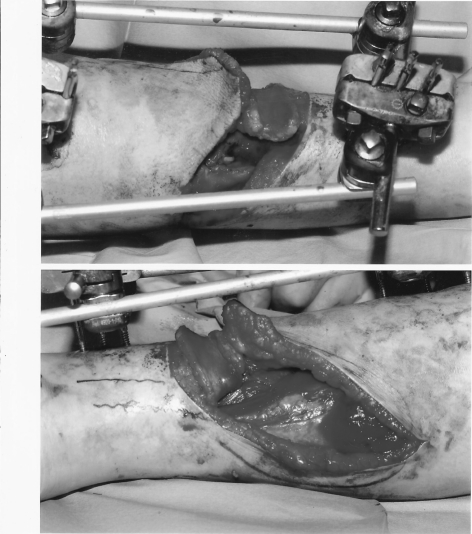
Our results showed that, overall, 31% of children received involvement from plastic surgeons either by way of skin grafting, local flaps11,12 or microvascular free flaps. The majority of plastic surgery involvement was for treatment of Grade III fractures (77%). In our unit, the most commonly used technique for soft tissue reconstruction was local flaps, in particular, the use of distally based fasciocutaneous flaps13 and adipo-fascial flaps (Figs 2 and 3).14,15 Our results were dominated by the use of local fasciocutaneous flaps which showed a low complication rate, with only two flaps, showing minor complications, both superficial wound infections. Islanding of the distally based fasciocutaneous flap was undertaken to allow greater defect coverage as well as an improved aesthetic appearance.13
Figure 2.
External fixation before adipofascial flap.
Figure 3.

Same child as in Figure 2 showing healing of the adipofascial flap.
Other series6,16 have shown an increased usage of micro vascular techniques and, when undertaking local flaps, have favoured the use of myocutaneous flaps.16 Our series shows that we have a low complication rate with the utilisation of local fasciocutaneous flaps with only two minor complications and no episodes of local flap failure. The advantage of local flaps are that they require less operating and consultant times compared to microvascular techniques. The guidelines suggest that there is no definitive clinical evidence for the use of one form of soft tissue coverage over another. Guidelines suggest that, from experimental data, metaphyseal fractures around the ankle might be best covered by fasciocutaneous flaps.4 To date, only two patients have needed surgical revision for cosmetic defects of local flaps. Both flaps were treated with liposuction at the pedicle and the removal of excess scar tissue.
Current literature3 suggests that open fractures in children heal faster and with less complications than in adults. The incidence of infections both superficial and deep was 7% which compares favourably with similar studies in adults which varies from 9.5–24%.16–18 There was one child who suffered from osteomyelitis and this is thought to be attributed to a referral from a peripheral hospital resulting in delayed involvement of plastic surgeons. The children who suffered superficial skin infections and flap failure were all older than 11 years, in agreement with Song et al.,3 who demonstrated that healing of open tibial fractures is better in children under the age of 11 years.
In the first decade from 1985–1994, there were 49 children who were diagnosed with open tibial fractures; from the period of 1995–2004, there were only 21 children who were diagnosed with open tibial fractures in the same department within the same catchment area. This decrease may be due to increasing government intervention of speeding vehicles in built-up areas. This finding was also reported by Weiss et al.19 who showed a decreasing incidence of tibial shaft fracture in adults of 12% in a more statistically significant study over a period of 6 years.
Throughout the series, no child suffered compartment syndrome and this was comparable to results of Jones et al.6 in a similar institute in Glasgow. The lack of children suffering from compartment syndrome combined with the 7% figure of wound infection further the idea that healing of children's open tibial fractures is associated with less morbidity than that of adults.1,2,3,5
There was strong correlation between Gustilo classification, the length of hospital stay and the stage of the reconstruction ladder used. Grade I fractures had an average of hospital stay of 6.7 days, Grade II an average of 11.2 days and Grade III an average of 19.4 days. It was also noted that 77% of Grade III fractures required involvement from plastic surgeons. It was also noted that skin grafting was used throughout the spectrum of Gustilo-graded fractures further re-instating the need for the early opinion of plastic surgeons and dispelling the myth that only Grade III fractures require involvement from plastic surgeons.
Conclusions
More emphasis must be placed upon the combined and early involvement of both plastic and orthopaedic surgeons in the management of children's open tibial fractures. The simplest approach as advised by the national guidelines would be to have senior plastic and orthopaedic surgeons present at the time of initial debridement to form a combined and effective management plan. With regards to soft tissue cover, we advocate the early use of local fasciocutaneous flaps which appear to be associated with few complications. The delay of plastic surgery involvement was associated with increased morbidity. The social and psychological impact this injury can have on a child should not be neglected. The management of open tibial fractures requires an effective multidisciplinary approach to provide children with an optimal outcome.
Acknowledgments
This work was given, in part, as a poster presentation at the Summer BAPRAS Meeting 2009. Royal Armouries, Leeds, UK.
References
- 1.Robb J. Open fractures in children: difference between adult and children's fractures. In: Court-Brown CM, McQueen M, Quaba AA, editors. Management of Open Fractures. 1st edn. London: Martin Dunitz; 1996. pp. 333–42. [Google Scholar]
- 2.Stewart KJ, Tytherleigh-Strong G, Bharathwaj S, Quaba AA. The soft tissue management of children's open tibial fractures. J R Coll Surg Edinb. 1999;44:24–30. [PubMed] [Google Scholar]
- 3.Song KM, Sangeorzan B, Benirschke S, Browne R. Open fractures of the tibia in children. J Paediatr Orthop. 1996;16:635–9. doi: 10.1097/00004694-199609000-00016. [DOI] [PubMed] [Google Scholar]
- 4.Standards for the management of open fractures of the lower limb. London: Royal Society of Medicine Press; 2009. British Association of Plastic, Reconstructive and Aesthetic Surgeons. [Google Scholar]
- 5.Kreder HJ, Armstrong P. A review of open tibia fractures in children. J Paediatr Orthop. 1995;15:482–8. doi: 10.1097/01241398-199507000-00015. [DOI] [PubMed] [Google Scholar]
- 6.Jones BG, Duncan RD. Open tibial fractures in children under 13 years of age – 10 years' experience. Injury. 2003;34:776–80. doi: 10.1016/s0020-1383(03)00031-7. [DOI] [PubMed] [Google Scholar]
- 7.Naique SB, Pearse M, Nanchahal J. Management of severe open tibial fractures: the need for combined orthopaedic and plastic surgical treatment in specialist centres. J Bone Joint Surg Br. 2006;88:351–7. doi: 10.1302/0301-620X.88B3.17120. [DOI] [PubMed] [Google Scholar]
- 8.Toms AD, Green AL, Giles S, Thomas PB. The current management of tibial fractures: are clinical guidelines effective? Ann R Coll Surg Engl. 2003;85:413–6. doi: 10.1308/003588403322520825. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Fischer MD, Gustilo RB, Varecka TF. The timing of flap coverage, bonegrafting, and intramedullary nailing in patients who have a fracture of the tibial shaft with extensive soft-tissue injury. J Bone Joint Surg Am. 1991;73:1316–21. [PubMed] [Google Scholar]
- 10.Caudle RJ, Stern PJ. Severe open fractures of the tibia. J Bone Joint Surg Am. 1987;69:801–7. [PubMed] [Google Scholar]
- 11.Ponten B. The fasciocutaneous flap: its use in soft tissue defects of the lower leg. Br J Plast Surg. 1981;34:215–20. doi: 10.1016/s0007-1226(81)80097-5. [DOI] [PubMed] [Google Scholar]
- 12.Cormack GC, Lamberty BG. A classification of fasciocutaneous flaps according to their patterns of vascularisation. Br J Plast Surg. 1984;37:80–7. doi: 10.1016/0007-1226(84)90049-3. [DOI] [PubMed] [Google Scholar]
- 13.Erdmann MWH, Court-Brown CM, Quaba AA. A five-year review of islanded distally based fasciocutaneous flaps on the lower limb. Br J Plast Surg. 1997;50:421–7. doi: 10.1016/s0007-1226(97)90329-5. [DOI] [PubMed] [Google Scholar]
- 14.Lee S, Estella CM, Burd A. The lateral distally based adipofascial flap of the lower limb. Br J Plast Surg. 2001;54:303–9. doi: 10.1054/bjps.2001.3579. [DOI] [PubMed] [Google Scholar]
- 15.Lin SD, Chou CK, Lin TM, Wang HJ, Lai CS. The distally based lateral adipofascial flap. Br J Plast Surg. 1998;51:96–102. doi: 10.1054/bjps.1997.0267. [DOI] [PubMed] [Google Scholar]
- 16.Gopal S, Majumder S, Batchelor AG, Knight SL, De Boer P, Smith RM. Fix and flap: the radical orthopaedic and plastic treatment of severe open fractures of the tibia. J Bone Joint Surg Br. 2000;82:959–66. doi: 10.1302/0301-620x.82b7.10482. [DOI] [PubMed] [Google Scholar]
- 17.Gustilo RB, Mendoza RM, Williams DN. Problems in the management of type III (severe) open fractures: a new classification of type III open fractures. J Trauma. 1984;24:742–6. doi: 10.1097/00005373-198408000-00009. [DOI] [PubMed] [Google Scholar]
- 18.Keating JF, Blachut PA, O'Brien PJ, Court-Brown CM. Reamed nailing of Gustilo grade-III B tibial fractures. J Bone Joint Surg Br. 2000;82:1113–6. doi: 10.1302/0301-620x.82b8.10566. [DOI] [PubMed] [Google Scholar]
- 19.Weiss RJ, Montgomery SM, Ehlin A, Al Dabbagh Z, Stark A, Jansson KA. Decreasing incidence of tibial shaft fractures between 1998 and 2004: information based on 10,627 Swedish inpatients. Acta Orthop. 2008;79:526–33. doi: 10.1080/17453670710015535. [DOI] [PubMed] [Google Scholar]
- 20.Levy AS, Wetzler M, Lewars M, Bromberg J, Spoo J, Whitelaw GP. The orthopedic and social outcome of open tibia fractures in children. Orthopedics. 1997;20:593–8. doi: 10.3928/0147-7447-19970701-05. [DOI] [PubMed] [Google Scholar]